Back to Journals » International Journal of General Medicine » Volume 15
Impact of Weight Loss on the Severity of Albuminuria in Obese Diabetic Patients Undergoing Laparoscopic Sleeve Gastrectomy and One-Anastomosis Gastric Bypass
Authors Salman AA , Salman MA , Aon MH, Mahdy RE, Abdallah A, Shemy GG, Hassan AM, Amin FAS, Labib S
Received 4 March 2022
Accepted for publication 21 July 2022
Published 4 August 2022 Volume 2022:15 Pages 6405—6413
DOI https://doi.org/10.2147/IJGM.S365113
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Ahmed Abdallah Salman,1 Mohamed Abdalla Salman,2 Mohamed H Aon,1 Reem Ezzat Mahdy,3 Ahmed Abdallah,2 Gamal Galal Shemy,4 Ahmed M Hassan,4 Fatema Alzahraa Samy Amin,5 Safa Labib1
1Internal Medicine Department, Faculty of Medicine, Cairo University, Cairo, Egypt; 2General Surgery Department, Faculty of Medicine, Cairo University, Cairo, Egypt; 3Internal Medicine Department, Faculty of Medicine, Assiut University, Assiut, Egypt; 4General Surgery Department, Faculty of Medicine, Al-Azhar University, Assiut Branch, Assiut, Egypt; 5Clinical Pathology Department, Faculty of Medicine, Cairo University, Cairo, Egypt
Correspondence: Ahmed Abdallah Salman, Internal Medicine Department, Faculty of Medicine, Cairo University, Cairo, Egypt, Tel +20 1000468664, Email [email protected]
Aim: To examine the effect of weight-loss induced bariatric procedures on albuminuria levels among diabetic patients suffering from obesity.
Methods: Adults patients who suffer from morbid obesity and type 2 diabetes mellitus (T2DM) were included in a prospective cohort study. Subjects were scheduled to undergo laparoscopic sleeve gastrectomy (LSG) or one-anastomosis gastric bypass (OAGB). The albumin-to-creatinine ratio (ACR) was adopted to assess the degree of albuminuria. Microalbuminuria was determined as a ratio of > 2.5– 30 mg/mmol and > 3.5– 30 mg/mmol for males and females, respectively, while macroalbuminuria was diagnosed when the ACR exceeded > 30 mg/mmol.
Results: The mean uACR decreased significantly from 20.95± 16.89 to 9.92± 12.69mg/mmol in LSG cohort (p < 0.001), and from 19.52± 16.65 to 9.34± 11.77mg/mmol in the OAGB cohort, with no statistically considerable differences between both cohorts at the end of follow-up (p = 0.78). Twelve months after the procedures, the percentages of cases with microalbuminuria decreased significantly to 23.8% and 23.9%, respectively (p < 0.001); likewise, the percentages of cases with macroalbuminuria significantly decreased to 7.9% and 7.5% in the LSG and OAGB groups, respectively (p < 0.001). There were no statistically considerable differences between LSG and OAGB regarding the percentages of patients with micro or macroalbuminuria at the end of follow-up. Besides, there were no significant associations between the degree of weight loss and improvement (p = 0.959) or remission (p = 0.73) of microalbuminuria.
Conclusion: Bariatric surgery significantly reduced the severity of albuminuria 1-year after the procedure, with no preference for one procedure over the other.
