Back to Journals » Risk Management and Healthcare Policy » Volume 15
Impact of Occupational Risks of Medical Staff on Willingness to Occupational Mobility in COVID-19 Pandemic
Authors Li F , Liu S, Huang H, Tan B
Received 3 February 2022
Accepted for publication 11 April 2022
Published 17 April 2022 Volume 2022:15 Pages 685—702
DOI https://doi.org/10.2147/RMHP.S360892
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr Jongwha Chang
Fuda Li,1 Shuang Liu,1 Huaqian Huang,2 Bangzhe Tan1
1Business School, Hunan Normal University, Changsha, People’s Republic of China; 2Guangdong Polytechnic of Industry and Commerce, Guangzhou, People’s Republic of China
Correspondence: Huaqian Huang, Guangdong Polytechnic of Industry and Commerce, Guangzhou, Guangdong Province, 510510, People’s Republic of China, Tel +86 18022122203, Email [email protected]
Purpose: Medical staff are a crucial resource in the battle against the COVID-19 pandemic but are vulnerable to both SARS-CoV-2 infection and negative psychological outcomes. This study evaluated medical staff’s occupational risks, professional identity, and occupational mobility intention during the pandemic.
Patients and Methods: The questionnaire was anonymous. All respondents were Chinese medical personnel.
Results: Our findings suggest that the professional risks faced by medical professionals can enhance their professional mobility willingness and weaken their professional identity. They cannot only directly enhance their professional mobility willingness but also indirectly strengthen their professional mobility willingness through professional identity. The objective support and subjective support obtained by medical professionals cannot only alleviate the negative impact of occupational risk on professional identity alone but also jointly, and in the process of their joint mitigation, the former has been internalized and absorbed, while the latter has a stronger mitigation effect. The objective support and subjective support obtained by medical professionals can neither alone nor jointly alleviate the direct and positive impact of occupational risk on the willingness of occupational mobility.
Conclusion: The occupational risks faced by medical personnel can improve their willingness to move professionally and weaken their occupational identity. Early screening of high-risk groups for turnover intention among health care workers and more psychosocial health care and physical protection are needed during the COVID-19 pandemic in China.
Keywords: occupational risks, occupational mobility intention, professional identity, social support, COVID-19 pandemic
Introduction
Occupational mobility refers to workers changing their occupations and the process of modifying workers’ roles.1 The occupational mobility intention of medical staff represents their tendency before engaging in occupational mobility. Perceived and handled risks have a significant impact on a series of psychological activities and behavioral intentions.2 Occupational risks also affect a range of attitudes and behaviors related to one’s job.3 Occupational risks include the possibility of stress, stress, danger, and other serious consequences caused by a particular work environment.4 The outbreak of the COVID-19 pandemic started in Wu Han and gradually spread across the country, resulting in the closure of cities, villages, communities, and schools. As domestic outbreaks were effectively controlled, foreign outbreaks (especially in western countries) began, and the risk of foreign imports remained high. When would the global outbreak be effectively contained? Since the crisis began, health care personnel have been working on the front lines in the fight against the virus and have faced challenges at work. Some research clearly shows that hospitals and health care facilities may face major risks for COVID-19 transmission due to airborne spread or indirect (ie, via fomites) transmission.5,6 According to resource protection theory, this concentrated exposure to workplace risks can seriously threaten the resources of health care workers in a short period, thus prompting them to take steps to avoid further loss of resources.7
According to the theory of job search, the main reason for individual career mobility is economic motivation.8,9 Usually, individuals will compare costs and benefits when choosing career mobility. When the benefits of career transition are higher than the costs, individuals are more willing to undertake career mobility.1 During the COVID-19 pandemic, medical staff have repeatedly thought about how to avoid further loss of resources and compare the costs and benefits of occupational mobility, and to ask the question, “Should I continue to remain in this long-criticized profession5?” 2019 Occupational mobility in relation to the coronavirus disease, although not directly producing occupational mobility behaviors, has severely affected the stability of health care workers during the COVID-19 epidemic and is detrimental to the stability of the health care profession and the safety of health care workers.5
Professional identity is an internal incentive for professional development and is the result of overcoming externalities and a sense of alienation in one’s profession and realizing the internal unity of personal value and meaning with professional value and meaning.10,11 It requires professionals to accept and love their career from the bottom of their hearts. The professional identity of medical staff directly affects the desired intensity of their professional growth and relates to emotional experiences, such as the level of job burnout and the index of job happiness.12,13 During the outbreak of the COVID-19 pandemic, many occupational risks faced by medical staff seriously impacted their occupational attitude and reduced their sense of identity with the medical profession, resulting in the desire to seek another career. Some scholars have proven that occupational identity has a significant, negative influence on occupational mobility intention.14,15 Against the background of the COVID-19 pandemic, what role does occupational identity play between the occupational risks faced by medical staff and occupational mobility intention? This requires further discussion.
Social support is the degree to which an individual feels valued, cared for, and respected by his/her family or others, and can be qualitatively divided into objective support (visible or actual support) and subjective support (experienced or emotional support).16,17 During the COVID-19 pandemic, medical staff have received financial support, free online training, subsidies, labor rights, and protection of interests; objective support from family members, friends, relatives, health management departments, industry organizations, and companies; and subjective support such as condolences, care, and psychological counseling. Can these social support factors alleviate the impact of occupational risks, such as viral infection and an uncertain return time on the occupational mobility intention and occupational identity of medical staff? Can the mediating role of occupational identity between these occupational risks and occupational mobility intentions be further mitigated? These questions need to be answered by empirical research.
