Back to Journals » Pragmatic and Observational Research » Volume 13
Impact of the COVID-19 Pandemic on Trauma Service Utilization at a New York City Level I Trauma Center
Authors Rosen B, Pelle AL, Lakhi NA
Received 11 June 2022
Accepted for publication 10 August 2022
Published 5 September 2022 Volume 2022:13 Pages 93—103
DOI https://doi.org/10.2147/POR.S378189
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor David Price
Benjamin Rosen,1 Annemarie L Pelle,1 Nisha A Lakhi1,2
1Department of Surgery, New York Medical College, School of Medicine, Valhalla, New York, USA; 2Department of Trauma Surgery, Richmond University Medical Center, Staten Island, New York, USA
Correspondence: Nisha A Lakhi, Department of Obstetrics and Gynecology/Trauma Surgery, Richmond University Medical Center, 355 Bard Avenue, Staten Island, New York, 10310, USA, Tel +1 718-818-1823, Email [email protected]
Background: The COVID-19 pandemic globally impacted trauma facilities and overall healthcare utilization. This study was conducted to characterize the utilization of trauma services at our Level I Trauma Center in New York City during the COVID-19 pandemic compared to the preceding pre-pandemic year.
Methods: A retrospective study of patient presenting to our Level 1 Trauma Center in Staten Island, New York. The pre-pandemic data was extracted from March 1st, 2019–February 29th, 2020. The pandemic year was divided into two phases: the initial wave (March 1st–Sept 1st, 2020) and the protracted phase (September 1st, 2020–March 1st, 2021). Patients were identified using ICD-10 coding and data regarding patient factors, mechanism of injury, and service utilization was extracted from the medical record. Statistical analysis was performed using IBM SPSS v.24.
Results: A total of 1650 trauma activations registered during the pre-pandemic phase, 691 during the initial wave, and 826 during the protracted phase. Compared to pre-pandemic, the number of Level 1 trauma activations remained unchanged, however mechanisms of injury shifted. Gunshot wounds (2.6% vs 1.2%), motorcycle crash (4.2% vs 2.0%) and blunt force injury caused by an object (strike injuries) (2.7% vs 1.3%) significantly increased during the initial wave (p-value < 0.05). There was a significant decrease in the percentage of both female (2.93% vs 2.33% vs 5.64%, p-value < 0.01) and pediatric (3.30% vs 3.64% vs 12.9%, p-value < 0.001) assault activations during the initial wave and protracted phase when compared to pre-pandemic levels, respectively. No significant changes were observed for self-harm, falls, accidents, burns, sports injuries, stab wounds, autobody collisions, or motor vehicle accident activations.
Conclusion: Trauma centers should be prepared for increases in violent trauma. We also emphasize the need to implement strategies to raise public awareness of pediatric and female assault in the domestic setting, particularly during a mandatory stay-at-home policy where underreporting may occur.
Keywords: trauma center, COVID-19, mechanism of injury, service utilization
Introduction
On March 1st 2020, the first case of the SARS-Cov-2 pandemic was confirmed in New York City. As such, New York was the first state to start lockdown orders and mandatory quarantining. Starting March 16th, schools closed and on March 20th non-essential businesses closed as well. This drastically changed the daily lives of many people and influenced daily decisions, including seeking out medical care. 1,2 From the beginning of the COVID-19 emergency, the infectivity of the virus discouraged patients from visiting trauma centers, hospitals, and doctor offices. Consequently, there was a decrease in trauma patients seeking emergency care.3,4 Some researchers have suggested that decreases in trauma activations can be attributed to avoidance of trauma reporting as patients avoided hospitals in an effort to not contract the virus. Social distancing and quarantine measures reinforced this behavior as trauma centers, hospitals and doctor offices were thought of as areas for high-risk contact with sick patients5–8 This suggests that the decrease in trauma activations during the pandemic may not actually reflect a decreased incidence of injuries, but rather a deliberate avoidance of patients to frequent trauma centers during the initial wave of the pandemic.9 Furthermore, the avoidance of necessary medical care may have resulted in increased medical complications resulting in further harm and increased medical consultations.10 This study aims to compare the variation of volume and mechanisms of trauma activations, as well as patient characteristics such as gender and age, at a New York City Level I Trauma Center during the initial wave and protracted phase of the COVID-19 pandemic. To this end, we compared trauma data observed in the previous years to compare these changes, identify potential causes driving these changes, and investigate future interventions to prepare trauma centers for future pandemics to optimize the healthcare system’s response.
