Back to Journals » Research and Reports in Urology » Volume 14
Impacts of Neoadjuvant Hormonal Therapy Prior to Robot-Assisted Radical Prostatectomy on Postoperative Hormonal- and Sexual-Related Quality of Life – Assessment by Patient-Reported Questionnaire
Authors Ogawa S, Hasegawa A, Makabe S, Onagi A, Matsuoka K, Kayama E, Koguchi T, Hata J, Sato Y, Akaihata H, Kataoka M, Haga N, Kojima Y
Received 18 October 2021
Accepted for publication 2 February 2022
Published 19 February 2022 Volume 2022:14 Pages 39—48
DOI https://doi.org/10.2147/RRU.S342063
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Panagiotis J Vlachostergios
Soichiro Ogawa,1 Akihisa Hasegawa,1 Shunta Makabe,1 Akifumi Onagi,1 Kanako Matsuoka,1 Emina Kayama,1 Tomoyuki Koguchi,1 Junya Hata,1 Yuichi Sato,1 Hidenori Akaihata,1 Masao Kataoka,1 Nobuhiro Haga,2 Yoshiyuki Kojima1
1Department of Urology, Fukushima Medical University School of Medicine, Fukushima, Japan; 2Department of Urology, Fukuoka University Faculty of Medicine, Fukuoka, Japan
Correspondence: Soichiro Ogawa, Department of Urology, Fukushima Medical University School of Medicine, 1, Hikarigaoka, Fukushima, 960-1295, Japan, Tel +81 24 547 1316, Fax +81 24 548 3393, Email [email protected]
Purpose: Neoadjuvant hormonal therapy (HT) before radical prostatectomy (RP) is not recommended by current guidelines in terms of oncological outcomes. Despite this, neoadjuvant HT is sometimes conducted before RP for a small proportion of patients in clinical practice. This study evaluated the impacts of neoadjuvant HT on hormonal- and sexual-related quality of life (QOL) among patients who underwent robot-assisted RP (RARP).
Materials and Methods: Participants comprised 470 patients divided into a non-neoadjuvant HT group (n = 408) and a neoadjuvant HT group (n = 62). Hormonal- and sexual-related QOL were measured using the Expanded Prostate Cancer Index Composite (EPIC) questionnaire.
Results: Hormonal summary scores at 6 and 9 months, function scores before and 3, 6, and 9 months and bother score at 6 months after RARP were significantly lower in the neoadjuvant HT group than in the non-neoadjuvant HT group. Sexual function scores were decreased in the neoadjuvant HT group compared to the non-neoadjuvant HT group before and 6 months after RARP. In the neoadjuvant HT group, sexual function at 3 months after RARP was significantly worse in patients with > 5 months of neoadjuvant HT than in patients with ≤ 5 months of neoadjuvant HT. Conversely, sexual bother at 3 months after RARP was significantly worse in patients with ≤ 5 months of neoadjuvant HT than in patients with > 5 months of neoadjuvant HT.
Conclusion: Vintage neoadjuvant HT prior to RARP should not be recommended due to not only oncological outcomes, but also the impacts on postoperative hormonal- and sexual-related QOL.
Keywords: androgen deprivation therapy, Expanded Prostate Cancer Index Composite, quality of life, hormonal therapy, neoadjuvant, robot-assisted radical prostatectomy
Introduction
Radical prostatectomy (RP) has been performed for localized and locally advanced prostate cancer (PCa).1,2 Since long-term survival is expected for patients who undergo RP, postoperative quality of life (QOL) represents a major issue in the treatment of PCa.
Systemic neoadjuvant treatment prior to surgery has been performed for some kinds of malignancy, with the intention of improving prognosis by decreasing positive margins, metastatic lymph nodes and disseminated microscopic metastases. As for PCa, vintage hormonal therapy by agents such as anti-androgen drugs and luteinizing hormone-releasing hormone (LHRH) agonists before RP can achieve downstaging, but neither biochemical recurrence nor cancer-specific survival appear related to neoadjuvant hormonal therapy (HT).3 As a result, neoadjuvant HT prior to RP is not recommended in current guidelines except for in clinical trials.4–6 Despite this recommendation, vintage neoadjuvant HT before RP has still been conducted for a small proportion of patients, even in recent years.7,8 Hormonal therapy is known to cause a variety of adverse events (AEs), including hot flashes, gynecomastia, degenerated libido, and erectile dysfunction,9 thereby decreasing QOL.10,11
To date, the effects of neoadjuvant HT on QOL after RP are not fully understood. Elucidating the influence of neoadjuvant HT on postoperative QOL is significant, because patients require information about potential risks before deciding on treatment.12 Therefore, this study examined postoperative hormonal- and sexual-related QOL using a patient-reported questionnaire to reveal the impacts of neoadjuvant HT on QOL after robot-assisted RP (RARP).
