Back to Journals » International Journal of Women's Health » Volume 9
Impact of patient demographics, tumor characteristics, and treatment type on treatment delay throughout breast cancer care at a diverse academic medical center
Authors Khanna S, Kim KN, Qureshi MM, Agarwal A, Parikh D, Ko NY, Rand AE, Hirsch AE
Received 26 August 2017
Accepted for publication 12 October 2017
Published 6 December 2017 Volume 2017:9 Pages 887—896
DOI https://doi.org/10.2147/IJWH.S150064
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Elie Al-Chaer
Shivani Khanna,1 Kristine N Kim,1 Muhammad M Qureshi,1 Ankit Agarwal,1 Divya Parikh,1 Naomi Y Ko,2 Alexander E Rand,1 Ariel E Hirsch1
1Department of Radiation Oncology, Boston Medical Center, Boston University School of Medicine, 2Department of Hematology Oncology, Boston Medical Center, Boston MA, USA
Purpose and objective: The aim of this study was to examine the impact of patient demographics, tumor characteristics, and treatment type on time to treatment (TTT) in patients with breast cancer treated at a safety net medical center with a diverse patient population.
Patients and methods: A total of 1,130 patients were diagnosed and treated for breast cancer between 2004 and 2014 at our institution. We retrospectively collected data on patient age at diagnosis, race/ethnicity, primary language spoken, marital status, insurance coverage, American Joint Committee on Cancer (AJCC) stage, hormone receptor status, and treatment dates. TTT was determined from the date of breast cancer biopsy to treatment start date. Nonparametric Mann–Whitney U-test (or Kruskal–Wallis test when appropriate) and multivariable quantile regression models were employed to assess for significant differences in TTT associated with each factor.
Results: Longer median TTT was noted for Black (P=0.002) and single (P=0.002) patients. AJCC stage IV patients had shorter TTT (27.5 days) compared to earlier AJCC patients (36, 35, 37, 37 days for stage 0, I, II, III, respectively), P=0.028. Age, primary language spoken, insurance coverage, and hormone receptor status had no significant impact on TTT. On multivariate analysis, race/ethnicity remained the only significant factor with Black reporting longer TTT, P=0.025. However, race was not a significant factor for time from first to second treatment. More Black patients were noted to be single (P<0.0001) and received chemotherapy as first treatment (P=0.008) compared to White, Hispanic, or other race/ethnicity patients.
Conclusion: In this retrospective analysis, Black patients had longer TTT, were more likely to receive chemotherapy as first treatment, and have a single marital status. These patient factors will help identify vulnerable patients and guide further research to understand the barriers to care and the impact of treatment delays on outcomes.
Keywords: breast cancer, treatment delay, patient demographics, race, tumor characteristics
Introduction
Breast cancer is the most commonly diagnosed malignancy and the second leading cause of cancer death among women in the USA. The National Cancer Institute estimates that there were 252,710 new breast cancer cases and 40,610 deaths in 2017.1 Unfortunately, breast cancer disparities in outcomes among different races and vulnerable populations have been a long-standing problem. Previously, breast cancer incidence rates had been higher for White women than for Black women in the USA, but in 2012, the incidence rates converged.2 Despite this, the disparity in mortality between White and Black women continues to widen, and Black women are 42% more likely to die from breast cancer than their White counterparts.2 Even with an increase in the use of screening mammography across races in the USA, there remain socioeconomic and race-related disparities in treatment and outcomes.3 Specifically, large multi-institutional studies have demonstrated differences in cancer stage at diagnosis, types of treatment available and outcomes by primary language spoken, race, insurance coverage, marital status, and other demographic factors.3–18
Previous studies of breast cancer disparities have looked at delays to care across the cancer continuum. Research has revealed that delays to treatment are significantly associated with low socioeconomic status and race.19 A meta-analysis of 87 studies by Richards et al showed that delays of >3–6 months after an initial diagnosis may have a 12% lower 5-year survival than those without delay.13
Breast cancer treatment is complex, with potentially several different sequential treatments: surgery, chemotherapy, and radiation therapy. Delays anywhere along the treatment pathway can have a significant impact on mortality. Studies have shown that treatment delay >4 weeks to postoperative chemotherapy or 8 weeks to initiation of postoperative radiotherapy is associated with shorter disease-free and overall survival.21–24 Despite these findings, there are limited data in the literature regarding treatment delay across the entire patient diagnosis and treatment pathway.