Methods
This retrospective study was conducted at Richmond University Medical Center (Staten, Island, New York) and New York Medical College (Valhalla, New York). The study protocol (protocol number: #14609) was reviewed by the Institutional Review Board of New York Medical College and received an IRB exemption. The data accessed complied with relevant data protection and privacy regulations.
The primary objective of this study was to quantify and characterize the utilization of trauma services at our Level I trauma center in New York City during the COVID-19 pandemic compared to the preceding pre-pandemic year. Richmond University Medical Center is a 470+ bed healthcare facility and one of two acute care facilities that serves nearly 500,000 residents of xxx. The medical center provides Level I Adult & Level II Pediatric Trauma services and care for most of the penetrating traumas on Staten Island, New York. It offers one of the largest arrays of emergency, inpatient, ambulatory, mental health, and substance abuse programs in the state of New York. Our trauma center serves an ethnically diverse population (29.1% Hispanic, 22.5% Black) in which 23.7% of residents are foreign born.
The pre-pandemic data was extracted from March 1st, 2019–February 29th, 2020. The pandemic year was divided into two phases: the initial wave (March 1st–Sept 1st, 2020) and the protracted phase (September 1st, 2020–March 1st, 2021). These dates were determined based on the timeline of the New York City quarantine and social distancing measures.1,2 Primary outcome consisted of differences between the COVID-19 cohorts and control pre-pandemic cohort with respect to type of injury, trauma activations, inpatient hospitalization, admission to Intensive Care Unit, and length of stay. For secondary outcomes, data was stratified by patient age and gender. The age groups used for stratification were <18 years of age, 18–64, and >65 years old for age.
Diagnoses and procedures were encoded according to the International Classification of Diseases, 10th Edition, Clinical Modification (ICD-10). Data elements were extracted directly from our trauma registry’s electronic health records using the ICD-10 codes to identify subjects. Additional data points collected included patient age, gender, mechanism of injury, level of trauma activation (Level 1, Level 2, Level 3), hospital admission service, Intensive Care Unit (IUC) admission, and length of hospital/ICU stay. Level 1 trauma activations were reserved for the most emergent patients. Level 1 activations included patients that were hemodynamically unstable, all major penetrating trauma involving the torso, open or unstable pelvic fractures, long bone fractures, head trauma with loss of consciousness, high impact collisions, as well as trauma with 1st or 2nd degree burns covering more than 20% of the body surface area. Level 2 trauma activations were for less severe injuries that still warranted the immediate attention of the trauma team. Level 3 activations were for non-emergent conditions requiring evaluation and possible admission. Appendix 1 describes specific criterium for Level of activation at our Trauma center (Appendix 1). Type of Injury was classified by mechanism of occurrence. The term “Accident” was used to encompass several unspecified events that included bumping into an object (ie wall); inadvertent contact with a sharp object (ie knife, glass); inadvertent contact with a blunt object; being caught, crushed, jammed, or pinched between two objects; or an accidental kick or knock from another person.
Statistical analysis was performed with use of SPSS for Windows (version 24; IBM). The Mann–Whitney U-test was used for continuous parameters, and the chi-square test was used for categorical parameters. The level of significance was initially set at p < 0.05, with Bonferroni correction to adjust for multiple testing. For significant multiple group categorical parameters, post-hoc testing was performed to detect differences between groups by calculating the adjusted residual. An adjusted residual that was more than 1.96 was used to indicate significance with a level of 0.05.
An a priori power analysis was performed using G-Power software to approximate the number of patients need to provide a sample of sufficient power. Based on data from Silvani et al, we estimated a medium effect size, d = 0.5.11 Assuming two tails t test with 95% power and alpha = 0.05, a minimum number of 210 patients would be enough to provide a sample of sufficient power.