Materials and Methods
Patients
A total of 542 consecutive patients who underwent RARP at Fukushima Medical University Hospital, Fukushima, Japan between April 2013 and September 2019 participated in this observational clinical cohort study. All patients underwent RARP using a four-arm Da Vinci Si surgical system (Intuitive Surgical Incorporation, Sunnyvale, CA, USA). Combined posterior and anterior intraperitoneal approaches and early exposure of the seminal vesicles and vasa deferentia were carried out. Nerve-sparing surgery was performed for D’Amico low-intermediate risk patients13 without suspicious lesions on magnetic resonance imaging. The nerve-sparing techniques were inter- or intrafascial based on periprostatic fascial anatomy.14
Neoadjuvant HT
Vintage neoadjuvant HT had already been started by urologists at the referring hospitals due to patient concerns regarding disease progression during the preoperative waiting period, or as part of combination therapy with radiation that was later canceled. Patients were given non-steroidal anti-androgen drugs, LHRH agonists, or LHRH agonists in combination with anti-androgen drugs, as so-called combined androgen blockade (CAB). Dosing duration and types of hormonal agents were selected by the previous urologists of each patient.
Data Collection
Figure 1 shows the flow chart for patient selection. Of the 542 patients, 21 patients who stopped visiting our outpatient clinic within 12 months after RARP and 31 patients who received salvage and/or adjuvant therapies such as hormonal or radiotherapy within the first 12 months were excluded. Another 19 patients who started neoadjuvant HT after preoperative evaluation were also ruled out. In addition, a patient in whom RARP was converted to open surgery due to severe adhesion to the rectum was also excluded. A final total of 470 patients was therefore analyzed in this study.
According to whether neoadjuvant HT was administered at least once, patients were divided into two groups: the neoadjuvant HT group (n = 62); and the non-neoadjuvant HT group (n = 408) (Figure 1). The following data were collected and analyzed for this study: patient age as of the time of surgery; initial prostate-specific antigen (PSA) values; clinical T stage; biopsy grade group (GG) according to the International Society of Urological Pathology classification;15 biopsy Gleason score (GS); D’Amico risk classification;13 and the number of patients who underwent nerve-sparing procedures. All study protocols were approved by the Ethics Committee of Fukushima Medical University (clinical approval no. 2334) and performed in accordance with the principles of the Declaration of Helsinki. All patients provided written informed consent prior to study commencement.
Evaluation of Hormonal- and Sexual-Related QOL Before and After RARP
To evaluate disease-specific QOL, patients were hand-delivered and asked to complete the Japanese version of EPIC questionnaire by nurses or outpatient clinicians preoperatively, and at 1, 3, 6, 9, and 12 months postoperatively.16 The Japanese version of EPIC has already been validated and used for large-scale studies in Japan.17,18 EPIC has 50 items regarding function, bother, and satisfaction. Function and bother compose the hormonal, sexual, urinary, and bowel domains, consisting of three hormonal (summary, function, and bother), three sexual (summary, function, and bother) five urinary (summary, function, bother, irritative/obstruction, and incontinence), and three bowel (summary, function, and bother) scales, respectively. All EPIC items consist of 5-point Likert scales. Scores range from 0 to 100, with higher scores indicating better health status. In this study, urinary, bowel, and satisfaction scales were excluded because the aim of this study was to clarify the impacts of neoadjuvant HT prior to RARP on postoperative hormonal- and sexual-related QOL, and hormonal therapy has been reported to have no effect on urinary, bowel or satisfaction QOL scores.11,19
Statistical Analysis
Statistical analyses were conducted using the Mann–Whitney U-test followed by preliminary Shapiro–Wilk test for continuous variables. The chi-squared and Fisher’s exact test were performed to compare the distribution of categorical outcome variables such as clinical T stage, biopsy GG (GS), D’Amico risk classification and use of nerve-sparing procedures. Mann–Whitney’s U-test was applied to compare age at the time of surgery, initial PSA values and scores on EPIC questionnaires at 1, 3, 6, 9, and 12 months postoperatively. Statistical analyses were performed using SPSS® Statistics version 26 for Windows® (Statistical Package for Social Science, Chicago, IL) or STATCEL® version 3 software (add-in software for Microsoft Excel; OMS Publishing Inc., Saitama, Japan). Values of p < 0.05 were defined as statistically significant.