In summary, this study is based on resource conservation theory and career search theory. In the period of the COVID-19 pandemic, medical staff’s professional risk, professional identity, social support, and professional flow have interfaced with the relationship between the conceptual model. This has occurred through empirical methods validating medical staff’s professional risk regarding the will of the occupation flow mechanism, further exploring career identity in one of the important intermediary roles and two dimensions of social support (objective and subjective support) in one of the important regulatory roles. This paper aims to solve the problem of the relationship between occupational risks and the occupational mobility intention of medical staff, and to provide a reference for the practical problem of maintaining the stability of medical staff under the influence of the COVID-19 pandemic.
Literature Review and Hypotheses
Occupational Risk and Occupational Mobility
Occupational mobility refers to workers changing occupations and the process of changing the role of workers.18 The professional mobility of medical professionals is the process of when they switch to another profession, changing from medical to non-medical jobs. The willingness of medical professionals to move professionally is a tendency or intention before they develop professional mobility.19 Medical professionals are one of the vital forces in promoting the development of the medical industry, and a key factor in enhancing the quality of medical services. During the COVID-19 pandemic, although the professional willingness of medical professionals does not directly result in professional mobility behavior, it seriously affects the stability of medical professional teams, and is not conducive to storing energy for the restoration and development of the medical industry.
People’s perceived and coping risks have a significant impact on a range of psychological activities and behavioral intentions.20 Occupational risks include the possibility of stress, stress, danger, and other serious consequences caused by a specific work environment.11 Generally, any occupation may suffer some kind of loss or danger, such as police threats,12 misdiagnoses,14,15 judges holding someone accountable in the wrong case,21 and so on. According to the theory of resource conservation,22 individuals are driven to protect existing resources and to acquire new ones. If an individual’s resources are threatened or lost and not replenished promptly, he/she will take measures to avoid further loss of resources.22 During the COVID-19 pandemic, medical staff have faced occupational risks such as contracting the virus on the job, being overworked in testing for the virus, and even enduring scolding and beatings from patients. These risks not only threaten the economic sources and physical/mental health of medical professionals, but also cause great professional distress. As a result, medical professionals have to use a great amount of finances, time, and mental resources to respond.23 During the epidemic, to avoid further loss of immunization resources, medical professionals have considered adopting occupational mobility measures such as looking for other career opportunities. According to the theory of career search, the main reason for individual occupational mobility caused by economic motivation is that individuals usually compare costs and benefits when making career mobility choices. When the benefits of career conversion are higher than the costs paid, individuals are more willing to engage in career mobility.24 For other industries, some scholars have discussed the relationship between occupational risks and the willingness to change jobs or quit one’s current job. Occupational risks are an important factor affecting doctors’ job burnout.25 Professional risk has a good predictive effect on turnover intention, and the inherent and social risks in professional risk have a positive effect on the turnover intention of organizational members.26 Based on the above analysis, the following hypotheses are proposed:
H1: In the context of the COVID-19 pandemic, the professional risks faced by medical professionals can enhance their willingness to move professionally.
The Mediating Role of Professional Identity
Professional identity is an intrinsic motivating factor for the development of professional people. It is the result of overcoming the externalities and alienation of the profession and achieving personal value and meaning, as well as the internal unity of professional value and meaning.27 The professional identity of medical staff directly affects the intensity of their career development and is related to burnout and the emotional experience of workplace well-being.28 During the COVID-19 outbreak, medical personnel have needed to meet assist patients and other personnel in the course of their work, and have faced inevitable viral infection and psychological burden during this period.28 Career identity has a significant negative impact on the willingness to move professionally.29,30 Therefore, this study asserts that in the case of the COVID-19 pandemic, the professional risks faced by medical professionals will reduce their professional identity and further increase their willingness to move. Based on the above analysis, the following hypotheses are proposed:
H2: In the context of the COVID-19 pandemic, the occupational risks faced by medical professionals can weaken their professional identity. H3: In the context of the COVID-19 pandemic, the occupational identity of medical professionals mediates between their occupational risks and their willingness to change jobs.
The Moderating Role of Social Support
Social support is the degree to which an individual feels valued, cared for, and respected by his/her family or others16 and can be qualitatively divided into objective support (visible or actual support) and subjective support (experienced or emotional support).17 Scholars have conducted a series of studies on the relationship between social support and mental health.31,32 For example, Park investigated the moderating effect of social support on smartphone use after work and job burnout.33 However, there is still a lack of research on the social support of medical professionals, and only some scholars have explored it. Wang found that medical professionals hope to gain understanding and support from friends and relatives.34 Sochos found that with the improvement of social support, the job burnout of medical professionals decreased correspondingly, and different types of social support have different impacts on the job burnout of medical professionals.35 Wang analyzed the relationship between the job burnout of medical professionals and social support, and proposed suggestions for improving the social support of medical professionals to alleviate job burnout.34 These findings provide a useful reference for this study to explore the social support of medical professionals in the context of the COVID-19 pandemic.
