Back to Journals » Drug Design, Development and Therapy » Volume 16
Impact of Remdesivir on SARS-CoV-2 Clearance in a Real-Life Setting: A Matched-Cohort Study
Authors Spagnuolo V , Voarino M, Tonelli M , Galli L , Poli A, Bruzzesi E, Racca S, Clementi N , Oltolini C, Tresoldi M, Rovere Querini P, Dagna L , Zangrillo A, Ciceri F, Clementi M, Castagna A
Received 5 April 2022
Accepted for publication 26 July 2022
Published 19 October 2022 Volume 2022:16 Pages 3645—3654
DOI https://doi.org/10.2147/DDDT.S369473
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Professor Anastasios Lymperopoulos
Vincenzo Spagnuolo,1 Marta Voarino,2 Marco Tonelli,2,3 Laura Galli,1 Andrea Poli,1 Elena Bruzzesi,2 Sara Racca,3 Nicola Clementi,2,3 Chiara Oltolini,1 Moreno Tresoldi,4 Patrizia Rovere Querini,2,5 Lorenzo Dagna,2,6 Alberto Zangrillo,2,7 Fabio Ciceri,2,8 Massimo Clementi,2,3 Antonella Castagna1,2 On behalf of the COVID-BioB Study Group
1Unit of Infectious Diseases, Istituto di Ricovero e Cura a Carattere Scientifico (IRCCS), San Raffaele Scientific Institute, Milan, Italy; 2Faculty of Medicine and Surgery, Vita-Salute San Raffaele University, Milan, Italy; 3Unit of Microbiology and Virology, IRCCS San Raffaele Scientific Institute, Milan, Italy; 4General Medicine and Advanced Care Unit, IRCCS San Raffaele Scientific Institute, Milan, Italy; 5Internal Medicine, Diabetes, and Endocrinology Unit, IRCCS San Raffaele Scientific Institute, Milan, Italy; 6Unit of Immunology, Rheumatology, Allergy and Rare Diseases, IRCCS San Raffaele Scientific Institute, Milan, Italy; 7Anesthesia and Intensive Care Department, IRCCS San Raffaele Scientific Institute, Milan, Italy; 8Hematology and Bone Marrow Transplant Unit, IRCCS San Raffaele Scientific Institute, Milan, Italy
Correspondence: Vincenzo Spagnuolo, Unit of Infectious Diseases, Istituto di Ricovero e Cura a Carattere Scientifico (IRCCS), San Raffaele Scientific Institute, Milan, Italy, Tel +390226437907, Fax +390226437903, Email [email protected]
Background: Evidence regarding the impact of remdesivir (RDV) on SARS-CoV-2 viral clearance (VC) is scarce. The aim of this study was to compare VC timing in hospitalized COVID-19 patients who did or did not receive RDV.
Methods: This was a matched-cohort study of patients hospitalized with pneumonia, a SARS-CoV-2-positive nasopharyngeal swab (NPS) at admission, and at least one NPS during follow-up. Patients who received RDV (cases) and those who did not (controls) were matched in a 1:2 ratio by age, sex, and PaO2/FiO2 (P/F) values at admission. NPSs were analyzed using real-time polymerase chain reaction. Time to VC (within 30 days after hospital discharge) was estimated using the Kaplan–Meier curve. A multivariable Cox proportional hazard model was fitted to determine factors associated with VC.
Results: There were 648 patients enrolled in the study (216 cases and 432 controls). VC was observed in 490 patients (75.6%), with a median time of 25 (IQR 16– 34) days. Overall, time to VC was similar between cases and controls (p = 0.519). However, time to VC was different when considering both RDV treatment status and age (p = 0.007). A significant finding was also observed when considering both RDV treatment status and P/F values at admission (p = 0.007). A multivariate analysis showed that VC was associated with a younger age (aHR = 0.990, 95% CI 0.983– 0.998 per every 10-year increase in age; p = 0.009) and a higher baseline P/F ratio (aHR=1.275, 95% CI 1.029– 1.579; p=0.026), but not with RDV treatment status.
