Back to Journals » Patient Preference and Adherence » Volume 16
Impacts of Medical Security Level on Treatment Outcomes of Drug-Resistant Tuberculosis: Evidence from Wuhan City, China
Authors Liu X, Lin KH , Li YH, Jiang JN, Zhong ZD, Xiong YB, Zhou J, Xiang L
Received 13 September 2022
Accepted for publication 9 December 2022
Published 20 December 2022 Volume 2022:16 Pages 3341—3355
DOI https://doi.org/10.2147/PPA.S389231
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Johnny Chen
Xiao Liu,1,* Kun-He Lin,1,* Yue-Hua Li,2 Jun-Nan Jiang,3 Zheng-Dong Zhong,1 Ying-Bei Xiong,1 Jin Zhou,1 Li Xiang1,4
1School of Medicine and Health Management, Huazhong University of Science and Technology, Wuhan, People’s Republic of China; 2Wuhan Center for Tuberculosis Control and Prevention, Wuhan Pulmonary Hospital, Wuhan, People’s Republic of China; 3School of Public Administration, Zhongnan University of Economics and Law, Wuhan, People’s Republic of China; 4HUST Base of National Institute of Healthcare Security, Huazhong University of Science and Technology, Wuhan, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Li Xiang, Huazhong University of Science and Technology, Wuhan, People’s Republic of China, Email [email protected]
Background: Drug-resistant tuberculosis (DR-TB) is an increasingly serious global issue. DR-TB has a lower success rate and more severe interruption of treatment than ordinary tuberculosis. Incomplete treatment not only reduces recovery rate in DR-TB patients but also increases the spread of DR-TB. Optimizing medical security policies for DR-TB can reduce the economic burden of patients and can thereby improve treatment success rate.
Methods: Patients with DR-TB who were registered in Wuhan Center for Tuberculosis Control and Prevention from January 2016 to December 2019 were selected as research subjects. General descriptive statistical analysis methods were used in analyzing patients’ treatment outcomes and medical security compensation rate. The binary logistic regression was used in analyzing the impacts of medical security level on treatment outcomes of DR-TB.
Results: A total of 409 DR-TB patients were included in the study, and the refusal rate was 12.47%. The treatment success rate was only 37.09% for patients who started treatment and had treatment outcomes. The total out-of-pocket expenses (OOPs) per capita for DR-TB patients were 13,005.61 Chinese yuan. The outpatient effective compensation ratio (ECR) of DR-TB patients was only 51.04%. The outpatient ECR of DR-TB with subsidies of public health projects (SPHPs) were nearly 80% higher than those without SPHP. high outpatient ECR helped optimize treatment outcomes (P < 0.001, OR = 1.038). The inpatient ECR had no effect on patients’ treatment outcomes (P = 0.158, OR = 0.986).
Conclusion: Many DR-TB patients did not receive complete treatment. The key breakthrough point in improving DR-TB treatment outcomes is to optimize the outpatient medical insurance compensation policy. Including the costs of DR-TB in expenses for severe diseases in outpatient care is recommended, and financial investment should be appropriately increased to ensure the high coverage ratio of subsidies for public health projects.
Keywords: drug-resistant tuberculosis, medical security, treatment outcomes
Background
Tuberculosis (TB) remains one of the leading causes of deaths from infectious diseases.1,2 Drug-resistant TB (DR-TB) is a type of TB resistant to anti-TB drugs. DR-TB is a stubborn disease and decreases the chance of successful treatment and survival. The epidemic of DR-TB remains a major public health threat in many countries and has been one of the main obstacles to the success of achieving 2030 targets set in the End TB Strategy.3,5 Controlling the epidemic of DR-TB plays a vital role in global TB control and public health.6,7 One-third of new TB cases and one-half of previously treated cases in China exhibited anti-TB drug resistance. TB drug resistance is serious and on the rise in China.8,9 The number of DR-TB patients in China accounts for 14% of the world’s total, ranking second only to India, and is one of the countries with the heaviest burden of DR-TB.10
Limited access with treatment remains the major barriers to TB control in many low- and middle-income countries.11 Treatment of DR-TB is complicated, expensive, and often unsuccessful, resulting in a low cure rate, high mortality rate, and low follow-up rate.12,14 The global loss rate of patients with DR-TB is as high as 15%.13 The outcomes of patients who have not receive DR-TB treatment and those who have been treated but have been lost to follow-up or have incomplete or failed treatment are critically important.5 Some studies suggested that the transmission of resistant strains within a population is already a major problem.4,15,16 Treatment noncompliance and interruption diminish the quality of life of people living with DR-TB and increase disease transmission.17 Reduce the rate of treatment interruption rate of DR-TB can prevent the development of the drug-resistant forms of TB and reduce the transmission of DR-TB.9
China’s DR-TB control faces the challenges, such as poor accessibility and quality.5,18,19 One national survey in China showed that 73% of patients with TB had interrupted or suspended treatment.20 The Global TB Report 2020 shows that the proportion of people started on DR-TB treatment in total of 146 countries and territories who successfully completed treatment was 57%, while China has a 54% success rate in treating DR-TB.10 A study showed that the success rate of first-time smear positive DR-TB patients in Wuhan was 55.0%.21 Most cases of multidrug-resistant and extensively drug-resistant TB resulted from primary transmission.9 Given the number of patients in China, a high rate of treatment interruption can have massive public health implications, increase the risk of morbidity and mortality in the poor, and increase costs associated with illness.20
Treatment outcomes of DR-TB are affected by many factors, such as health status, general demographic characteristics, and psychological and social support.3,5,22–24 However, some studies have indicated that financial factor is the most cited reason for interrupted or suspended treatment for TB.20,25–30 Medical treatment imposes a high economic burden to patients with TB.31–35 The median cost for DR-TB is almost six times that for drug-susceptible TB.3 Patients with DR-TB incur huge expenditure.25,36–38 Many patients have dropped out or discontinued treatment because of difficulties in affording care.
