Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 10 » Issue 1
Impact of roflumilast on exacerbations of COPD, health care utilization, and costs in a predominantly elderly Medicare Advantage population
Authors Moll K, Sun S, Ellis J, Howe A, Amin A
Received 11 December 2014
Accepted for publication 10 February 2015
Published 16 March 2015 Volume 2015:10(1) Pages 565—576
DOI https://doi.org/10.2147/COPD.S79025
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Richard Russell
Keran Moll,1 Shawn X Sun,2 Jeffrey J Ellis,1 Andrew Howe,1 Alpesh Amin3
1Comprehensive Health Insights, Inc., Humana, Louisville, KY, USA; 2Health Economics and Outcomes Research, Forest Laboratories, LLC, an affiliate of Actavis, Inc., Jersey City, NJ, USA; 3Department of Medicine, University of California-Irvine, Orange, CA, USA
Background: Chronic obstructive pulmonary disease (COPD) exacerbations are associated with declining lung function and health-related quality of life, and increased hospitalization and mortality. Clinical trials often poorly represent the elderly and thus have only partial applicability to their clinical care.
Objective: To compare exacerbations, COPD-related health care utilization (HCU), and costs in a predominantly elderly Medicare COPD population initiated on roflumilast versus those not initiated on roflumilast.
Methods: Deidentified administrative claims data from a large, national payer were utilized. Medicare patients aged 40–89 years with at least one COPD diagnosis from May 1, 2010 to December 31, 2012 were included. Members with at least one roflumilast pharmacy claim (index) were assigned to the roflumilast group and those without were assigned to the non-roflumilast group. Proxy index dates for the non-roflumilast group were randomly assigned for similar distribution of all patients’ time at risk. Subjects with at least one pre-index COPD exacerbation had to be continuously enrolled for ≥365 days pre-index and post-index. Unadjusted and adjusted difference-in-difference (DID) analyses contrasted pre-index with post-index changes in exacerbations, HCU, and costs of roflumilast treatment compared with non-roflumilast treatment.
Results: A total of 500 roflumilast and 60,145 non-roflumilast patients were included (mean age 69.7 and 72.3 years, respectively; P<0.0001). Unadjusted DID favored roflumilast for all exacerbations, with greater pre-index to post-index reductions in mean per 30-day COPD-related hospitalizations (-0.0182 versus -0.0013, P=0.009), outpatient visits (-0.2500 versus -0.0606, P<0.0001), and COPD-related inpatient costs (-US$141 versus -US$11, P=0.0346) and outpatient costs (-US$31 versus -US$4, P<0.0001). Multivariate analyses identified significantly improved pre-index to post-index COPD-related total costs (P=0.0005) and total exacerbations (P<0.0001) for the roflumilast group versus non-roflumilast group.
Conclusion: In a predominantly elderly Medicare COPD population, newly initiated roflumilast patients displayed similar or significantly better unadjusted reductions in all exacerbation-related, COPD-related HCU-related, and COPD-related costs outcomes compared with non-roflumilast patients. These analyses also suggest better adjusted COPD-related costs and total exacerbations for roflumilast-initiated patients.