During the COVID-19 pandemic outbreak, medical professionals have mainly obtained support from family, friends, and relatives. Additionally, there is much support from the external environment, such as medical management departments, medical associations, hospitals, and other economic support, free online trainings, subsidies, the protection of the rights and interests of labor, and other forms of objective support and sympathy subjective support, care, and psychological counseling. Social support can protect individuals in a state of stress, which indicates the corresponding buffering effect.16 As the coronavirus outbreak occurred worldwide, medical professionals focused on viral infection, long-term income, interruptions, occupational exposure risk concentration of stress, and medical professional groups to obtain objective and subjective support to ease the influence of stress on flow professional intention and professional identity, and to further ease professional identity in the intermediary role between stress and occupational mobility intention. According to resource conservation theory,22 medical professionals suffering from social pathologies will receive more social, objective, and subjective support from medical staff personnel, and will suffer economic losses and use mental resources to obtain more compensation, making career risk less perceivable. Eliminating the career risk of occupational mobility will directly affect the negative influence and professional identity, and further ease the professional identity in professional risk and the professional intermediary role between flow intention. In the case of the COVID-19 pandemic, medical professionals have received both objective and subjective support from family members, friends, and relatives, medical management departments, medical professionals’ associations, and hospitals, all of which can play a role in the above mitigation process. Subjective support is more meaningful than objective support because although it is not an objective reality, as a perceived psychological reality, it can affect people’s behavior and development.17 Therefore, when objective and subjective support work together in the above mitigation process, objective support (objective reality) needs to be internalized into subjective support (psychological reality) to play a practical mitigation role. Based on the above analysis, the following hypothesis is proposed:
H4: In the context of the COVID-19 pandemic, objective support (H4a) and subjective support (H4b) experienced by medical professionals alone could mitigate the negative impact of occupational risks on occupational identity. H5: In the context of the COVID-19 pandemic, both objective and subjective support for medical professionals could mitigate the negative impact of occupational risks on occupational identity; the latter was more effective. H6: In the context of the COVID-19 pandemic, objective support (H6a) and subjective support (H6b) experienced by medical professionals alone could mitigate the direct positive impact of their occupational risks on their occupational mobility intentions. H7: In the context of the COVID-19 pandemic, both objective and subjective support for medical professionals could jointly mitigate the direct positive impact of their occupational risks on their occupational mobility intentions; the latter had a stronger mitigating effect. H8: In the context of the COVID-19 pandemic, objective support (H8a) and subjective support (H8b) independently alleviated the mediating role of occupational identity between occupational risks and occupational mobility. H9: In the context of the COVID-19 pandemic, objective and subjective support for medical professionals could jointly mitigate the mediating effect of their occupational identity between occupational risks and occupational mobility intention; the latter had a stronger mitigating effect.
Research Model
Based on resource conservation theory and career search theory, medical professionals’ risk regarding occupational flow will influence and further explore career identity, and two dimensions of social support (objective and subjective support) in one of the important intermediary functions and regulation functions will be put forward in the following research model (Figure 1):
 |
Figure 1 Research model. |
Materials and Methods
Measurement Indicators
The following actions were taken to ensure that the measurement tools had good reliability and validity. First, we used international journals to identify reliable scales published by authoritative bodies. As the scales were developed in English-speaking contexts, we used a translation–back-translation process to develop the scales. For this, we invited two Ph.D. students from the United States and the United Kingdom to translate the English scales into Chinese. Following this, two Ph.D. students in the field of management were invited to translate the scales back into English. Finally, two professors of English were invited to compare the three versions of the scales and suggest any changes needed to avoid linguistic ambiguities.
Occupational Risks (OR)
There are great differences in the risks faced by different occupations. The risk scale of other occupations is not suitable for the professional risks of medical staff, and the relevant research on the measurement of professional risks of medical staff is almost absent. Therefore, this study draws on relevant research4 during the outbreak of the COVID-19 pandemic. Five senior medical staff were interviewed using the WeChat and Tencent social tools (QQ), and the medical staff occupational risk scale in the context of the outbreak of the COVID-19 pandemic was developed, including 3 items such as “during the outbreak of the COVID-19 pandemic, you are very worried about having contact with new coronavirus patients in your workplace.” This scale uses a 5-point Likert scale. The higher the score, the greater the professional risk of medical staff.
Occupational Mobility Intention (OMI)
Based on relevant studies,36,37 during the outbreak of the COVID-19 pandemic, this study interviewed 5 senior medical staff with the help of WeChat and QQ, and developed an occupational mobility intention scale for medical staff in the context of the COVID-19 pandemic, including 4 items such as “During the COVID-19 pandemic, you have often considered giving up your medical career.” The scale adopts a 5-point Likert scale; the higher the rating, the stronger the medical staff’s occupational mobility.
Professional Identity (PI)
In this study, based on related research,38,39 the coronavirus was examined during the outbreak. With WeChat and QQ, five senior medical staff members were socially interviewed, and the development of the coronavirus under the outbreak of the medical staff professional identity scale, including “During the COVID-19 pandemic, you believe that the future expectations and goals will be implemented in the medical staff job” and three other entries. The scale adopted a 5-point Likert scale; the higher the rating, the stronger the professional identity of medical staff.
Social Support (SOS)
In this study, based on related research,16,17 social support will be divided into objective support (visible, actual support) and subjective support, emotional support (experience), objective support, OBS including, “During the COVID-19 pandemic, health management department, health organizations and health agencies actively provide you with free online training” and 3 other items; subjective support (SUS) includes three items: “During the COVID-19 pandemic, your family understands, supports and cares for you.” The scale adopted the Likert rating scale; the higher the rating, the more social support the medical staff received.
