Back to Journals » Journal of Asthma and Allergy » Volume 13
Impact of Prematurity and Severe Viral Bronchiolitis on Asthma Development at 6–9 Years
Authors Garcia-Garcia ML , Gonzalez-Carrasco E , Bracamonte T, Molinero M, Pozo F , Casas I , Calvo C
Received 24 April 2020
Accepted for publication 10 August 2020
Published 18 September 2020 Volume 2020:13 Pages 343—353
DOI https://doi.org/10.2147/JAA.S258447
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Amrita Dosanjh
Maria Luz Garcia-Garcia,1 Ersilia Gonzalez-Carrasco,2 Teresa Bracamonte,1 Mar Molinero,3 Francisco Pozo,3 Inmaculada Casas,3 Cristina Calvo4
1Pediatrics Department, Severo Ochoa University Hospital, Fundación IDIPHISA, Alfonso X El Sabio University Madrid, Spain. Translational Research Network in Pediatric Infectious Diseases (RITIP), Madrid, Spain; 2Department, Severo Ochoa University Hospital, Fundación IDIPHISA. Alfonso X El Sabio University, Madrid, Spain; 3Respiratory Virus and Influenza Unit, National Microbiology Center (ISCIII), Madrid, Spain; 4Pediatric Infectious Diseases Department, Fundación IdiPaz, Translational Research Network in Pediatric Infectious Diseases (RITIP), Madrid, Spain. TEDDY Network (European Network of Excellence for Pediatric Clinical Research), Italy. La Paz University Hospital, Madrid, Spain
Correspondence: Maria Luz Garcia-Garcia Email [email protected]
Background: Premature birth is associated with increased susceptibility for viral infections and chronic airway morbidity. Preterm children, even moderate and late, may be at risk for short- and long-term respiratory morbidities.
Objective: Our main goal was to compare the burden of two conditions, severe bronchiolitis and prematurity (early and moderate-late), on asthma development at 6– 9 years.
Patients and Methods: A retrospective cohort of all preterm (< 37weeks gestational age) and full-term children hospitalized for bronchiolitis, with current age between 6 and 9 years, was created. A second cohort was made up of preterm children, without admission for bronchiolitis, randomly chosen from the hospital premature births database. Prevalence and risk factors for asthma were analysed. Parents completed the International Study of Asthma and Allergies in Childhood (ISAAC) Questionnaire for asthma symptoms for children 6– 7 years. Lung function and aeroallergen sensitization were evaluated.
Results: Of the 480 selected children, 399 could be contacted and agreed to participate: 133 preterm and 114 full-term cases with admission for bronchiolitis and 146 preterm control children without admission for bronchiolitis. The frequency of current asthma at 6– 9 years was higher in preterm cases (27%) compared with full-term-cases (15%) and preterm controls (14%) (p=0.04). Among hospitalized-bronchiolitis children, prematurity (p=0.04), rhinovirus infection (p=0.03), viral coinfection (p=0.04) and paternal asthma (p=0.003) were risk factors for asthma at 6– 9 years. Among premature children, with and without bronchiolitis admission, the risk factors for asthma at 6– 9 years were admission for bronchiolitis (p=0.03) and aeroallergen sensitisation (p=0.01). Moderate and late preterm children without admission for bronchiolitis showed similar prevalence of current asthma than full-term ones, previously admitted for bronchiolitis.
Conclusion: Preterm birth is an important early life risk factor for asthma in childhood. The addition of other risk factors, such as severe bronchiolitis, especially by rhinovirus or viral coinfections, are associated with even higher risk for subsequent asthma.
Keywords: asthma, wheezing, prematurity, bronchiolitis, rhinovirus, respiratory syncytial virus
Infants born prematurely have a high risk of complications both in the short and in the long term. Regarding respiratory morbidity, prematurity is associated with increased susceptibility for viral infections and with chronic airway morbidity.1 Both conditions are strongly related to recurrent wheezing (RW) and asthma, especially in infants born before 32 weeks of gestational age (wGA). On the other hand, babies born between 33 and 36 wGA have been considered almost as full-term babies. However, it has been recently described that late-preterm infants have higher hospital admission rates for respiratory viral infections than full-term ones, approaching those of early preterm infants.2 Our group, in a recent study, found that there is increased resource utilization, not only among early-preterm but also in moderate-preterm children caused by respiratory infections, as many of them require readmissions and more medical support than full-term children.3
On the other hand, severe bronchiolitis has been linked to an increased risk for early wheezing and asthma.4–6 Montgomery et al7 found that hospital admission for respiratory infections in infancy was associated with increased risk of asthma after age 5 years, particularly among early-preterm children. Blanken et al8 showed, in otherwise healthy preterm infants, that palivizumab treatment resulted in a significant reduction in the number of wheezing days during the first year of life, even after the end of the treatment. These findings suggest that early respiratory viral infections are an important risk factor for RW and asthma in preterm infants during the first years of life.
