Back to Journals » Clinical Interventions in Aging » Volume 11
Impact of whole body electromyostimulation on cardiometabolic risk factors in older women with sarcopenic obesity: the randomized controlled FORMOsA-sarcopenic obesity study
Authors Wittmann K, Sieber C, von Stengel S, Kohl M , Freiberger E, Jakob F, Lell M, Engelke K, Kemmler W
Received 4 July 2016
Accepted for publication 29 August 2016
Published 18 November 2016 Volume 2016:11 Pages 1697—1706
DOI https://doi.org/10.2147/CIA.S116430
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Richard Walker
Katharina Wittmann,1 Cornel Sieber,2 Simon von Stengel,1 Matthias Kohl,3 Ellen Freiberger,2 Franz Jakob,4 Michael Lell,5 Klaus Engelke,1 Wolfgang Kemmler1
1Institute of Medical Physics, Faculty of Medicine, Friedrich-Alexander University of Erlangen-Nürnberg, 2Institute for Biomedicine of Aging, Faculty of Medicine, Friedrich-Alexander University of Erlangen-Nürnberg, Erlangen, 3Faculty of Medical and Life Sciences, University of Furtwangen, 4Musculoskeletal Research Center, University of Würzburg, Würzburg, 5Department of Radiology and Nuclear Medicine, Klinikum Nürnberg, Paracelsus Medizinische Privatuniversität, Nürnberg, Germany
Background: Sarcopenic obesity (SO) is characterized by a combination of low muscle and high fat mass with an additive negative effect of both conditions on cardiometabolic risk. The aim of the study was to determine the effect of whole-body electromyostimulation (WB-EMS) on the metabolic syndrome (MetS) in community-dwelling women aged ≥70 years with SO.
Methods: The study was conducted in an ambulatory university setting. Seventy-five community-dwelling women aged ≥70 years with SO living in Northern Bavaria, Germany, were randomly allocated to either 6 months of WB-EMS application with (WB-EMS&P) or without (WB-EMS) dietary supplementation (150 kcal/day, 56% protein) or a non-training control group (CG). WB-EMS included one session of 20 min (85 Hz, 350 µs, 4 s of strain–4 s of rest) per week with moderate-to-high intensity. The primary study endpoint was the MetS Z-score with the components waist circumference (WC), mean arterial pressure (MAP), triglycerides, fasting plasma glucose, and high-density lipoprotein cholesterol (HDL-C); secondary study endpoints were changes in these determining variables.
Results: MetS Z-score decreased in both groups; however, changes compared with the CG were significant (P=0.001) in the WB-EMS&P group only. On analyzing the components of the MetS, significant positive effects for both WB-EMS groups (P≤0.038) were identified for MAP, while the WB-EMS group significantly differed for WC (P=0.036), and the WB-EMS&P group significantly differed for HDL-C (P=0.006) from the CG. No significant differences were observed between the WB-EMS groups.
Conclusion: The study clearly confirms the favorable effect of WB-EMS application on the MetS in community-dwelling women aged ≥70 years with SO. However, protein-enriched supplements did not increase effects of WB-EMS alone. In summary, we considered this novel technology an effective and safe method to prevent cardiometabolic risk factors and diseases in older women unable or unwilling to exercise conventionally.
Keywords: sarcopenia, obesity, whole-body electromyostimulation, cardiovascular, metabolic risk, metabolic syndrome, community-dwelling, older people
Introduction
Sarcopenic obesity (SO), the combination of low muscle and high fat mass,1 is reported to be a frequent condition among women aged ≥70 years. According to Batsis et al2 up to 94% of people aged ≥60 years can be classified as SO. SO is predominately caused by a decrease of physical activity (PA) in combination with stable caloric intake, malnutrition, and hormonal changes.3 Older people with SO demonstrated poor health, reduced functional capacity, and quality of life right up to loss of independence and institutionalization.1 Besides the problem of progressive loss of muscle mass, the adjuvant accumulation of (intra-) abdominal fat in summary induces a higher risk for cardiometabolic diseases.4–7 Regular exercise favorably affected most risk factors and diseases in old age.8 Resistance training may be an important factor not only to maintain muscle mass but also with respect to the prevention and therapy of metabolic risk factors and disorders.9 However, the majority of older people unfortunately do not fulfill the recommended exercise doses for positive impact on muscle mass, obesity, or other issues of cardiometabolic risk factors.10 For people who are unable or unwilling to exercise with the necessary amount and effort, whole-body electromyostimulation (WB-EMS) may be an option.11 In fact, WB-EMS is time-efficient and less debilitating, thus producing higher acceptance among nonathletes.12 Furthermore, WB-EMS has demonstrated positive effects on muscle and fat mass, and a gain of functional capacity in older sedentary people.13 However, even though there is some evidence that WB-EMS and WB-EMS-induced changes of body composition favorably decreased the metabolic syndrome (MetS) in older people,4,11 no study clearly addresses this issue. We consider this issue to be important for this cohort because the prevalence of the MetS is: a) increased among the elderly14 and b) subjects with SO are at a high risk for cardiometabolic diseases.15 Thus, the primary aim of this study was to determine the effect of WB-EMS on the MetS in women with SO. Additionally, we evaluate the effect of an adjuvant protein-rich diet in this cohort of older, inactive woman with low muscle and high fat mass.16
Our main hypothesis was that WB-EMS training significantly affected the MetS as defined by the National Cholesterol Education Program Adult Treatment Panel III (NCEP ATP III) criteria17 in community-dwelling women with SO aged ≥70 years compared with a non-training, non-supplemented control group (CG). As our secondary hypothesis, we expected that additional protein supplement significantly increases the effect of WB-EMS on the MetS compared with WB-EMS application without supplementation.