Data Collection
To collect data for the current study, the heads of different institutions were contacted for permission. Then, doctors from different hospitals, including government, private, and semi-government, were approached. Due to the current condition in the world due to the spread of coronavirus, many doctors were approached through online forms. Informed consent was obtained, and the confidentiality of the information was assured. Demographic sheets and three questionnaires of OR, OMI, PI, and SOS were provided to them to collect data. The Institutional Review Board of Hunan Normal University approved the study design and data collection. All procedures involving human participants were conducted based on the ethical standards of the institutional research committee, the ethical standards of the APA, and the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. Because this study obtained personal information from the participants, their consent was needed. The objectives were communicated to the individuals who participated, and they were also informed of the confidentiality of the information they provided. Participants were also told that they had the option to end the survey if they felt uncomfortable answering any of the questions in the questionnaire. Finally, a total of 272 questionnaires were collected, 183 of which were valid, with an effective response rate of 67.28%. The basic information of the interviewees is shown in Table 1. Among them, all respondents under the age of 20 were hospital interns because urgent nucleic acid tests require so much medical staff that young medical interns are also required to work.
 |
Table 1 Demographic Description of the Sample |
Results
The Common Method Biases Test
This study of potential error variable control for common method bias testing of sample data, namely, using AMOS 22.0 confirmatory factor analysis, and based on this general common method bias as a latent variable model, if containing common method biases, involves latent variables of the fit of the model, is significantly better than not containing common variance deviation of the latent variable model, then the common method bias effect was inspected. According to the inspection results (Table 2 for joining the common method biases latent variables, model fitting index CMIN lower 1.566, CMIN/DF lower 0.005, NFI increased by 0.001, RMSEA lower 0.001, IFI, TLI, CFI had no change), on the whole, joining the common method biases latent variables after the fit of the model was not significantly improved, so this study sample data do not contain serious common method biases.
 |
Table 2 Common Method Biases Test |
Reliability and Validity Analysis
In this study, SPSS 19.0 was used for the reliability test, and the results (Table 3) showed that the Cronbach’s alpha coefficients of six variables (dimensions), such as occupational risks, were all greater than 0.8, indicating that the scale of this study had good reliability.
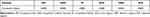 |
Table 3 Reliability Analysis |
AMOS 22.0 was used for confirmatory factor analysis, and the results (Table 4) showed that the main model fitting indices CMIN/DF (1.111) were less than 2, NFI (0.934), IFI (0.993), TLI (0.991), and CFI (0.993) were all greater than 0.9, and RMSEA (0.025) was less than 0.05, indicating that the overall model fitting was ideal. The combination of reliability (CRs) of occupational risks (0.850), occupational mobility intention (0.824), professional identity (0.813), objective support (0.846) and subjective support (0.854) are all greater than 0.7. The average variances (AVEs) of occupational risks (0.653), occupational mobility intentions (0.544), professional identity (0.596), objective support (0.650) and subjective support (0.663) are all greater than 0.5,40 showing that five variables, such as professional risk (dimensions), of the measurement model have good convergent validity. Discriminant validity can be tested by comparing the AVE square root of a variable with the absolute value of all correlation coefficients involved in the variable; that is, if the AVE square root of all variables is greater than the absolute value of all correlation coefficients involved in the corresponding variable, this means there is good discriminant validity between variables.41 The difference between the validity of test results (Table 5), according to the five variables such as professional risk (dimensions) of the AVE square root involved, was greater than the corresponding variable (dimensions) of all the absolute values of the correlation coefficient, the shaded part in Table 5; for example, professional identity (PI) of the AVE square root (0.772) is greater than that involving professional identity (PI) of all relevant coefficients (0.606, 0.763, 0.619, 0.454) of absolute value, so 5 variables such as professional identity (dimensions) have a good difference between validity.
 |
Table 4 Confirmatory Factor Analysis and Convergence Validity Test |
 |
Table 5 Discriminant Validity Test |
Descriptive Statistical Analysis
SPSS 19.0 was used for descriptive statistical analysis and correlation analysis. The results (Table 6) showed that the mean value of five variables (dimensions), including occupational risks, was between 2.56–3.34, and the standard deviation was between 0.878–1.035. The absolute value of skewness (0.141–0.669) and the absolute value of kurtosis (0.426–1.064) of the five variables (dimension) such as occupational risk are all less than 3, and the absolute value of kurtosis (0.426–1.064) are all less than 10, indicating that the sample data are approximately normally distributed on the whole, and the subsequent regression analysis can be carried out smoothly. Occupational risks were significantly and positively correlated with occupational mobility intention (r=0.574, P < 0.05) and negatively correlated with occupational identity (r=−0.508, P < 0.05), objective support (r=−0.375, P < 0.05), and subjective support (r=−0.434, P < 0.05). Occupational mobility intention was negatively correlated with occupational identity (r=−0.617, P < 0.05), objective support (r=−0.537, P < 0.05), and subjective support (r=−0.434, P < 0.05). Occupational identity was significantly and positively correlated with objective support (r=0.506, P < 0.05) and subjective support (r=0.416, P < 0.05). Objective support was positively correlated with subjective support (r=0.314, P < 0.05).
 |
Table 6 Descriptive Statistical Analysis and Correlation Analysis |
Hypothesis Testing
Regression analysis was conducted using PROCESS 3.3 based on SPSS 19.0, and the results are shown in Table 7. Model M1 is used for testing H1, M2, and M6 for testing H2 and H3, M3 and M4 for testing H4a and H4b, and M7 and M8 for testing H5a and H5b. H6a and H6b were tested by a bootstrap test of the mediating effect of mediating variables at different levels (mean-SD, mean, mean+SD)] and the moderating mediating effect index.42 M5 and M9 are complete models, which put two moderators, objective support and subjective support, into the model at the same time.
 |
Table 7 Regression Analysis Results |
Main Effect Test
The positive effect of occupational risks on the willingness of professional mobility was significant (M1, B = 0.487, P < 0.05). That is, the occupational risks faced by medical professionals can enhance their willingness for professional mobility during the COVID-19 pandemic, so H1 was supported.