Keywords: COPD, roflumilast, exacerbations, health care utilization, Medicare
Introduction
Chronic obstructive pulmonary disease (COPD) is a progressive disease characterized by persistent airflow limitation, chronic and progressive dyspnea, cough, and sputum production, and is often complicated by exacerbations. COPD-related exacerbations have serious health consequences and are associated with declines in lung function, reduction in health-related quality of life, and hospitalization and mortality.1 The economic impact of exacerbations is evidenced by the cost of COPD exacerbation-related hospitalizations, accounting for the largest share of direct medical costs associated with COPD.2 The elderly COPD population poses an ever more common challenge with regard to diagnosis and treatment.3 COPD is often underdiagnosed in elderly patients due in part to concurrent age-related changes in lung function.4 The increased prevalence of comorbid conditions in the elderly COPD patient can also contribute to the difficulty of diagnosis and treatment selection.3,5,6 Clinical trials upon which new COPD treatments are approved by the US Food and Drug Administration are often poorly representative of the real-world elderly population and thus have only partial applicability to the clinical care of an elderly patient.6
Until recently, therapy for COPD patients of all ages had been guided primarily by airflow limitation and as such provided limited clinical guidance for a disease that is accepted as heterogeneous and complex.7,8 The most recent iteration of the Global Initiative for Chronic Obstructive Lung Disease (GOLD) treatment guidelines allow for patient assessment based not only on forced expiratory volume in one second values, but also patient-specific symptomology and exacerbation history, and assigns patient categorization and treatment according to four groups (A, B, C, and D).9 Current COPD treatment options recommended by the GOLD treatment guidelines to relieve symptoms and prevent exacerbations include smoking cessation, long-term oxygen therapy, inhaled corticosteroids (ICS), oral corticosteroids, bronchodilator therapy, and roflumilast, a phosphodiesterase-4 inhibitor available on the US market.9
Roflumilast is indicated as a treatment option to reduce the risk of exacerbations in patients with severe COPD associated with chronic bronchitis and a history of exacerbations.10 This agent has been shown to reduce exacerbation frequency in patients with severe airflow limitation, history of exacerbations, and chronic cough and sputum,11,12 as would typically be found in the severe group D GOLD classification. While greater sensitivity of elderly patients to roflumilast cannot be explicitly ruled out, no differences in safety or effectiveness have been observed between older and younger clinical trial subjects.10
An assessment of real-world utilization of roflumilast is essential to better understand the characteristics of COPD patients for whom it is prescribed, the appropriateness of its use, and associated outcomes, as measured by health care utilization (HCU) and exacerbation occurrence. To date, there is no description of an elderly COPD population within which roflumilast is being utilized in actual clinical practice. This study endeavored to characterize a predominantly elderly Medicare COPD population initiated on roflumilast and to compare post-initiation outcomes with a population not initiated on roflumilast.
Materials and methods
Study design and subject selection
This retrospective study utilized deidentified health care claims from a large Medicare Advantage Prescription Drug health plan. Medical and pharmacy claims data were extracted from May 1, 2010 to December 31, 2012, and were used to identify potential subjects, to measure baseline characteristics, and to examine the outcomes of interest. Medicare Advantage Prescription Drug plan members between 40 and 89 years of age with at least one COPD diagnosis, as identified by the ICD-9-CM (International Classification of Diseases, Ninth Revision, Clinical Modification) diagnosis codes of 491.x, 492.x, or 496.x, were identified as potential subjects. From this pool of potential subjects, members with at least one pharmacy claim for roflumilast were identified and the first observed roflumilast claim was assigned as the index date. Subjects in the “roflumilast-treated group” were required to have 12 months of continuous pre-index enrollment, 12 months of continuous post-index enrollment, and at least one pre-index COPD exacerbation of any severity (see Table 1 for exacerbation definition algorithm).13,14 The remaining pool of initially identified potential subjects was eligible for inclusion in the “non-roflumilast treated group”. Proxy index dates, based on the distribution of the difference between pre-index exacerbation date and index date of the roflumilast-treated group, were randomly assigned to the non-roflumilast subjects so that the distribution of all non-roflumilast subjects’ time at risk was similar to that in the roflumilast-treated group.15 Once proxy index dates were assigned, continuous enrollment criteria, age requirements at index date, and pre-index exacerbation criteria were applied and the final non-roflumilast-treated group was identified. The research protocol was reviewed and received approval by an independent institutional review board prior to initiation of the study. A waiver of informed consent and a waiver of authorization to use protected health information were granted.
Subject characteristics
Subject enrollment data provided sex, race/ethnicity, low income subsidy status (defined as Medicare beneficiaries with income below 150% of poverty level), and Medicare dual eligibility status. Age was calculated as of the index date. Geographic region was based on the subject’s state of residence on the index date. Comorbidity burden was measured by the Deyo-Charlson Comorbidity Index (DCCI). The DCCI uses 17 categories of comorbidity to calculate a score that reflects the cumulative increased likelihood of 1-year mortality and is based on ICD-9 diagnoses and procedure codes, and their associated weights.16,17 In addition to the DCCI score, other comorbid respiratory conditions of interest were identified by their associated ICD-9-CM codes. These conditions included respiratory tract cancer, cystic fibrosis, fibrosis from tuberculosis, bronchiectasis, pneumoconiosis, pulmonary fibrosis, pulmonary tuberculosis, and pulmonary sarcoidosis.