Methods
Trial design
The FORMOsA-Sarcopenic Obesity Study (SOS) was a unicenter, controlled, semi-blinded trial with a parallel group design and three study arms, balanced randomization and stratification for age. The study is part of the Sarcopenia and Osteoporosis (FORMOsA) project and was partially supported by the “Bavarian Research Foundation”. The study was conducted between September 2013 and January 2016 by the Institutes of Medical Physics and Biomedicine of Aging, University of Erlangen-Nürnberg (FAU), Germany. The University of Erlangen-Nürnberg Ethics Committee (Ethikantrag 301_13B) and the Federation Radiation Protection Agency (Bundesamt für Strahlenschutz, Z5-22462/2-2014-030) approved the study. After study start, no important changes in methods were made.
After detailed information, all study participants gave written informed consent. The FORMOsA-SOS trial was registered under www.ClinicalTrials.gov (NCT02356016). We strictly adhered to the CONSORT statement for the reporting of randomized controlled trials.
Participants
Sample size calculation refers to another primary study endpoint not presented here: appendicular skeletal muscle mass (ASMM) as the variable fraction of the skeletal muscle index (SMI: ASMM/[body height];2 measured in kg/m2). In order to detect a difference of 300 g (standard deviation [SD]: 375 g) in ASMM between the WB-EMS and control groups, 25 participants/group were necessary to generate 80% power and a two-sided significance level of 5%. The difference of 300 g is in agreement with recent results of a WB-EMS study in females aged ≥70 years.12
Recruitment
Overall, 7,900 randomly selected women, aged ≥70 years, living independently in the Erlangen-Nürnberg area were contacted by letter using citizen registration records provided by the municipality. This letter listed the key study eligibility criteria. Of the 1,401 women who replied, 1,325 were invited and further checked for eligibility based on the following inclusion criteria: a) sarcopenia (SMI <5.75 kg/m2)18 and b) obesity (>35% body fat).19 Exclusion criteria were: a) use of medication (eg, glucocorticoids, statins, active vitamin-D metabolites, anabolic steroids, and selective estrogen receptor modulators), injuries or diseases (eg, Cushing syndrome, and other endocrine, neuronal, and metabolic myopathies) affecting muscle mass or preventing WB-EMS application (eg, TotalEndoProthesis; cardiac arrhythmia, renal insufficiency, cancer, and epilepsy); b) trained status (ie, exercising >60 min/week); c) >4 weeks of absence during the interventional period; and d) alcohol abuse (ie, >40 g/d). Following our criteria, 101 community-dwelling women aged ≥70 years were eligible; 26 of the 101 eligible women declined to participate mainly due to the randomization process and the corresponding mandatory group allocation, but we nevertheless achieved our recruitment goal of 75 women (Figure 1). Recruitment and eligibility assessments were conducted between June and December 2014.
Randomization procedures
Stratified for age (strata of 5 years), 75 participants were randomly assigned to three study arms: a) WB-EMS; b) WB-EMS and protein supplementation (WB-EMS&P); and c) non-training CG by a uniform allocation rate (1:1:1) (Figure 1). For allocation, lots were drawn by the participants. Each of the 75 lots were put in opaque plastic shells (“kinder egg,” Ferrero, Italy) and drawn from a bowl so that participants and researchers never knew the allocation beforehand.
Blinding
Research assistants/outcome assessors were blinded with respect to the status of the participants, ie, they were not informed or allowed to ask about participant status (WB-EMS, WB-EMS&P, or CG).