Results
Patient Characteristics
Patient characteristics for each group are listed in Table 1. Median age at surgery and initial PSA values were similar between groups. The numbers of patients with clinical T1c, T2, and T3 stage in the neoadjuvant HT group were 28 (45.2%), 34 (54.8%), and 0 (0%), respectively. On the other hand, the numbers of patients with clinical T1c, T2, and T3 stage in the non-neoadjuvant HT group were 121 (29.7%), 260 (63.7%), and 26 (6.4%), respectively. This distribution differed significantly between groups (p = 0.013). A significant difference in the distribution of biopsy GG (GS) was apparent between groups (p = 0.0015). However, D’Amico risk classification did not differ significantly between groups (p = 0.324). No difference was seen in the distribution of the numbers of patients who received nerve-sparing procedures (p = 0.692).
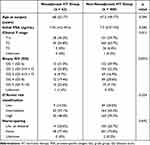 |
Table 1 Background Characteristics and Pre- and Intraoperative Parameters of Patients |
EPIC Questionnaire Collection Rates
Collection rates for the EPIC questionnaire in the neoadjuvant HT group before and 1, 3, 6, 9, and 12 months after RARP were 82.3%, 90.3%, 95.2%, 96.8%, 95.2%, and 98.4%, respectively. Collection rates in the non-neoadjuvant HT group at each time point were 78.9%, 89.5%, 93.0%, 92.6%, 91.9%, 93.9%, and 97.1%, respectively. Collection rates at each time point did not differ significantly between groups. Overall collection rates at each time point were 79.4%, 89.6%, 93.0%, 92.6%, 94.0% and 97.2%, respectively.
Comparison of Hormonal- and Sexual-Related QOL Between Neoadjuvant HT and Non-Neoadjuvant HT Groups
Hormonal summary scores at 6 and 9 months after RARP were significantly lower in the neoadjuvant HT group than in the non-neoadjuvant HT group (p = 0.002 and 0.017, respectively) (Figure 2). Hormonal function scores before and at 3, 6, and 9 months after RARP were significantly lower in the neoadjuvant HT group than in the non-neoadjuvant HT group (p = 0.005, 0.031, 0.0009, and 0.008, respectively). Similarly, hormonal bother score at 6 months after RARP was significantly lower in the neoadjuvant HT group than in the non-neoadjuvant HT group (p = 0.025).
Sexual function scores were significantly lower in the neoadjuvant HT group than in the non-neoadjuvant HT group throughout the entire observation period. Significant differences in sexual function score between neoadjuvant HT and non-neoadjuvant HT groups were seen before and at 6 months after RARP (p = 0.027 and 0.021, respectively). No significant difference in sexual summary or bother scores were seen between neoadjuvant HT and non-neoadjuvant HT groups during the observational period. We examined hormonal summary, hormonal function, hormonal bother, and sexual function scores, as those scores had shown statistical differences between non-neoadjuvant HT and neoadjuvant HT groups (Figure 2).
Effects of Neoadjuvant HT Duration and Hormonal Agent Type on QOL
Median duration of neoadjuvant HT was 5 months. Associations between neoadjuvant HT duration and QOL scores in patients who received neoadjuvant HT are shown in Figure 3. Scores for hormonal summary, function and bother did not differ significantly between groups. Sexual function at 3 months were significantly worse in patients with > 5-month neoadjuvant HT than in those with ≤ 5-month neoadjuvant HT (p = 0.047).