Keywords: bariatric surgery, laparoscopic sleeve gastrectomy, one-anastomosis gastric bypass, microalbuminuria
Introduction
Diabesity (a term donates coexistence of obesity and diabetes mellitus) is a growing global health concern with a progressive increase in its incidence in the Middle East and Africa.1 The occurrence of type 2 diabetes mellitus (T2DM) is rising globally due to the sedentary behavior and high caloric density food that acts on susceptible genotypes.2 On the other hand, the incidence of obesity has been tripled in the past few decades.3 While the interaction between T2DM and obesity is established, there are many uncertainties about the pathophysiological mechanisms underlying association. Obesity is a known contributor to insulin resistance and hyperglycemia through induction of chronic inflammation, dysfunctional entero-insular axis, and excessive release of adipokines.4,5 Regardless of the underlying mechanism, the coexistence of obesity and T2DM significantly exacerbates the risk of various metabolic complications.6 Thus, recent guidelines emphasize the significance of weight loss on optimizing glycemic states in T2DM.7
Chronic kidney disease (CKD) is one of the most undesirable adverse effects of diabesity. Diabetic nephropathy is assumed to occur in nearly one-third of T2DM subjects, which, in return, can cause renal dysfunction and chronic renal failure.8 On the other hand, obesity alone represents an independent risk factor for CKD; excessive weight causes renal hyperfiltration and proteinuria, which consequently contributes to developing CKD.9 When obesity and diabetes co-exist, the risk of glomerulopathy, renal hypertension, and CKD increased progressively.10 Previous work showed that microalbuminuria, a well-recognized surrogate of renal dysfunction, is an early sign in obese patients with diabetic kidney disease; the magnitude of albuminuria was demonstrated to be considerably related to the body weight in diabetic patients suffering from obesity.11 Furthermore, microalbuminuria was shown to be an early indicator of end-stage renal disease (ESRD) and cardiovascular comorbidities in these category of patients.9 Thus, it is logical to assume an improvement in the degree of albuminuria is a marker of resolution of obesity-mediated renal injury following any successful weight loss strategy.
Metabolic surgery, the most efficacious weight reduction approach, has a well-known effect on diabetes control in cases with T2DM.12,13 The improvement is mainly seen in the early postoperative period even before the weight loss is observed, and it is more obvious in patients who achieve the weight loss surgically than the non-surgical methods.14,15
The physiopathological mechanisms that ameliorate glucose homeostasis following metabolic surgery are still unclear. Nonetheless, it is thought that the different gastrointestinal surgeries may have various effects and mechanisms of action. Bariatric surgery can help incorporate knowledge and multidisciplinary proficiency to supply a combination of conservative and surgical approaches for Type II diabetes. These treatments must be viewed as complementary choices and not alternative strategies, with the same aim of managing diabetes and attaining cure.16 In addition, a growing body of literature indicated a positive impact of weight reduction in post-bariatric renal functions, especially in diabetic patients.17
However, the effect of metabolic procedures on albuminuria, as an early predictor of progressive renal disease, has not been well studied yet. Therefore, the current work aimed to examine the effect of weight reduction following bariatric operations on albuminuria levels among diabetic patients suffering from obesity and to examine whether the type of surgery has a role in post-procedure albuminuria.
Subjects and Methods
Study Design and Population
In a prospective, observational study, adult cases (16–60 years old) who were scheduled to undergo laparoscopic sleeve gastrectomy (LSG) or one-anastomosis gastric bypass (OAGB) were recruited through the period from June 2014 to April 2018. Patients were deemed eligible if they had T2DM, a BMI >35 kg/m2, and a history of resistance to conservative approaches for weight loss. The study complied with the Declaration of Helsinki.
Factors that were viewed when deciding on the type of operation to be done were preoperative BMI, existence of GERD, eating behavior, and point of view for every participant. Participants suffering from morbid obesity were advised that LSG should give inferior results compared to OAGB. Participants with GERD were advised about the possible refluxogenic adverse effect of LSG and the data results showing considerable resolution in reflux after OAGB.
American diabetes association (ADA) guidelines were adopted to define T2DM guided by fasting plasma glucose (FPG) concentration: clinical diabetes was determined as FPG ≥126 mg/dl or (glycosylated hemoglobin) HbA1c ≥6.5, that was ensured by repeated blood samples unless the subject has clinical symptoms or glucose level of 200 mg/dl and previous history of the disease and/or usage of anti-diabetes drugs.18
We excluded patients with endocrinal causes for obesity, advanced medical conditions precluding anesthesia, not intending to modify lifestyle after operation, psychiatric contraindication, inconvenient social circumstances, previous bariatric operation, gestation, or lactation at screening or operation. All eligible cases signed written informed consent. The local ethical committee of Cairo University Hospitals approved the protocol.
Data Collection and Operational Definitions
Data were collected preoperatively then 1-year after the surgery. The data included demographic findings, history of chronic diseases, blood pressure, anthropometric measures, FPG, HbA1c, estimated glomerular filtration rate (eGFR), urine albumin-to-creatinine ratio (uACR), level of albuminuria, low-density lipoprotein (LDL), triglyceride, and cholesterol values.