Intervention
We set up three study groups. Two groups carried out 26 weeks of the WB-EMS protocol, while the non-training CG was requested to maintain their habitual life style. Our setting was an ambulatory university setting, so all WB-EMS participants exercised at the Institute of Medical Physics, which is centrally located and can be easily reached by public transport. All the sessions were supervised by certified trainers who also logged the participants’ attendance. The intervention was conducted between February and September 2015. Baseline characteristics of the three study groups are listed in Table 1.
  | Table 1 Baseline characteristics of the three study groups |
WB-EMS intervention
WB-EMS equipment (miha bodytec®, Gersthofen, Germany) enables the simultaneous activation of up to 14–18 regions or 8–12 muscle groups (both upper legs, both upper arms, bottom, abdomen, chest, lower back, upper back, latissimus dorsi, and four free options; up to 2.800 cm2 stimulated area) with selectable intensity for each region. The latter includes the possibility to select and modify current intensity during the WB-EMS session per individual and body region. In the present study, up to four participants simultaneously performed a video-guided WB-EMS program in a dorsal sitting/lying position (Figure 2) with slight movements of the lower and upper limbs once a week. Bipolar electric current was applied at a frequency of 85 Hz and an impulse width of 350 μs intermittently with 4 s of EMS-simulation using a direct impulse boost and 4 s of rest. Starting with 11 min of WB-EMS application, the length of the session was progressively increased to 20 min after 8 weeks; this duration was maintained for the rest of the training period. Due to body regions and individual disparities in current sensitivity, we were unable to prescribe the exact intensity (in mA). Thus, in order to generate a sufficient but tolerable intensity of the EMS application, participants were encouraged to exercise at a rate of perceived exertion (RPE) between 5 and 6 (ie, “hard” to “hard+”) on the Borg 10-point Category Ratio Scale.20 In order to achieve this goal, the (current) intensity was individually adapted for each body region with the participants’ agreement during the first session and after 6 and 12 weeks. The corresponding settings were saved for each muscle group/region in order to generate a fast, reliable, and valid setting in the subsequent sessions. From these initial settings, instructors slightly increased the (current) intensity every 3–5 min in close cooperation with the participants and thus maintained the prescribed RPE during the session.
  | Figure 2 WB-EMS application with slight movements in a supine sitting/lying position. |
Protein supplementation
The WB-EMS&P group was provided with nutritional supplement (FortiFit; Nutricia, Erlangen, Germany) with a high protein component. A standard portion of 40 g/day of the supplement represented a caloric value of 638 kJ and contained 56% (21 g) of whey protein with a high L-leucin component (2.8 g/portion), 10 g of carbohydrates (4.2 g sugar), 3 g of fat (including 0.8 g of saturated fatty acids), 1.3 g of fiber, and a mixture of vitamins and minerals. We aimed to generate a total daily protein intake of at least 1.2 g/kg body mass/day in each WB-EMS&P participant.
Nutritional counseling/vitamin D supplementation
Based on the baseline dietary records of the participant, a graduate nutritionist provided a 1-h group lecture and individual counseling for all participants of the WB-EMS&P group, with focus on the importance of protein intake. All participants were informed about the relevance of energy balance. Furthermore, all the women were provided with 800 IE/day of vitamin D (cholecalciferol). Compliance with the vitamin D and dietary supplements prescription was monitored by monthly phone calls.
Outcomes
Primary outcome parameter
- Change of the MetS Z-score conformable to the NCEP ATP III criteria of the MetS17 from baseline to 26-week follow-up.
Secondary outcome parameters
- Changes in variables determining the MetS from baseline to 26-week follow-up:
- Waist circumference (WC)
- Mean arterial pressure (MAP)
- Triglycerides (TGs)
- Fasting plasma glucose (FPG)
- High-density lipoprotein cholesterol (HDL-C).
Assessments
Baseline and 6-month follow-up tests were consistently performed by the same research assistant at the same time of day (±1 h).
Body height and WC were determined using calibrated devices. Body mass and composition were determined via dual-energy X-ray absorptiometry (QDR 4500a; Hologic, Bedford, MA, USA).
The MetS, as defined in the NCEP ATP III criteria,17 consists of five parameters: 1) increased WC (≥88 cm in women; ≥102 cm in men); 2) increased blood pressure (≥130 mmHg systolic or ≥85 mmHg diastolic); 3) increased TGs (≥150 mg/dL); 4) increased FPG (≥110 mg/dL); and 5) decreased HDL-C (≤50 mg/dL in women). For the present study, we used the MetS Z-score according to Johnson et al.21 The Z-score was calculated in the following way: ([50 – HDL-C]/SD – HDL-C) + ([TGs – 150]/SD – TGs) + ([FPG – 100]/SD – FPG) + ([WC – 88]/SD – WC) + ([MAP – 100]/SD – MAP). Negative Z-scores as well as negative Z-score changes can be considered as favorable.