Mediation Effect Test
Occupational risks had a significant, negative impact on occupational identity (M6, B=−0.470, P < 0.05); that is, during the COVID-19 pandemic, the occupational risks faced by medical professionals weakened their professional identity, so H2 was supported. Compared with Model M1, both occupational risks (independent variable) and occupational identity (mediating variable) were included in M2, and the positive impact of occupational risks on occupational mobility intention was significant (M2, B=0.298, P < 0.05) and decreased, while the negative impact of occupational identity on occupational mobility intention was significant (M2, B=−0.402, P < 0.05). In other words, during the COVID-19 pandemic, the occupational risks faced by medical professionals cannot only directly enhance their occupational mobility willingness, but also indirectly strengthen their occupational mobility willingness through their occupational identity. H3 is true.
To further test the mediating effect of occupational identity, the PROCESS 3.3 macro of SPSS 19.0 was used for the bootstrap test (repeated 5000 times, confidence level 95%). The results (Table 8) showed that the mediating effect of occupational identity was significant (B=0.189, 95% CI =[0.127,0.226]), and H3 was verified again. In addition, the mediating effect of occupational identity accounted for 38.81% of the total effect, indicating that the occupational risks faced by medical professionals during the COVID-19 pandemic had a direct effect on their occupational mobility intentions.
 |
Table 8 Bootstrap Test of Mediating Effect of Occupational Identity (Repeated for 5000 Times) |
Regulation Effect Test
(1) The moderating effect of occupational risks on occupational identity
According to Model M7, the regression coefficient of the interaction between occupational risks and objective support (OR×OBS) was significant (M7, B=0.169, P < 0.05); that is, in the case of the COVID-19 pandemic, the objective support experienced by medical professionals could mitigate the negative impact of occupational risks on occupational identity, so H4a was supported. Objective support for further analysis of how to reduce the negative impact of occupational risks on professional identity, at the same time, using the collocation method and J - N [36], simple slope inspection results (Table 9), revealed that in the collocation method, the simple slope in objective support was significant at low levels (OBS = mean - sd, B = −0.486, P < 0.05), while in objective support, it was not significant at high levels (OBS = mean + sd, B =- 0.152, P < 0.05). In the j-n method, when the objective support is less than the cutoff point, the simple slope is significant (OBS < 0.882, P < 0.05), while when the objective support is greater than the cutoff point, the simple slope is not significant (OBS < 0.882, P < 0.05). To better understand the moderating effect of objective support between occupational risks and occupational identity, SPSS 19.0 was used to produce Figure 2. The regression fitting curve between occupational risks and occupational identity is steeper when objective support is high (OBS=mean+sd) and low (OBS=mean-sd).
 |
Table 9 Simple Slope Test |
 |
Figure 2 The moderating effect of objective support between occupational risks and occupational identity. |
According to Model M8, the regression coefficient of the interaction term of occupational risks and subjective support (OR × SUS) is significant (M8, B = 0.252, P < 0.05). That is, in the context of the COVID-19 pandemic, the subjective support obtained by medical professionals can alleviate the negative impact of occupational risks on professional identity, so H4B is supported. To further analyze how subjective support alleviates the negative impact of occupational risks on occupational identity, a simple slope test was conducted using the point selection method and j-n method [36]. The results (Table 9) demonstrated that in the point selection method, the simple slope was significant at the low level of subjective support (SUS = mean -sd, B = −0.590, P < 0.05), but not significant at the high level of subjective support (SUS = mean + sd, B = −0.076, P >0.05). In the j-n method, the simple slope is significant when subjective support is less than the boundary point (SUS < 0.714, P < 0.05), but not significant when subjective support is greater than the boundary point (SUS < 0.714, P < 0.05). To better understand the moderating effect of subjective support on occupational risks and occupational identity, SPSS 19.0 was used to make Figure 3. The regression curve between occupational risks and professional identity is steeper than that under the high level of subjective support (SUS = mean +sd).
 |
Figure 3 The moderating effect of subjective support between occupational risks and occupational identity. |
M9, relative to the Model M7 and M8 in objective support and subjective support both in terms of regulating variables, professional risk with objective for support interactive items (OR×OBS) of regression coefficients was not significant (M9, B = 0.150, P>0.05) st13, professional risk and subjective support interactive items (OR×SUS) regression coefficient significantly (M9, B = 0.191, P < 0.05), the regulating effect of objective support was internalized absorption. Therefore, in the case of the COVID-19 pandemic, objective and subjective support experienced by medical professionals could jointly mitigate the negative impact of occupational risks on occupational identity, and the latter had a stronger mitigating effect. Thus, H5 was established. For further analysis of how objective and subjective support relieve occupational risks while simultaneously negatively influencing professional identity and the use of the collocation method for the simple slope test [36], the results (Table 9) indicate that a simple slope in objective support and subjective support significantly doubled low levels (OBS = mean - sd, SUS = mean - sd, B = 0.552, P < 0.05), while in objective support and subjective support, combination levels were not significant (OBS = mean + sd, SUS = mean + SD, B = 0.045, P > 0.05). To better understand the joint moderating effect of objective support and subjective support on occupational risks and occupational identity, SPSS 19.0 was used to generate Figure 4. The regression fitting curve between occupational risks and occupational identity is steeper under both objective and subjective support (OBS=mean+sd, SUS=mean+sd) than under both objective and subjective support (OBS=mean-sd, SUS=mean-sd).
 |
Figure 4 Simultaneous moderating effects of objective support and subjective support between occupational risk and occupational identity. |
(2) The moderating effect of occupational risks on occupational mobility intention
According to Model M3, the regression coefficient of the interaction between occupational risk and objective support (OR×OBS) was not significant (M3, B=−0.038, P > 0.05); that is, in the case of the COVID-19 pandemic, the objective support experienced by medical professionals could not mitigate the direct, positive impact of occupational risk on occupational mobility intention, so H6a was not established. According to Model M4, the regression coefficient of the interaction item between occupational risk and subjective support (OR×SUS) was not significant (M4, B=−0.046, P > 0.05); that is, in the case of the COVID-19 pandemic, the subjective support obtained by medical professionals could not mitigate the direct positive impact of occupational risk on occupational mobility intention, so H6b was not valid.