To fight DR-TB, globally five priority actions have been proposed, one of which is increasing political commitment to ensure necessary financing.5 DR-TB prevention and control have been the important components of the national TB control program in China.20 China has adopted many measures to improve DR-TB treatment success rate; for example, the central government has provided annual earmarked funding to cover the cost of X-ray examinations and sputum smear tests for TB.11 In addition, China’s ongoing health system reform toward universal healthcare coverage provides important opportunities to improve access to appropriate care to prevent, diagnose, and treat DR-TB and protect patients from financial hardship.18 Payments for DR-TB treatment in China are from the social basic medical insurance (BMI), critical illness insurance (CII), medical assistance (MA), and patients themselves.11 The Chinese government has two social BMI schemes: the Urban and Rural Residents Basic Medical Insurance (URRBMI) and Urban Employee Basic Medical Insurance (UEBMI).11 The UEBMI mainly protects the working or retired people, whereas the URRBMI mainly protects unemployed residents, farmer, or students. Some provinces and cities in China have added corresponding cost guarantee policies for DR-TB on the basis of national basic policies. Among them, Wuhan, a sub-provincial city in central China, has launched a special public health subsidy (SPHP) for MDR-TB outpatient expenses through government financial funds. Studies have shown that the proportion of all patients’ out-of-pocket expenses (OOPs) in China is 28.8%, which means that the effective compensation ratio (ECR) of medical security was close to 70%.11 But the proportion of most DR-TB patients’ OOPs were 40%, which means that the ECR of medical security was only 60%.39 Medical security level of DR-TB needs to be improved.
Although some studies have pointed out that material support combined with other social support interventions is feasible and effective in improving treatment success for patients with DR-TB.3 Some studies have suggested raising the level of medical security coverage to improve treatment success rate of DR-TB patients.3,18,40 Evidence of the direct relationship between the level of medical security compensation and treatment outcomes of DR-TB patients is lacking, especially in China. In the present study, the impact of medical security levels on patients’ treatment outcomes was investigated in patients with DR-TB in Wuhan, China and suggestions for improving and providing reference for the prevention and control of DR-TB in other cities in China and other countries were proposed.
Method
Study Design
We conducted a retrospective review study using data from the electronic clinical records of Wuhan Pulmonary Hospital. The analysis content of this study is mainly divided into three parts. The first is the analysis of the medical security level. Based on the dimension of universal health coverage proposed by WHO, this study analyzes the medical security level of DR-TB in Wuhan from three aspects: the population covered, the cost covered and the service covered. It includes the analysis of qualitative materials such as the coverage of people, threshold, compensation ratio, and payment limit of Wuhan medical security policy. It also includes the analysis of quantitative indicators commonly used internationally to reflect the level of medical security, such as inpatient ECR and outpatient ECR. The second is the analysis of patient treatment outcomes, including important indicators such as treatment refusal rate, treatment success rate and treatment interruption rate. The third is the analysis of the influence of medical security level on the treatment outcomes with the inpatient ECR and outpatient ECR as the independent variable and the treatment outcomes as the dependent variable. The specific research design is shown in Figure 1.
Study Site
We selected Wuhan City, Hubei Province, China as our study site. Hubei Province is located in the central region of China and is representative of China in economic level and demographic characteristics. We selected Wuhan for several reasons. First, Wuhan lies on the central of China. It is one of the subprovincial cities in China. with a population of 13.65 million. Wuhan has good TB detection and care performance, so many patients with DR-TB prefer to receive treatment in the city. To obtain more samples, this study selected Wuhan as the study city. Second, Wuhan has had a digitized Hospital Information System (HIS) and TB Information Management System (TBIMS). The accessibility and quality of historical data made our analysis feasible.
Data Collection
We collected qualitative data on the medical security policy of DR-TB in Wuhan through interviews from Wuhan Municipal Healthcare Security Administration, Wuhan Municipal Health Commission, Wuhan Center For Disease Control and Prevention, and Wuhan Pulmonary Hospital (Wuhan Center for Tuberculosis Control and Prevention). The content of qualitative data collection mainly includes policy documents and policy implementation. The main indicators include the coverage of people, threshold, compensation ratio, payment limit, etc.
We collected quantitative data of DR-TB from HIS and TBIMS of Wuhan Pulmonary Hospital (Wuhan Center for Tuberculosis Control and Prevention). We collected sociodemographic profile (such as age, gender, occupation, and marriage) and treatment outcomes of DR-TB from TBMIS. We collected treatment fees and compensation of DR-TB patients from HIS.