Results
Distribution of Trauma Activations According to Age and Gender During the COVID-19 Pandemic
A total of 1650 trauma activations registered during the pre-pandemic phase of the COVID-19 pandemic at this trauma center, 691 trauma activations during the initial wave, and 826 during the protracted phase. Trauma activations showed variations in trends according to both gender-related and age-related demographic criteria. There were no statistically significant differences observed for the overall distribution of gender-related or age-related trauma activations when comparing the pre-pandemic period to the initial wave. However, the percentage of pediatric trauma activations and female trauma activations decreased during the protracted phase of the pandemic, while male trauma activations increased (Table 1).
 |
Table 1 Demographics of Patients Involved in Trauma Activations During the Pre-Pandemic Period, Initial Wave, and Protracted Phase of the COVID-19 Pandemic |
Primary Endpoint: Changes in Trauma Activations Stratified by ICD Code During the COVID-19 Pandemic
The primary endpoint of this study concerned changes in trauma activations categorized by ICD-10 codes, which were found to vary disproportionately: gunshot wounds (GSW), motorcycle collisions (MCC), and blunt force injuries caused by an object (strike injuries) were found to increase during the initial wave of the pandemic, while pedestrian injuries were found to decrease (Table 2). The percent increase in GSWs during the initial wave was significant, with 18 patients (2.6%) treated for GSWs during this period, 16 patients (1.9%) treated during the protracted phase compared to 19 patients (1.2%) treated during the entirety of the pre-pandemic period (p-value <0.05) (Table 3). Similarly, the percent increase in MCCs during the initial wave was found to be statistically significant with 29 collisions (4.2%) during the initial wave, 15 collisions (1.8%) during the protracted phase and 33 collisions (2.0%) during the entirety of the pre-pandemic period (p-value <0.001) (Table 2). After secondary analysis of MCCs stratified by gender during the initial wave, this increase was determined to exist predominantly in males as opposed to females (p-value <0.01) (Table 3). Lastly, the percent increase in strike injuries resulting in trauma activations during the initial wave was significant, with 19 patients (2.7%) treated for strike injuries during this period, 12 patients (1.7%) treated during the protracted phase and 22 patients (1.3%) treated during the entirety of the pre-pandemic period (p-value <0.05) (Table 2). After secondary analysis of strike injury trauma activations stratified by gender and age during the initial wave, these injuries were disproportionately observed in males as opposed to females (p-value <0.01) (Table 3) and these injuries were largely seen in patients between the age of 18–64 years (Table 4).
 |
Table 2 Mechanism of Injury for Trauma Activations During the Pre-Pandemic Period, Initial Wave and Protracted Phase of the COVID-19 Pandemic |
 |
Table 3 Mechanism of Injury for Trauma Activations During the Pre-Pandemic Period, Initial Wave, and Protracted Phase of the COVID-19 Pandemic Stratified by Gender |
 |
Table 4 Mechanism of Injury for Trauma Activations During the Pre-Pandemic Period, Initial Wave, and Protracted Phase of the COVID-19 Pandemic Stratified by Age |
Overall, the only trauma activation found to decrease during the initial wave of the pandemic was secondary to pedestrian injuries, with 19 activations (2.7%) during the initial wave, compared to 48 activations (5.8%) during the protracted phase and 104 activations (6.3%) during the pre-pandemic phase (p-value <0.001) (Table 2). Upon secondary analysis of pedestrian trauma activations stratified by both gender and age during the initial wave, this decrease was found to be similar across both males and females (Table 3) but was found to disproportionately affect patients 18–64 years old (Table 4).
No statistically significant changes were observed concerning self-harm, sports injuries, bike accidents, or motor vehicle accidents (Table 2). However, secondary analysis of assault injuries stratified by age and gender demonstrated a statistically significant percent decrease in the number of both female and pediatric assault trauma activations during both the acute and protracted phase of the pandemic. Female assault activations in the pre-pandemic period totaled 38 (5.64%), decreased to 8 (2.93%) during the initial wave and 7 (2.33%) during the protracted phase of the pandemic (p-value <0.01) (Table 3). Similarly, there was a significant decrease in the number of pediatric assault activations with only 2 (3.30%) registered during the initial wave and 2 (3.64%) during the protracted phase, as compared to 21 activations (12.9%) during the pre-pandemic phase (p-value <0.001) (Table 4).