Compared with Models M3 and M4, two moderators, objective support and subjective support, were included in M5. The regression coefficient of the occupational risk and objective support interaction item (OR×OBS) was not significant (M5, B=−0.022, P > 0.05), and the regression coefficient of the occupational risk and subjective support interaction item (OR×SUS) was significant (M5, B=−0.031, P > 0.05). Therefore, in the case of the COVID-19 pandemic, the objective support and subjective support experienced by medical professionals did not jointly mitigate the direct, positive impact of occupational risk on occupational mobility intention, and H7 was not valid.
Testing the Mediating Effects with Regulation
To test the mediating effects of objective support and subjective support on the mediating effects (h8a, h8b) and joint mediating effects (H9) of occupational identity on the relationship between occupational risk and occupational mobility intention, this study used an SPSS 19.0-based process (3.3 macro) to conduct a bootstrap test on the mediating effect and moderating mediating effect index42 of professional identity under different levels of objective and subjective support (mean SD, mean, mean + SD). The results of the bootstrap test with a moderated mediating effect (Table 10) revealed the following:
 |
Table 10 Bootstrap Test with Moderated Mediating Effect (Repeated 5000 Times) |
(1) The mediating effect of professional identity was significant at the low level of objective support (OBS = mean SD, B = 0.144, 95% CI = [0.080, 0.221]), but not at the high level of objective support (OBS = mean + SD, B = 0.045, 95% CI = [- 0.019, 0.124]), and the former was significantly stronger than the latter (Bmean+sd-Bmean-sd = - 0.099, 95% CI = [- 0.197, - 0.025]). In addition, the mediating effect index of objective support was significant (IMM = −0.050, 95% CI = [−0.099, - 0.013]). Therefore, in the case of the COVID-19 pandemic, the objective support of medical professionals can alleviate the intermediary role of professional identity between occupational risk and the willingness to change jobs. Hence, H6a was established.
(2) The mediating effect of professional identity was significant at the low level of subjective support (SUS = mean SD, B = 0.208, 95% CI = [0.123, 0.301]), but not significant at the high level of subjective support (SUS = mean + SD, B = 0.027, 95% CI = [- 0.029, 0.091]), and the former was significantly stronger than the latter (Bmean+sd-Bmean-sd = - 0.181, 95% CI = [- 0.276, - 0.098]). In addition, the mediating effect index of subjective support was significant (IMM = −0.089, 95% CI = [−0.135, - 0.048]). Thus, in the case of the COVID-19 pandemic, the subjective support of medical professionals can alleviate the intermediary role of professional identity between occupational risk and willingness of occupational mobility, and h6b was established.
(3) The mediating effect of professional identity was significant at the low level of objective support and subjective support (OBS = mean - SD, SUS = mean - SD, B = 0.147, 95% CI = [0.071, 0.231]) but not at the high level of objective support and subjective support (OBS = mean + SD, SUS = mean + SD, B = −0.012, 95% CI = [−0.063, 0.043]), and the former was significantly stronger than the latter (Bmean+sd-Bmean-sd = −0.159, 95% CI = [−0.262), −0.069]). In addition, the mediating effect of objective support was not significant (IMMOBS = −0.028, 95% CI = [−0.069, 0.006]), the mediating effect index of subjective support was significant (IMMSUS = −0.051, 95% CI = [−0.087, - 0.018]), and the mediating effect of objective support was absorbed. Thus, in the case of the COVID-19 pandemic, the objective and subjective support experienced by medical professionals can jointly alleviate the intermediary role of occupational identity between occupational risk and occupational mobility intention, and the latter has a stronger mitigation role; thus, H9 is supported.
Discussion and Future Work
Discussion
Based on the theory of resource preservation and the theory of career search, this study is based on the period of the COVID-19 pandemic. This paper constructed a conceptual model of the relationship among professional risk, professional identity, social support, and the professional mobility willingness of medical professionals, thereby verifying the mechanism of the role of professional risk in their professional mobility willingness through empirical methods, and further explored the important intermediary role of professional identity and the important regulation of the two dimensions of social support (objective and subjective support). A questionnaire survey was conducted among Chinese medical personnel, and regression analysis and hypothesis testing were performed using the SPSS 19.0-based process 3.3 macro. The results showed the following:
(1) The professional risks faced by medical professionals can enhance their professional mobility willingness and weaken their professional identity. They cannot only directly enhance their professional mobility willingness, but also indirectly strengthen their professional mobility willingness through professional identity. In addition, the intermediary effect of professional identity accounted for 38.81% of the total effect; hence the direct effect of the professional risk faced by medical professionals on their willingness to move.
(2) The objective and subjective support experienced by medical professionals cannot only alleviate the negative impact of occupational risk on professional identity alone but also jointly, and in the process of their joint mitigation, the former has been internalized and absorbed, while the latter has a stronger mitigation effect.
(3) The objective support and subjective support obtained by medical professionals can neither alone nor jointly alleviate the direct, positive impact of occupational risk on the willingness of occupational mobility.
(4) The objective and subjective support experienced by medical professionals cannot only alleviate the intermediary role of professional identity in career risk and the willingness of career mobility, but also in the process of their joint mitigation role; the former’s mitigation role is internalized and absorbed, and the latter’s mitigation role is stronger.