Our main goal was to compare the impact of two conditions, severe bronchiolitis and prematurity (early and moderate-late), on RW and asthma development at 6–9 years. To achieve this aim, we compared the frequency of RW and asthma among preterm and full-term 6–9-year-old cases hospitalized for bronchiolitis and a control group of preterm children without admission for bronchiolitis.
Patients and Methods
An observational, analytical, cross-sectional study was conducted at Severo Ochoa University Hospital between October/2016 and June/2017. The study was approved by the Medical Ethics Committee and was conducted in accordance with the Declaration of Helsinki.
Clinical Assessment
All 6–9-year-old preterm children (born before 37 wGA) previously hospitalized for bronchiolitis (preterm cases) in the first two years of age, since September/2008 to December/2011, were included and randomly matched with all full-term children, 6 to 9-year old, also admitted for bronchiolitis in the same period of time (full-term cases). During the hospital stay, a structured questionnaire with clinical variables was filled out in a prospective manner (Appendix 1). Perinatal data were extracted from clinical records. Three polymerase chain reaction assays were performed in nasopharyngeal aspirates to detect 16 respiratory viruses.9–11
The control group was made up of preterm children, without admission for bronchiolitis (preterm controls), randomly chosen from the hospital premature births database (born in the same period as the other two groups: from September/2006 to December/2009).
Parents were contacted by phone from October/2016 to Mar/2017 and were invited to take part in the follow-up study. After signing the informed consent, an interview based on a structured questionnaire was performed to obtain information on: wheezing episodes; related hospital admissions; physician-diagnosed atopic dermatitis; allergic rhinitis; food allergy; pet contacts; daycare attendance; siblings; parental smoking habits; allergy; eczema and asthma in first-order family members diagnosed by a medical doctor.
The International Study of Asthma and Allergies in Childhood (ISAAC) Questionnaire for asthma symptoms for children 6–7 years, previously validated and translated to Spanish, was answered by parents/caregivers.12 The core questions include “ever had wheezing,” “wheezing in the last 12 months,” “ever had asthma,” and symptoms present in the last 12 months: “sleep disturbed due to wheezing ≥1 night per week,” “wheezing due to exercise” and “speech limited due to wheezing.”
Lung Function
Spirometry was performed according to established guidelines13 using a Jaeger MasterScope-PC spirometer (VIASYS HealthCare GmbH, Hoechberg, Germany) at the follow-up visit. The following spirometry values were collected: FVC (forced vital capacity), FEV1 (forced expiratory volume in one second), FEV1/FVC and FEF25-75 (mean forced expiratory flow between 25% and 75% of FVC). Results were presented as percentage of predicted values with reference values of Zapletal14 and z-score of predicted values with reference values of the Global Lung Function Initiative (GLI).15
The bronchodilator test was considered positive when there was a 12% increase in the FEV1 compared with baseline after administration of 400 μg salbutamol.
Skin Prick Tests
Allergic sensitisation was evaluated performing skin prick tests (SPT) for common inhaled allergens. Standardized extracts (Abelló R) were used with a positive control (10 mg/mL histamine) and a negative control (glycerol-saline carrier solution). Papule diameters equal to or exceeding that obtained with histamine were considered positive.
Clinical Definitions
-Bronchiolitis: first episode of acute onset expiratory dyspnea with previous signs of viral respiratory infection in an infant < 24 months.
-Recurrent wheezing: two or more wheezing episodes in the first 3 years of life, excluding bronchiolitis.
-Current Asthma: affirmative response to the question 2 of the ISAAC questionnaire, “has your child had wheezing or whistling in the chest in the past 12 months”. That is the one which in the validation studies has shown a better correlation with current prevalence of asthma.16
-Preterm (PT): children born before 37 wGA
- Early preterm: children born before 32 wGA
-Moderate preterm: children born between 32° to 336 wGA
-Late preterm: children born between 34° to 366 wGA
Sample Size
Accepting an alpha-risk: 0.05 and a beta-risk: 0.2 in a two-sided test, 119 subjects were necessary in both groups to find a statistically significant proportion difference in the prevalence of current asthma, expected to be 0.15 in the full-term group and 0.3 in the PT-cases group. The same sample size calculation was performed to compare the difference among PT-cases and PT-control groups (with an expected prevalence for this group of 15%).