The spot urine ACR measurements were adopted to evaluate albuminuria. The microalbuminuria was determined as an ACR of >2.5–30 mg/mmol and >3.5–30 mg/mmol for males and females, respectively. The macroalbuminuria was diagnosed when the ACR exceed >30 mg/mmol. The improvement in albuminuria was defined as any decrease in the levels of albuminuria. On the other hand, albuminuria cases, who had ACR of <2.5 mg/mmol at the end of follow-up, were defined as remitting cases.
The T2DM status at the end of follow-up was classified based on ADA; HbA1c lower than 5.7% with no diabetes drugs was viewed as remission and HbA1c 5.7–6.5% without diabetes drugs as partial remission.18
Surgical Technique
For patients who underwent LSG, pneumoperitoneum was induced using CO2. The Harmonic Scalpel™ (Ethicon Endo-Surgery) was used to dissect the gastrocolic ligament. A 36-Fr orogastric tube was put into the stomach and adjusted towards the pylorus. The gastric resection was performed using a laparoscopic linear stapler. For cases submitted to OAGB, a 50 mL gastric pouch was created, and loop gastrojejunostomy was carried out 200 cm from Treitz ligament. We have implemented the Rutledge approach, but instead of transverse anastomosis, longitudinal gastrojejunostomy with 4.5 cm blue cartridge on the posterior aspect of the pouch has been adopted.
Study’s Outcomes
The primary outcomes in this study were the change in mean uACR and the change in the percentages of cases with different grades of albuminuria at the end of follow-up. The secondary outcomes included the difference in the percentages of cases with different grades of albuminuria between LSG and OAGB groups, the changes in eGFR at the end of follow-up, the correlation between albuminuria changes and weight loss, the changes in blood glucose profile after 1 year, and the percentages of cases with improved or resolved T2DM at the end of the study.
Statistical Methodology
Statistical analysis was carried out through SPSS version 22. All variables were tested for distribution normality using Kolmogorov–Smirnov test. Based on data normality, mean ± standard deviation (SD) or median (range) were utilized for the expression of continuous data. Categorical variables were expressed as numbers and percentages. The change between the baseline and follow-up period was examined using paired-t-test or Wilcoxon signed-rank test for continuous variables and McNemar test for categorical variables. The two groups were compared using independent t-test or Mann–Whitney test for continuous variables and Chi-square test for categorical variables. The p values were corrected with Bonferroni correction whenever indicated due to multiple comparisons. The rejection of the null hypothesis was stated when the p-value was <0.05.
Results
A total of 130 subjects were included (LSG group = 63; OAGB group = 67). The mean age in the LSG cohort was 41.44±7.81 years, and the majority were males (61.9%), while the mean age in the OAGB group was 41.75±7.81 years (p = 0.82) and 62.7% were males (p = 0.92). The preoperative BMI was comparable between both groups (42.92±4.03kg/m2 in the LSG group versus 41.88±3.45kg/m2 in the OAGB group; p = 0.116). Preoperatively, both LSG and OAGB had comparable values regarding history of smoking (p = 0.694), hypertension (p =0.486), fasting blood glucose (p = 0.417), HbA1C (p = 0.706), and lipid profile (p > 0.05). The preoperative uACR was comparable between the LSG and OAGB groups (20.95±16.89 versus 19.52±16.65mg/mmol, respectively; p =0.628). The preoperative data are shown in Table 1. Preoperatively, 41.3% and 41.8% of the patients had microalbuminuria in the LSG and OAGB groups, respectively, while 31.7% and 26.9% of cases had macroalbuminuria in the LSG and OAGB groups, respectively (Figure 1).
 |
Table 1 Preoperative Data of the Examined Groups |
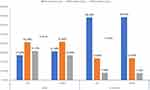 |
Figure 1 Percentages of patients with different classes of albuminuria pre and 1-year after the intervention. |
The mean uACR decreased significantly from 20.95±16.89 to 9.92±12.69mg/mmol in the LSG group (p <0.001), and from 19.52±16.65 to 9.34±11.77mg/mmol in the OAGB group. The eGFR increased significantly in the OAGB group only (p =0.049; Table 2).
 |
Table 2 The Change in Renal Parameters in Each Group |
Twelve months after the procedures, percentages of patients with microalbuminuria decreased substantially to 23.8% and 23.9%, respectively (p <0.001); likewise, the percentages of patients with macroalbuminuria significantly decreased to 7.9% and 7.5% in the LSG and OAGB groups, respectively (p <0.001; Figure 1).