The number of patients treated by anti-androgen monotherapy, LHRH agonists monotherapy, and CAB were 14, 24, and 24, respectively. Median durations of neoadjuvant HT were 5.5 months (range, 0.5–24 months), 3 months (1–12 months), and 5.5 months (range, 1–10 months), respectively. Associations between hormonal agent types and QOL scores in patients who received neoadjuvant HT are shown in Figure 4. No significant differences in hormonal or sexual function scores were seen between patients treated with anti-androgen monotherapy (n = 14) and those who received LHRH agonists with/without anti-androgen drugs (n = 48).
Discussion
We assessed the impacts of neoadjuvant HT on postoperative hormonal- and sexual-related QOL in patients who underwent RARP. We demonstrated that neoadjuvant HT could affect hormonal- and sexual-related QOL after RARP. Furthermore, sexual function and bother in those patients who received neoadjuvant HT could be affected by the duration of neoadjuvant HT prior to RARP.
The distribution of clinical T stage and biopsy GG differed significantly between groups. On this point, PCa before treatment has not been confirmed as a risk factor for sexual dysfunction.20 Clinical T stage and biopsy GG that show significant differences in distributions between groups thus would not influence postoperative sexual-related QOL.
The first possible cause of declines in hormonal- and sexual-related QOL is a low serum concentration of testosterone. A previous study reported that serum testosterone concentration after cessation of LHRH agonist therapy did not always recover to baseline levels.21 Furthermore, prolonged castration levels of testosterone have been more likely to be observed in elderly patients, even after completion of hormonal therapy.22 Low serum testosterone levels have been associated with mood changes and depression.23,24 In addition, some studies revealed that hot flashes might be related to low testosterone concentration, even though no precise pathogenesis has been elucidated.12,25 With respect to sexual QOL issues, erectile dysfunction and decreased libido in PCa patients treated with hormonal therapy are directly related to low serum testosterone levels.12,26,27 These results indicate that the decreases in serum testosterone caused by neoadjuvant HT might induce declines in hormonal- and sexual-related QOL, which would continue for at least 12 months after RARP.
Another possible cause of declines in hormonal- and sexual-related QOL by neoadjuvant HT is low androgenic activity. Of the 62 patients in the neoadjuvant HT group, 14 received monotherapy with an anti-androgen drug. Anti-androgen drugs allow the maintenance of serum testosterone concentration since they bind to their receptors, blocking negative feedback of testosterone actions at the hypothalamus and pituitary gland. Nonetheless, monotherapy with anti-androgen drugs is known to result in AEs like gynecomastia and erectile dysfunction.11,28,29 Based on those previous studies, low levels of serum testosterone and/or androgenic activities caused by neoadjuvant HT might have affected hormonal- and sexual-related QOL after RARP in our cohort.
This study demonstrated that sexual function in patients receiving neoadjuvant HT for > 5 months at 3 months after RARP was worse than that in patients who received neoadjuvant HT for ≤ 5 months. Serum testosterone concentration theoretically plays a key role in sexual responses like penile erection and libido. Serum testosterone concentration decreases with hormonal therapy, causing erectile dysfunction and reduced libido.12 However, hormonal therapy-induced decreases in serum testosterone concentration are generally reported to recover with time after the completion of hormonal therapy, although this depends on the duration of hormonal therapy. The longer the duration of hormone administration, the longer serum testosterone take to recover.30 Previous studies support the notion that significant differences in sexual function at 6, 9, and 12 months after RARP are derived from the recovery of serum testosterone in both ≤ 5-month and > 5-month neoadjuvant HT groups. On the other hand, no difference in sexual function score was observed at 1 month after RARP. This cause could be attributed to the characteristics of the EPIC questionnaire, which includes questions about the frequency of sexual activities over the past 4 weeks. In other words, in our study, surveys at 1 month after RARP still reflected perioperative conditions. This may be why sexual function scores at 1 month after RARP did not differ significantly between groups with ≤ 5 months and > 5 months of neoadjuvant HT, aside from testosterone concentration.