Conclusion: Time to VC was similar in cases and controls. However, there was a benefit associated with using RDV in regard to time to VC in younger patients and in those with a P/F ratio ≤ 200 mmHg at hospital admission.
Keywords: COVID-19, remdesivir, SARS-CoV-2, viral clearance
Introduction
Remdesivir (RDV) is a nucleotide prodrug of an adenosine analog. It binds to RNA-dependent RNA polymerase and inhibits viral replication by prematurely terminating RNA transcription.1 RDV is active in vitro against a broad spectrum of different viruses including Ebola, severe acute respiratory syndrome coronavirus (SARS-CoV), Middle East respiratory syndrome-related coronavirus (MERS-CoV), and SARS-CoV-2.2–4 In particular, different preclinical studies have demonstrated the efficacy of RDV in blocking SARS-CoV-2 infection in human cells and animal models.3,5,6
Currently, RDV is the only antiviral drug approved by both the European Medicines Agency and the Food and Drug Administration for the treatment of hospitalized coronavirus disease-19 (COVID-19) patients.7,8 However, the efficacy of RDV as a therapeutic agent for severe COVID-19 is still in question;9 although, the early use of RDV in non-hospitalized patients at high-risk of disease progression has been associated with a significantly lower risk of hospitalization or death.10 In hospitalized patients, the first stage of the Adaptive COVID-19 Treatment Trial (ACCT-1)11 indicated that the use of RDV was associated with a reduced time to recovery, a reduced risk of clinical progression, and improved mortality in patients on low-flow oxygen. Other studies have also provided evidence relative to the efficacy and safety of RDV for the treatment of COVID-19.12–17
In contrast, the SOLIDARITY and DisCoVeRy trials18,19 did not find a significant effect of RDV on overall mortality, the initiation of ventilation, or hospital-stay duration. It is on this basis that the World Health Organization does not recommend the use of RDV in COVID-19 hospitalized patients.20 In addition, evidence for the effect of RDV on SARS-CoV-2 viral clearance (VC) is scarce and contradictory. Different studies19,21,22 have shown that the use of RDV is not associated with nasopharyngeal viral load changes, while other studies23,24 have demonstrated that RDV treatment was associated with faster viral decay. However, these studies were all characterized by small sample sizes or follow-up periods that did not exceed the hospitalization period. Therefore, this large-sample-size study was conducted to evaluate the effect of RDV on VC timing in COVID-19 hospitalized patients for 1 month following hospital discharge.
Methods
This retrospective, matched-cohort study was conducted at the Istituto di Ricovero e Cura a Carattere Scientifico (IRCCS) San Raffaele (Milan, Italy). San Raffaele Hospital is a tertiary health care center designated as a COVID-19 hub by the Italian health authorities.
Adult patients (≥18 years) with the following characteristics were included in the study: laboratory-confirmed SARS-CoV-2 infection determined by real-time polymerase chain reaction (RT-PCR) on nasopharyngeal swab specimens performed at hospital admission; imaging studies demonstrating the presence of pneumonia (interstitial involvement and/or consolidation seen on chest x-rays or computed tomography scans); hospitalization at San Raffaele Hospital during the timeframe from February 25, 2020 to April 12, 2021; availability of at least one follow-up nasopharyngeal swab (from 5 days after hospitalization to 30 days after discharge). Patients discharged from the hospital with a positive nasopharyngeal swab continued to be followed in our center. The first follow-up nasopharyngeal swab was performed 10–14 days after hospital discharge, and if positive, was repeated every 7–10 days until negative.
Patients who received RDV were cases, while those who did not receive RDV were controls. Cases and controls were matched in a 1:2 ratio according to: age (±5 years), sex, and the arterial partial pressure of oxygen (PaO2)/fraction of inspired oxygen (FiO2) value (± 10 mmHg) on admission. The PaO2/FiO2 (P/F) ratio represents the ratio between PaO2 as determined by arterial blood gas analysis, and the percentage of oxygen supplied (FiO2).
Matching with replacement was used, hence, matches between cases and controls were made regardless of whether the chosen control was already paired with another case. Replacement allows the same patient to be matched more than once, ensuring the best match for each case with control patients and reducing the probability of inappropriate matches.