Secondary Endpoints: Changes in Trauma Activations, Hospital Admissions, and ICU Stays During the COVID-19 Pandemic
The secondary endpoints of this study concerned changes in trauma activation categories, admissions to inpatient services, and the length of stay for patients transferred to the ICU during the acute and protracted phases of the COVID-19 pandemic. Compared to pre-pandemic numbers, Level 1 trauma activations remained unchanged throughout the acute and protracted phases of the pandemic (Table 5). However, Level 2 trauma activations and episodes resulting in no activation status decreased during the initial wave, while Level 3 trauma activations increased (trauma consultation). Specifically, Level 2 trauma activations decreased from 1032 activations (62.55%) during the pre-pandemic period to 386 activations (55.86%) during the initial wave and then returned to 512 activations (61.99%) during the protracted phase (p-value <0.001). Level 3 activations significantly increased from 387 consultations (23.45%) during the pre-pandemic phase to 203 consultations (29.38%) during the initial wave and returned to 177 consultations (21.43%) during the protracted phase (p-value <0.001) (Table 5).
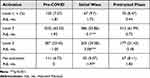 |
Table 5 Trauma Activation Levels During the Pre-Pandemic Period, the Initial Wave and Protracted Phases of the Pandemic |
Utilization of hospital admission services post-trauma is shown in Table 6. Overall, inpatient hospital admissions increased to the internal medicine and orthopedic surgery service during the protracted phase of the pandemic, while admissions decreased to the trauma surgery service. Interestingly, no statistically significant differences were found in the ICU length of stays for patients admitted to the hospital from the trauma center during the acute and protracted phases of the COVID-19 pandemic (Table 7).
 |
Table 6 Inpatient Admission Services from Trauma Activations During the Pre-Pandemic Period, the Initial Wave and Protracted Phases of the Pandemic |
 |
Table 7 ICU Length of Stay from Trauma Activations During the Pre-Pandemic Period, the Initial Wave and Protracted Phases of the Pandemic |
Discussion
Our study aimed to characterize the impact of COVID-19 and the subsequent quarantine policies on trauma activations at a Level 1 Trauma Center in New York City. The COVID-19 pandemic had demonstrable effects on the total volume of patients visiting the Trauma Center. Overall, we saw a decrease in trauma patients during the six-month-long initial wave of the pandemic.7,8 This decrease is likely secondary to social distancing measures and reduced attendance to emergency departments as patients avoided medical treatment during the pandemic.12,13
One interesting finding in our study was a 70% decrease in pediatric assault activations in the initial wave that persisted into the protracted phase. Similarly, we observed an almost 50% decrease in female assault activations during the same periods. Some research has suggested that decreases in trauma activations and hospitalizations may be attributed to a decrease incidence of injuries due to social distancing and quarantining.5 However, as previously mentioned, the decrease in trauma activations may not actually reflect decreased incidence of injuries but a rather deliberate avoidance of patients to seek emergency care during the pandemic.6,14 Underreporting assault is well documented across the literature as other researchers have expressed concerns that the pandemic and quarantine orders led to more assault trauma victims to remain at home with their injuries, which is of particular concern for women and children.15 However, the overall presumption of avoidance of care during the pandemic conflicts with other studies, which found a marked increase in the proportion of injuries, burns and wounds because the home environment is a frequent nidus for accidents.16 Interestingly, this study observed a significant increase in male trauma activations during the protracted phase. This rise in male trauma activations during the protracted phase may be secondary to the lifting of restrictions, leading males to eagerly resume daily activities and escape the confines of home.