After an overnight fast, blood was sampled in the morning in a sitting position from an antecubital vein. The serum samples were centrifuged at 3,000 RPM for 20 min and analyzed by the “Zentrallabor” of the Medical Department, University of Erlangen-Nürnberg. Glucose, HDL-C, and TGs (Olympus Diagnostica GmbH, Hamburg, Germany) were determined.
Blood pressure was determined in a lying position after 10 min of rest with an automatic oscillometric device (Bosco; Bosch, Jungingen, Germany). All measurements were taken in a non-fasting condition. Participants were asked to avoid relevant PA 12 h before the tests and to refrain from coffee or tea for at least 2 h prior to testing. MAP was derived from systolic and diastolic pressures, weighted 1/3 systolic and 2/3 diastolic.
Demographic parameters, pre-study PA and exercise levels, health risk factors, and quality of life parameters were sampled using the validated baseline questionnaires.22,23 Follow-up questionnaires asked for changes in medication, diseases, lifestyle, PA, exercise,24 dietary pattern, and nutritional supplementation, ie, parameters that may affect the study endpoints. Before and after the intervention phase, all participants kept a 3-day dietary record (two weekdays and one weekend day).25 From standard portions, all food items were converted to g/day and the foods were coded and analyzed for nutrient composition using the software EBISpro version 11 for Windows (Erhard, Willstätt, Germany) including the “Bundeslebensmittelschlüssel” version 3.01.
Statistical procedures
The intention to treat analysis included all participants who were randomly assigned to the study groups. R statistics software (R Development Core Team, Vienna, Austria) was used in combination with multiple imputation by Amelia II.26 The full dataset was used for multiple imputations, with imputation being repeated 100 times. Amelia II confirmed that the multiple imputations worked well in all cases. Normal distribution of the primary and secondary outcomes presented in this contribution was statistically and graphically checked. Within-group changes were analyzed by dependent Student’s t-tests. In order to determine differences between the groups, one-way analysis of variance was applied using the approach of Allison27 to combine the results of the imputed datasets. In case of relevant differences, pairwise t-tests comparisons with pooled SD were conducted. In order to adjust for multiple testing P-values obtained in the pairwise comparisons, we used the method of Holm.28 All tests were two-tailed, significance was accepted at P<0.05 or adjusted at <0.05.
Results
The percentage of patients lost to follow-up was 10% in the WB-EMS groups and 12% in the CG. Reasons for withdrawal are given in Figure 1. WB-EMS session attendance rate was high and did not significantly vary between the two groups (WB-EMS: 89%±6% vs WB-EMS&P: 88%±7%; P=0.453).
All participants of the WB-EMS&P group were fully compliant with the required dietary supplement intake, which was in accordance with our supplementation lists. Furthermore, all members said that they had taken the prescribed dose of 800 IE/day of vitamin D without interruption.
With respect to changes of parameters that may confound our results, we did not detect relevant variations within or between the groups. Lifestyle, PA, or exercise did not vary during the intervention period. Further, no participant reported worsening of diseases that may have confounded our primary results. However, four participants (WB-EMS: n=1; WB-WMS&P: n=2; CG: n=1) stated injuries that prevented WB-EMS and/or reduced habitual activity or exercise outside FORMOsA for longer than 2 weeks (with a maximum of 4 weeks).
Energy (−139±228 kcal, P=0.019) and protein intake (−0.07±0.21 g/kg/body mass/day, P=0.173) changed in the WB-EMS group only. However, due to the dietary supplements, energy intake remained at pre-study level and each participant of the WB-EMS&P group obtained the prescribed protein intake of at least 1.20 g/kg body mass/day. Carbohydrates and fat intake remained stable in the WB-EMS and CG (P≥0.799) and slightly decreased in the WB-EMS&P group (carbohydrates: 5.3%, P=0.306; fat: 7.6%, P=0.154). Dietary vitamin D intake did not change relevantly in the study groups (≤3%; P=0.821) during the interventional period.
Finally, none of the participants complained about serious side effects, but one test person lost interest and finally quit because of a feeling of discomfort during WB-EMS application.