Inclusion Criteria
Wuhan City residents with DR-TB confirmed between January 2016 and December 2019 were enrolled in this study.
Exclusion Criteria
Patients who had confirmed DR-TB but were not Wuhan residents were not included in this study because they may have returned to their place of residence for treatment and were lost to follow-up.
Sample Size
As Wuhan Pulmonary Hospital is the only designated hospital for DR-TB in Wuhan, which was in charge of the diagnosis and treatment of all DR-TB patients who lived in Wuhan. This study exported the treatment outcomes, treatment costs and compensation information of all DR-TB patients in Wuhan through system of TBIMS and HIS of Wuhan Pulmonary Hospital, and conducted a census of all patients who met the inclusion criteria. A total of 664 DR-TB patients were registered in the Wuhan TBIMS from 2016 to 2019. But 409 DR-TB patients’ fulfilling the inclusion criteria were included in the final analysis. We analyzed demographic characteristics to these 409 patients.
TBIMS only included treatment outcomes and general demographic characteristics of DR-TB patients. Therefore, we linked the patient in TBIMS (409 cases) with the patients in HIS in order to acquire precise information on the expenditure relating to DR-TB treatment. We successfully matched 358 cases (hereinafter referred to as a “patients who started treatment”). We analyzed medical expenses coverage for these 385 patients who started treatment.
Of the 358 patients who started treatment, 48 DR-TB patients have not yet finished treatment and therefore have no treatment outcomes. Therefore, the 48 patients who had not finished treatment were excluded from the treatment outcome analysis, and only the remaining 310 patients with treatment outcomes were analyzed.
This study pays more attention to the interruption of treatment due to inadequate medical security, so 118 patients who death or treatment failed will excluded from the analysis of the impact of medical security level on treatment outcomes. Only 192 patients with successful treatment and those who were lost to follow-up were included in the analysis.
The specific sample screening process is shown in Figure 2.
Definition of Key Indicators
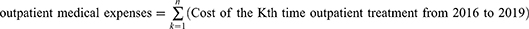
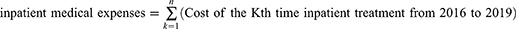
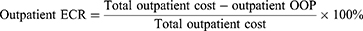
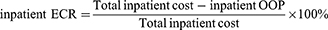
Definitions of Medical Expenses
The medical expenses of a DR-TB patient refers to the patient’s all the medical expenses incurred in the treatment of DR-TB in Wuhan Pulmonary Hospital from 2016 to 2019. The outpatient medical expenses of a DR-TB patient refers to the patient’s all the medical expenses incurred in the outpatient treatment of DR-TB in Wuhan Pulmonary Hospital from 2016 to 2019. The inpatient medical expenses of a DR-TB patient refers to the patient’s all the medical expenses incurred in the inpatient treatment of DR-TB in Wuhan Pulmonary Hospital from 2016 to 2019.
Definitions of Medical Security Level
We identified medical security by a commonly used framework introduced by the China Medical Security Administration. The framework includes BMI, CII, MA, and other special government subsidies. The index we selected to measure the level of medical security is the internationally commonly used ECR of medical security, including outpatient ECR and inpatient ECR. ECR of medical security refers to the actual reimbursement of all medicare expenses as a percentage of a patient’s total medical expenses.
Definitions of Treatment Outcomes
According to the WHO guidelines and relevant literature,3,5,41 the treatment outcomes indicators in this study included treatment success, lost to follow-up, treatment refusal, and others. Treatment success included treatment completed and cure. Lost to follow-up indicates that treatment is interrupted for two consecutive months or more. Treatment-refusal refers to patients diagnosed with DR-TB who refuse to receive treatment. Others include “treatment failed” and “died”. Treatment success and lost to follow-up were most frequently reported invoked as indicators of treatment outcomes.3 Therefore, the treatment outcome in the dependent variable of binary logistic regression in this study only included treatment success and lost to follow-up.
Data Analysis
Data were analyzed using SPSS 24.0, and statistical significance was set at p <0.05. Numbers and percentages were used in describing the characteristics of the study subjects. Chi-square test and T test were used in identifying differences in social demographics between patients with DR-TB that started treatment and those who refused treatment. ANOVA was used in analyzing differences in the cost of DR-TB treatment and compensation between patients with DR-TB and different types of BMI. T test was used in identifying differences in the cost of DR-TB treatment and compensation between patients with DR-TB with and without SPHP.
Univariate binary logistic regression was used in screening factors associated with DR-TB treatment outcomes. Significant factors based on the univariate binary logistic (p < 0.05) were used for adjustment in multivariate analysis. To prevent the collinearity between the outpatient effective compensation ratio (ECR) and inpatient ECR, we constructed three models. In model 1, the dependent variable was treatment outcomes, the key explanatory variable was inpatient ECR, and the control variables were significant factors based on univariate binary logistic. In model 2, the dependent variable was also treatment outcomes, the key explanatory variable was outpatient ECR, and the control variables were the same as model 1. In model 3, the dependent variable was treatment outcomes, the key explanatory variable was inpatient ECR and outpatient ECR, and the control variables were the same as model 1.