There was no statistically considerable difference between LSG and OAGB regarding the percentages of patients with microalbuminuria after 12 months (p =0.961). Almost 72% in the LSG had improved albuminuria, compared to 67.4% in the OAGB (P =0.650), while 56.5% had remitting albuminuria in the LSG cohort, in comparison to 54.3% in the OAGB cohort (p =0.83; Figure 2).
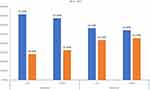 |
Figure 2 Percentages of improved and remitted albuminuria 1-year after the intervention. |
In addition, no significant associations were detected between percent of total weight loss and percentage of improved or remitting albuminuria (Table 3).
 |
Table 3 Relation Between Total Weight Loss and Albuminuria Changes |
With regard to the changes in metabolic parameters, body weight, blood pressure, fasting blood sugar, HbA1C, and lipid profile decreased significantly after either LSG or OAGB (p <0.05). The differences in these parameters between LSG and OAGB were not significant 1-year after the procedure (p >0.05), except for HDL-cholesterol. The percentage of complete T2DM remission was 46% in the LSG cohort and 46.35% in the OAGB cohort (p =0.72; Table 4).
 |
Table 4 The Change in Metabolic Parameters in Each Group |
Discussion
Few data are available regarding the effect of bariatric operations on the prevalence of post-procedure albuminuria, and whether one technique has superior results over the others in terms of the changes in the degree of albuminuria. In the current work, we compared different procedures (OAGB vs LSG) in terms of their effect on urinary albumin excretion. The choice of the operation for every participant was based on shared decision-making between the patient and the multidisciplinary team.
We demonstrated that bariatric surgery led to a statistically significant reduction in the degree of albuminuria among diabetic patients suffering from obesity. This reduction was consistent following LSG and OAGB, with no statistically significant difference. Similarly, previous studies failed in identifying differences between the effect of OAGB and LSG in terms of comorbidities improvement.19
On the other hand, no significant association was detected between the percent of total weight loss and the degree of albuminuria improvement.
Historically, eGFR was the marker of choice for progressive renal disease; however, eGFR is limited by being time-consuming with poor accuracy in detecting early renal damage.20 Thus, over the past years, albuminuria has been viewed as a reliable marker for renal damage in a variety of settings; microalbuminuria is an independent predictor for renal damage, progressive renal disease, acute renal failure, and ESRD.21 Moreover, microalbuminuria significantly predicts the risk of cardiovascular disease and death.22 Excess albumin excretion is prevalent in diabetic patients suffering from obesity owing to the synergistic adverse effect of both metabolic abnormalities on renal functions23; the damage of glomerular filtration barrier due to hypertension and hyperglycemia, cytokines release from adipose tissue and increased intrabdominal pressure secondary to excessive visceral fat are among the many theories proposed for albuminuria development in diabesity.24,25 Previous reports demonstrated that microalbuminuria presents early in obese cases with diabetic nephropathy; the degree of albuminuria was found to be significantly correlated with body weight in diabetic patients suffering from obesity as well.11 Thus, it is logical to assume an improvement in the degree of albuminuria should be a marker of the resolution of diabesity-mediated renal injury following any successful weight-loss strategy. In the present study, bariatric surgery resulted in a statistically substantial decline in the severity of albuminuria, with both techniques leading to a notable resolution. No significant association was found between weight loss and albuminuria.
In line with our results, Agrawal et al26 demonstrated a considerable decrease in the prevalence of albuminuria 1-year after bariatric surgery, especially in diabetic patients. No significant correlation was found between albuminuria and degree of weight reduction in another retrospective study by the same author group.27 Another two recent reports by Young et al28 and Park et al29 demonstrated a notable reduction in the microalbuminuria 1-year after bariatric operations in diabetic subjects with obesity. Notably, a 2015 report by Carlsson et al30 demonstrated a lower incidence of albuminuria in patients suffering from morbid obesity undergoing metabolic operations, in comparison to subjects suffering from obesity who receive conservative management.