RDV (Gilead Sciences; GS-5734) was administered intravenously with a loading dose on the first day (200 mg) followed by 100 mg every day for 4 days. Patients treated with a 10-day course of RDV were not included in this analysis. Use of RDV was contraindicated in patients with an estimated glomerular filtration rate <30 mL/min.
Nasopharyngeal swabs collected from patients were submitted to the San Raffaele Scientific Institute Laboratory of Microbiology, Virology and Serology for RT-PCR testing. The laboratory uses the COBAS 6800 system (Roche Diagnostics, Basel, Switzerland). COBAS 6800 amplifies the ORF1a-1b and E genes and has a limit of 100 copies of viral RNA per milliliter of transport media when amplifying gene R and 43 copies/mL when amplifying gene E. The instrument can yield qualitative (positive and negative) and quantitative results. The quantitative results are expressed in cycle threshold (Ct) values. Any Ct value below 40 corresponded to a positive nasopharyngeal swab and values above 40 were considered a negative swab.
This study was a sub-study of the COVID-19 Patients Characterization, Biobank, Treatment Response and Outcome Predictor (COVID-BioB) Study that was approved by the Ethics Committee of San Raffaele Hospital (protocol No. 34/int/2020) and registered on ClinicalTrials.gov (NCT04318366). All patients signed an informed consent form. Our research complied with the Declaration of Helsinki.
Statistical Analyses
Results are reported as medians (interquartile range, IQR) and frequencies (%). The distribution of continuous variables were compared between cases and controls using the Wilcoxon rank-sum test or the chi-square/Fisher’s exact test for categorical variables.
Time to VC by nasopharyngeal swab was estimated using the Kaplan–Meier curve. The curve was then compared with the Log rank test according to some baseline characteristics. Follow-up began at hospital admission (baseline) and ended on the date of the first negative nasopharyngeal swab (within 30 days after discharge), or, in case of no negative swab, at the date of last positive swab or death. There were no competing events.
To account for indication bias associated with RDV treatment, we estimated individual propensities for receipt of RDV treatment (a propensity-score) with the use of a multivariable logistic regression model that included the following independent variables: age, gender, weight, number of comorbidities, PaO2/FiO2, duration of symptoms at hospital admission, concomitant use of biological drugs, concomitant use of steroids, creatinine, alanine aminotransferase, C-reactive protein, and absolute lymphocyte count at hospitalization (> or ≤1 × 109 cells/mm3).
A multivariable Cox proportional hazard model was fitted to determine factors associated with the risk of a negative nasopharyngeal swab. The adjusted hazard ratios (aHRs) with their corresponding 95% confidence intervals (CIs) are reported. The predicted probabilities of RDV treatment (propensity-score) from the logistic regression model were used to calculate the stabilized inverse probability-weighted (IPW) weight. The multivariable Cox model included a priori factors known to have a potential effect on the outcome or on baseline covariates with a p-value <0.05 in the univariable analysis and were analyzed using a stabilized IPW weight. These covariates were fitted as time-fixed and measured at baseline.
The model was stratified according to the time of hospital admission (before and after September 1, 2020). This was done as both RDV cases and controls were distributed differently within the two time periods and to better account for differences in the use of other concomitant treatments (mainly steroids or biological drugs) during the two time periods. The aHRs of negative nasopharyngeal swabs are reported with their corresponding 95% CIs for significant covariates. The assumption of the proportional hazard was examined by use of interactions of the predictors and the function of time and was confirmed for all significant covariates.
For all analyses, two-sided p-values <0.05 were considered statistically significant. All analyses were performed using SAS Software, release 9.4 (SAS Institute, Cary, NC).