Statistical Analysis
Continuous variables were expressed as mean and standard deviation (SD), and through counts and percentages for categorical variables. After checking normal distribution, continuous variables were compared through Student t-tests. Categorical variables were compared using Chi-squared test with Bonferroni correction for multiple comparisons and results were expressed as odds ratio (OR). A two-sided value of P < 0.05 was considered statistically significant.
To control for potentially confounding variables and to examine the independent contribution of the explicative variables on the likelihood of developing RW and asthma, a backward stepwise binomial logistic regression model was built. All the variables with P-value < 0.1 were introduced in the multivariate analysis. Adjusted odds ratios (OR) with 95% confidence intervals were calculated. All analyses were performed using the Statistical Package for the Social Sciences (SPSS), Version 21.0.
Results
We included 160 children in each group. Parents were contacted by telephone, being able to contact and obtain consent for their participation in 393 cases: 133 preterm cases, 114 full-term cases and 146 preterm controls, all aged between 6 and 9 years at the time of inclusion in the study. Figure 1.
 |
Figure 1 Flow chart of patients included in the study. |
The basic characteristics of the 393 children included are presented in Table 1. Mean age at the entry of the study for the whole group was 6.7 ± 0.8 years, being slightly higher in the preterm control group, p<0.001. Gestational age was similar in both groups of preterm children as well as the proportion of moderate and late prematurity.
 |
Table 1 Baseline Characteristics of the Three Groups of Children Included in the Study: Preterm and Full Term Admitted for Bronchiolitis and Preterm Controls without Admission for Bronchiolitis |
There were some significant differences among the three groups in some background factors. Preterm cases suffered more maternal exposure to active smoking during pregnancy (p=0.03), whereas full-term ones showed higher rates of atopic dermatitis (p=0.02), daycare attendance (p=0.04) and male gender (p=0.01). Preterm controls (p=0.02), had less siblings < than 5 years (p=0.05), less paternal atopy (p=0.04) and less siblings with asthma (p=0.005). No differences were found among the three groups regarding allergic rhinitis or food allergy.
Recurrent Wheezing
Overall, 283 (76%) children presented RW at the follow-up. The frequency of RW was significantly lower in preterm controls compared to the other two groups. Preterm cases required admission for an episode of severe RW more frequently than full-term cases and preterm controls, although the difference did not reach statistical significance (p = 0.08). Table 2.
Maintenance treatment with inhaled corticosteroids and montelukast was prescribed more often in children admitted for bronchiolitis, both preterm and full-term cases, compared to preterm-controls. Table 2.
Recurrent Wheezing: Preterm-Cases vs Full-Term-Cases Comparison
When only children with history of admission for bronchiolitis, both preterm and full-term, were compared, we found that positive viral detection during the admission for bronchiolitis was associated with 3.5 times higher probability of developing RW in comparison with children with negative viral identification. Other factors also related to RW were day care attendance and paternal asthma. Table 3.
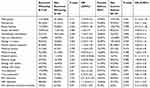 |
Table 3 Bivariate Analysis of Factors Associated with Recurrent Wheezing in Preterm and Full-Term Children with History of Admission for Bronchiolitis |
The variables associated with RW with P-value <0.10 were analysed by logistic regression. Positive viral detection, paternal asthma and daycare centre assistance maintained their independent association with RW. Table 4.
 |
Table 4 Multivariate Test of Possible Risk Factors for Recurrent Wheezing by a Backward (LR) Stepwise Logistic Procedure in Preterm and Full-Term Children with History of Admission for Bronchiolitis |
Prematurity [42 (64%) vs 91 (50%), p=0.03] and rhinovirus infection (HRV) [23 (38%) vs 35 (20%), p=0.02] during the admission for bronchiolitis were associated with severe RW requiring hospitalization. In contrast, children with respiratory syncytial virus (RSV) detection had lower risk of hospitalization for RW than those RSV-negative [18 (29%) vs 92 (53%), (p=0.01)].