At baseline, 30% (WB-EMS&P) to 35% (WB-EMS) of this cohort of community-dwelling women aged ≥70 years with SO suffered from MetS according to NCEP ATP-III. MetS Z-score significantly (P=0.001) improved in the WB-EMS&P group; however, the reduction among the WB-EMS group was less than expected and did not reach a statistically significant level (P=0.173) (Table 2). In parallel, only the WB-EMS&P (P=0.007) but not the WB-EMS group (P=0.105) differed significantly from the CG that was slightly worse (P=0.324) (Table 2), so we deduce that WB-EMS training alone does not significantly improve the MetS (Z-score) in community-dwelling older woman, as we hypothesized. With respect to our secondary hypothesis, the difference between the two WB-EMS groups was not significant either (P=0.235), thus we have to revise this hypothesis too.
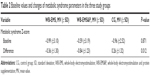
Looking behind the constituting variables of the MetS Z-score we found significant differences. Baseline values, changes, and inter-group differences of selected parameters of the MetS Z-score are shown in Table 3. WC decreased in both WB-EMS groups (WB-EMS: −1.5%±2.3%, P=0.004; WB-EMS&P: 0.7%±1.6%, P=0.053) and was maintained in the CG (P=0.963). In parallel, MAP significantly decreased in both verum groups (WB-EMS: −8.1%±10.1% P=0.001 and WB-EMS&P: −9.0%±8.9%; P≤0.001) only. In the CG, HDL-C decreased significantly (6.6%±9.5%, P=0.007) with no significant changes in the WB-EMS (−1.8%±8.6%, P=0.373) or WB-EMS&P group (2.6%±10.7%, P=0.141). Slightly negative (CG, P=0.290), no (WB-EMS), or slightly favorable changes (P=0.301) were observed for TGs, while FPG non-significantly decreased (P>0.40) in all study groups. With respect to specific (pairwise) between-group differences, we did not determine significant results between the WB-EMS groups. In detail, both groups significantly differed from the CG for MAP (P≤0.038); furthermore, the WB-EMS groups significantly varied for WC (P=0.036) and the WB-EMS&P group significantly differed for HDL-C (P=0.006) from the CG.
  | Table 3 Baseline values and changes of selected parameters constituting the metabolic syndrome Z-score according to the NCEP ATP III criteria17 |
Discussion
The present study clearly confirmed our hypothesis of a favorable effect of WB-EMS-application on the MetS in this cohort of community-dwelling women aged ≥70 years with SO, though the effect was significant in the WB-EMS group with additional protein supplementation only. Although the latter finding did not clearly confirm our secondary hypothesis, we assumed that protein supplementation may have an additive effect to resistance type exercise with respect to the MetS. However, based on the present literature, this estimation was vague, although the effect of resistance training, which may be the type of exercise most prone to WB-EMS, with or without additional protein supplementation on cardiometabolic risk was very rarely addressed.29–31 After 12 weeks of resistance exercise with high volume and intensity, DeNysschen et al29 did not report an effect of additional protein supplementation (either 26.6 g whey or 25.5 g soy protein/day compared with placebo) on (abdominal) body fat, serum lipids, and lipoproteins in their cohort of middle-aged hyperlipidemic, predominantly overweight men. Unfortunately, the sample size (n≤10/subgroup) of this study may have been too low to generate adequate power to clearly address this issue. However, generating a more adequate statistical power, Kemmler et al30 demonstrated that 16 weeks of high-intensity resistance exercise with or without additional proteins (total protein intake: ≥1.5 g/kg body mass/day) did not result in significant group differences with respect to improvements of the MetS in a comparable male cohort. In parallel, after 6 months of a predominantly resistance-type protocol conducted with moderate volume and high intensity (80% of 1 repetition maximum), Weinheimer et al31 did not demonstrate a significant additional effect of whey protein (20, 40, or 60 g/day) on the MetS in middle-aged overweight to obese persons. However, the above-listed studies considerably vary from the sarcopenia status and the intervention of the older women of the present study; thus a direct comparison is difficult. Reducing the complexity of this issue, at least the positive effect of (whey) protein on cardiometabolic risk factors (ie, fat mass, hypertension, lipids and lipoproteins, and inflammatory markers) has been confirmed.32
Revisiting the primary hypothesis of the study, the fact that despite comparable high and significant effects on muscle mass in both WB-EMS groups, Kemmler et al33 suggested that the mechanism of WB-EMS effects on cardiometabolic risk factors may not be necessarily muscle-induced. Indeed, the traditional belief of a generally beneficial effect of muscle tissue on cardiometabolic risk34 is vague. Even for glucose tolerance or insulin sensitivity in overweight and obese persons, recent findings by Kuk et al35 suggested that skeletal muscle mass per se is not associated with cardiometabolic parameters. Reductions of WC, which is considered a valid determinant of (intra-) abdominal fat,36,37 a parameter closely related to MetS,35,38,39 was also comparable between the WB-EMS groups, thus this parameter cannot be mentioned for the lack of significant effects of isolated WB-EMS on the MetS. In summary, we conclude that there is a minor additive effect of protein to resistance exercise that contributes to the results presented here.