Results
In the period from February 25, 2020 to April 12, 2021, data from 1040 hospitalized patients with COVID-19 were recorded in the Covid BioB database (https://covidbiob/covid19/home.php). This study included 648 hospitalized patients who met the inclusion criteria and were successfully matched: 216 cases and 432 controls. The median age was 64 years (54–77), 60.2% were male. Patient characteristics at hospital admission according to RDV treatment status are detailed in Table 1. As cases and controls were matched based on age, sex, and P/F ratio at admission, there was no difference in these characteristics among the two groups. In addition, there were no significant differences between the two groups in terms of prevalence of comorbidities (with the exception of chronic kidney disease) or in body mass index values.
 |
Table 1 Patient Characteristics, Respiratory Function, and Laboratory Values at Admission for Hospitalized COVID-19 Patients, Stratified by Remdesivir Treatment Status |
Patients were admitted to the hospital after a median of 8 (5–11) days from the onset of symptoms: 7 (4–9) days for cases and 8 (5–11) days for controls (p = 0.009). Among the cases, the drug was administered 1 (0–3) day after hospitalization. Only 43 patients (20.9%) started RDV ≤5 days from symptom onset. Length of hospitalization was similar between the two groups, but there were some important differences in COVID-19 therapies, as detailed in Table 2. These findings were related to the different timing of hospitalization between cases and controls. The majority of controls were hospitalized before September 2020 (during “the first wave”) when RDV, corticosteroids, and low molecular weight heparins were not yet recommended by international guidelines.
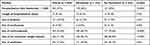 |
Table 2 Characteristics of Hospitalization and Concomitant Pharmacological Therapy That Was Administered to Patients, Stratified by Remdesivir Treatment Status |
Treatment with RDV was well-tolerated. The frequency of acute kidney injury was 1.4% among cases and 1.9% among controls (p = 0.759). Arrhythmias were detected in 3.2% of the cases and 3.3% of the controls (p = 1.000). Cases and controls did not have significantly different transaminases or serum creatinine values.
SARS-CoV-2 Clearance
The median number of nasopharyngeal swabs performed on each patient during follow-up was 8 (4–14). VC within 30 days following discharge was reached by 490 patients (75.6%). Of these 490 patients, 54.7% achieved VC during hospitalization, while the remaining 45.3% reached VC during the post-discharge follow-up period. Median time to VC was 25 (16–34) days.
Overall, time to VC was not significantly different between cases and controls (p = 0.519) (Figure 1A). However, time to VC was different when considering both RDV treatment status and age. The proportion of patients who achieved VC by 40 days following hospitalization was 89.5% among cases aged ≤65 years, 86.7% among controls aged ≤65 years, 74.5% among cases aged >65 years, and 75.6% among controls aged >65 years (p=0.007) (Figure 1B).
A significant finding was also observed when considering both RDV treatment status and P/F values at admission. The proportion of patients who achieved VC by 40 days following hospitalization was 87% among cases with a P/F >200 mmHg, 88.7% among controls with a P/F >200 mmHg, 82.1% among cases with a P/F ≤200 mmHg, and 75.3% among controls with ≤200 mmHg (p = 0.007) (Figure 1C).
Our multivariate analysis showed that a younger age (aHR = 0.990, 95% CI 0.983–0.998 per every 10 years, p = 0.009) and baseline PaO2/FiO2 >200 mmHg (aHR = 1.275, 95% CI 1.029–1.579; p = 0.026) were associated with VC (Table 3). RDV treatment status did not affect VC (aHR = 0.963, CI 0.747–1.241; p = 0.768).
 |
Table 3 Multivariable Cox Proportional Hazard Model: Factors Associated with Viral Clearance |
Among patients who achieved VC during the follow-up period, overall time to VC was similar among cases and controls (p = 0.075) (Figure 2A). However, RDV treatment status was associated with a higher probability of VC among patients with a P/F admission value ≤200 mmHg (p = 0.035) (Figure 2B), age ≤65 years (p = 0.050) (Figure 2C), and patients without comorbidities (p = 0.028) (Figure 2D). Among patients who achieved VC, cases experienced a greater decrease in Ct values than controls (Table 4), although, this finding should be interpreted with caution due to the small number of observations.