Despite the notable effect of metabolic operations on the severity of albuminuria, the mechanisms of albuminuria improvement following the surgery are still largely unknown. The established reduction in the inflammatory status following bariatric surgery may explain albuminuria resolution, as detailed by Park et al29 and others.31,32 Bariatric surgery resolves the obesity-induced inflammatory status, which can be subsequently associated with a reduction in the inflammatory insults towards the glomerular filtration barrier. The resolution of the lipotoxic effect of excessive adipose tissue and the glucotoxic effect of T2DM may represent a potential mechanism for albuminuria improvement following metabolic procedures.33
The favorable effect of metabolic surgery on albuminuria was demonstrated in this analysis, the considerable decrease in the uACR 12 months postoperative. This was similar to a meta-analysis study performed by Upala et al,34 in which a significant reduction in uACR was shown following metabolic operations. Moreover, Amor et al35 and Henegan et al36 reported an improvement of uACR after 1 year and 5 years of bariatric surgery, respectively.
A cumulative body of literature has established the beneficial role of metabolic operations on glycemic control among diabetic patients; previous reports indicated that bariatric surgery significantly improves the glycemic status and leads to diabetes remission in a considerable proportion of the patients.37 In the present study, we found that both LSG and OAGB led to a statistically significant reduction in the blood glucose and HbA1c 12 months after the operation; the percentage of complete T2DM remission was 46% in LSG group and 46.35% in OAGB group. These conclusions agree with recent meta-analysis studies that showed persistent improvement in glycemic control among patients who underwent bariatric surgery.38,39
The current work may constitute a influential research in the future, given the novelty of the contribution and its clinically relevant value. Most importantly, given the statistical results, the study underlines the fact that bariatric surgeries have a favorable impact on albuminuria. Hence, this can strengthen the theory that the effects of metabolic operations are mainly metabolic and physiological rather than anatomical/mechanistic. Despite that, we admit that this work is limited by its observational nature that did not permit us to perform proper random allocation of the patients or blinding of the study’s investigators. Also, the absence of the comparison with a group of patients who underwent conventional or intensive care of diabetes (no-surgery group) is another limitation.
In conclusion, bariatric surgery substantially cuts down the severity of albuminuria 1-year after the operation, with no preference for one over the other. This decrease was independent of the amount of weight loss. Future studies should examine the impact of the resolution of inflammatory markers, insulin resistance and hyperglycemia on the post-bariatric prevalence of albuminuria.
Novelty of the Work
Based on the published data, only a few reports have studied the changes in albuminuria after bariatric surgery. So this work adds a stream to the literature in terms of this novel topic. Besides, amongst the advantages of the current work is the reasonable number of cases in both groups with a fairly good follow-up period. This point may make our work quite singular as it is often not simple to get patients back for another look after 12 months.
Furthermore, it is plausible to say that this study may draw attention to potential mechanisms that may be driving the beneficial impact of metabolic procedures on the kidney and could provide promising horizons in terms of this aspect; and possibly make it an attractive goal for new therapeutic approaches in disorders related to obesity and kidney disease.
Funding
No sources of funding.
Disclosure
The authors report no conflicts of interest in relation to this work.
References
1. Farag YMK, Gaballa MR. Diabesity: an overview of a rising epidemic. Nephrol Dial Transplant. 2011;26:28–35. doi:10.1093/ndt/gfq576
2. Cho NH. IDF Diabetes Atlas.
3. WHO. Obesity and overweight: fact sheet. In: WHO Media Cent. WHO; 2016:1–6.
4. Chadt A, Scherneck S, Joost H-G, et al. Molecular links between Obesity and Diabetes: ‘Diabesity’. MDText.com, Inc.; 2000. Available from: http://www.ncbi.nlm.nih.gov/pubmed/25905279.