Pre-index and post-index medication utilization was measured based on pharmacy or J-coded medical claims adjudicated during the respective period. Respiratory-related medication use patterns were measured for the following classes: short-acting β2-agonists, long-acting β-agonists (LABAs), ICS, ICS/LABA combination products, short-acting anticholinergics, long-acting muscarinic antagonists (LAMAs), methylxanthines, and oral or intravenous corticosteroids. The combination regimen of ICS, LABA, and LAMA was also identified for subjects utilizing each of those three classes at least once during the respective period. Lastly, baseline antibiotic use and long-term oxygen use were identified.
Outcomes
The quantity and costs of COPD-related and total inpatient and outpatient services received, including inpatient hospitalizations, emergency room visits, outpatient office visits, and pharmacy claims, were assessed for both the 12-month pre-index and 12-month post-index periods. Medical claim place of service and current procedural terminology (CPT) codes were used to assign inpatient, emergency room, or outpatient office visit utilization and costs. Total pharmacy costs were defined as the sum of plan-paid and member-paid costs associated with all paid pharmacy claims. Total all-cause health care costs were defined as the sum of the respective total medical cost and total pharmacy cost components. All cost calculations included both member-paid and plan-paid components.
The proportion of subjects with inpatient hospitalized exacerbation, emergency room visit exacerbation, an ambulatory exacerbation identified by qualifying diagnosis, or an ambulatory exacerbation identified by qualifying steroid were assessed. Complete operational definitions of each exacerbation type can be found in Table 1. In the event that a patient had multiple exacerbation events and the time between each event was less than 14 days, the exacerbation “episode” would continue until there was a greater than 14-day space without exacerbation. Only the most severe exacerbation type within that episode was recorded. Any exacerbation occurring after that 14-day window would be a separated exacerbation episode. The occurrence of the aforementioned exacerbation types during the pre-index period was also assessed. The total number of exacerbations (any severity excluding those identified by qualifying antibiotic) experienced by each subject for both the pre-index and post-index periods was determined.
Statistical analysis
Members’ baseline demographics, comorbidities, medication used, exacerbations of different severity, HCU, and health care costs were summarized and compared across groups. Post-index exacerbations of different severity, HCU, and health care costs were also summarized and compared. Counts and percentages for categorical variables were calculated. For continuous variables, means and standard deviations were calculated. Bivariate comparisons of baseline characteristics between the roflumilast-treated group and non-roflumilast-treated group were conducted. Chi-square or Fisher’s exact tests and Wilcoxon rank sum tests were used to evaluate the statistical significance of differences in categorical and continuous variables, respectively.
A difference-in-difference (DID) analytic approach was utilized to contrast changes (12 months before versus 12 months after the index date) in HCU, costs, and exacerbations of the roflumilast-treated group compared with non-roflumilast-treated group. The DID analyses were conducted as univariate analyses for all utilization, cost, and exacerbation outcomes and as multivariate analyses for total COPD-related costs, number of total exacerbations, and number of severe exacerbations. For the univariate DID analyses, all utilization, cost, and exacerbation variables were normalized to a “per 30-day” value due to the allowed variance in member post-index follow-up time (at least 1 year). The 12-month pre-index versus 12-month post-index differences in exacerbation, cost, and utilization variables within each group were calculated and then the net differences (the DID) between the groups were determined and compared using a t-test with unequal variances assumed. Multivariate DID analyses were also conducted to adjust for any baseline differences (eg, comorbidities, baseline medication use) between the two cohorts and validate the respective univariate findings. For the multivariate DID analyses, a generalized linear model with a gamma distribution and log link was fitted to model total COPD costs. A generalized linear model with a negative binomial distribution and log link was fitted to model total exacerbations and severe exacerbations. The generalized estimating equation method was used to account for repeated measures of the same member. Several variables were entered into the three models, including index treatment group (roflumilast or non-roflumilast), demographic characteristics, baseline medical conditions, pre-index medication utilization, and pre-index all-cause health care costs. The total COPD costs model also adjusted for differences in baseline number of each exacerbation type.
All analyses of data were conducted using SAS version 9.3 and SAS Enterprise Guide 5.1 (SAS Institute Inc., Cary, NC, USA). The a priori alpha level for all comparative analyses was 0.05 and all statistical tests were two-tailed.
Results
Study populations and baseline characteristics
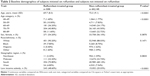
After application of the study inclusion and exclusion criteria, a total of 60,645 Medicare Advantage Prescription Drug members were identified, comprising 500 for the roflumilast-treated group and 60,145 for the non-roflumilast-treated group (Table 2). Significant differences between the roflumilast and non-roflumilast-treated groups were observed for age and low income subsidy. The roflumilast-treated group was younger on average relative to the non-roflumilast-treated group (69.7 versus 72.3 years, P<0.0001). A greater proportion of roflumilast subjects qualified for a low income subsidy relative to non-roflumilast subjects (48.60% versus 25.03%, P<0.0001). No statistically significant differences were observed for sex, race/ethnicity, or geographic region of residence.