The purpose of our study is to assess the disparities in both the time to first treatment and the time to second treatment in order to better understand treatment delay throughout the entirety of breast cancer care. We stratify patients by age at diagnosis, race/ethnicity, primary language spoken, insurance coverage, marital status, tumor stage, and hormone receptor status. This study is also novel because it is based at a large academic institution that serves as the major safety net hospital in New England, and the results are evaluated in a setting where the majority of patients are non-White.
Patients and methods
Patient selection
A total of 1,547 patients were diagnosed with breast cancer between April 2004 and April 2014 at our academic medical institution. All patients received multidisciplinary care involving surgeons, medical oncologists, radiation oncologists, radiologists, and allied health professionals prior to the initiation of treatment. We excluded 417 patients from the study for the following reasons: patients did not have complete biopsy information prior to surgery or biopsy was not performed at this institution (n=275), treatment started >365 days after initial diagnosis (n=4), patients transferred their medical care to another institution after receiving their diagnosis (n=125), patients refused all care after receiving their diagnosis (n=6), or patients had metastatic disease from another primary cancer (n=7).
Data collection and study variables
Clinical Data Warehouse staff reviewed the institution’s medical records for breast cancer patients diagnosed in the stated time frame. The data collected included patient’s age, race/ethnicity, primary language spoken, marital status, insurance coverage, and American Joint Committee on Cancer (AJCC) stage at diagnosis. Age at diagnosis was categorized as ≤50, >50 to ≤70, and >70 years old. Race/ethnicity was categorized as Black, White, Hispanic, and others. Primary language spoken was categorized as English, Spanish, Haitian Creole, and others. Marital status was categorized as married, single, and others (including divorced, widowed, separate, and other status). Insurance coverage was categorized as private/commercial, charity/Medicaid/self-pay/uninsured, and Medicare.
The research team reviewed individual patient medical records to collect tumor information, date of pathologic diagnosis, dates of treatment, and type of treatment(s) received. Data on tumor information included tumor hormone receptor status: estrogen receptor (ER), progesterone receptor (PR), and human epidermal growth factor receptor 2 (HER2). Stage at diagnosis was classified according to the 2002 AJCC classification scheme: 0, I, II, III, and IV.
Treatment
Patients underwent a combination of surgery, radiation therapy, chemotherapy, and hormone therapy. Time to treatment (TTT) was calculated from the date of biopsy to the date of first treatment received. In addition to the first treatment received, information on follow-up treatment was ascertained for all patients.
Statistical analysis
Descriptive statistics were computed to describe the patient cohort. Frequencies are presented as number of patients (column %) and time metrics as median (interquartile range [IQR]). Nonparametric Mann–Whitney U-test or Kruskal–Wallis test (when appropriate) was used to assess the differences in the distribution of TTT and the time to second treatment by patient, tumor, and treatment characteristics. Dwass–Steel–Critchlow–Fligner multiple comparison procedure was used to perform pairwise comparisons. The procedure controls for experiment-wise error rate. Furthermore, multivariable quantile (median) regression models were employed, and covariate-adjusted parameter estimates with 95% confidence intervals (CIs) were computed. For each time metric, the estimates generated from quantile regression are interpreted as difference in time interval (days) associated with one unit change in each covariate. Only those covariates that had an overall P-value <0.1 in the univariate model were selected for the multivariate model.
All of the analyses were two-sided, and P-values <0.05 were considered statistically significant. All statistical computations were performed on SAS 9.1 system (SAS Institute Inc., Cary, NC, USA).
Ethics
Approval for this research was granted by the institutional review board at Boston Medical Center. All medical records were de-identified for this study, and thus, patient consent to review medical records was not required as part of the institutional review board approval.
Results
Of the 1,130 patients diagnosed with breast cancer, 910 (80.5%) patients received surgery, 162 (14.3%) patients received chemotherapy, and 58 (5.1%) patients received hormone therapy as first treatment. A total of 955 (84.5%) underwent second treatment. The distribution of second treatment received was as follows: radiation therapy (36.4%, n=411), chemotherapy (22.8%, n=258), hormone therapy (13.3%, n=150), and surgery (12.0%, n=136).