Our study showed that hormonal-related QOL did not differ significantly according to the kinds of hormonal drugs. LHRH agonists are well known to induce a flare-up phenomenon and hot flashes.19 On the other hand, anti-androgen drugs directly inhibit androgen activity in breast tissues and indirectly increase estrogen concentrations, causing breast pain and gynecomastia.31 These hormone-related AEs caused by both LHRH agonists and anti-androgen agents are known to be associated with decreased QOL.10,11 This is probably why no significant difference was observed in hormonal-related EPIC scores due to differences in drugs. As for sexual-related QOL, sexual dysfunction induced by anti-androgen monotherapy is generally less severe than that associated with medical castration.11 However, our study found no difference in sexual function scores based on evaluation by hormonal agent types. Anatomical structures related to sexual function are generally damaged by RP, resulting in protracted sexual dysfunction regardless of the type of hormonal agent.32,33 In recent years, the application of various neoadjuvant regimens before RP based on new anti-androgen drugs such as apalutamide have been under investigation. Although the mechanisms of action of these new drugs differ from those of vintage anti-androgens, our results indicate the potential impact of neoadjuvant HT with new hormonal drugs on hormonal- and sexual-related QOL after RARP.34
Few studies appear to have addressed the impact of neoadjuvant HT prior to RARP on postoperative QOL.35 Another strength of this investigation was the higher collection rates of patient-reported questionnaires compared with a previous study.35 Our findings provide information that should help patients and clinicians in decision-making and subsequent treatment. Several limitations to this study need to be considered. First, QOL was not evaluated before neoadjuvant HT. Postoperative QOL is known to be affected by pretreatment QOL.36,37 Therefore, QOL needs to be assessed before neoadjuvant HT. In our study, patients in the neoadjuvant HT group had already been given hormonal drugs as part of radiohormonal therapy or based on the judgment of previous urologists. This is why no data were available to evaluate QOL before hormonal therapy. Second, serum testosterone concentration was not measured, because this was a questionnaire-based study. Third, the duration of follow-up was relatively short. A study with longer follow-up is desired to elucidate the effects of neoadjuvant HT on postoperative QOL.
Conclusion
Neoadjuvant HT prior to RARP would affect postoperative hormonal- and sexual-related QOL. Neoadjuvant HT duration also has impacts on sexual QOL. We believe that neoadjuvant HT prior to RARP should not be recommended from the perspective of not only oncological outcomes, but also the effects on postoperative hormonal- and sexual-related QOL.
Acknowledgments
The authors wish to thank Yusuke Kirihana, Hiroki Natsuya, Shunsuke Yoshioka, Tomoyuki Kumekawa, Yusuke Hakozaki, Kei Yaginuma, Yuki Harigane, Yu Endo, Yuki Harigane, Hitomi Imai, Yuta Matsuoka, Satoru Meguro, Ryo Tanji, Ruriko Honda-Takinami, and Seiji Hoshi for data entry work. The abstract of this paper was presented at the American Urological Association 2021 annual meeting as a poster presentation (Las Vegas, September 11, 2021). The poster abstract was published in “Poster Abstracts” in the Journal of Urology (https://www.auajournals.org/doi/10.1097/JU.0000000000002024.01). However, the full contents of this paper have not been published previously.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Moris L, Cumberbatch MG, Van den Broeck T, et al. Benefits and Risks of Primary Treatments for High-risk Localized and Locally Advanced Prostate Cancer: an International Multidisciplinary Systematic Review. Eur Urol. 2020;77(5):614–627. doi:10.1016/j.eururo.2020.01.033
2. van Poppel H, Everaerts W, Tosco L, Joniau S. Open and robotic radical prostatectomy. Asian J Urol. 2019;6(2):125–128. doi:10.1016/j.ajur.2018.12.002
3. Kumar S, Shelley M, Harrison C, Coles B, Wilt TJ, Mason MD. Neo-adjuvant and adjuvant hormone therapy for localised and locally advanced prostate cancer. Cochrane Database Syst Rev. 2006;2006(4):Cd006019.