Some limitations of the study have to be addressed to allow the reader to estimate the generalizability, applicability, and relevance of our results.
(a) The use of a MetS Z-score that summarizes the multiple aspects of the cardiometabolic risk may be irritating at first; however, creating a continuous score is much more sensitive to changes than to evaluate the prevalence of the MetS per se or the number of prevalent MetS risk factors.21 A limitation of the MetS calculation is that all parameters were equally weighted, although some parameters might have a bigger impact on the development of cardiometabolic diseases than others. (b) One may argue that the statistical power of the study was too low to address the MetS, because our sample size calculation was based on the ASMM as the more critical endpoint with respect to an intervention that focuses on women with SO. However, a recent study addressed a high intensity training resistance training protocol, ie, an exercise method very close to a WB-EMS intervention,40 indicating that the sample size calculated for ASMM (n=25 per group) was sufficient to address the MetS in parallel. However, we have to admit that the power to evaluate the presumably less prominent effect of additional (to WB-EMS) protein supplements on the MetS (and on ASMM) may have been indeed too low. We were aware of this problem; however, in stark contrast to the data reported by Batsis et al2 and even when focussing on the SMI16 as the sole sarcopenia criteria (which may also be considered as a study limitation), the prevalence of sarcopenia in community-dwelling older women is rare, at least in Germany.41 Also, bearing in mind the additional obesity criteria and the factor that this cohort is hard to convince to exercise frequently, we were finally contended to even generate the estimated sample size of 25 eligible women/group (out of n=1,325), necessary to address the effect of our primary hypothesis. In summary, we consider the additional protein issue more as an experimental hypothesis with a pilot study character. (c) With respect to the intervention, the WB-EMS application in a lying/sitting supine position 20 min once a week may have been too gentle, at least considering the unexpected high physical fitness level of the cohort (Table 1). In parallel, average protein intake at baseline was unexpectedly high in all groups (Table 1). Our protocol scheduled a daily protein supplementation of >1.2–<1.4 g/kg body mass/day for the WB-EMS&P group, which may be too close to the 1.0–1.1 g/kg/day of the dietary protein intake of the non-supplemented groups (WB-EMS and CG) to generate a relevant effect.
Conclusion
Although our result might not be generalizable across all cohorts with sarcopenia or SO, it indicates at least the general effectiveness, safety, attractiveness, and feasibility of WB-EMS. However, taking into account the lower strain threshold of institutionalized women, we speculatively expected higher effects compared with our multimorbid but unexpectedly fit community dwelling cohort. Addressing the relevance of WB-EMS in older people with unfavorable body composition and functional limitation, we conclude that multimodal exercise protocol with endurance, resistance, and coordination would be definitely superior to WB-EMS application. However, as a matter of fact, the majority of older people are either no more capable or/and unexperienced to participate in intense and time-consuming exercise protocols.42 Thus, the take home message of this article is that WB-EMS can be considered as an appropriate training option for people unable or unwilling to exercise conventionally.
Acknowledgments
The authors would like to thank the “Bayerische Forschungsstiftung” (Munich, Germany) for supporting the FORMOsA project. They further acknowledge the support of miha-bodytec (Gersthofen, Germany), Nutricia (Erlangen, Germany), and physiomed (Leipersdorf, Germany).
The present work was performed in fulfillment of the requirements for obtaining the degree “Dr. med.”
Disclosure
The authors report no conflicts of interest in this work.