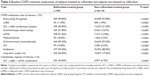
The baseline comorbidities of the study groups are described in Table 3. There was no significant difference between the roflumilast-treated group and the non-roflumilast-treated group in baseline DCCI score (2.62 versus 2.63, respectively, P=0.8569). Relative to the non-roflumilast-treated group, the roflumilast-treated group had a significantly greater prevalence of congestive heart failure (CHF), bronchiectasis, pneumoconiosis, and pulmonary fibrosis. The non-roflumilast-treated group had a greater prevalence of diabetes with complications, renal disease, and metastatic carcinoma.
Significant differences in baseline medication utilization between the roflumilast-treated group and non-roflumilast-treated group were observed across all COPD medication classes and therapy combinations examined (Table 4). Subjects who had been initiated on roflumilast were significantly greater baseline utilizers of COPD medications and therapy combinations compared with their non-roflumilast counterparts. A combination regimen of interest, comprised of ICSs, LABAs, and LAMAs, was used to a far greater extent during the pre-index period by the roflumilast-treated group relative to the non-roflumilast-treated group (50.60% versus 6.75%, respectively, P<0.0001).
Significant differences between the roflumilast-treated group and the non-roflumilast-treated group were observed across all forms of pre-index all-cause and COPD-related HCU, with the roflumilast-treated group exhibiting greater utilization (Table 5). The lone exception was the use of all-cause outpatient services, where there was no difference between groups in the proportion of members with at least one visit in the pre-index period. Roflumilast-treated subjects were far greater utilizers of COPD-related inpatient services during the pre-index period, as measured by members with at least one visit, compared with the non-roflumilast-treated group (40.80% versus 7.89%, respectively, P<0.0001). This finding aligns with more subjects in the roflumilast-treated group experiencing at least one severe pre-index exacerbation (37.40% versus 6.25%, P<0.0001) and having a greater mean number of total pre-index exacerbations (6.02 versus 2.13, P<0.0001) than subjects with a recent exacerbation but not subsequently initiated on roflumilast (Table 5).
Significant differences between the roflumilast-treated group and the non-roflumilast-treated group were observed across the various pre-index all-cause and COPD-related costs, with the roflumilast-treated group exhibiting greater costs (Table 5). Of note, the subjects who initiated roflumilast following an exacerbation had significantly greater pre-index COPD-related inpatient costs ($7,160 versus $960, P<0.0001) and pre-index COPD-related total pharmacy costs ($3,999 versus $714, P<0.0001) compared with subjects who did not initiate roflumilast after a recent exacerbation.
HCU and cost outcomes
The only significant HCU, univariate DID between the roflumilast-treated group and non-roflumilast-treated group was found in the mean number of COPD-related hospitalizations per 30 days and in the mean number of COPD-related outpatient visits per 30 days (Table 6). The results of the univariate DID analyses for changes in all-cause health care costs and in COPD-related health care costs are also presented in Table 6. There were no significant univariate DID comparisons for any of the all-cause health care cost measures. The changes in mean COPD-related inpatient costs per 30 days was significantly different between the two groups (−$130, P=0.0346). The pre-index mean COPD-related inpatient costs for the roflumilast-treated group were $588 per 30 days (rounded to nearest whole dollar) while the post-index COPD-related inpatient costs were $447 per 30 days. This equates to an absolute change (ie, difference) of −$141. The corresponding absolute change for the non-roflumilast-treated group in mean COPD-related inpatient costs was −$11. The DID in these absolute pre-index to post-index changes was significant (P=0.0346) and equal to −$130. Additionally, a significant DID between the roflumilast-treated group and non-roflumilast-treated group was found in outpatient COPD-related costs per 30 days (−$26, P<0.0001). While no significant univariate DID comparison was found for mean total COPD-related costs (−$43, P=0.2580), the multivariate DID analysis did reveal that the covariate-adjusted pre-index to post-index period change in costs for the roflumilast-treated group was significantly different (P=0.0005) and favorable in comparison with the covariate-adjusted change in costs for the non-roflumilast-treated group (parameter estimate, −0.2754; 95% confidence interval [CI], −0.4294, −0.1215).