The majority of the patients were between the ages 50 and 70 years (51.7%, n=584) and reported English as their primary language spoken (70.7%, n=799). Non-White race/ethnicity was reported in 64.5% (n=729) of the patient cohort reflecting a diverse patient population. At the time of diagnosis, 35.6% (n=402) of the patient cohort was married, 37.3% (n=421) was single, while 27.2% (n=307) reported their marital status as others.
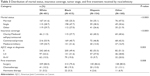
Of the 1,130 patients, complete hormone receptor status was available for 723 patients (~64% of the cohort). The patients were classified into following groups according to their ER/PR/HER2 status: 1) ER+/PR+/HER2- (67.8%, n=490), 2) ER-/PR-/HER2+ (12.5%, n=90), and 3) ER-/PR-/HER2- (19.8%, n=143). Full characteristics are presented in Table 1. The median TTT and the time from first to second treatment were 36 days (IQR =31) and 69 days (IQR =74), respectively.
Time to first treatment by demographics
In the univariate analysis comparing median TTT by demographics, there was no significant association of patient age (overall P=0.36), primary language spoken (overall P=0.26), and insurance coverage (overall P=0.64) with TTT. Pairwise comparisons did not identify any significant differences among subgroups within each factor.
Black women were found to have longer TTT (39 days) compared to White, Hispanic, and other women (35, 32, and 33 days, respectively) (overall P<0.01). On pairwise comparisons, the overall significance was primarily driven from Black vs White (P<0.01). In the analysis of marital status and TTT, married patients had significantly shorter TTT (33 days) compared to single (38 days) and other groups (35 days) (overall P<0.01). In pairwise comparisons, the married vs single (P<0.01) and married vs others (P=0.04) comparisons were significant (Table 1).
Time to first treatment by tumor characteristics and first treatment received
Patients diagnosed with stage IV disease had the shortest TTT (27.5 days) compared to patients diagnosed with earlier stages (overall P=0.03). Stage IV patients had significantly shorter TTT compared to stage III (P=0.05) and stage II (P=0.04).
Overall, time to first treatment did not correlate strongly with the type of first treatment received (overall P=0.08) (Table 1).
Time to first treatment: multivariate model
In the multivariate model with race/ethnicity, marital status, AJCC stage, and first treatment received (all factors with overall P<0.1 in the univariate analysis), race/ethnicity was the only independent predictor of TTT (overall P=0.03). Black patients had longer TTT compared to White patients (adjusted parameter estimate 4.5, 95% CI: 0.69, 8.3, P=0.03). When compared to married patients, single patients still had longer TTT (adjusted parameter estimate 4.0, 95% CI: 0.26, 7.7, P=0.04) (Table 1).
Time to second treatment by demographics
Younger patients (≤50 years) had a longer lapse in time from their first to second treatment (76 days) compared to older patients (68 days for >50 to ≤70 years and >70 years) (overall P=0.02). On pairwise comparison, age ≤50 years vs >50 to ≤70 years was significant (P=0.02). Marital status predicted time to second treatment (overall P=0.01), single (75 days) patients had longer time to second treatment compared to married (66 days) with a pairwise P-value of 0.01 (Table 2).
Time to second treatment by tumor characteristics and first treatment received
In contrast to the analysis of TTT, patients with early-stage disease had a shorter median time to second treatment (54.5 and 59 days for stages 0 and I, respectively) compared to more advance stage disease (154 and 91 days for stages III and IV, respectively) (overall P<0.01). Pairwise comparisons resulted in several significant differences: stage 0 vs stage II (P<0.01), stage 0 vs stage III (P<0.01), stage I vs stage II (P<0.01), stage I vs stage III (P<0.01), and stage II vs stage III (P<0.01).
ER+/PR+/HER2- patients had the shortest time from first to second treatment (63 days) compared to 73 and 76 days for ER-/PR-/HER2+ and ER-/PR-/HER2-, respectively (overall P<0.01). In pairwise analysis, ER+/PR+/HER2- was significantly different from ER-/PR-/HER2+ (P=0.05) and ER-/PR-/HER2- (P=0.01).
Surgical patients had the shortest time to second treatment (62 days) compared to patients who got chemotherapy (203 days) or hormone therapy (123 days) as their first treatment (overall P<0.01). In pairwise analysis, surgical patient was significantly less delayed compared to chemotherapy (P<0.01) and hormone therapy (P<0.01) groups (Table 2).