Results
Policy and Implementation Status
BMI
In Wuhan, in contrast to the URRBMI, the UEBMI has not established a financing scheme for general outpatient care. The general outpatient compensation rate of the URRBMI is 50%. The reimbursement cap line of outpatient care in the URRBMI was set at 400 Chinese yuan (CNY) for total visits in a year. Wuhan had not yet included DR-TB in the scope of compensation for severe diseases in outpatient care.
Inpatient medical expenses for DR-TB in Wuhan have been implemented in accordance with the inpatient compensation policies of different types of medical insurance, and no preferential policy has been formulated. Within an insurance year, medical expenses within the scope of the medical insurance compensation of insured persons exceeding the threshold of the CII are reimbursed proportionally by the CII (Table 1).
 |
Table 1 Inpatient Compensation Policy of BMI in Wuhan |
MA
Diseases covered by the compensation of outpatient severe diseases can apply for MA for outpatient expenses. However, DR-TB has not been included in outpatient intensive management, so they only enjoy inpatient MA. The inpatient compliant OOP medical costs after reimbursement by BMI and CII is in accordance with the following standards:
- The compensation ratio of MA for key assistance objects and targeted poverty alleviation objects with archived cards is 70%, and the annual assistance cap line is 26,000 CNY.
- The compensation ratio of MA for low-income persons experiencing difficulties is 60%, and the annual assistance ceiling is 10,000 CNY.
- When the OOP medical costs of poverty-stricken objects and other difficult objects identified by the district people’s government reach 1.5 times the per capita disposable incomes of urban and rural residents in the previous year released by the statistics department, assistance is provided to the part exceeding 1.5 times according to the proportion of 50%. The annual rescue cap is 10,000 CNY.
SPHP
An SPHP is a subsidy program for the outpatient treatment of multidrug resistance and was started by Wuhan in 2016 through the government’s special public health funds. The scheme only compensated patients with MDR-TB and has not yet included patients with other types of DR-TB because of limited financial health funds. SPHPs do not compensate for inpatient expenses and for treatment complications, comorbidities, and other adjuvant drugs. The rescue cap of an SPHP is 50,000 CNY.
Basic Information of Patients
A total of 409 patients with DR-TB included 358 patients (87.53%) who had started treatment, and the refusal rate was 12.47%. The mean age of the patients was 50.83 years, and 72.37% of them were males. The proportion of unemployed patients was the highest (75.31%). The marital status of patients was mainly married, accounting for 61.86%. Among the types of BMI, 36.92% of patients had UEBMI, 57.21% had URRBMI, and 5.87% had no BMI. Approximately 39.12% of patients with DR-TB received SPHP, and 60.88% did not receive SPHP. Differences in the distribution of marital status, BMI type, and SPHP were found between patients who started treatment and those who refused treatment (Table 2).
 |
Table 2 Demographic Characteristics of DR-TB Patients (N=409) |
Medical Expenses Coverage
Policy Benefit Rate of Patients with DR-TB
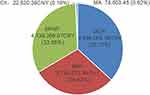
A total of 358 patients with DR-TB started treatment, of which 334 were reimbursed by BMI (the benefit rate was only 93.30%) and 160 were compensated by an SPHP (the benefit rate was 44.69%; Table 3). Only three patients used CII (0.84%), and 13 patients received MA (3.63%). Among the total financing sources of DR-TB, the highest was OOP (36.73%), followed by SPHP (32.65%), and BMI (29.82%). CII and MA accounted for less than 1% (Figure 3).
 |
Table 3 Policy Benefit Rate of DR-TB Patients Who Started Treatment (N=358) |
Medical Expenses and Compensation Rate
The total inpatient cost per capita of patients with DR-TB was 18,486.09 CNY. The total outpatient costs per capita were 16,927.25 CNY. The total medical expense per capita was 35,413.34 CNY. The total OOP expense per capita was 13,005.61 CNY. The inpatient ECR per capita of patients with DR-TB were 53.11%. The outpatient ECR per capita of DR-TB patients were 51.04%. In Table 4, it showed that type of BMI can affect the level of inpatient fees and compensation. In Table 5, it showed that whether there was SPHP can affect the level of inpatient fees and compensation.
 |
Table 4 Inpatient Expenses and the Effective Compensation Rate of DR-TB Patients (N=358) |
 |
Table 5 Outpatient Expenses and the Effective Compensation Rate of DR-TB Patients (N=358) |
Treatment Outcomes
Basic Information of Treatment Outcomes
A total of 358 patients with DR-TB started treatment, and 48 patients have not finished treatment yet. Only another 310 patients have treatment outcomes; 115 patients of them (37.09%) met the requirements for “treatment success”, and 77 patients (24.84%) were lost to follow-up. In the group without BMI, only two patients (9.52%) met the requirements for “treatment success.” In the group without an SPHP, only 21 patients (12.07%) met the requirements for “treatment success” (Figure 4).