 |
Table 4 Cycle Threshold (Ct) Values, Stratified by Remdesivir Treatment Status, in Patients Who Achieved Viral Clearance |
Discussion
In our study, we evaluated the effect of RDV on VC timing in COVID-19 hospitalized patients for 1 month following hospital discharge. We observed that a younger age and a higher PaO2/FiO2 ratio on admission were associated with VC. This is consistent with previous studies that identified older age and disease severity as risk factors for delayed VC.25–28 Zou et al29 showed that the viral RNA shedding pattern of patients with COVID-19 was similar to that of patients with influenza, whereby nasopharyngeal viral clearance was delayed in patients at advanced ages and with more severe forms of disease. In addition, older patients are more often affected by comorbidities. Previous work27 has also shown an association between the presence of comorbidities and slower SARS-CoV-2 clearance. However, RDV treatment status was not associated with VC. Other studies have reported similar findings.19,21,22,30 This could reflect the timing of RDV treatment, which may be administered too late to effectively impact VC. Wong et al31 demonstrated that early remdesivir treatment was associated with a significantly greater increase in Ct values on day 7. In our study, RDV was administered, on average, 8 days after symptom onset with only 43 patients (20.9%) starting it ≤5 days from symptom onset.
It is possible that RDV better exerts its antiviral activity in the lower respiratory tract than in the upper respiratory tract. This has been previously reported in preclinical trials6 where the administration of intravenous or inhaled remdesivir significantly reduced viral burdens in a nonhuman primate model of SARS-CoV-2 infection in both bronchoalveolar lavage fluid and respiratory tract tissues but not in nasal or throat swabs specimens.32 A complicating factor in our study concerned different concomitant therapies between cases and controls. Steroids were administered to more cases than controls. These drugs have been associated with potential delayed VC,33 although this evidence has been questioned by different studies.30,34
Interestingly, there was an observed effect of RDV on VC in some patient subgroups. When we considered use of RDV and either age or respiratory impairment at admission (the two factors with a significant effect on time to VC), we observed significant difference between groups. Younger RDV patients and RDV patients with a P/F at admission of ≤200 mmHg derived more benefits in terms of time to VC. These findings were confirmed when only patients who achieved VC during follow-up were considered. In these patients, treatment with RDV was associated with a decreased time to VC in those with a P/F ≤200 mmHg at admission and ≤65 years of age, when compared to controls. Younger patients have a more efficient immune response compared to older patients.35 In this population characterized by a lower nasopharyngeal viral load and faster viral decay,36 the antiviral activity of RDV may further facilitate VC.
Disease severity has been described as a possible risk factor for delayed VC and higher nasopharyngeal viral loads.37 In these patients, at high risk of clinical progression and delayed VC, our findings may increase the strength of recommendation for the use of RDV treatment.
Strengths and Limitations
The main strengths of this study include the large number of patients who were evaluated and a relatively long follow-up period. However, there are several limitations. First, we cannot exclude a potential selection bias given that included patients needed to have at least two nasopharyngeal swabs. This criterion excluded patients who exhibited a more aggressive disease course and died within a few days of hospital admission. Second, viral sequencing was not routinely performed and, therefore, it was not possible to assess the likely effects of SARS-CoV-2 variants of concern (VOCs) on the timing of VC and RDV efficacy. However, given that RDV targets the highly conserved viral RNA-dependent polymerase, it is likely that RDV maintains efficacy against emerging SARS-CoV-2 VOCs.38 Indeed, recent data has shown that RDV remains active against the SARS-CoV-2 Omicron variant and other VOCSs.39 Third, Ct values and their relative changes were available only for a minority of patients, which may limit the generalizability of our findings. Finally, most controls were hospitalized before September 1, 2020, while most cases were hospitalized afterward this date. To mitigate this discrepancy, the multivariate analysis that assessed the predictive factors for VC was stratified by date of hospitalization (“first wave” and “second wave”).
Conclusions
In conclusion, overall time to VC was not significantly different between patients who received or did not receive RDV treatment. However, the use of RDV was associated with a benefit concerning time-to-VC in patients younger than 65 years of age and in those with a P/F ratio ≤200 mmHg on hospital admission.