References
Stenholm S, Harris TB, Rantanen T, Visser M, Kritchevsky SB, Ferrucci L. Sarcopenic obesity: definition, cause and consequences. Curr Opin Clin Nutr Metab Care. 2008;11(6):693–700. | ||
Batsis JA, Barre LK, Mackenzie TA, Pratt SI, Lopez-Jimenez F, Bartels SJ. Variation in the prevalence of sarcopenia and sarcopenic obesity in older adults associated with different research definitions: dual-energy X-ray absorptiometry data from the national health and nutrition examination survey 1999–2004. J Am Geriatr Soc. 2013;61(6):974–980. | ||
Dominguez LJ, Barbagallo M. The cardiometabolic syndrome and sarcopenic obesity in older persons. J Cardiometab Syndr. 2007;2(3):183–189. | ||
Kim SH, Chung JH, Song SW, Jung WS, Lee YA, Kim HN. Relationship between deep subcutaneous abdominal adipose tissue and metabolic syndrome: a case control study. Diabetol Metab Syndr. 2016;8:10. | ||
Lee J, Hong YP, Shin HJ, Lee W. Associations of sarcopenia and sarcopenic obesity with metabolic syndrome considering both muscle mass and muscle strength. J Prev Med Public Health. 2016;49(1):35–44. | ||
Klip A, Paquet MR. Glucose transport and glucose transporters in muscle and their metabolic regulation. Diabetes Care. 1990;13(3):228–243. | ||
Reaven GM. Banting lecture 1988. Role of insulin resistance in human disease. Diabetes. 1988;37(12):1595–1607. | ||
Cornelissen VA, Fagard RH, Coeckelberghs E, Vanhees L. Impact of resistance training on blood pressure and other cardiovascular risk factors: a meta-analysis of randomized, controlled trials. Hypertension. 2011;58(5):950–958. | ||
Strasser B, Schobersberger W. Evidence for resistance training as a treatment therapy in obesity. J Obes. 2011;2011.pii:482564. | ||
Chodzko-Zajko WJ, Proctor DN, Fiatarone Singh MA, et al. American College of Sports Medicine position stand. Exercise and physical activity for older adults. Med Sci Sports Exerc. 2009;41(7):1510–1530. | ||
Kemmler W, Bebenek M, Engelke K, von Stengel S. Impact of whole-body electromyostimulation on body composition in elderly women at risk for sarcopenia: the Training and ElectroStimulation Trial (TEST-III). Age (Dordr). 2014;36(1):395–406. | ||
Kemmler W, von Stengel S. Whole-body electromyostimulation as a means to impact muscle mass and abdominal body fat in lean, sedentary, older female adults: subanalysis of the TEST-III trial. Clin Interv Aging. 2013;8:1353–1364. | ||
Kemmler W, Schliffka R, Mayhew JL, von Stengel S. Effects of whole-body electromyostimulation on resting metabolic rate, body composition, and maximum strength in postmenopausal women: the training and electrostimulation trial. J Strength Cond Res. 2010;24(7):1880–1887. | ||
De Luis DA, Lopez Mongil R, Gonzalez Sagrado M, Lopez Trigo JA, Mora PF, Castrodeza Sanz J; Group Novomet. Prevalence of metabolic syndrome with International Diabetes Federation Criteria and ATP III Program in patients 65 years of age or older. J Nutr Health Aging. 2010;14(5):400–404. | ||
Lu CW, Yang KC, Chang HH, Lee LT, Chen CY, Huang KC. Sarcopenic obesity is closely associated with metabolic syndrome. Obes Res Clin Pract. 2013;7(4):e301–e307. | ||
Goisser S, Kemmler W, Porzel S, et al. Sarcopenic obesity and complex interventions with nutrition and exercise in community-dwelling older persons – a narrative review. Clin Interv Aging. 2015;10:1267–1282. | ||
Executive summary of the third report of The National Cholesterol Education Program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (Adult Treatment Panel III). JAMA. 2001;285(19):2486–2497. | ||
Janssen I, Baumgartner RN, Ross R, Rosenberg IH, Roubenoff R. Skeletal muscle cutpoints associated with elevated physical disability risk in older men and women. Am J Epidemiol. 2004;159(4):413–421. | ||
Physical status: the use and interpretation of anthropometry. Report of a WHO expert committee. World Health Organ Tech Rep Ser. 1995;854:1–452. | ||
Borg E, Kaijser L. A comparison between three rating scales for perceived exertion and two different work tests. Scand J Med Sci Sports. 2006;16(1):57–69. | ||
Johnson JL, Slentz CA, Houmard JA, et al. Exercise training amount and intensity effects on metabolic syndrome (from Studies of a Targeted Risk Reduction Intervention through Defined Exercise). Am J Cardiol. 2007;100(12):1759–1766. | ||