Exacerbation outcomes
Post-index reductions in mean COPD exacerbations per 30 days were seen for both the roflumilast-treated and non-roflumilast-treated groups (Table 6). The univariate DID analyses revealed that the roflumilast-treated group experienced a significantly greater absolute pre-index to post-index reduction in the following exacerbation types, based on mean number of exacerbations per 30 days: overall exacerbations; severe exacerbations; moderate exacerbations presenting in the emergency room; moderate exacerbations presenting to an outpatient facility; and moderate exacerbations prescribed steroid treatment. The multivariate DID analyses for total number of exacerbations and number of severe exacerbations support the corresponding univariate findings. The covariate-adjusted pre-index to post-index period change in mean number of total exacerbations for the roflumilast-treated group was significantly different (P<0.0001) and favorable in comparison with the covariate-adjusted change in costs for the non-roflumilast-treated group (parameter estimate, −0.1299; 95% CI −0.1930, −0.0669). The covariate-adjusted reduction in mean number of severe exacerbations for the roflumilast-treated group exhibited a borderline significant difference (P=0.0582) and favorable comparison with the covariate-adjusted change in severe exacerbations for the non-roflumilast-treated group (parameter estimate, −0.1801; 95% CI −0.3664, 0.0062).
Discussion
Roflumilast, an anti-inflammatory phosphodiesterase-4 inhibitor, has been shown in clinical trials to reduce exacerbation rates and improve lung function in patients with COPD.11,12,18 A post hoc analysis revealed that the mean annual exacerbation rate in patients with very severe COPD (GOLD stage IV) a mean age of 65 years, and treated with roflumilast was 36% lower than in patients treated with placebo (1.01 versus 1.59 mean exacerbations per year, respectively, P=0.024).19 Further, a post hoc analysis of patients with GOLD stage III–IV disease found that treatment with roflumilast shifts patients from a baseline frequent exacerbator state (defined as two or more events per year) to a less frequent exacerbation state (zero or one events).20 While the necessity of targeting roflumilast to subgroups of COPD patients with a greater likelihood of treatment benefit is evident,21 there is little information regarding the use of roflumilast in actual clinical practice. In this study, the authors examined the baseline characteristics of a predominantly elderly Medicare beneficiary population with at least one exacerbation in the year prior to roflumilast initiation. Patient characteristics, 12-month post-initiation HCU, costs, and exacerbation occurrence in this roflumilast population were contrasted with a non-roflumilast population also with a recent exacerbation.
Several key findings are noted when contrasting the post-initiation HCU, costs, and exacerbation occurrence of the roflumilast-treated group with the non-roflumilast-treated group. Mean 30-day, all-cause total health care costs decreased post-index for both the roflumilast-treated and non-roflumilast-treated groups. However, there were no significant DID comparisons for any of the all-cause health care cost measures. Similarly, while within-group decreases in all-cause HCU were observed for both the roflumilast-treated group and the non-roflumilast-treated group, no significant DID comparisons for any of the all-cause utilization measures were identified. Conversely, mean COPD-related inpatient hospitalizations per 30 days and COPD-related outpatient visits per 30 days displayed a significant DID favorable to the roflumilast-treated group. For example, in the roflumilast-treated group, the pre-index mean number of COPD-related outpatient visits per 30 days was 0.7575 (approximately one visits per 40 days) while the post-index mean per 30 days was 0.5075 (approximately one visits per 60 days). This equates to an absolute change (ie, difference) of −0.2500, with a negative value indicating clinical improvement. The corresponding absolute change for the non-roflumilast-treated group in mean COPD-related outpatient visits per 30 days was −0.0606. The DID in these absolute pre-index to post-index changes was significant (P<0.0001) and equal to −0.1894 (roflumilast change minus non-roflumilast change), with the negative value favorable to the roflumilast-treated group. The HCU findings align with the only significant DID cost comparisons found, ie, mean 30-day COPD-related inpatient costs and mean 30-day COPD-related outpatient costs.