Recurrent Wheezing: Preterm Cases vs Preterm-Controls Comparison
Besides admission for bronchiolitis, other factors also related to the development of RW in premature children were maternal asthma, neonatal respiratory distress syndrome and bronchopulmonary dysplasia (BPD) Table 5.
 |
Table 5 Bivariate Analysis of Factors Associated with Recurrent Wheezing and Asthma at 6–9 Years in Preterm Children with and without Admission for Bronchiolitis |
After logistic regression, the variables independently associated with RW were admission for bronchiolitis, which increased the risk 7 times and maternal asthma (Table 6).
Preterm children with siblings with asthma [OR=3.03 (CI95% 1.60–5.81), p=0.001] or atopy [OR=2.64 (CI95% 1.30–5.30), p=0.005] had the highest risk of suffering at least an episode of RW severe enough to require admission.
Asthma Symptoms
The frequency of current asthma at 6–9 years was 19% for the entire population and was significantly higher in preterm cases (27%) compared with full-term-cases (15%) and preterm controls (14%) groups (p=0.04). Table 7.
As shown in Table 7, a statistically significant difference was found among the preterm cases and the other two groups while evaluating the prevalence of ever asthma, exercise-induced wheezing in the past 12 months and sleep disturbed due to wheezing in the past 12 months.
In addition, speech limited due to wheezing in the past 12 months and ever wheezing were more prevalent in preterm cases than in full-term cases and preterm controls, almost reaching statistical significance (p=0.05).
Asthma: Preterm Cases vs Full-Term Cases Comparison
The variables significantly associated with current asthma in preterm and full-term cases hospitalized for bronchiolitis in the bivariate analyses were prematurity, paternal asthma and the following characteristics of the bronchiolitis admission: intensive care admission (ICU); viral coinfection and HRV detection (Table 3). After logistic regression, the variables independently associated with asthma development at 6–9 years were HRV detection, viral coinfection during bronchiolitis, paternal asthma and ICU admission (Table 8).
Asthma: Preterm-BLT vs Preterm-Non-BLT Comparison
The risk of current asthma in the whole preterm group was 2.2 times higher in those with admission for bronchiolitis (Table 5). Other factors associated with asthma at 6–9 years were: paternal asthma and atopy.
Finally, after multivariable analysis, the independent risk factors for the development of asthma at 6–9 years in both groups of preterm children were: admission for bronchiolitis and paternal asthma (Table 9).
Comparison of Full-Term-Cases vs Moderate and Late Preterm-Controls
To compare the burden of moderate and late prematurity (excluding early prematurity) vs admission for bronchiolitis in RW and asthma development, we compared the respiratory morbidity among full-term cases and late and moderate preterm controls. The frequency of RW was higher in full-term cases (85% vs 61%, p<0.001), as well as the prescription of inhaled corticosteroids (47% vs 30%, p=0.009) or montelukast (38% vs 23%, p=0.02). However, no significant differences were seen in the rate of hospitalization for RW (21% vs 20%, p= 0.830) or in the affirmative responses to the following questions of the ISAAC Questionnaire: current asthma (15% vs 17%, p=0.734), ever asthma (18% vs 17%, p=0.874), exercise-induced wheezing (6% vs 9%, p=0.452) and sleep disturbed due to wheezing (6% vs 9%, p= 0.452).
Skin Prick Tests
SPT was performed in 269 children, 81 preterm cases, 82 full-term cases and 106 preterm controls. Aeroallergen sensitization was significantly less frequent in preterm cases (31%) than in full-term (52%) or in preterm controls (45%) (p <0.001).
We compared the proportion of children with aeroallergen sensitization between RSV and HRV single infections, excluding coinfections (N=92) and its association with current asthma. Twenty-one per cent of RSV-children with positive SPT developed asthma compared to 4.5% of RSV-children with negative SPT. Regarding HRV, 57% of HRV patients with positive SPT and 20.5% of HRV-patients with negative SPT (p=0.024) reported current asthma.
Lung Function
Acceptable and repeatable spirometry was obtained in 233 children. No significant differences were found among the three groups in the pulmonary function parameters evaluated: FEV-1, FVC, FEV-1/FVC, FEF50 (Table 10).
Overall, 9 children presented FEV-1 <80% of the theoretical value. Of these, 4 were preterm cases (1 of them with BPD), 4 preterm controls and 1 full-term case. Only 2 of these 9 children with lower lung function did not present RW or asthma until the end of the study. There were also no significant differences in the post bronchodilator lung function values among the 3 groups.