Time to second treatment: multivariate model
Advanced AJCC stage remained a significant predictor of longer time to second treatment after adjusting for other factors (overall P<0.01). Pairwise comparisons resulted in several significant differences: stage 0 vs stage II (P<0.01), stage 0 vs stage III (P<0.01), stage I vs stage II (P<0.01), stage I vs stage III (P<0.01), and stage II vs stage III (P=0.03). Finally, chemotherapy (adjusted parameter estimate 125, 95% CI: 111.2, 138.8, P<0.01) and hormone therapy (adjusted parameter estimate 54, 95% CI: 2.8, 105.2, P=0.04) patients had longer time to second treatment compared to surgical patients, reflecting the different durations of systemic and local treatment modalities (Table 2).
Race/ethnicity and patient characteristics
Race/ethnicity correlated with marital status, insurance coverage, AJCC stage, and first treatment received. The distribution of single marital status was 47.7, 38.3, 30.6, and 28.7% among Black, Hispanic, other, and White women, respectively (P<0.01). More Black, Hispanic, and other patients (27.7, 40.3, and 40.6%) had charity/Medicaid/self-pay/uninsured as their insurance status compared to their White counterparts (11.5%) (P<0.01). Advanced disease presentation (stages III–IV) was noted among Black and other women (19.0 and 20.0%) compared to their White and Hispanic counterparts (15.5 and 9.7%) (P<0.01). A total of 19.3% of Black patients underwent chemotherapy as their first treatment compared to White, Hispanic, and other race/ethnic patients (10.2, 13.0, and 13.1%, respectively) (P<0.01) (Table 3).
  | Table 3 Distribution of marital status, insurance coverage, tumor stage, and first treatment received by race/ethnicity |
Subgroup analysis of race/ethnicity and time to first treatment
When the results were stratified by marital status, the longest time to first treatment was noted among single White patients (39 days) and Black patients (41 days) compared to single Hispanic patients (33 days) and others (32 days) (overall P<0.01). Black patients with AJCC stage III disease had 44 days until first treatment compared to White patients who had 28.5 days (overall P=0.03). When the results were stratified by the type of first treatment, Black patients had a longer duration to chemotherapy as first treatment (46 days) compared to White patients (31 days), Hispanic patients (41.5 days), or other race patients (35 days) (Table 4).
Discussion
The US Department of Health and Human Services, the American Cancer Society, and many other national organizations have identified reducing health care disparities, particularly in the setting of cancer care, as a key goal in the effort to improve health outcomes nationally.25 On a smaller scale, there have been successful local interventions to reduce health care disparity in breast cancer care in Black women. These interventions include culturally sensitive educational community programs that focus on preventative health measures with the understanding that Black women are known to have more barriers to cancer detection and care compared to White women.26,27
Black and Hispanic women with breast cancer are more often uninsured or insured by Medicaid and present with more advanced disease than White women.28 In particular, Black women with breast cancer are more likely than White women to present with advanced stage and more aggressive disease and are more likely to have Medicaid coverage.9 This is also true for Hispanic women, who, along with Black women, are more likely to be diagnosed at a later stage of disease and be uninsured or have Medicaid.24,25 Our analysis shows similar disparities for Black women compared to their White counterparts. AJCC stages 0, I–II, and III–IV were reported in 49.4, 31.6, and 19.0% of Black women as compared to 60.4, 24.2, and 15.5% of White women, respectively, indicating more advanced disease presentation for Black women. A similar disparity was noted in insurance coverage in this study with 27.7% of Blacks in charity/Medicaid/self-pay/uninsured group as compared to only 11.5% of Whites. The highest percentage of commercial/private insurance coverage was reported among White women (53.9%), with Black women reporting the lowest percentage (40.7%) in this study.
With respect to the impact of race on treatment delay, some researchers have found that Black women have longer delays than White women, whereas other researchers did not note a significant difference.20 Our analysis shows a disparity in TTT for Black women, with both White and Hispanic women having shorter time to first treatment. This finding is despite the ethnically diverse patient population at our institution, which serves as a major safety net hospital. Of note, Black patients who received chemotherapy as first treatment had a longer TTT (46 days) compared to White patients (31 days). Interestingly, among patients who received second treatment, race was not significantly associated with time to second treatment, unlike time to first treatment. One possible explanation may be that once patients initiate treatment after diagnosis, they are in more frequent contact with health care providers and thus more likely to not have delays throughout their course of care.