Impact of Medical Security Level on the Treatment Outcomes of Patients with DR-TB
Treatment failure and death were patients who had to discontinue treatment due to disease factors. However, this study focused on the impact of medical security level on treatment success or interruption (lost to follow-up). So only patients with successful treatment and those who were lost to follow-up were included in the analysis. The treatment outcomes were used as the dependent variable, with a value of 0 for loss to follow-up and 1 for treatment success.
Univariate binary logistic regression was used in analyzing factors associated with treatment outcomes (Table 6). Univariate analysis showed that the relationship between inpatient ECR and treatment outcomes was not statistically significant (P = 0.934, OR = 1.000). Univariate analysis showed treatment outcomes optimized with increasing outpatient ECR of DR-TB (P < 0.001, OR = 1.034). Except marriage, other general demographic characteristics were significant in univariate analysis.
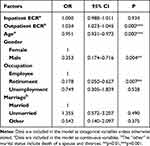 |
Table 6 Univariate Binary Logistic Regression Results of Factors Influencing on Treatment Outcomes of DR-TB. (N=192) |
Significant factors based on univariate binary logistic (age, gender, and occupation) were used for adjustment in multivariate analysis (Table 7). Model 1 only considered inpatient ECR. After controlling for demographic factors, our findings showed that the relationship between inpatient ECR and treatment outcomes was not statistically significant (P = 0.934, OR = 1.000). Model 2 only considered outpatient ECR. After controlling for demographic factors, treatment outcomes optimized with increasing outpatient ECR of DR-TB (P < 0.001, OR = 1.034). Model 3 considered inpatient ECR and outpatient ECR, and the results still showed that not only a statistically significant association between outpatient ECR and treatment outcomes was found (P < 0.001, OR = 1.038) but also statistically significant association between inpatient ECR and treatment outcomes was not found (P = 0.158, OR = 0.986).
 |
Table 7 Binary Logistic Regression Results of Effective Compensation Rate on Treatment Outcomes of DR-TB. (N=192) |
Discussion
Treatment Outcomes for DR-TB Still Need to Be Optimized
The proportion of patients with DR-TB in Wuhan who started treatment was 87.53%, which was higher than that of the global MDR/RR-TB in 2019 (86.0%).10 The possible reason is that Wuhan is the central city of the provincial capital, and thus the result may be lower in other third-tier cities. The proportion of lost patients in Wuhan accounted for 24.84%, which was at a high level compared with other research results (17%, 19.2%).13,42 The population base of patients with DR-TB in China is relatively large, and thus many patients who have refused treatment and have been lost to follow-up have been recorded. DR-TB patients who do not receive appropriate treatment may suffer from more dangerous forms of drug resistance and increased risk of relapse and death.42,43 In addition, patients with DR-TB can infect other residents through air transmission. Studies have found that more than half of DR-TB cases are caused by primary transmission.5 That is, patients with DR-TB do not receive standardized and systematic treatment, and thus not only their health is not guaranteed but also they pose a serious threat to the health of healthy people. Therefore, the success rate of treatment for patients with DR-TB should be improved. The social benefits of this approach far outweigh personal benefits, and the approach has a strong positive externality, which is beneficial to disease control and global health.
Improving the Outpatient ECR of Medical Security Can Optimize Treatment Outcomes for DR-TB
DR-TB treatment outcomes affect demographic factors such as age,22 which is consistent with some of the influencing factors in the present study. In addition, we found that the higher the outpatient ECR in DR-TB patients the more likely the treatment outcome was to be successful. It is suggested that the lack of outpatient compensation may lead to the increase of the rate of treatment loss of follow-up, which may help explain findings in previous studies that showed a marked increase in patient loss after outpatient treatment was initiated.42 According to a theory about the demand of health service, medical security can change the health service consumption behavior of patients by changing health service price, thereby changing the demand and utilization of a health service. Therefore, the perceived price of patients with DR-TB decreases with the increasing level of outpatient compensation, so the demand increases and the rate of treatment interruption decreases.
The inpatient ECR has no effect on treatment outcomes, and the main reason may be that the price elasticity of hospitalized demand is small.44 The hospitalization of patients with DR-TB is mostly urgent, and services, such as surgery, are necessary. Even if patients perceive a price to be high, they still need to receive inpatient treatment. Thus, the price elasticity of hospitalized demand is small. However, outpatient treatment is mostly follow-up intensive treatment involving drug treatment and examinations, and the price elasticity of demand is relatively large. Hence, outpatient demand is more affected by price changes, and outpatient service utilization is affected by the level of compensation. Compared with the impact of medical security compensation level on treatment outcomes mentioned in previous studies, this study focused on the impact of outpatient compensation level on treatment outcomes. It suggests that the main medical security policy optimization for DR-TB should focus on the compensation of outpatient.
General demographic characteristics, such as gender and age, are the inherent characteristics of patients and cannot be changed by policy intervention for optimizing treatment outcomes. Through medical insurance policy intervention, patient outcomes can be changed by changing outpatient ECR. In summary, this study showed that the key breakthrough point in improving DR-TB treatment outcomes is to optimize the outpatient medical insurance compensation policy.