Discussion
This study compared the burden of prematurity and bronchiolitis in the development of asthma at 6–9 years. The frequency of asthma at 6–9 years in previously healthy premature children, without admission for bronchiolitis, was, in our series, higher than that described for the general population at 6–7 years,17 and similar to that of full-term children with history of admission for bronchiolitis. These results were observed, not only in the most immature preterm children but also in those moderate and late preterm without respiratory admissions in the first two years of life. As far as we know, this is the first study that compares the respiratory burden of late and moderate prematurity with one of the best-known risk factors for asthma and recurrent wheezing, such as bronchiolitis. Our results also suggest that, although preterm children with admission for bronchiolitis had twice the risk of asthma at 6–9 years when compared to full-term-cases, the moderate and late preterm controls, were also at increased risk for asthma and this is as high as that associated with severe bronchiolitis in full-term children.
Prematurity and severe bronchiolitis are two of the main risk factors for the development of RW and asthma. Even though the majority of studies have focused on the long-lasting impact of RSV-infections in full-term children, recent studies have observed increased risk of asthma and RW in preterm children with a history of RSV bronchiolitis in infancy.7,18 Early hospitalization with RSV-infection in preterm infants has been associated with more than twice the risk of ongoing respiratory morbidity, especially among those with BPD or lower gestational age.19 Like RSV, HRV-respiratory infections have also been associated with higher risk of asthma at 6 years. In our series, apart from the family history of asthma or atopy classically described, the factors independently associated with asthma at 6–9 years in children admitted for bronchiolitis, were HRV infection, viral coinfection and prematurity, that will be discussed below.
Regarding viral etiology, HRV-bronchiolitis has acquired enormous relevance, not only in RW but also in asthma development, becoming one of the strongest risk factors for asthma at 6 years.20 Jackson et al21,22 found that early life HRV-wheezing, but not RSV, was associated with asthma at 13 years, increasing the risk by 3.3 times. A recent meta-analysis suggests that HRV-wheezing illness in the first 3 years is associated with subsequent wheezing and asthma and this association remains significant at ≥10 years.23 Focusing on preterm infants, Drysdale et al24 in a follow-up study up to 1 year concluded that HRV-infected infants suffered greater chronic respiratory morbidity compared with the RSV-infected ones. Our results support that severe HRV-bronchiolitis is an independent risk factor for asthma at 6–9 years not only in full-term but also in preterm children. HRV-bronchiolitis was also, in our series, a risk factor for severe RW requiring hospitalization, as well as the negative detection of RSV. The mechanism is not fully understood but the results of Perez et al25 suggest that natural HRV-infection in premature children elicits airway secretion of Th2 (IL-4 and IL-13) and Th17 (IL-17) cytokines, which may promote recruitment of neutrophils, immature dendritic cells, and memory T cells in the airways.
Interestingly, RSV-bronchiolitis was associated in our series with lower prevalence of asthma at 6–9 years than non-RSV- ones. These results are in line with those from Carroll et al,26 Mochizuki et al27 and Scheltema et al,28 who found non-significant associations on RSV immunoprophylaxis in premature children, on prevention of asthma at 4.5–6 years. All these data, together with ours, suggest that RSV may not play such a crucial role in asthma development in preterm children as previously thought. The current lower relevance of RSV as inducer of asthma in favour of other viruses, especially HRV, can partly be explained because until the implantation of molecular diagnostic methods, RSV was almost the only respiratory virus detected and included in follow-up studies, so that its role may have been overestimated.
The role of viral respiratory coinfections remains controversial.29 Regarding long-term evolution, our group found in 244 children admitted for bronchiolitis, significantly higher prevalence of asthma at 6–8 years in those with viral coinfection.30 Our current results also support the greater risk of asthma after viral coinfection, although it is worth highlighting that HRV participates in a great proportion of these coinfections. In a previous report, our group found a 9-fold probability higher of having detectable nasal thymic stromal lymphopoietin (TSLP) in infants with RSV+HRV coinfection, suggesting that these coinfections may lead to an altered mediator profile which biases towards a T2 immune response, thus favouring asthma development.31
Regarding prematurity, our results confirm the association between preterm delivery and asthma, with the highest prevalence, 27% being in premature infants who also suffered a severe bronchiolitis needing hospital admission. Fake et al32 in the EPICure study found 25% of asthma at 11 years in extremely premature children (≤25 weeks). In our series, despite the fact that only 25% of children were <32 wGA, the prevalence of asthma at 6–9 years in preterm cases was almost identical to that reported in extremely preterm by Fawke et al.32 These results suggest that the burden of severe bronchiolitis in moderate and late preterm infants may increase their risk of asthma to a similar level as most extreme premature infants.