COVID-BioB Study Group
Badalucco F1,2,Baiardo Redaelli M7, Baldissera E6, Bigai G2, Boffini N6, Borio G2, Bossolasco S1, Bottanelli M1,2, Calabrò MG7, Calvisi S5, Campochiaro C6, Canetti D1, Canti V3, Castellani J2, Cavalli G2,6, Cavallo L2, Cernuschi M1, Chiurlo M1,2, Cilla M6, Cinel E2, Cinque P1, Clemente T1,2, Conte C2, Da Prat V5, Danise A1, De Lorenzo R2, De Luca G6, Dell’Acqua A6, Dell’Acqua R1, Della Torre E6, Della Torre L1, Di Terlizzi G5, Dumea I2, Farolfi F2, Ferrante M2,5, Frangi C2, Gallina G3, Germinario B2, Gianotti N1, Guffanti M1, Hasson H1, Lalla F2, Landoni G7, Lanzillotta M2, Li Voti R2, Mainardi I1,2, Mancini N2,3, Mastrangelo A1,2, Messina E1, Moizo E7, Monardo R1,2, Montagna M2, Monti G7, Mori G1,2, Morsica G1, Muccini C1,2, Nozza S1, Pascali M2, Papaioannu Borjesson R1,2, Patrizi A5, Pieri M7, Ponta G1,2, Prestifilippo D2, Ramirez G2,6, Ranzenigo M1,2, Ripa M1,2, Sapienza J2, Sartorelli S2,6, Seghi F2, Tassan Din C1, Tomelleri A2,6, Turi S7, Uberti-Foppa C1,2.
All authors listed in the COVID-BioB study group contributed to the collection and review of the data.
Data Sharing Statement
The datasets used and analyzed during this study are available from the corresponding author upon reasonable request.
Acknowledgments
This work was presented in part at the 10th ID Week, Virtual edition, September 29-October 3, 2021. Poster number 505. We would like to thank JournalEdit [https://www.journaledit.com/] for reviewing this manuscript for English language.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This research received a specific grant from Gilead Sciences (Medical Grant 12573). The sponsor had no involvement in the study design, or in the collection, analysis or interpretation of the data, or in the writing of the report.
Disclosure
Dr Vincenzo Spagnuolo reports grants from Gilead Sciences Srl, during the conduct of the study. Dr Chiara Oltolini reports grants from Gilead Sciences, during the conduct of the study. The authors report no other conflicts of interest in this work.
References
1. COVID-19 Treatment Guidelines Panel. Coronavirus disease 2019 (COVID-19) treatment guidelines. National Institutes of Health. Available from: https://www.covid19treatmentguidelines.nih.gov/.
2. Eastman RT, Roth JS, Brimacombe KR, et al. Remdesivir: a review of its discovery and development leading to emergency use authorization for treatment of COVID-19. ACS Cent Sci. 2020;6:672–683. doi:10.1021/acscentsci.0c00489
3. Wang M, Cao R, Zhang L, et al. Remdesivir and chloroquine effectively inhibit the recently emerged novel coronavirus (2019-nCoV) in vitro. Cell Res. 2020;30:269–271. doi:10.1038/s41422-020-0282-0
4. Sheahan TP, Sims AC, Leist SR, et al. Comparative therapeutic efficacy of remdesivir and combination lopinavir, ritonavir, and interferon beta against MERS-CoV. Nat Commun. 2020;11(1):222. doi:10.1038/s41467-019-13940-6
5. Zhou P, Yang XL, Wang XG, et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020;579:270–273. doi:10.1038/s41586-020-2012-7
6. Williamson BN, Feldmann F, Schwarz B, et al. Clinical benefit of remdesivir in rhesus macaques infected with SARS-CoV-2. Nature. 2020;585:273–276. doi:10.1038/s41586-020-2423-5
7. Food and Drug Administration. NDA Approval 214787. Available from: https://www.accessdata.fda.gov/drugsatfda_docs/appletter/2020/214787Orig1s000ltr.pdf.
8. European Medicines Agency. Veklury EPAR Medicine Overview. Available from: https://www.ema.europa.eu/en/documents/overview/veklury-epar-medicine-overview_en.pdf.