5. Cətoi AF, Pârvu A, Mureşan A, et al. Metabolic mechanisms in obesity and type 2 diabetes: insights from bariatric/metabolic surgery. Obes Facts. 2015;8:350–363. doi:10.1159/000441259
6. Wells JCK. The diabesity epidemic in the light of evolution: insights from the capacity–load model. Diabetologia. 2019;62:1740–1750. doi:10.1007/s00125-019-4944-8
7. Dixon JB, Zimmet P, Alberti KG, et al. Bariatric surgery: an IDF statement for obese type 2 diabetes. Surg Obes Related Dis. 2011;7:433–447. doi:10.1016/j.soard.2011.05.013
8. Sun YM, Su Y, Li J, et al. Recent advances in understanding the biochemical and molecular mechanism of diabetic nephropathy. Biochem Biophys Res Commun. 2013;433:359–361. doi:10.1016/j.bbrc.2013.02.120
9. Maric-Bilkan C. Obesity and diabetic kidney disease. Med Clinics North Am. 2013;97:59–74. doi:10.1016/j.mcna.2012.10.010
10. Kramer H, Luke A, Bidani A, et al. Obesity and prevalent and incident CKD: the hypertension detection and follow-up program. Am J Kidney Dis. 2005;46:587–594. doi:10.1053/j.ajkd.2005.06.007
11. Eijkelkamp WBA, Zhang Z, Remuzzi G, et al. Albuminuria is a target for renoprotective therapy independent from blood pressure in patients with type 2 diabetic nephropathy: post hoc analysis from the reduction of endpoints in NIDDM with the angiotensin II antagonist losartan (RENAAL) trial. J Am Soc Nephrol. 2007;18:1540–1546. doi:10.1681/ASN.2006050445
12. Benaiges Boix D, Goday Arno A, Pedro-Botet J. Bariatric surgery for the treatment of type 2 diabetes mellitus. Med Clin (Barc). 2012;138:391–396. doi:10.1016/j.medcli.2011.04.009
13. Cummings DE, Arterburn DE, Westbrook EO, et al. Gastric bypass surgery vs intensive lifestyle and medical intervention for type 2 diabetes: the CROSSROADS randomised controlled trial. Diabetologia. 2016;59:945–953. doi:10.1007/s00125-016-3903-x
14. Fenske WK, Pournaras DJ, Aasheim ET, et al. Can a protocol for glycaemic control improve type 2 diabetes outcomes after gastric bypass? Obes Surg. 2012;22:90–96. doi:10.1007/s11695-011-0543-6
15. Lee WJ, Te HM, Wang W, et al. Effects of obesity surgery on the metabolic syndrome. Arch Surg. 2004;139:1088–1092. doi:10.1001/archsurg.139.10.1088
16. Gentileschi P, Bianciardi E, Benavoli D, Michela C. Metabolic surgery for type II diabetes: an update. Acta Diabetol. 2021;58:1153–1159. doi:10.1007/s00592-021-01722-w
17. Chagnac A, Weinstein T, Herman M, et al. The effects of weight loss on renal function in patients with severe obesity. J Am Soc Nephrol. 2003;14:1480–1486. doi:10.1097/01.ASN.0000068462.38661.89
18. American Diabetes Association. Diabetes care: standards of medical care in diabetes—2018. Diabetes Care. 2018. doi:10.2337/dc18-S002
19. Perrone F, Bianciardi E, Ippoliti S, et al. Long-term effects of laparoscopic sleeve gastrectomy versus Roux-en-Y gastric bypass for the treatment of morbid obesity: a monocentric prospective study with minimum follow-up of 5 years. Updates in Surgery. 2017;69:101–107. doi:10.1007/s13304-017-0426-z
20. Lopez-Giacoman S. Biomarkers in chronic kidney disease, from kidney function to kidney damage. World J Nephrol. 2015;4:57. doi:10.5527/wjn.v4.i1.57
21. Coresh J, Astor BC, Greene T, et al. Prevalence of chronic kidney disease and decreased kidney function in the adult US population: third National Health and Nutrition Examination Survey. Am J Kidney Dis. 2003;41:1–12. doi:10.1053/ajkd.2003.50007
22. Gansevoort RT, Matsushita K, van der Velde M, et al. Lower estimated GFR and higher albuminuria are associated with adverse kidney outcomes. A collaborative meta-analysis of general and high-risk population cohorts. Kidney Int. 2011;80:93–104. doi:10.1038/ki.2010.531