The initial wave of the COVID-19 pandemic had varying effects on the number of trauma patients presenting with specific mechanisms of injuries. Of note, our study observed an increase in gunshot wounds during the initial wave of the pandemic. Similarly, gunshot wounds and penetrating traumas were found to increase in a multicenter retrospective analysis of trauma patients presenting to 11 American College of Surgeons Level I and II trauma centers, spanning seven counties in California.15 Specifically, our study demonstrated that these gunshot victims were predominantly male. It is important to note that this increase in gunshot wounds may be a uniquely American problem, as gun sales reached an all-time high during the pandemic.17,18 Similarly, our study found an increase in strike victims, specifically in males 18–65 years old, during the initial wave of the pandemic. While our study initially demonstrated no significant change in trauma activations secondary to stabbings overall, after stratifying the data by age, a significant increase in stabbings was observed in the 18–65 age group. Importantly, this escalation in violent trauma has been well documented in other studies.4,13,15 Of note, lockdown orders may have exacerbated certain personal issues as people were forced to spend more time inside and many people underwent financial stressors due to job loss during the pandemic. It is important to realize that as various personal stressors increase, so does the propensity for violence, which has been well documented.18 Our study also demonstrated a decrease in trauma activations secondary to pedestrian injury during the initial wave, which has been supported by other studies. As many people remained home during the initial wave of the pandemic, there was less opportunity for pedestrian injury.19 This reduction was likely connected to the city-wide shutdown that occurred during the pandemic, which resulted in significantly less pedestrian activity in New York City. This decrease was specific to the 18–65-year-old age group across both genders, while pediatric and elderly pedestrian trauma activations demonstrated no significant changes. In the protracted phase of the pandemic, the number of female trauma activations secondary to falls increased, which may be secondary to resumption of a more active lifestyle.
Interestingly, there was no significant change in motor vehicle collision trauma patients. We originally hypothesized that MVCs would likely decrease secondary to people working from home, thereby no longer commuting to work.20 Another unique finding from our study was a 50% increase in motorcycle collisions in male patients during the initial wave. Although no such findings have been demonstrated so far in the literature,21,22 this trend was consistent with data from our area.23,24 A report from the Institute for Traffic Safety Management and Research demonstrated that fatal motorcycle accidents in New York State increased more than 30% in 2020 compared to 2019 despite a decrease in road traffic.23 Additionally, in 2020, men accounted for 90% of all city car accidents, an increase from around 78% during previous years.24 New York City officials postulated that the surge in motor vehicle deaths occurred due to the pandemic’s emptying effect on streets, which led to less traffic, more speeding, and other unsafe driving behaviors.24 Interestingly, our study observed no changes in sports-related trauma activations, though many sports leagues and activities were cancelled during the pandemic. However, this consistent rate of sport trauma injuries may reflect people trying new outdoor, socially distanced activities that compensated for the loss of organized sports. Of note, while some literature has shown a higher incidence of anxiety and depression during the COVID-19 pandemic, our data showed no change in trauma activations secondary to self-harm.25 It was posited that the increased incidence of depression and anxiety may lead to increased self-harm, but this trend was not witnessed at our trauma center.
In terms of trauma classifications, activations in the initial wave were significantly affected in each category, except Level 1 traumas. One may argue that the decrease in Level 2 trauma activations was the result of increased quarantine measures, which may have prevented opportunities for patients to sustain injuries.7,8,26 Level 3 activations, the trauma activation designated to the most stable patients, increased significantly. This may reflect the inability of patients to visit their primary care doctors. During the pandemic, many primary care physicians retired and most offices were not seeing patients in person, as such these physicians often referred patients to their local Emergency Department for minor injuries that did not require emergent treatment.10
With respect to inpatient admissions of trauma patients, our study found a significant increase in patients admitted to the internal medicine service during the protracted phase of the pandemic. This trend may demonstrate a phenomenon in which patients may have missed routine healthcare appointments during the pandemic, but when these patients suffered a trauma, they were found to require additional medical treatment.10 Similarly, we found a marked increase of orthopedic admissions during the protracted phase of the pandemic and a relative decrease in the initial wave when compared to the prior year. These findings are consistent with an Australian study that observed a 15.6% decrease in orthopedic surgery from March to April of 2020 compared to the previous year.20 Interestingly, our study found no significant changes in the length of stay for trauma patients admitted to the intensive care unit during the COVID-19 pandemic. During the pandemic, ICU beds became scarce as severely afflicted COVID-19 patients required ventilatory support. Due to the infectivity of the virus, it was hypothesized that the ICU length of stay would likely increase for trauma patients due to the possibility of concurrent COVID-19 infection. However, we found no such data to support this theory.