Moderate and late preterm currently constitute over 80% of all preterm births33 and generally, have been assumed not to encounter many respiratory problems later in life. However, in the last years, there has been increasing concern about the development of wheezing and asthma in childhood, with higher frequency than full-term children, although current evidence is controversial. Vrijlandt et al34 in a large prospective cohort study showed that at preschool age, moderately preterm infants revealed more nocturnal cough or wheeze during or without a cold and increased use of inhaled steroids. At the age of 5 years, rates of respiratory symptoms between moderate and early preterm born children were similar. However, these authors recently reported that adolescents (13–14 years) born moderate and late preterm had only slightly more lung function abnormalities than those born full term, and did not differ in the maximal exercise test and in physical activity level.35,36 However, these conclusions may be limited by the small number of patients included in the study, being 37 moderate and late preterm and 34 full-term children. Voge et al37 found that healthy late preterm infants had a higher incidence of asthma by school age than full-term ones, with a hazard ratio of 1.44 after controlling for maternal and passive smoke and a family history of asthma or atopy, with an almost significant difference (p=0.07). The results of Maijakaisa et al38 confirmed the association between preterm delivery and asthma and the risk in late preterm children was almost double when compared with children born at term. Our study demonstrates for the first time that the risk of asthma at 6–9 years in moderate and late preterm children is similar to that of full-terms who have been hospitalised for a severe bronchiolitis, which is one of the strongest risk factors for asthma development.4–7 Other respiratory symptoms such as ever wheezing, ever asthma, and respiratory symptoms present in the last 12 months were also reported with a similar frequency by late and moderate preterm as by full-term children previously hospitalized for bronchiolitis.
In our study, mean spirometric values at 6–9 years were normal in the three groups, without differences among them. However, significant lower FEV-1/FVC ratio values were observed in children with RW and lower FEV1, FVC, FEV1/FVC and FEF50 values in children with severe RW. Similarly, in the SPRING study, in which preterm infants between 32 and 35 weeks were included, with and without admission for RSV infection, no differences in lung function were observed when comparing the two groups overall, although those children with worse pulmonary function had greater respiratory morbidity with more frequent RW.39
The strengths and weaknesses of our study are those inherent in the observational nature of the study design. We do not know the prevalence of asthma nor the respiratory evolution in the children not followed-up. And several epidemiologic factors analysed relied on parental self-reporting, and hence there is potential recall bias.
In conclusion, this work provides evidence that prematurity itself is related with increased prevalence of asthma at 6–9 years. Severe bronchiolitis, mainly HRV-bronchiolitis and viral coinfection bronchiolitis, is an independent risk factors for asthma in childhood. These findings may be helpful in developing preventive strategies that could minimize the respiratory burden of preterm-born infants.
Disclosure
The authors declare no conflicts of interest in this work.
References
1. Been JV, Lugtenberg MJ, Smets E, et al. Preterm birth and childhood wheezing disorders: a systematic review and metaanalysis. PLoS Med. 2014;11(1):e1001596.