9. Gyselinck I, Janssens W. Remdesivir, on the road to DisCoVeRy. Lancet Infect Dis. 2022;22(2):153–155. doi:10.1016/S1473-3099(21)00559-4
10. Gottlieb RL, Vaca CE, Paredes R, et al. Early remdesivir to prevent progression to severe Covid-19 in outpatients. N Engl J Med. 2022;386:305–315. doi:10.1056/NEJMoa2116846
11. Beigel JH, Tomashek KM, Dodd LE, et al. Remdesivir for the Treatment of Covid-19 - Final Report. N Engl J Med. 2020;383:1813–1826. doi:10.1056/NEJMoa2007764
12. Olender SA, Perez KK, Go AS, et al. Remdesivir for severe coronavirus disease 2019 (COVID-19) versus a cohort receiving standard of care. Clin Infect Dis. 2021;73(11):e4166–e4174. doi:10.1093/cid/ciaa1041
13. Lapadula G, Bernasconi DP, Bellani G, et al. Remdesivir-Ria Study Group. Remdesivir use in patients requiring mechanical ventilation due to COVID-19. Open Forum Infect Dis. 2020;7:ofaa481. doi:10.1093/ofid/ofaa481
14. Perveen RA, Nasir M, Talha KA, Selina F, Islam MA. Systematic review on current antiviral therapy in COVID-19 pandemic. Med J Malaysia. 2020;75:710–716.
15. Garibaldi BT, Wang K, Robinson ML, et al. Comparison of time to clinical improvement with vs without remdesivir treatment in hospitalized patients with COVID-19. JAMA Netw Open. 2021;4:e213071. doi:10.1001/jamanetworkopen.2021.3071
16. Mozaffari E, Chandak A, Zhang Z, et al. Remdesivir treatment in hospitalized patients with COVID-19: a comparative analysis of in-hospital all-cause mortality in a large multi-center observational cohort. Clin Infect Dis. 2021;2021:ciab875.
17. Marrone A, Nevola R, Sellitto A, et al. Remdesivir plus dexamethasone versus dexamethasone alone for the treatment of COVID-19 patients requiring supplemental O2 therapy: a prospective controlled non-randomized study. Clin Infect Dis. 2022;2022:ciac014.
18. Pan H, Peto R; WHO Solidarity Trial Consortium. Repurposed antiviral drugs for Covid-19 - interim WHO solidarity trial results. N Engl J Med. 2021;384:497–511.
19. Ader F, Bouscambert-Duchamp M, Hites M, et al. Remdesivir plus standard of care versus standard of care alone for the treatment of patients admitted to hospital with COVID-19 (DisCoVeRy): a Phase 3, randomised, controlled, open-label trial. Lancet Infect Dis. 2022;22:209–221. doi:10.1016/S1473-3099(21)00485-0
20. World Health Organization. Therapeutics and COVID-19: living guideline. Available from: https://www.who.int/publications/i/item/WHO-2019-nCoV-therapeutics-2022.3.
21. Goldberg E, Ben Zvi H, Sheena L, et al. A real-life setting evaluation of the effect of remdesivir on viral load in COVID-19 patients admitted to a large tertiary centre in Israel. Clin Microbiol Infect. 2021;27:917.e1–917.e4. doi:10.1016/j.cmi.2021.02.029
22. Barratt-Due A, Olsen IC, Nezvalova-Henriksen K, et al. Evaluation of the effects of remdesivir and hydroxychloroquine on viral clearance in COVID-19: a randomized trial. Ann Intern Med. 2021;174:1261–1269. doi:10.7326/M21-0653
23. Regan J, Flynn JP, Rosenthal A, et al. Viral load kinetics of severe acute respiratory syndrome coronavirus 2 in hospitalized individuals with coronavirus disease 2019. Open Forum Infect Dis. 2021;8:ofab153. doi:10.1093/ofid/ofab153
24. Lingas G, Néant N, Gaymard A, et al. Effect of remdesivir on viral dynamics in COVID-19 hospitalized patients: a modelling analysis of the randomized, controlled, open-label DisCoVeRy trial. J Antimicrob Chemother. 2022;77(5):dkac048.