Kemmler W, Riedel H. Körperliche Belastung und Osteoporose – Einfluβ einer 10monatigen Interventionsmaβnahme auf ossäre und extraossäre Risikofaktoren einer Osteoporose. Dtsch Z Sportmed. 1998;49(9):270–277. | ||
Fahrenberg J, Myrtek M, Wilk D, Kreutel K. [Multimodal assessment of life satisfaction: a study of patients with cardiovascular diseases]. Psychother Psychosom Med Psychol. 1986;36(11):347–354. | ||
Kemmler W, Weineck J, Kalender WA, Engelke K. The effect of habitual physical activity, non-athletic exercise, muscle strength, and VO2max on bone mineral density is rather low in early postmenopausal osteopenic women. J Musculoskelet Neuronal Interact. 2004;4(3):325–334. | ||
Volkert D, Kreuel K, Heseker H, Stehle P. Energy and nutrient intake of young-old, old-old and very-old elderly in Germany. Eur J Clin Nutr. 2004;58(8):1190–1200. | ||
Honaker J, King G, Blackwell M. Amelia II: a program for missing data. JSS. 2011;45:1–47. | ||
Alison P. Missing Data. Thousand Oaks, CA: Sage Publication; 2002. | ||
Holm S. A simple sequentially rejective multiple test procedure. Scand J Stat. 1979;6:65–70. | ||
Denysschen CA, Burton HW, Horvath PJ, Leddy JJ, Browne RW. Resistance training with soy vs whey protein supplements in hyperlipidemic males. J Int Soc Sports Nutr. 2009;6:8. | ||
Kemmler W, Wittke A, Bebenek M, Frohlich M, von Stengel S. High intensity resistance training methods with and without protein supplementation to fight cardiometabolic risk in middle-aged males: a randomized controlled trial. Biomed Res Int. 2016;2016:9705287. | ||
Weinheimer EM, Conley TB, Kobza VM, et al. Whey protein supplementation does not affect exercise training-induced changes in body composition and indices of metabolic syndrome in middle-aged overweight and obese adults. J Nutr. 2012;142(8):1532–1539. | ||
Pal S, Radavelli-Bagatini S. The effects of whey protein on cardiometabolic risk factors. Obes Rev. 2013;14(4):324–343. | ||
Kemmler W, Teschler M, Weissenfels A, et al. Whole-body Electromyostimulation to fight sarcopenic obesity in community-dwelling older women at risk. Results of the randomized controlled FORMOsA-sarcopenic obesity study. Osteoporos Int. 2016;27(10):3261–3270. | ||
Bayol SA, Bruce CR, Wadley GD. Growing healthy muscles to optimise metabolic health into adult life. J Dev Orig Health Dis. 2014;5(6):420–434. | ||
Kuk JL, Kilpatrick K, Davidson LE, Hudson R, Ross R. Whole-body skeletal muscle mass is not related to glucose tolerance or insulin sensitivity in overweight and obese men and women. Appl Physiol Nutr Metab. 2008;33(4):769–774. | ||
Kamel EG, McNeill G, Van Wijk MC. Usefulness of anthropometry and DXA in predicting intra-abdominal fat in obese men and women. Obes Res. 2000;8(1):36–42. | ||
Despres JP, Prud’homme D, Pouliot MC, Tremblay A, Bouchard C. Estimation of deep abdominal adipose-tissue accumulation from simple anthropometric measurements in men. Am J Clin Nutr. 1991;54(3):471–477. | ||
Haffner SM. Abdominal adiposity and cardiometabolic risk: do we have all the answers? Am J Med. 2007;120(9 Suppl 1):S10–S16; discussion S16–S17. | ||
Despres JP, Lemieux I. Abdominal obesity and metabolic syndrome. Nature. 2006;444(7121):881–887. | ||
Kemmler W, Teschler M, Weiβenfels A, et al. Effects of whole-body electromyostimulation versus high-intensity resistance exercise on body composition and strength: a randomized controlled study. Evid Based Complement Alternat Med. 2016;2016:9236809. | ||
Kemmler W, von Stengel S, Engelke K, Sieber C, Freiberger E. Prevalence of sarcopenic obesity in Germany using established definitions: baseline data of the FORMOsA study. Osteoporos Int. 2016;27(1):275–281. | ||
Clark DO. Physical activity and its correlates among urban primary care patients aged 55 years or older. J Gerontol B Psychol Sci Soc Sci. 1999;54(1):S41–S48. | ||
Schafer I, von Leitner EC, Schon G, et al. Multimorbidity patterns in the elderly: a new approach of disease clustering identifies complex interrelations between chronic conditions. PLoS One. 2010;5(12):e15941. | ||
McAuley E, Konopack JF, Motl RW, Rosengren K, Morris KS. Measuring disability and function in older women: psychometric properties of the late-life function and disability instrument. J Gerontol A Biol Sci Med Sci. 2005;60(7):901–909. | ||
Dias N, Kempen GI, Todd CJ, et al. [The German version of the Falls Efficacy Scale-International Version (FES-I)]. Z Gerontol Geriatr. 2006;39(4):297–300. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.