Overall, our study may guide trauma centers as to how to prepare for future pandemics. Certain injuries that may be expected to increase could include gunshot wounds, motorcycle collisions, and strike injuries. Our study hopes to inform trauma centers to plan accordingly for these types of injuries and to prepare trauma bays as necessary. However, our study has many limitations. First, our findings are limited to the data of only one trauma center during the COVID-19 pandemic, which may prevent this study from elucidating generalizable conclusions to other trauma centers. Future research studies may benefit from analyzing the pandemic data from multiple trauma centers during the COVID-19 pandemic. Secondly, not all mechanisms of injury could be deduced from the EMR system, and few patients were categorized as “unknown”. However, in light of the large sample size and power of our study, we hope that this helps shape preparedness for future pandemics.
Conclusions
In conclusion, our study revealed significant changes in trauma service utilization during the COVID-19 pandemic, revealing distinguishing characteristics across both gender and age. During the initial wave of the pandemic, we reported an increase in gunshot trauma and strike victims. Trauma centers should expect similar trends in violent trauma in future pandemics. One of the measures trauma centers should be prepared to implement in future pandemic is increased resources for a trauma center’s critical care units as the penetrating trauma has shown to consistently increase in trauma centers nationally. We also emphasize the need to implement strategies to raise public awareness of assault in the domestic setting, particularly during a mandatory stay-at-home policy. Increased outreach and social services could aid in this effort. This study aids in understanding how a global pandemic and subsequent lockdown policies contribute to trauma service utilization. This information can be utilized for future resource allocation and for trauma prevention during future pandemics.
Disclosure
The authors declare no conflicts of interest in this work.
References
1. Department of Health and Mental Hygiene (DOHMH). Covid-19 daily counts of cases, hospitalizations, and deaths: NYC open data. NYC Open Data; November 13, 2021. Available from: https://data.cityofnewyork.us/Health/COVID-19-Daily-Counts-of-Cases-Hospitalizations-an/rc75-m7u3.
2. Kerr A. Timeline: How Covid-19 took over NYC. Investopedia; April 5, 2021. Available from: https://www.investopedia.com/historical-timeline-of-covid-19-in-new-york-city-5071986.
3. Chiba H, Lewis M, Benjamin ER, et al. “Safer at home”: the effect of the COVID-19 lockdown on epidemiology, resource utilization, and outcomes at a large urban trauma center. J Trauma Acute Care Surg. 2021;90(4):708–713. doi:10.1097/TA.0000000000003061
4. Navsaria PH, Nicol AJ, Parry CDH, Matzopoulos R, Maqungo S, Gaudin R. The effect of lockdown on intentional and nonintentional injury during the COVID-19 pandemic in Cape Town, South Africa: a preliminary report. S Afr Med J. 2020;111:110–113.
5. Graham-Harrison E, Giuffrida A, Smith H, Ford L. Lockdowns around the world bring rise in domestic violence. Guardian; March 28, 2020. Available from: https://www.theguardian.com/society/2020/mar/28/lockdowns-world-rise-domestic-violence.
6. Gupta A, Stahl A. For abused women, a pandemic lockdown holds dangers of its own. New York Times; March 24, 2020. Available from: https://www.nytimes.com/2020/03/24/us/coronavirus-lockdown-domestic-violence.html.