Conclusion
Based on interactive social support theory and resource conservation theory, this study established a direct effect model and a buffer effect model of social support, constructed a moderated mediation model of the relationship between social support, career mobility intention, career risk and career identity of health care workers during the new coronavirus pneumonia epidemic, and verified the mechanism of social support on the career mobility intention of medical staff during the COVID-19 pandemic through empirical methods. This study expanded the application areas of social support theory and resource conservation theory. With the help of mutual social support theory, it explored the mutual construction process of the joint efforts of supporters and the supported, and established a pioneering direct effect model and a buffer effect model of social support, thus bridging the gap between the traditional separation of the two research states. The study of the relationship between social support and career mobility intentions of health care workers is enriched, providing a new perspective for future research on the relationship between the two.
Future Work
In this study, only from the perspective of the period of the COVID-19 pandemic was the mechanism of the effect of medical professional occupational risk on the willingness of professional mobility investigated. There were many factors affecting the willingness of medical professional occupational mobility, such as job burnout, job satisfaction, and entrepreneurial tendency. Therefore, future research can integrate variables such as job burnout, job satisfaction, and entrepreneurial tendency to build a research model to investigate the mechanism of their effects on the willingness of medical professional career mobility. This study only discussed the regulatory role of social support, but it can also be used as an antecedent variable to affect career identity, so future research can further deepen and expand on this. In addition, there are also some study limitations in this study, as the data investigations were conducted during the development of the new crown epidemic, and it is difficult to determine whether the results of our study would have been the same in the absence of the new crown epidemic.
Ethical Approval and Consent to Participate
Information about the purpose of the study, the nature of voluntary participation, and risks associated with participation are presented in the information section of the survey. This study was approved by the ethics committee of Hunan Normal University. Informed consent was obtained from all participants. Throughout the study, information was kept confidential, and anonymous data were recorded. This study was carried out according to the Declaration of Helsinki.
Acknowledgment
This research was supported by Hunan Key Laboratory of Macroeconomic Big Data Mining and its Application; Hunan Provincial Social Science Achievement Review Committee Project (No. XSP22YBC199); The Outstanding Young Project of Education Department of Hunan Province (No. 21B0051).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Bosch N, Weel BT. Labour-market outcomes of older workers in the Netherlands: measuring job prospects using the occupational age structure. Economist. 2013;161(2):199–218. doi:10.1007/s10645-013-9202-8
2. Heshka JT, Palleschi C, Howley H, Wilson B, PS Wells. A systematic review of perceived risks, psychological and behavioral impacts of genetic testing. Genet Med. 2008;10(1):19–32. doi:10.1097/gim.0b013e31815f524f
3. Quinlan M, Bohle P. Overstretched and unreciprocated commitment: reviewing research on the occupational health and safety effects of downsizing and job insecurity. Int J Health Serv. 2009;39(1):1–44. doi:10.2190/HS.39.1.a
4. Kjøllesdal M, Magnusson K. Occupational risk of COVID-19 by country of birth. A register-based study. J Public Health. 2021;1–7. doi:10.1093/pubmed/fdab362
5. Hou H, Pei Y, Yang Y, et al. Factors associated with turnover intention among healthcare workers during the Coronavirus disease 2019 (COVID-19) pandemic in China. Risk Manag Healthc Policy. 2021;14:4953–4965. doi:10.2147/RMHP.S318106
6. Dinoi A, Feltracco M, Chirizzi D, et al. A review on measurements of SARS-CoV-2 genetic material in air in outdoor and indoor environments: implication for airborne transmission. Sci Total Environ. 2022;809:151137. doi:10.1016/j.scitotenv.2021.151137
7. Bhagwati JN, Srinivasan TN. The general equilibrium theory of effective protection and resource allocation. J Int Econ. 1973;3(3):259–281. doi:10.1016/0022-1996(73)90017-2
8. van Hooft EAJ, Kammeyer-Mueller JD, Wanberg CR, Kanfer R, Job Search BG. Employment success: a quantitative review and future research agenda. J Appl Psychol. 2021;106(5):674–713. doi:10.1037/apl0000675
9. Dall’Ora C, Ball J, Reinius M, Griffiths P. Burnout in nursing: a theoretical review. Hum Resour Health. 2020;18:411. doi:10.1186/s12960-020-00469-9
10. Beijaard D, Meijer PC, Verloop N. Reconsidering research on teachers’ professional identity. Teach Teach Educ. 2004;20(2):107–128. doi:10.1016/j.tate.2003.07.001
11. Armstrong GS, Griffin ML. Does the job matter? Comparing correlates of stress among treatment and correctional staff in prisons. J Crim Just. 2004;32(6):577–592. doi:10.1016/j.jcrimjus.2004.08.007
12. Martin M, Marchand A, Boyer R, Martin N. Predictors of the development of posttraumatic stress disorder among police officers. J Trauma Dissociation. 2009;10(4):451–468. doi:10.1080/15299730903143626
13. Kremer L, Hofman JE. Teachers’ professional identity and burn-out. Res Sci Educ. 1985;34(1):89–95. doi:10.1177/002248718503600612