Outside of race, there are many known variables that may contribute to treatment delay. For example, insurance coverage often dictates access to care and lack of health insurance is associated with inferior access to primary and preventative care.29 Previous studies have shown that uninsured patients and those covered with Medicaid are more likely to present with advanced disease and have decreased survival compared to privately insured patients.30,31 Our study did not find a statistically significant association between insurance type and time to first treatment. This may reflect the nature of this institution being the largest safety net hospital in the region that serves a large proportion of care to the uninsured and Medicaid beneficiaries. In addition, given that neoadjuvant chemotherapy is used primarily to downstage large breast tumors to facilitate breast conservation surgery and that metastatic patients receive chemotherapy as primary treatment, chemotherapy as first treatment can be used as a pseudo-marker for more advanced stage tumors.32 This is consistent with our data that showed more Black patients using charity/Medicaid/self-pay/uninsured as insurance compared to White patients and Black patients presenting with more advanced disease and using chemotherapy as first treatment.
Furthermore, in previous studies, being married has been shown to have a survival advantage for patients with cancer. Unmarried women are more likely to be diagnosed with advanced disease and have a higher mortality rate than their married counterparts.33,34 In our study, married patients had significantly shorter TTT and time to second treatment compared to single patients. Also, 47.7% of Black patients were single compared to Hispanic, other, and White patients (38.3, 30.6, and 28.7%, respectively). The longest time to first treatment was noted among single Black patients (41 days) and White patients (39 days) compared to single Hispanic and other patients. The relationship between the marital status of Black patients and their delays in time to first treatment should be further investigated.
Our study demonstrated significant associations between treatment delay and demographic factors previously shown to affect mortality such as race and marital status. However, this study did not look at survival outcomes. Many early studies have shown that delay in the diagnosis and delivery of effective treatments for breast cancer results in advanced states of disease and increased breast cancer mortality. However, recent studies on treatment delay are more mixed and many show no difference in survival related to treatment delay.8,11,35–37 These conflicting results may be explained by differences in patient selection, cutoffs for treatment delay, and availability of biological, clinical, and socioeconomic covariates. Our study is limited to a single institution and does not address comorbid medical conditions or all possible cofounders of tumor characteristics and demographic factors like socioeconomic status. Another possible limitation is the inclusion of all AJCC stages since in metastatic disease, the approach to optimal timing of treatment differs from that in earlier stages and is often decided on an individual basis according to hormonal status, previous treatments, patient symptoms, and preferences.39 Further research is needed to understand the direct impact of treatment delays on clinical outcomes in order to guide potential interventions to reduce treatment delays.
The major strength of our study is that it assesses disparities in both the time to first treatment and the time from first to second treatment in order to better understand treatment delay throughout the entire course of breast cancer care. On multivariate analysis, advanced tumor stage was a significant predictor of longer time from first to second treatment, with AJCC stage III patients having the longest interval (median of 154 days) compared to stage 0 (54.5 days), stage I (59 days), and stage II (79 days). First treatment modality also remained a significant predictor; patients who received chemotherapy first had significantly longer time to second treatment compared to surgical patients. This may simply reflect the fact that it may take longer to recover from the effects of chemotherapy before receiving the second treatment.
Patients who receive chemotherapy as first treatment likely have more advanced disease and thus more perceived urgency to initiate treatment.32 In this study, there was no statistically significant difference in the time to first treatment based on treatment modality in the multivariate model. In locally advanced stage disease, it is not known whether the time from breast cancer diagnosis to neoadjuvant chemotherapy affects survival. A previous study showed that delay (>55 days) in neoadjuvant chemotherapy had an increased risk of death, especially in HER2-positive patients.38 In our study, it is unclear if patients who received chemotherapy as first treatment were being treated for metastatic disease or as neoadjuvant therapy, and this is a question that could be further investigated.
Few studies have evaluated breast cancer disparities in truly multiethnic populations and compared two or more population subsets with White counterparts.12 Given that our study population is a large, multiethnic cohort over an extended time period, the results of this study can be used as a paradigm to better understand breast cancer disparities in other urban and ethnically diverse communities. Similar to previous literature, our results demonstrate that Black patients present more often with charity/uninsured insurance status and more advanced AJCC breast cancer stage, require chemotherapy as first treatment, and have significantly longer TTT delays compared to their non-White counterparts. This study shows that despite the progress in improving access to health care, demographic factors and tumor biology remain the drivers of disparity in time to breast cancer treatment and warrant further investigation.