4. Mohler JL, Antonarakis ES. NCCN Guidelines Updates: management of Prostate Cancer. J Natl Compr Canc Netw. 2019;17(5.5):583–586. doi:10.6004/jnccn.2019.5011
5. Sanda MG, Cadeddu JA, Kirkby E, et al. Clinically Localized Prostate Cancer: AUA/ASTRO/SUO Guideline. Part II: recommended Approaches and Details of Specific Care Options. J Urol. 2018;199(4):990–997. doi:10.1016/j.juro.2018.01.002
6. Meyer F, Bairati I, Bédard C, Lacombe L, Têtu B, Fradet Y. Duration of neoadjuvant androgen deprivation therapy before radical prostatectomy and disease-free survival in men with prostate cancer. Urology. 2001;58(2 Suppl 1):71–77. doi:10.1016/S0090-4295(01)01245-6
7. McClintock TR, von Landenberg N, Cole AP, et al. Neoadjuvant Androgen Deprivation Therapy Prior to Radical Prostatectomy: recent Trends in Utilization and Association with Postoperative Surgical Margin Status. Ann Surg Oncol. 2019;26(1):297–305. doi:10.1245/s10434-018-7035-z
8. Hu JC, Hung SC, Ou YC. Assessments of Neoadjuvant Hormone Therapy Followed by Robotic-Assisted Radical Prostatectomy for Intermediate- and High-Risk Prostate Cancer. Anticancer Res. 2017;37(6):3143–3150. doi:10.21873/anticanres.11672
9. Nguyen PL, Alibhai SM, Basaria S, et al. Adverse effects of androgen deprivation therapy and strategies to mitigate them. Eur Urol. 2015;67(5):825–836. doi:10.1016/j.eururo.2014.07.010
10. Downing A, Wright P, Hounsome L, et al. Quality of life in men living with advanced and localised prostate cancer in the UK: a population-based study. Lancet Oncol. 2019;20(3):436–447. doi:10.1016/S1470-2045(18)30780-0
11. Sharifi N, Gulley JL, Dahut WL. Androgen deprivation therapy for prostate cancer. JAMA. 2005;294(2):238–244. doi:10.1001/jama.294.2.238
12. Higano C. Androgen deprivation therapy: monitoring and managing the complications. Hematol Oncol Clin North Am. 2006;20(4):909–923. doi:10.1016/j.hoc.2006.03.013
13. D’Amico AV, Whittington R, Malkowicz SB, et al. Biochemical outcome after radical prostatectomy, external beam radiation therapy, or interstitial radiation therapy for clinically localized prostate cancer. JAMA. 1998;280(11):969–974. doi:10.1001/jama.280.11.969
14. Potdevin L, Ercolani M, Jeong J, Kim IY. Functional and oncologic outcomes comparing interfascial and intrafascial nerve sparing in robot-assisted laparoscopic radical prostatectomies. J Endourol. 2009;23(9):1479–1484. doi:10.1089/end.2009.0369
15. Egevad L, Delahunt B, Srigley JR, Samaratunga H. International Society of Urological Pathology (ISUP) grading of prostate cancer - An ISUP consensus on contemporary grading. Apmis. 2016;124(6):433–435. doi:10.1111/apm.12533
16. Takegami M, Suzukamo Y, Sanda MG, et al. [The Japanese translation and cultural adaptation of Expanded Prostate Cancer Index Composite (EPIC)]. Nihon Hinyokika Gakkai Zasshi. 2005;96(7):657–669. Japanese. doi:10.5980/jpnjurol1989.96.657
17. Ueno S, Kitagawa Y, Onozawa M, et al. Background factors and short-term health-related quality of life in patients who initially underwent radical prostatectomy or androgen deprivation therapy for localized prostate cancer in a Japanese prospective observational study (J-CaP Innovative Study-1). Prostate Int. 2018;6(1):7–11. doi:10.1016/j.prnil.2017.05.004
18. Koga H, Naito S, Ishiyama H, et al. Patient-reported health-related quality of life up to three years after the treatment with permanent brachytherapy: outcome of the large-scale, prospective longitudinal study in Japanese-Prostate Cancer Outcome Study by Permanent I-125 Seed Implantation (J-POPS). Brachytherapy. 2019;18(6):806–813. doi:10.1016/j.brachy.2019.06.006
19. Sountoulides P, Rountos T. Adverse effects of androgen deprivation therapy for prostate cancer: prevention and management. ISRN Urol. 2013;2013:240108. doi:10.1155/2013/240108
20. Lewis RW, Fugl-Meyer KS, Bosch R, et al. Epidemiology/risk factors of sexual dysfunction. J Sex Med. 2004;1(1):35–39. doi:10.1111/j.1743-6109.2004.10106.x