14. Carlos-María A, Gabriela T, Alberto CJ. Work characteristics, motivational orientations, psychological work ability and job mobility intentions of older workers. PLoS One. 2018;13(4):e0195973. doi:10.1371/journal.pone.0195973
15. Van der Heijden BI, Peeters MC, Le Blanc PM, Van Breukelen JW. Job characteristics and experience as predictors of occupational turnover intention and occupational turnover in the European nursing sector. J Vocat Behav. 2018;108:108–120. doi:10.1016/j.jvb.2018.06.008
16. Cohen S, Wills TA. Stress, social support, and the buffering hypothesis. Psychol Bull. 1985;98(2):310–357. doi:10.1093/restud/rdu037
17. Leskel U, Melartin T, Ryts LH, et al. The influence of major depressive disorder on objective and subjective social support: a prospective study. J Nerv Ment Dis. 2008;196(12):876–883. doi:10.1097/NMD.0b013e31818ec6cf
18. Dlouhy K, Biemann T. Path dependence in occupational careers: understanding occupational mobility development throughout individuals’ careers. J Vocat Behav. 2018;104:86–97. doi:10.1016/j.jvb.2017.10.009
19. Lugito NPH, Kurniawan A, Lorens JO, Sieto NL. Mental health problems in Indonesian internship doctors during the COVID-19 pandemic. J Affect Disord. 2021;6:100283. doi:10.1016/j.jadr.2021.100283
20. Slovic P. Perception of risk. Science. 1987;236(4799):280–285. doi:10.1126/science.3563507
21. Kargl W. Truth, conviction and knowledge in criminal procedures. Arch fur Rechts. 2019;105(2):171–204. doi:10.25162/arsp-2019-0009
22. Halbesleben JRB, Neveu J, Paustian-Underdahl SC, Westman M. Getting to the “COR”: understanding the role of resources in conservation of resources theory. J Manage. 2014;40(5):1334–1364. doi:10.1177/0149206314527130
23. Rizki SA, Kurniawan J, Budimulia P, et al. Knowledge, attitude, and practice in Indonesian health care workers regarding COVID-19. Asia Pac J Public Health. 2021;33(5):662–664. doi:10.1177/10105395211011017
24. Wermeling L. Why social workers leave the profession: understanding the profession and workforce. Adm Soc Work. 2013;37(4):329–339. doi:10.1080/03643107.2012.693057
25. Yuan H, Xu W, Hu H. Young Chinese doctors and the pressure of publication. Lancet. 2013;381(9864):e4. doi:10.1016/S0140-6736(13
26. Chiang Y, Chang Y. Stress, depression, and intention to leave among nurses in different medical units: implications for healthcare management/nursing practice. Health Policy. 2012;108(2–3):149–157. doi:10.1016/j.healthpol.2012.08.027
27. Huang SX, Ham SA, Varghese M, JD Yoon. Moral elevation, physician role models, and selected markers of professional identity formation and well-being: a secondary analysis from two national surveys. South Med J. 2022;115(2):129–135. doi:10.14423/SMJ.0000000000001357
28. Tang M, Sun Y, Zhang K, et al. Associated factors of professional identity among nursing undergraduates during COVID-19: a cross-sectional study. Int J Nurs Sci. 2022;9(1):107–113. doi:10.1016/j.ijnss.2021.09.005
29. Yu H, Guan X, Zheng X, Hou Z. Career adaptability with or without career identity: how career adaptability leads to organizational success and individual career success? J Career Assess. 2018;26(4):717–731. doi:10.1177/1069072717727454
30. Equeter E, Hellemans C. Personal determinants of intention to achieve inter- and intra-organizational mobility. Can J Behav Sci. 2016;48(3):171–181. doi:10.1037/cbs0000043
31. Chen Y, Xu Y. Exploring the effect of social support and empathy on user engagement in online mental health communities. Int J Env Res Pub He. 2021;18:685513. doi:10.3390/ijerph18136855
32. Yang F, Jiang Y. Heterogeneous influences of social support on physical and mental health: evidence from China. Int J Env Res Public Health. 2020;17:683818. doi:10.3390/ijerph17186838
33. Park J, Kim S, Lee H. Effect of work-related smartphone use after work on job burnout: moderating effect of social support and organizational politics. Comput Hum Behav. 2020;105:106194. doi:10.1016/j.chb.2019.106194
34. Wang L, Wang H, Shao S, Jia G, Xiang J. Job burnout on subjective well-being among Chinese female doctors: the moderating role of perceived social support. Front Psychol. 2020;11:435. doi:10.3389/fpsyg.2020.00435
35. Sochos A, Bowers A, Kinman G. Work stressors, social support, and burnout in junior doctors: exploring direct and indirect pathways. J Employ Couns. 2012;49(2):62–73. doi:10.1002/j.2161-1920.2012.00007.x
36. Kramer A, Kramer KZ. The potential impact of the Covid-19 pandemic on occupational status, work from home, and occupational mobility. J Vocat Behav. 2020;119:103442. doi:10.1016/j.jvb.2020.103442
37. Groes F, Kircher P, Manovskii I. The U-shapes of occupational mobility. Rev Econ Stud. 2015;82(2):659–692. doi:10.1093/restud/rdu037
38. Clandinin DJ, Cave MT. Creating pedagogical spaces for developing doctor professional identity. Med Educ. 2008;42(8):765–770. doi:10.1111/j.1365-2923.2008.03098.x
39. Lingard L, Garwood K, Schryer CF, Spafford MM. A certain art of uncertainty: case presentation and the development of professional identity. Soc Sci Med. 2003;56(3):603–616. doi:10.1016/S0277-9536(02)00057-6
40. Fornell C, Larcker DF. Structural equation models with unobservable variables and measurement error: algebra and statistics. J Marketing Res. 1981;18(3):382–388. doi:10.1177/002224378101800313
41. Ou CXJ, Davison RM. Interactive or interruptive? Instant messaging at work. Decis Support Syst. 2011;52(1):61–72. doi:10.1016/j.dss.2011.05.004
42. Hayes AF. An index and test of linear moderated mediation. Multivar Behav Res. 2015;50(1):1–22. doi:10.1080/00273171.2014.962683
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