23. Minoo F, Mahdavi-Mazdeh M, Abbasi M-R, et al. Impact of the severity of obesity on microalbuminuria in obese normotensive nondiabetic individuals. J Ren Inj Prev. 2015;4:34–348. doi:10.12861/jrip.2015.08
24. Jauregui A, Mintz DH, Mundel P, et al. Role of altered insulin signaling pathways in the pathogenesis of podocyte malfunction and microalbuminuria. Curr Opin Nephrol Hypertens. 2009;18:539–545. doi:10.1097/MNH.0b013e32832f7002
25. Sharma K, RamachandraRao S, Qiu G, et al. Adiponectin regulates albuminuria and podocyte function in mice. J Clin Invest. 2008;118:1645–1656. doi:10.1172/JCI32691
26. Agrawal V, Khan I, Rai B, et al. The effect of weight loss after bariatric surgery on albuminuria. Clin Nephrol. 2008;70:194–202. doi:10.5414/CNP70194
27. Agrawal V, Krause KR, Chengelis DL, et al. Relation between degree of weight loss after bariatric surgery and reduction in albuminuria and C-reactive protein. Surg Obes Relat Dis. 2009;5:20–26. doi:10.1016/j.soard.2008.07.011
28. Young LA, Nor Hanipah Z, Brethauer SA, et al. Long-term impact of bariatric surgery in diabetic nephropathy. Surg Endosc. 2019;33:1654–1660. doi:10.1007/s00464-018-6458-8
29. Park S, Kim YJ, Choi C, et al. Bariatric surgery can reduce albuminuria in patients with severe obesity and normal kidney function by reducing systemic inflammation. Obes Surg. 2018;28:831–837. doi:10.1007/s11695-017-2940-y
30. Carlsson LMS, Romeo S, Jacobson P, et al. The incidence of albuminuria after bariatric surgery and usual care in Swedish obese subjects (SOS): a prospective controlled intervention trial. Int J Obes. 2015;39:169–175. doi:10.1038/ijo.2014.72
31. Hafida S, Mirshahi T, Nikolajczyk BS. The impact of bariatric surgery on inflammation: quenching the fire of obesity? Current Opinion in Endocrinology. Diabetes Obes. 2016;23:373–378.
32. Rao SR. Inflammatory markers and bariatric surgery: a meta-analysis. Inflamm Res. 2012;61:789–807. doi:10.1007/s00011-012-0473-3
33. Naira M, Le Roux CW, Docherty NG. Mechanisms underpinning remission of albuminuria following bariatric surgery. Curr Opin Endocrinol Diabetes Obes. 2016;23:366–372. doi:10.1097/MED.0000000000000279
34. Upala S, Wijarnpreecha K, Congrete S, et al. Bariatric surgery reduces urinary albumin excretion in diabetic nephropathy: a systematic review and meta-analysis. Surg Obes Relat Dis. 2016;12:1037–1044. doi:10.1016/j.soard.2015.11.019
35. Amor A, Jiménez A, Moizé V, et al. Weight loss independently predicts urinary albumin excretion normalization in morbidly obese type 2 diabetic patients undergoing bariatric surgery. Surg Endosc. 2013;27:2046–2051. doi:10.1007/s00464-012-2708-3
36. Heneghan HM, Cetin D, Navaneethan SD, et al. Effects of bariatric surgery on diabetic nephropathy after 5 years of follow-up. Surg Obes Relat Dis. 2013;9:7–14. doi:10.1016/j.soard.2012.08.016
37. Kashyap SR, Gatmaitan P, Brethauer S, et al. Bariatric surgery for type 2 diabetes: weighing the impact for obese patients. Cleve Clin J Med. 2010;77:468–476. doi:10.3949/ccjm.77a.09135
38. Khorgami Z, Shoar S, Saber AA, et al. Outcomes of bariatric surgery versus medical management for type 2 diabetes mellitus: a meta-analysis of randomized controlled trials. Obes Surg. 2019;29:964–974. doi:10.1007/s11695-018-3552-x
39. Baskota A, Li S, Dhakal N, et al. Bariatric surgery for type 2 diabetes mellitus in patients with BMI <30 kg/m2: a systematic review and meta-analysis. PLoS One. 2015;10. doi:10.1371/journal.pone.0132335
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