21. Murthy V, Norman AR, Shahidi M, et al. Recovery of serum testosterone after neoadjuvant androgen deprivation therapy and radical radiotherapy in localized prostate cancer. BJU Int. 2006;97(3):476–479. doi:10.1111/j.1464-410X.2006.06013.x
22. Pickles T, Agranovich A, Berthelet E, et al. Testosterone recovery following prolonged adjuvant androgen ablation for prostate carcinoma. Cancer. 2002;94(2):362–367. doi:10.1002/cncr.10219
23. Almeida OP, Waterreus A, Spry N, Flicker L, Martins RN. One year follow-up study of the association between chemical castration, sex hormones, beta-amyloid, memory and depression in men. Psychoneuroendocrinology. 2004;29(8):1071–1081. doi:10.1016/j.psyneuen.2003.11.002
24. Mohile SG, Mustian K, Bylow K, Hall W, Dale W. Management of complications of androgen deprivation therapy in the older man. Crit Rev Oncol Hematol. 2009;70(3):235–255. doi:10.1016/j.critrevonc.2008.09.004
25. Spetz AC, Hammar M, Pettersson W, Varenhorst E. Hot flushes and prostate cancer: pathogenesis and treatment. BJU Int. 2002;90(4):
26. Dacal K, Sereika SM, Greenspan SL. Quality of life in prostate cancer patients taking androgen deprivation therapy. J Am Geriatr Soc. 2006;54(1):85–90. doi:10.1111/j.1532-5415.2005.00567.x
27. Casey RG, Corcoran NM, Goldenberg SL. Quality of life issues in men undergoing androgen deprivation therapy: a review. Asian J Androl. 2012;14(2):226–231. doi:10.1038/aja.2011.108
28. Di Lorenzo G, Perdonà S, De Placido S, et al. Gynecomastia and breast pain induced by adjuvant therapy with bicalutamide after radical prostatectomy in patients with prostate cancer: the role of tamoxifen and radiotherapy. J Urol. 2005;174(6):2197–2203. doi:10.1097/01.ju.0000181824.28382.5c
29. Schröder FH, Collette L, de Reijke TM, Whelan P. Prostate cancer treated by anti-androgens: is sexual function preserved? EORTC Genitourinary Group. European Organization for Research and Treatment of Cancer. Br J Cancer. 2000;82(2):283–290. doi:10.1054/bjoc.1999.0916
30. Nascimento B, Miranda EP, Jenkins LC, Benfante N, Schofield EA, Mulhall JP. Testosterone Recovery Profiles After Cessation of Androgen Deprivation Therapy for Prostate Cancer. J Sex Med. 2019;16(6):872–879. doi:10.1016/j.jsxm.2019.03.273
31. Di Lorenzo G, Autorino R, Perdonà S, De Placido S. Management of gynaecomastia in patients with prostate cancer: a systematic review. Lancet Oncol. 2005;6(12):972–979. doi:10.1016/S1470-2045(05)70464-2
32. Alivizatos G, Skolarikos A. Incontinence and erectile dysfunction following radical prostatectomy: a review. ScientificWorldJournal. 2005;5:747–758. doi:10.1100/tsw.2005.94
33. Namiki S, Kaiho Y, Mitsuzuka K, et al. Long-term quality of life after radical prostatectomy: 8-year longitudinal study in Japan. Int J Urol. 2014;21(12):1220–1226. doi:10.1111/iju.12586
34. Tafuri A, Cerruto MA, Antonelli A. Neoadjuvant Strategies Before Radical Prostatectomy for High Risk Prostate Cancer in the Era of New Hormonal Agents. Curr Drug Targets. 2021;22(1):68–76. doi:10.2174/1389450121666200621194409
35. Chen MC, Kilday PS, Elliott PA, et al. Neoadjuvant Leuprolide Therapy with Radical Prostatectomy: long-term Effects on Health-related Quality of Life. Eur Urol Focus. 2020;7(4):779–787. doi:10.1016/j.euf.2020.03.001
36. Kurimura Y, Haga N, Yanagida T, et al. The preoperative pad test as a predictor of urinary incontinence and quality of life after robot-assisted radical prostatectomy: a prospective, observational, clinical study. Int Urol Nephrol. 2020;52(1):67–76. doi:10.1007/s11255-019-02301-3
37. Namiki S, Ishidoya S, Nakagawa H, et al. The relationships between preoperative sexual desire and quality of life following radical prostatectomy: a 5-year follow-up study. J Sex Med. 2012;9(9):2448–2456. doi:10.1111/j.1743-6109.2012.02788.x
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.