Post-index reductions in mean COPD exacerbations per 30 days, of all severities, were seen for both the roflumilast-treated and non-roflumilast-treated groups. The roflumilast-treated group experienced a significantly greater absolute pre-index to post-index reduction in all exacerbation types, with the exception of those defined by antibiotic use. For example, in the roflumilast-treated group, the pre-index mean number of overall exacerbations per 30 days was 0.4955 (approximately one exacerbation of any severity every 45 days) while the post-index mean per 30 days was 0.3382 (approximately one exacerbation of any severity every 65 days). This equates to an absolute change (ie, difference) of −0.1573, with a negative value indicating clinical improvement. The corresponding absolute change for the non-roflumilast-treated group in mean number of overall exacerbations per 30 days was −0.0538. The DID in these absolute pre-index to post-index changes was significant (P<0.0001) and equal to −0.1035 (roflumilast change minus non-roflumilast change), with the negative value favorable to roflumilast. This finding, as with the utilization and cost findings, is tempered by the likelihood that the non-roflumilast-treated group had less severe COPD relative to the roflumilast-treated group and any post-index change in therapy amongst the non-roflumilast-treated group was not assessed. However, the desired directional decrease in the majority of exacerbation types for the roflumilast-treated group was observed and in accordance with previous findings in severe to very severe COPD patients initiated on roflumilast.18,20
An inherent challenge in retrospective administrative claims analysis of roflumilast use, and comparative effectiveness research in general,22 is the difficulty in identifying an appropriate comparator group. This challenge is reflected in the lack of peer-reviewed, retrospective, administrative claims-based cost studies comparing roflumilast with different treatment regimens. Published economic evaluations of roflumilast are model-based23–25 or were conducted in parallel with prospective clinical trials.26 This challenge applies to the aforementioned univariate analyses of the present study and manifests in two ways, ie, determination of and comparator group selection by COPD severity and comorbidity burden. While administrative claims can provide information on key variables indicative of COPD severity, such as severity of baseline exacerbations and frequency and HCU, it cannot provide several variables that are recommended for use in the clinical setting to assign disease severity and guide treatment decisions. Such variables include smoking status, airflow limitations (as measured by forced expiratory volume in one second), and patient-reported outcomes such as symptom frequency and severity, all of which are key variables utilized in the most recent GOLD treatment guidelines.9 Secondly, comparator selection based on similar concomitant disease states, while amenable to administrative claims analyses, is challenging when the treatment group consists of roflumilast-treated, likely severe COPD patients. For example, a higher incidence of CHF was found in the roflumilast-treated group compared with the non-roflumilast-treated group (24.0% versus 17.6%, respectively, P<0.0002). The incidence rate in both groups is similar to findings (11%–52%) in other studies.27 Both CHF and COPD are chronic progressive diseases complicated by exacerbations. CHF may manifest both obstructive and restrictive ventilatory defects, thereby amplifying or masking the characteristic airflow limitation of COPD.27 The favorability in COPD-related outcome measures, relative to the all-cause outcome measures, for roflumilast treatment compared with non-roflumilast treatment as found in the univariate DID analyses may be due to the presence of comorbid conditions, such as CHF, that independently require high levels of HCU and costs.28
With the aforementioned challenge in mind and in an effort to validate the univariate DID findings, multivariate models adjusted for pre-index concomitant disease (eg, CHF) and available COPD severity markers (eg, use of inhaled steroids, oxygen therapy), as well as other baseline covariates, were applied to total COPD-related costs, number of total exacerbations, and number of severe exacerbations. The multivariate DID models largely validated the corresponding univariate analyses of these three outcome measures, because the roflumilast-treated group in comparison with the non-roflumilast-treated group exhibited a statistically significant (P<0.0001) greater pre-index to post-index decrease in number of total exacerbations and a borderline statistically significant (P=0.0582) greater pre-index to post-index decrease in number of severe exacerbations. While the univariate DID found no significant difference in COPD-related costs between the two groups, the multivariate DID exhibited a statistically significant (P=0.0005) greater pre-index to post-index decrease for the roflumilast-treated group compared with the non-roflumilast-treated group. The multivariate DID findings, combined with the univariate findings, of this real-world roflumilast utilization and COPD outcomes study align with prior clinical trial-based studies that found roflumilast to significantly decrease COPD exacerbations11,12,18 and health care costs.26 This study also substantiates other real-world studies utilizing administrative claims data that have shown roflumilast to either significantly decrease29,30 or trend toward a significant decrease31 in exacerbations, health care costs, or HCU. The value of these findings for health care decision-makers lies in the ability to discern changes in COPD resource utilization and costs compared with overall HCU and costs. Further, these findings provide further insight into the beneficial impact of roflumilast in a predominantly elderly population with severe COPD. Ongoing clinical trials will further assess the benefits of roflumilast, as an addition to other standards of therapy, in patients with severe COPD and frequent exacerbations.32
Several limitations to this study, in addition to those already discussed, are worth noting. While multivariate regression modeling was utilized to reduce selection bias or strengthen any causal inferences, its ability to do so is limited to the covariates included in the model. As with all claims-based studies, the validity of subject identification and diagnostic classification, as well as the identification of disease-related utilization and costs, may be impacted by provider, region, or site-specific coding practices.