Conclusion
We demonstrate that Black patients had significantly longer time from diagnosis to treatment compared to other race patients in a setting where the majority of patients are non-White. The study also assesses both the time to first treatment and the time to second treatment, which will help the field better understand treatment delay throughout the continuum of breast cancer care.
Acknowledgment
No funding was received for this research.
Disclosure
The authors report no conflicts of interest in this work.
References
National Cancer Institute [webpage on the Internet]. Cancer of the Breast – SEER Stat Fact Sheets; 2017. National Institutes of Health. Available from: http://seer.cancer.gov/statfacts/html/breast.html. Accessed October 23, 2017. | ||
DeSantis CE, Fedewa SA, Goding Sauer A, Kramer JL, Smith RA, Jemal A. Breast cancer statistics, 2015: convergence of incidence rates between black and white women. CA Cancer J Clin. 2015;66(1):31–42. | ||
Harper S, Lynch J, Meersman SC, Breen N, Davis WW, Reichman MC. Trends in area-socioeconomic and race-ethnic disparities in breast cancer incidence, stage at diagnosis, screening, mortality, and survival among women ages 50 years and over (1987–2005). Cancer Epidemiol Biomarkers Prev. 2009;18(1):121–131. | ||
Cheung MR. Assessing the impact of socio-economic variables on breast cancer treatment outcome disparity. Asian Pac J Cancer Prev. 2013;14(12):7133–7136. | ||
Shavers VL, Brown ML. Racial and ethnic disparities in the receipt of cancer treatment. J Natl Cancer Inst. 2002;94(5):334–357. | ||
Parikh DA, Chudasama R, Agarwal A, et al. Race/ethnicity, primary language, and income are not demographic drivers of mortality in breast cancer patients at a diverse safety net academic medical center. Int J Breast Cancer. 2015;2015:835074. | ||
Bairati I, Jobin E, Fillion L, Larochelle M, Vincent L. Determinants of delay for breast cancer diagnosis. Cancer Detect Prev. 2007;31(4):323–331. | ||
Brazda A, Estroff J, Euhus D, et al. Delays in time to treatment and survival impact in breast cancer. Ann Surg Oncol. 2010;17(Suppl 3):291–296. | ||
Du W, Simon MS. Racial disparities in treatment and survival of women with stage I–III breast cancer at a large academic medical center in metropolitan Detroit. Breast Cancer Res Treat. 2005;91(3):243–248. | ||
Gorin SS, Heck JE, Cheng B, Smith SJ. Delays in breast cancer diagnosis and treatment by racial/ethnic group. Arch Intern Med. 2006;166(20):2244–2252. | ||
Caplan LS, Helzlsouer KJ. Delay in breast cancer: a review of the literature. Public Health Rev. 1993;20:187–214. | ||
Newman LA, Martin IK. Disparities in breast cancer. Curr Probl Cancer. 2007;31:134–156. | ||
Richards M, Westcombe A, Love S, Littlejohns P, Ramirez A. Influence of delay on survival in patients with breast cancer: a systematic review. Lancet. 1999;353(9159):1119–1126. | ||
Whitman S, Ansell D, Orsi J, Francois T. The racial disparity in breast cancer mortality. J Community Health. 2011;36(4):588–596. | ||
Wilkinson GS, Edgerton F, Wallace HJ, Reese P, Patterson J, Priore R. Delay, stage of disease and survival from breast cancer. J Chronic Dis. 1979;32:365–373. | ||
Yu XQ. Socioeconomic disparities in breast cancer survival: relation to stage at diagnosis, treatment and race. BMC Cancer. 2009;9:364. | ||
Deshpande AD, Jeffe DB, Gnerlich J, Iqbal AZ, Thummalakunta A, Margenthaler JA. Racial disparities in breast cancer survival: an analysis by age and stage. J Surg Res. 2009;153(1):105–113. | ||
Gwyn K, Bondy ML, Cohen DS, et al. Racial differences in diagnosis, treatment, and clinical delays in a population-based study of patients with newly diagnosed breast carcinoma. Cancer. 2004;100(8):1595–1604. | ||
Cross CK, Harris J, Recht A. Race, socioeconomic status, and breast carcinoma in the U.S: what have we learned from clinical studies. Cancer. 2002;95(9):1988–1999. | ||