Insufficient ECR of Outpatient Medical Security for DR-TB is Harmful to the Standardized Treatment of Patients
The total outpatient cost of DR-TB per capita is 16,927.25 CNY. The outpatient ECR of patients with DR-TB is only 51.04%. Outpatient ECR without an SPHP is only 2.23%. The level of outpatient compensation for DR-TB is insufficient, consistent with other studies.34 High outpatient treatment cost and low outpatient compensation level lead to high OOP cost for patients receiving outpatient care. In addition, patients still need to pay part of their OOP costs for hospitalization. The total OOP cost per capita for patients with DR-TB is as high as 13,005.61 CNY. DR-TB imposes a heavy economic burden. The proportion of patients with DR-TB is as high as 75.31%. Low income leads to poor financial affordability. Other studies have pointed out that high cost leads to the high likelihood of noncompliance.20 However, the ECR of outpatient in Wuhan is low and is thus harmful to the standardized treatment of patients.
The reasons for the insufficient level of outpatient compensation in Wuhan can be attributed to the multilevel medical security policy. The UEBMI in Wuhan has not yet established a financing scheme for general outpatient care. The reimbursement cap line of general outpatient care in URRBMI was set at 400 Chinese CNY for total visits in a year. The general outpatient compensation rate of BMI is extremely low to compensate the outpatient cost of DR-TB. Wuhan has not yet included DR-TB in the scope of compensation for severe diseases in outpatient care. This situation not only prevents patients from enjoying a high proportion of outpatient compensation but also prevents outpatient expenses for DR-TB from being included in CII and MA. The reason is that the scope of compensation for CII and MA is the outpatient expenses of severe diseases and inpatient expenses. However, the cost of DR-TB is mainly outpatient cost, and the number of patients whose inpatient costs meet the compensation requirements of CII and MA is low, so the benefit rate of patients is low. The results showed that the benefit rate of CII for DR-TB is only 0.84% and the rate of MA is only 3.63%. Therefore, the outpatient costs incurred by patients with DR-TB in Wuhan can only be guaranteed by SPHPs. The outpatient ECR of DR-TB with an SPHP are nearly 80% higher than that without an SPHP. Patients with SPHPs have an 11.77% lower rate of treatment loss than those without SPHPs. However, the benefit rate of SPHP is as low as 44.69% possibly because of the lack of financial subsidy funds. Therefore, the level of DR-TB outpatient compensation should be improved, and the costs of DR-TB should be included in the expenses of severe diseases in outpatient care. Some other regions in China have made this attempt, which provide a good experience.11 In addition, government financial input should be appropriately increased to ensure that the coverage rate of SPHP is high enough to help improve the level of DR-TB compensation.
Conclusion
By analyzing data in Wuhan, China, we found that many patients with DR-TB gave up treatment or interruption of treatment. Improving the outpatient ECR of DR-TB patients can effectively improve treatment success rate of DR-TB. While the inpatient ECR has no effect on treatment outcomes. So the key breakthrough point in improving DR-TB treatment outcomes is to optimize the outpatient medical security compensation policy. However, the outpatient ECR of DR-TB in Wuhan is low. The main reasons are as follows: first, Wuhan has not yet included DR-TB in the scope of compensation for severe diseases in outpatient care, and thus the benefit rates of CII and MA are low. Second, insufficient financial subsidies lead to a low proportion of people covered by SPHPs. Including the costs of DR-TB in the expenses of severe diseases in outpatient care is recommended. Moreover, financial investment in DR-TB treatment should be appropriately increased. This approach will improve the actual compensation level of DR-TB, improve the success rate of DR-TB treatment, and improve the efficiency of DR-TB control.
Abbreviations
TB, tuberculosis; DR-TB, drug-resistant tuberculosis; BMI, basic medical insurance; CII, critical illness insurance; MA, medical assistance; URRBMI, Urban and Rural Residents Basic Medical Insurance; UEBMI, Urban Employee Basic Medical Insurance; SPHP, subsidies of public health projects; HIS, Hospital Information System; TBIMS, TB Information Management System; OOP, out-of-pocket; ECR, effective compensation ratio; CNY, Chinese yuan; UECII, urban employee critical illness insurance; URRCII, urban and rural resident critical illness insurance.
Data Sharing Statement
All data generated or analysed during this study were kept confidential by WuHan Tuberculosis Hospital in HuBei Province, China. The datasets are available from the corresponding author on reasonable request.
Ethics Approval and Consent to Participate
The ethical approval for data collection came from the biomedical ethics review committee of Huazhong University of science and Technology (S170. June 30, 2021). The writer and research team confirm that this research caused no harm (physical or mental) to any participants. The research process complies with the Declaration of Helsinki. The investigation was conducted after written informed consent was obtained from all participants.
Funding
This study was supported by the National Natural Science Foundation of China, Grant No. 71874058.
Disclosure
The authors declare that they have no competing interests.