Conclusion
This study describes a predominantly elderly Medicare population with recent exacerbation who had been initiated on roflumilast. This population displayed several baseline characteristics that coincide with a severe COPD population including, but not limited to, a high utilization rate of ICS/LABA/LAMA combination therapy, frequent hospitalizations, and frequent exacerbations. Univariate analyses of 12-month post-initiation of roflumilast revealed decreases in exacerbations and some markers of HCU, notably severe exacerbations requiring hospitalization. Multivariate analyses identified statistically significant improved outcomes for roflumilast patients compared with non-roflumilast patients for COPD-related costs and number of total exacerbations. These findings align with and/or augment prior clinical trials and real-world studies that also found favorable outcomes for roflumilast compared with alternative standards of care. Future research should endeavor to identify methods to combine the robust patient populations found via administrative claims-based research and validated COPD severity assessments found in patient-reported outcomes methodologies, as well as further explore the HCU effects of CHF in patients with COPD.
Acknowledgments
Assistance with editing and formatting of the manuscript for submission by Prescott Medical Communications Group (Chicago, IL, USA) was made possible by funding from Forest Laboratories, LLC, an affiliate of Actavis, Inc. (New York, NY, USA). This research was presented, in part, as a poster at the 2014 American Thoracic Society International Conference in San Diego, CA, USA.
Disclosure
KM, JJE, and AH are employees of Comprehensive Health Insights, Inc., and were paid consultants to Forest Laboratories, LLC, an affiliate of Actavis, Inc., in the development and execution of this study and manuscript. SXS is an employee of Forest Laboratories, LLC, an affiliate of Actavis, Inc., the sponsor of this study. AA was a consultant for Humana, Inc., and did not receive payment for manuscript development. The authors report no other conflicts of interest in this work.
References
Andersson F, Borg S, Jansson SA, et al. The costs of exacerbations in chronic obstructive pulmonary disease (COPD). Respir Med. 2002;96:700–708. | ||
Dalal AA, Christensen L, Liu F, et al. Direct costs of chronic obstructive pulmonary disease among managed care patients. Int J Chron Obstruct Pulmon Dis. 2010;5:341–349. | ||
Albertson TE, Schivo M, Zeki AA, et al. The pharmacological approach to the elderly COPD patient. Drugs Aging. 2013;30:479–502. | ||
Bhatt NY, Wood KL. What defines abnormal lung function in older adults with chronic obstructive pulmonary disease? Drugs Aging. 2008;25:717–728. | ||
Mannino DM, Watt G, Hole D, et al. The natural history of chronic obstructive pulmonary disease. Eur Respir J. 2006;27:627–643. | ||
Incalzi RA, Scarlata S, Pennazza G, et al. Chronic obstructive pulmonary disease in the elderly. Eur J Intern Med. 2014;25:320–328. | ||
Agusti A, Calverley PM, Celli B, et al. Characterisation of COPD heterogeneity in the ECLIPSE group. Respir Res. 2010;11:122. | ||
Wedzicha JA. The heterogeneity of chronic obstructive pulmonary disease. Thorax. 2000;55:631–632. | ||
Global Strategy for the Diagnosis, Management and Prevention of COPD, Global Initiative for Chronic Obstructive Lung Disease (GOLD) 2014. Available from: http://www.goldcopd.org. Accessed January 15, 2014. | ||
Daliresp [package insert]. St Louis, MO, USA: Forest Pharmaceuticals, Inc; 2013. | ||
Calverley PM, Rabe KF, Goehring UM, et al. Roflumilast in symptomatic chronic obstructive pulmonary disease: two randomised clinical trials. Lancet. 2009;374:685–694. | ||
Fabbri LM, Calverley PM, Izquierdo-Alonso JL, et al. Roflumilast in moderate-to-severe chronic obstructive pulmonary disease treated with long-acting bronchodilators: two randomised clinical trials. Lancet. 2009;374:695–703. | ||