25. Hirai N, Nishioka Y, Sekine T, et al. Factors associated with viral clearance periods from patients with COVID-19: a retrospective observational cohort study. J Infect Chemother. 2021;27:864–868. doi:10.1016/j.jiac.2021.02.015
26. Stehlik P, Alcorn K, Jones A, et al. Repeat testing for SARS-CoV-2: persistence of viral RNA is common, and clearance is slower in older people. Med J Aust. 2021;214(10):468–470. doi:10.5694/mja2.51036
27. Mondi A, Lorenzini P, Castilletti C, et al. Risk and predictive factors of prolonged viral RNA shedding in upper respiratory specimens in a large cohort of COVID-19 patients admitted to an Italian reference hospital. Int J Infect Dis. 2021;105:532–539. doi:10.1016/j.ijid.2021.02.117
28. Mancuso P, Venturelli F, Vicentini M, et al. Temporal profile and determinants of viral shedding and of viral clearance confirmation on nasopharyngeal swabs from SARS-CoV-2-positive subjects: a population-based prospective cohort study in Reggio Emilia, Italy. BMJ Open. 2020;10:e040380. doi:10.1136/bmjopen-2020-040380
29. Zou L, Ruan F, Huang M, et al. SARS-CoV-2 viral load in upper respiratory specimens of infected patients. N Engl J Med. 2020;382:1177–1179. doi:10.1056/NEJMc2001737
30. Sourander B, Andersson LM, Brink M, et al. No effect of remdesivir or betamethasone on upper respiratory tract SARS-CoV-2 RNA kinetics in hospitalised COVID-19 patients: a retrospective observational study. Infect Dis. 2022;54(10):1–10.
31. Wong CKH, Lau KTK, Au ICH, et al. Clinical improvement, outcomes, antiviral activity, and costs associated with early treatment with remdesivir for patients with Coronavirus Disease 2019 (COVID-19). Clin Infect Dis. 2022;74:1450–1458. doi:10.1093/cid/ciab631
32. Vermillion MS, Murakami E, Ma B, et al. Inhaled remdesivir reduces viral burden in a nonhuman primate model of SARS-CoV-2 infection. Sci Transl Med. 2022;14:eabl8282. doi:10.1126/scitranslmed.abl8282
33. Zhan Y, Shang J, Gu Y, et al. Efficacy of corticosteroid in patients with COVID-19: a multi-center retrospective study and meta-analysis. J Med Virol. 2021;93(7):4292–4302. doi:10.1002/jmv.26914
34. Spagnuolo V, Guffanti M, Galli L, et al. Viral clearance after early corticosteroid treatment in patients with moderate or severe covid-19. Sci Rep. 2020;10:21291. doi:10.1038/s41598-020-78039-1
35. Bajaj V, Gadi N, Spihlman AP, et al. Aging, immunity, and COVID-19: how age influences the host immune response to coronavirus infections? Front Physiol. 2021;11:571416. doi:10.3389/fphys.2020.571416
36. Néant N, Lingas G, Le Hingrat Q, et al. Modeling SARS-CoV-2 viral kinetics and association with mortality in hospitalized patients from the French COVID cohort. Proc Natl Acad Sci. 2021;118:e2017962118. doi:10.1073/pnas.2017962118
37. Magleby R, Westblade LF, Trzebucki A, et al. Impact of severe acute respiratory syndrome Coronavirus 2 viral load on risk of intubation and mortality among hospitalized patients with Coronavirus Disease 2019. Clin Infect Dis. 2021;73:e4197–e4205. doi:10.1093/cid/ciaa851
38. Takashita E, Kinoshita N, Yamayoshi S, et al. Efficacy of antibodies and antiviral drugs against Covid-19 omicron variant. N Engl J Med. 2022;386:995–998. doi:10.1056/NEJMc2119407
39. Vangeel L, Chiu W, De Jonghe S, et al. Remdesivir, molnupiravir and nirmatrelvir remain active against SARS-CoV-2 Omicron and other variants of concern. Antiviral Res. 2022;198:105252. doi:10.1016/j.antiviral.2022.105252
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