References
1. Li BY, Shi WP, Zhou CM., et al. Rising challenge of multidrug-resistant tuberculosis in China: a predictive study using Markov modeling. Infect Dis Poverty. 2020;9(1):65. doi:10.1186/s40249-020-00682-7
2. Herbert N, Sharma V, Masham BS, Sheehan BS, Hauser J, Zumla A. Concrete action now: UN High-Level Meeting on Tuberculosis. Lancet Infect Dis. 2018;18(7):709–710. doi:10.1016/S1473-3099(18)30171-3
3. Wen S, Yin J, Sun Q. Impacts of social support on the treatment outcomes of drug-resistant tuberculosis: a systematic review and meta-analysis. BMJ Open. 2020;10(10):e036985. doi:10.1136/bmjopen-2020-036985
4. Lange C, Chesov D, Heyckendorf J, Leung CC, Udwadia Z, Dheda K. Drug-resistant tuberculosis: an update on disease burden, diagnosis and treatment. Respirology. 2018;23(7):656–673. doi:10.1111/resp.13304
5. Zheng XB, Diwan VK, Zhao Q, et al. Treatment quality and outcome for multidrug-resistant tuberculosis patients in four regions of China: a cohort study. Infect Dis Poverty. 2020;9(1):97. doi:10.1186/s40249-020-00719-x
6. Raviglione MC, Smith IM. XDR tuberculosis--implications for global public health. N Engl J Med. 2007;356(7):656–659. doi:10.1056/NEJMp068273
7. Morens DM, Fauci AS. Emerging infectious diseases: threats to human health and global stability. PLoS Pathog. 2013;9(7):e1003467. doi:10.1371/journal.ppat.1003467
8. Who W. Multidrug and extensively drug-resistant TB (M/XDR-TB): 2010 global report on surveillance and response[J]. Geneva Switzerland Who. 2010;35(6):2171–2178.
9. Zhao Y, Xu S, Wang L, et al. National survey of drug-resistant tuberculosis in China. N Engl J Med. 2012;366(23):2161–2170. doi:10.1056/NEJMoa1108789
10. WHO. Global Tuberculosis Report 2020. Geneva: World Health Organization; 2020. Available from:https://www.who.int/publications-detail-redirect/9789240013131.
11. Long Q, Jiang WX, Zhang H, Cheng J, Tang SL, Wang WB. Multi-source financing for tuberculosis treatment in China: key issues and challenges. Infect Dis Poverty. 2021;10(1):17. doi:10.1186/s40249-021-00809-4
12. Keshavjee S, Farmer PE. Picking up the pace--scale-up of MDR tuberculosis treatment programs. N Engl J Med. 2010;363(19):1781–1784. doi:10.1056/NEJMp1010023
13. Law S, Daftary A, O’Donnell M, Padayatchi N, Calzavara L, Menzies D. Interventions to improve retention-in-care and treatment adherence among patients with drug-resistant tuberculosis: a systematic review. Eur Respir J. 2019;53(1):1801030. doi:10.1183/13993003.01030-2018
14. Ahmad S, Mokaddas E. Current status and future trends in the diagnosis and treatment of drug-susceptible and multidrug-resistant tuberculosis. J Infect Public Health. 2014;7(2):75–91. doi:10.1016/j.jiph.2013.09.001
15. Fitzpatrick C, Floyd K. A systematic review of the cost and cost effectiveness of treatment for multidrug-resistant tuberculosis. Pharmacoeconomics. 2012;30(1):63–80. doi:10.2165/11595340-000000000-00000
16. Casali N, Nikolayevskyy V, Balabanova Y, et al. Evolution and transmission of drug-resistant tuberculosis in a Russian population. Nat Genet. 2014;46(3):279–286. doi:10.1038/ng.2878
17. Munro SA, Lewin SA, Smith HJ, Engel ME, Fretheim A, Volmink J. Patient adherence to tuberculosis treatment: a systematic review of qualitative research. PLoS Med. 2007;4(7):e238. doi:10.1371/journal.pmed.0040238
18. Long Q, Qu Y, Lucas H. Drug-resistant tuberculosis control in China: progress and challenges. Infect Dis Poverty. 2016;5:9. doi:10.1186/s40249-016-0103-3
19. Wang L, Liu J, Chin DP. Progress in tuberculosis control and the evolving public-health system in China. Lancet. 2007;369(9562):691–696. doi:10.1016/S0140-6736(07)60316-X
20. Long Q, Smith H, Zhang T, Tang S, Garner P. Patient medical costs for tuberculosis treatment and impact on adherence in China: a systematic review. BMC Public Health. 2011;11:393. doi:10.1186/1471-2458-11-393
21. Duan QH, Chen C, Zhang ZB, et al. Analysis on factors influencing the therapeutic outcome of the first-time retreated smear-positive pulmonary tuberculosis patients in Wuhan city. Chin J Antiuber. 2013;35(10):788–792.