Smith ER, Adams SA, Das IP, Bottai M, Fulton J, Hebert JR. Breast cancer survival among economically disadvantaged women: the influences of delayed diagnosis and treatment on mortality. Cancer Epidemiol Biomarkers Prev. 2008;17(10):2882–2890. | ||
Balduzzi A, Leonardi MC, Cardillo A, et al. Timing of adjuvant systemic therapy and radiotherapy after breast-conserving surgery and mastectomy. Cancer Treat Rev. 2010;36(6):443–450. | ||
Chen Z, King W, Pearcey R, Kerba M, Mackillop WJ. The relationship between waiting time for radiotherapy and clinical outcomes: a systematic review of the literature. Radiother Oncol. 2008;87(1):3–16. | ||
Huang J, Barbera L, Brouwers M, Browman G, Mackillop WJ. Does delay in starting treatment affect the outcomes of radiotherapy? A systematic review. J Clin Oncol. 2003;21(3):555–563. | ||
Plotogea A, Chiarelli AM, Mirea L, et al; Breast Screening Study Group. Factors associated with wait times across the breast cancer treatment pathway in Ontario. Springerplus. 2013;2:388. | ||
Koh HK, Graham G, Glied SA. Reducing racial and ethnic disparities: the action plan from the department of health and human services. Health Aff (Millwood). 2011;30:1822–1829. | ||
Garza MA, Luan J, Blinka M, et al. A culturally targeted intervention to promote breast cancer screening among low-income women in East Baltimore, Maryland. Cancer Control. 2005;12(Suppl 2):34–41. | ||
Karcher R, Fitzpatrick DC, Leonard DJ, Weber S. A community-based collaborative approach to improve breast cancer screening in underserved African American women. J Cancer Educ. 2014;29(3):482–487. | ||
Freedman RA, Virgo KS, He Y, et al. The association of race/ethnicity, insurance status, and socioeconomic factors with breast cancer care. Cancer. 2011;117(1):180–189. | ||
Shi L, Lebrun LA, Zhu J, Tsai J. Cancer screening among racial/ethnic and insurance groups in the United States: a comparison of disparities in 2000 and 2008. J Health Care Poor Underserved. 2011;22(3):945–961. | ||
Halpern MT, Bian J, Ward EM, Schrag NM, Chen AY. Insurance status and stage of cancer at diagnosis among women with breast cancer. Cancer. 2007;110(2):403–411. | ||
Ayanian J, Kohler B, Abe T, Epstein AM. The relation between health insurance coverage and clinical outcomes among women with breast cancer. N Engl J Med. 1993;329(5):326–331. | ||
Charfare H, Limongelli S, Purushotham AD. Neoadjuvant chemotherapy in breast cancer. Br J Surg. 2005;92:14–23. | ||
Aizer AA, Chen M-H, McCarthy EP, et al. Marital status and survival in patients with cancer. J Clin Oncol. 2013;31(31):3869–3876. | ||
Osborne C, Ostir GV, Du X, Peek MK, Goodwin JS. The influence of marital status on the stage at diagnosis, treatment, and survival of older women with breast cancer. Breast Cancer Res Treat. 2005;93(1):41–47. | ||
Caplan L. Delay in breast cancer: implications for stage at diagnosis and survival. Front Public Heal. 2014;2:87. | ||
McLaughlin JM, Anderson RT, Ferketich AK, Seiber EE, Balkrishnan R, Paskett ED. Effect on survival of longer intervals between confirmed diagnosis and treatment initiation among low-income women with breast cancer. J Clin Oncol. 2012;30(36):4493–4500. | ||
Smith EC, Ziogas A, Anton-Culver H. Delay in surgical treatment and survival after breast cancer diagnosis in young women by race/ethnicity. JAMA Surg. 2013;148:516–523. | ||
Sanford R, Lei X, Giordano SH, Tripathy D, Barcenas CH, Chavez-Mac Gregor M. Impact of delayed neoadjuvant systemic chemotherapy on survival outcomes in breast cancer patients. J Clin Oncol. 2016; 34:1038. | ||
Beslija S, Bonneterre J, Burstein HJ, et al; Central European Cooperative Oncology Group (CECOG). Third consensus on medical treatment of metastatic breast cancer. Ann Oncol. 2009;20(11):1771–1785. |
 © 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.