7. Nuñez JH, Sallent A, Lakhani K, et al. Impact of the COVID-19 pandemic on an emergency Traumatology service: experience at a tertiary trauma centre in Spain. Injury. 2020;51(7):1414–1418. doi:10.1016/j.injury.2020.05.016
8. Park C, Sugand K, Nathwani D, Bhattacharya R, Sarraf KM. Impact of the COVID-19 pandemic on orthopedic trauma workload in a London level 1 trauma center: the “golden month”. Acta Orthop. 2020;91(5):556–561. doi:10.1080/17453674.2020.1783621
9. Salottolo K, Caiafa R, Mueller J, et al. Multicenter study of US trauma centers examining the effect of the COVID-19 pandemic on injury causes, diagnoses and procedures. Trauma Surg Acute Care Open. 2021;6(1):e000655. doi:10.1136/tsaco-2020-000655
10. Dopfer C, Wetzke M, Zychlinsky Scharff A, et al. COVID-19 related reduction in pediatric emergency healthcare utilization - A concerning trend. BMC Pediatr. 2020;20(1):427. doi:10.1186/s12887-020-02303-6
11. Silvagni D, Baggio L, Meragliotta LT, et al. Neonatal and pediatric emergency room visits in a tertiary center during the COVID-19 pandemic in Italy. Pediatr Rep. 2021;13(2):168–176. doi:10.3390/pediatric13020023
12. Pines JM, Zocchi MS, Black BS; US Acute Care Solutions Research Group, et al. Characterizing pediatric emergency department visits during the COVID-19 pandemic. Am J Emerg Med. 41;2021:201–204. doi:10.1016/j.ajem.2020.11.037
13. Sephton BM, Mahapatra P, Shenouda M, et al. The effect of COVID-19 on a major trauma network. An analysis of mechanism of injury pattern, referral load and operative case-mix. Injury. 2021;52(3):395–401. doi:10.1016/j.injury.2021.02.035
14. Roesch E, Amin A, Gupta J, García-Moreno C. Violence against women during covid-19 pandemic restrictions. BMJ. 2020;369:m1712. doi:10.1136/bmj.m1712
15. Yeates EO, Grigorian A, Barrios C, et al. Changes in traumatic mechanisms of injury in Southern California related to COVID-19: penetrating trauma as a second pandemic. J Trauma Acute Care Surg. 2021;90(4):714–721. doi:10.1097/TA.0000000000003068
16. Sutherland M, McKenney M, Elkbuli A. Vehicle related injury patterns during the COVID-19 pandemic: what has changed? Am J Emerg Med. 2020;38(9):1710–1714. doi:10.1016/j.ajem.2020.06.006
17. Caputi TL, Ayers JW, Dredze M, Suplina N, Burd-Sharps S. Collateral crises of gun preparation and the COVID-19 pandemic: infodemiology study. JMIR Public Health Surveill. 2020;6(2):e19369. doi:10.2196/19369
18. Sarani B. COVID-19 and firearm injury: a uniquely American problem. J Am Coll Surg. 2021;232(2):168–169. doi:10.1016/j.jamcollsurg.2020.10.009
19. Sherman WF, Khadra HS, Kale NN, Wu VJ, Gladden PB, Lee OC. How did the number and type of injuries in patients presenting to a regional level I trauma center change during the COVID-19 pandemic with a stay-at-home order? Clin Orthop Relat Res. 2021;479(2):266–275. doi:10.1097/CORR.0000000000001484
20. Probert AC, Sivakumar BS, An V, et al. Impact of COVID-19-related social restrictions on orthopaedic trauma in a level 1 trauma centre in Sydney: the first wave. ANZ J Surg. 2021;91(1–2):68–72. doi:10.1111/ans.16375
21. Huang W, Lin Q, Xu F, Chen D. Effect of COVID-19 on epidemiological characteristics of road traffic injuries in Suzhou: a retrospective study. BMC Emerg Med. 2021;21(1):88. doi:10.1186/s12873-021-00483-7
22. Sedain B, Pant PR. Road traffic injuries in Nepal during COVID-19 lockdown. F1000Res. 2020;9:1209. doi:10.12688/f1000research.26281.2
23. The INSTITUTE FOR TRAFFIC SAFETY MANAGEMENT and Research (ITSMR) Report “New York state fact sheet on motorcycle crashes 2016–2020”. Available from: https://www.itsmr.org/wp-content/uploads/2022/01/Motorcycle-2016-2020-Nov-2021-POLICE-REPORTED.pdf.
24. Meyer D. NYC motorcycle, car deaths spiked in deadly 2020. The New York Post; January 1, 2021Available from: https://nypost.com/2021/01/01/motorcycle-driver-deaths-spike-in-nyc-streets/.
25. Hay D, Jamal MS, Al-Tawil K, et al. The effect of the COVID-19 pandemic on mental health associated trauma, admissions and fractures at a London major trauma centre. Ann R Coll Surg Engl. 2021;103(2):114–119. doi:10.1308/rcsann.2020.7026
26. van Aert GJJ, van der Laan L, Boonman-de Winter LJM, et al. Effect of the COVID-19 pandemic during the first lockdown in the Netherlands on the number of trauma-related admissions, trauma severity and treatment: the results of a retrospective cohort study in a level 2 trauma centre. BMJ Open. 2021;11(2):e045015. doi:10.1136/bmjopen-2020-045015
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