22. Kamara RF, Saunders MJ, Sahr F, et al. Social and health factors associated with adverse treatment outcomes among people with multidrug-resistant tuberculosis in Sierra Leone: a national, retrospective cohort study. Lancet Glob Health. 2022;10(4):e543–e554. doi:10.1016/S2214-109X(22)00004-3
23. Abubakar I, Lipman M. Reducing loss to follow-up during treatment for drug-resistant tuberculosis. Eur Respir J. 2019;53(1):1802268. doi:10.1183/13993003.02268-2018
24. Nellums LB, Rustage K, Hargreaves S, Friedland JS. Multidrug-resistant tuberculosis treatment adherence in migrants: a systematic review and meta-analysis. BMC Med. 2018;16(1):27. doi:10.1186/s12916-017-1001-7
25. Ruan YZ, Li RZ, Wang XX, et al. The affordability for patients of a new universal MDR-TB coverage model in China. Int J Tuberc Lung Dis. 2016;20(5):638–644. doi:10.5588/ijtld.15.0413
26. Jiang WX, Long Q, Lucas H, et al. Impact of an innovative financing and payment model on tuberculosis patients’ financial burden: is tuberculosis care more affordable for the poor? Infect Dis Poverty. 2019;8(1):21. doi:10.1186/s40249-019-0532-x
27. Jianzhao H, van den Hof S, Lin X, Yubang Q, Jinglong H, van der Werf MJ. van der Werf MJ. Risk factors for non-cure among new sputum smear positive tuberculosis patients treated in tuberculosis dispensaries in Yunnan, China. BMC Health Serv Res. 2011;11(1):97. doi:10.1186/1472-6963-11-97
28. Xu W, Lu W, Zhou Y, Zhu L, Shen H, Wang J. Adherence to anti-tuberculosis treatment among pulmonary tuberculosis patients: a qualitative and quantitative study. BMC Health Serv Res. 2009;9(1):169. doi:10.1186/1472-6963-9-169
29. Pan HQ, Bele S, Feng Y, et al. Analysis of the economic burden of diagnosis and treatment of tuberculosis patients in rural China. Int J Tuberc Lung Dis. 2013;17(12):1575–1580. doi:10.5588/ijtld.13.0144
30. Xu B, Fochsen G, Xiu Y, Thorson A, Kemp JR, Jiang QW. Perceptions and experiences of health care seeking and access to TB care--a qualitative study in rural Jiangsu Province, China. Health Policy (New York). 2004;69(2):139–149. doi:10.1016/j.healthpol.2003.11.006
31. Chen S, Zhang H, Pan Y, et al. Are free anti-tuberculosis drugs enough? An empirical study from three cities in China. Infect Dis Poverty. 2015;4:47. doi:10.1186/s40249-015-0080-y
32. Xiang L, Pan Y, Hou S, et al. The impact of the new cooperative medical scheme on financial burden of tuberculosis patients: evidence from six counties in China. Infect Dis Poverty. 2016;5:8. doi:10.1186/s40249-015-0094-5
33. Wei X, Zou G, Yin J, et al. Effective reimbursement rates of the rural health insurance among uncomplicated tuberculosis patients in China. Trop Med Int Health. 2015;20(3):304–311. doi:10.1111/tmi.12438
34. Pan Y, Chen S, Chen M, et al. Disparity in reimbursement for tuberculosis care among different health insurance schemes: evidence from three counties in central China. Infect Dis Poverty. 2016;5:7. doi:10.1186/s40249-016-0102-4
35. Tang S, Wang L, Wang H, Chin DP. Access to and affordability of healthcare for TB patients in China: issues and challenges. Infect Dis Poverty. 2016;5:10. doi:10.1186/s40249-016-0096-y
36. Mullerpattan JB, Udwadia ZZ, Banka RA, Ganatra SR, Udwadia ZF. Catastrophic costs of treating drug resistant TB patients in a tertiary care hospital in India. Indian J Tuberc. 2019;66(1):87–91. doi:10.1016/j.ijtb.2018.04.011
37. Sun Q, Yan Y, Bian XF, et al. Medical expense and economic burden analysis of multi-drug resistance tuberculosis patients. Chin Health Econ. 2011;30(1):33–35.
38. Xu CH, Ma W, Zhang CY, et al. Analysis on the reimbursement of medical expenses for multidrug resistant tuberculosis under three health insurance systems. Chin Prev Med. 2014;15(7):633–636.
39. Chen Y, Zhao Y. Multidrug-resistant tuberculosis in rural China: lack of public awareness, unaffordable costs and poor clinical management. BMJ Case Rep. 2018;2018:bcr2018225794. doi:10.1136/bcr-2018-225794
40. Hu XY, Gao GY. Evaluation of the effect of the capitation compensation mechanism among pulmonary tuberculosis patients with a full period of treatment. Infect Dis Poverty. 2021;10(1):78. doi:10.1186/s40249-021-00861-0
41. Organization W H. Definitions and Reporting Framework for Tuberculosis—2013 Revision. Arch Otorhinolaryngol. 2013;246(4):183–189.
42. Shringarpure KS, Isaakidis P, Sagili KD, Baxi RK. Loss-To-Follow-Up on Multidrug Resistant Tuberculosis Treatment in Gujarat, India: the WHEN and WHO of It. PLoS One. 2015;10(7):e0132543. doi:10.1371/journal.pone.0132543
43. Velayati AA, Farnia P, Hoffner S. Drug-resistant Mycobacterium tuberculosis: epidemiology and role of morphological alterations. J Glob Antimicrob Resist. 2018;12:192–196. doi:10.1016/j.jgar.2017.10.006
44. Zheng X, Liu G, Ji M, et al. Elasticity of the demand for health care services in China: a systematic review. Chin J Evidence Based Med. 2017;17(5):564–572.
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.