2. Pike KC, Lucas JS. Respiratory consequences of late preterm birth. Paediatr Respir Rev. 2015;16(3):182–188.
3. García-Garcia ML, González-Carrasco E, Quevedo S, et al. Clinical and Virological Characteristics of Early and Moderate Preterm Infants Readmitted With Viral Respiratory Infections. Pediatr Infect Dis J. 2015;34(7):693–699. doi:10.1097/INF.0000000000000718
4. Stein RT, Sherrill D, Morgan WJ, et al. Respiratory syncytial virus in early life and risk of wheeze and allergy by age 13 years. Lancet. 1999;354(9178):541–545. doi:10.1016/S0140-6736(98)10321-5
5. James K, Gebretsadik T, Escobar G, et al. Risk of childhood asthma following infant bronchiolitis during the respiratory syncytial virus season. J Allergy Clin Immunol. 2013;132(1):227–229. doi:10.1016/j.jaci.2013.01.009
6. Sigurs N, Aljassim F, Kjellman B, et al. Asthma and allergy patterns over 18 years after severe RSV bronchiolitis in the first year of life. Thorax. 2010;65(12):1045–1052. doi:10.1136/thx.2009.121582
7. Montgomery S, Bahmanyar S, Brus O, Hussein O, Kosma P, Palme-Kilander C. Respiratory infections in preterm infants and subsequent asthma: a cohort study. BMJ Open. 2013;3(10):e004034. doi:10.1136/bmjopen-2013-004034
8. Blanken MO, Rovers MM, Molenaar JM, et al. Respiratory syncytial virus and recurrent wheeze in healthy preterm infants. N Engl J Med. 2013;368(19):1791–1799. doi:10.1056/NEJMoa1211917
9. Coiras MT, Perez-Brena P, Garcia ML, Casas I. Simultaneous detection of influenza A, B, and C viruses, respiratory syncytial virus, and adenoviruses in clinical samples by multiplex reverse transcription nested-PCR assay. J Med Virol. 2003;69(1):132–144. doi:10.1002/jmv.10255
10. Coiras MT, Aguilar JC, Garcia ML, Casas I, Perez-Brena P. Simultaneous detection of fourteen respiratory viruses in clinical specimens by two multiplex reverse transcription nested-PCR assays. J Med Virol. 2004;72(3):484–495. doi:10.1002/jmv.20008
11. López-Huertas MR, Casas I, Acosta-Herrera B, García-García ML, Coiras MT, Perez-Brena P. Two RT-PCR based assays to detect human metapneumovirus in nasopharyngeal aspirates. J Virol Methods. 2005;129(1):1–7. doi:10.1016/j.jviromet.2005.05.004
12. Mata Fernández C, Fernández-Benitez M, Pérez Miranda M. Validation of the Spanish version of the Phase III ISAAC questionnaire on asthma. J Investig Allergol Clin Immunol. 2005;15(3):201–210.
13. Miller MR, Hankinson J, Brusasco V, et al. Standardisation of spirometry. Eur Respir J. 2005;26(2):319–338. doi:10.1183/09031936.05.00034805
14. Zapletal A, Paul T, Samanek N. Die Bedeutung heutiger Methoden der Lungenfunktionsdiagnostik zur Feststellung einer Obstruktion der Atemwege bei Kindern und Jugendlichen. Z Erkrank Atm-Org. 1977;149:343–371.
15. Quanjer PH, Stanojevic S, Cole TJ, et al. ERS Global Lung Function Initiative. Multi-ethnic reference values for spirometry for the 3-95-yr age range: the global lung function 2012 equations. Eur Respir J. 2012;40(6):1324–1343. doi:10.1183/09031936.00080312
16. Jenkins MA, Clarke JR, Carlin JB, et al. Validation of questionnaire and bronchial hyperresponsiveness against respiratory physician assessment in the diagnosis of asthma. Int J Epidemiol. 1996;25(3):609–616. doi:10.1093/ije/25.3.609
17. García-Marcos L, Batllés-Garrido J, Blanco-Quirós A, et al. Influence of two different geo-climatic zones on the prevalence and time trends of asthma symptoms among Spanish adolescents and schoolchildren. Int J Biometeorol. 2009;53(1):53–60. doi:10.1007/s00484-008-0190-3
18. Fauroux B, Gouyon JB, Roze JC, et al. Respiratory morbidity of preterm infants less than 33 weeks gestation without bronchopulmonary dysplasia: a 12-month follow-up of the CASTOR study cohort. Epidemiol Infect. 2014;142(7):1362–1374. doi:10.1017/S0950268813001738
19. Townsi N, Laing IA, Hall GL, Simpson SJ. The Impact of Respiratory Viruses on Lung Health After Preterm Birth. Eur Clin Respir J. 2018;5(1):1487214.