Lindenauer PK, Pekow PS, Lahti MC, et al. Association of corticosteroid dose and route of administration with risk of treatment failure in acute exacerbation of chronic obstructive pulmonary disease. JAMA. 2010;303:2359–2367. | ||
Mapel DW, Dutro MP, Marton JP, et al. Identifying and characterizing COPD patients in US managed care. A retrospective, cross-sectional analysis of administrative claims data. BMC Health Serv Res. 2011;11:43. | ||
Harvey R, Drzayich-Jankus D, Mosley D; United Healthcare. Random assignment of proxy event dates to unexposed individuals in observational studies: an automated technique using SAS®. Available from: http://www.mwsug.org/proceedings/2012/PH/MWSUG-2012-PH02.pdf. Accessed February 11, 2015. | ||
Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992;45:613–619. | ||
Klabunde CN, Potosky AL, Legler JM, et al. Development of a comorbidity index using physician claims data. J Clin Epidemiol. 2000;53:1258–1267. | ||
Rabe KF, Bateman ED, O’Donnell D, et al. Roflumilast – an oral anti-inflammatory treatment for chronic obstructive pulmonary disease: a randomized controlled trial. Lancet. 2005;366:563–571. | ||
Calverley PM, Sanchez-Toril F, McIvor A, et al. Effect of 1-year treatment with roflumilast in severe chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2007;176:154–161. | ||
Wedzicha JA, Rabe KF, Martinez FJ, et al. Efficacy of roflumilast in the COPD frequent exacerbator phenotype. Chest. 2013;143:1302–1311. | ||
Rennard SI, Calverley PM, Goehring UM, et al. Reduction of exacerbations by the PDE4 inhibitor roflumilast – the importance of defining different subsets of patients with COPD. Respir Res. 2011;12:18. | ||
Berger ML, Mamdani M, Atkins D, et al. Good research practices for comparative effectiveness research: defining, reporting and interpreting nonrandomized studies of treatment effects using secondary data sources: the ISPOR Good Research Practices for Retrospective Database Analysis Task Force Report – Part I. Value Health. 2009;12:1044–1052. | ||
Sun SX, Marynchenko M, Banerjee R, et al. Cost-effectiveness analysis of roflumilast/tiotropium therapy versus tiotropium monotherapy for treating severe-to-very severe COPD. J Med Econ. 2011;14:805–815. | ||
Hertel N, Kotchie RW, Samyshkin Y, et al. Cost-effectiveness of available treatment options for patients suffering from severe COPD in the UK: a fully incremental analysis. Int J Chron Obstruct Pulmon Dis. 2012;7:183–199. | ||
Samyshkin Y, Kotchie RW, Mörk AC, et al. Cost-effectiveness of roflumilast as an add-on treatment to long-acting bronchodilators in the treatment of COPD associated with chronic bronchitis in the United Kingdom. Eur J Health Econ. 2014;15:69–82. | ||
Rutten-van Mölken MP, van Nooten FE, Lindemann M, et al. A 1-year prospective cost-effectiveness analysis of roflumilast for the treatment of patients with severe chronic obstructive pulmonary disease. Pharmacoeconomics. 2007;25:695–711. | ||
Hawkins NM, Petrie MC, Jhund PS, et al. Heart failure and chronic obstructive pulmonary disease: diagnostic pitfalls and epidemiology. Eur J Heart Fail. 2009;11:130–139. | ||
Chatila WM, Thomashow BM, Minai OA, et al. Comorbidities in chronic obstructive pulmonary disease. Proc Am Thorac Soc. 2008;5:549–555. | ||
Wan Y, Shorr A, Sun S, et al. Impact of roflumilast on exacerbations among patients with chronic obstructive pulmonary disease (COPD) in the real world. Chest. 2013;144:745A. | ||
Fu A, Sun S, Huang X, et al. 30-Day readmission rate associated with roflumilast treatment among patients hospitalized for COPD. Chest. 2013;144:744A. | ||
Jain R, Cai Q, Sun SX, et al. Impact of roflumilast treatment on health care utilizations and costs among COPD patients in a managed care population. J Manag Care Pharm. 2014;20:S36. | ||
Calverley PM, Martinez FJ, Fabbri LM, et al. Does roflumilast decrease exacerbations in severe COPD patients not controlled by inhaled combination therapy? The REACT study protocol. Int J Chron Obstruct Pulmon Dis. 2012;7:375–382. |
 © 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.