20. Lemanske Jr. RF, Jackson DJ, Gangnon RE, et al. Rhinovirus illnesses during infancy predict subsequent childhood wheezing. J Allergy Clin Immunol. 2005;116(3):571–577. doi:10.1016/j.jaci.2005.06.024
21. Jackson DJ, Gangnon RE, Evans MD, et al. Wheezing rhinovirus illnesses in early life predict asthma development in high-risk children. Am J Respir Crit Care Med. 2008;178(7):667–672. doi:10.1164/rccm.200802-309OC
22. Rubner FJ, Jackson DJ, Evans MD, et al. Early life rhinovirus wheezing, allergic sensitization, and asthma risk at adolescence. J Allergy Clin Immunol. 2017;139(2):501–507. doi:10.1016/j.jaci.2016.03.049
23. Liu L, Pan Y, Zhu Y, et al. Association between rhinovirus wheezing illness and the development of childhood asthma: a meta-analysis. BMJ Open. 2017;7(4):e013034. doi:10.1136/bmjopen-2016-013034
24. Drysdale SB, Alcazar-Paris M, Wilson T, Smith M, Zuckerman M, Broughton S. Rhinovirus infection and healthcare utilisation in prematurely born infants. Eur Respir J. 2013;42(4):1029–1036. doi:10.1183/09031936.00109012
25. Perez GF, Pancham K, Huseni S, et al. Rhinovirus-induced airway cytokines and respiratory morbidity in severely premature children. Pediatr Allergy Immunol. 2015;26(2):145–152. doi:10.1111/pai.12346
26. Carroll KN, Gebretsadik T, Escobar GJ, et al. Respiratory syncytial virus immunoprophylaxis in high-risk infants and development of childhood asthma. J Allergy Clin Immunol. 2017;139(1):66–71. doi:10.1016/j.jaci.2016.01.055
27. Mochizuki H, Kusuda S, Okada K, Yoshihara S, Furuya H, Eaf S. Scientific Committee for Elucidation of Infantile Asthma. Palivizumab Prophylaxis in Preterm Infants and Subsequent Recurrent Wheezing. Six-Year Follow-up Study. Am J Respir Crit Care Med. 2017;196(1):29–38. doi:10.1164/rccm.201609-1812OC
28. Scheltema NM, Nibbelke EE, Pouw J, et al. Respiratory syncytial virus prevention and asthma in healthy preterm infants: a randomised controlled trial. Lancet Respir Med. 2018;6(4):257. doi:10.1016/S2213-2600(18)30055-9
29. Calvo C, García-García ML, Pozo F, et al. Respiratory Syncytial Virus Coinfections With Rhinovirus and Human Bocavirus in Hospitalized Children. Medicine. 2015;94(42):e1788. doi:10.1097/MD.0000000000001788
30. Garcia-Garcia ML, Calvo C, Ruiz S, et al. Role of viral coinfections in asthma development. PLoS One. 2017;12(12):e0189083. doi:10.1371/journal.pone.0189083
31. García-García ML, Calvo C, Moreira A, et al. Thymic stromal lymphopoietin, IL-33, and periostin in hospitalized infants with viral bronchiolitis. Medicine. 2017;96(18):e6787. doi:10.1097/MD.0000000000006787
32. Fawke J, Lum S, Kirby J, et al. Lung function and respiratory symptoms at 11 years in children born extremely preterm. EPICure Study Am J RespirCrit Care Med. 2010;182(2):237–245. doi:10.1164/rccm.200912-1806OC
33. Shapiro-Mendoza CK, Lackritz EM. Epidemiology of Late and Moderate Preterm Birth. Semin Fetal Neonatal Med. 2012;17(3):120–125. doi:10.1016/j.siny.2012.01.007
34. Vrijlandt EJ, Kerstjens JM, Duiverman EJ, Bos AF, Reijneveld SA. Moderately Preterm Children Have More Respiratory Problems During Their First 5 Years of Life Than Children Born Full Term. Am J Respir Crit Care Med. 2013;187(11):1234–1240. doi:10.1164/rccm.201211-2070OC
35. Vrijlandt E, Reijneveld SA, Aris-Meijer JL, Bos AF. Respiratory Health in Adolescents Born Moderately-Late Preterm in a Community-Based Cohort. J Pediatr. 2018;203:429–436. doi:10.1016/j.jpeds.2018.07.083
36. Kugelman A, Colin A. Late Preterm Infants: near Term But Still in a Critical Developmental Time Period. Pediatrics. 2013;132(4):741–751. doi:10.1542/peds.2013-1131
37. Voge GA, Carey WA, Ryu E, et al. What accounts for the association between late preterm births and risk of asthma? Allergy Asthma Proc. 2017;38(2):152–156. doi:10.2500/aap.2017.38.4021
38. Maijakaisa H, Keski-Nisula L, Georgiadis L, Räisänen S, Gissler M, Heinonen S. The Burden of Childhood Asthma and Late Preterm and Early Term Births. J Pediatr. 2014;164(2):295–299. doi:10.1016/j.jpeds.2013.09.057
39. Carbonell-Estrany X, Pérez-Yarza EG, García LS, et al. IRIS Study Group. Long-Term Burden and Respiratory Effects of Respiratory Syncytial Virus Hospitalization in Preterm Infants-The SPRING Study. PLoS One. 2015;10(5):e0125422. doi:10.1371/journal.pone.0125422
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.






