Back to Journals » Clinical Ophthalmology » Volume 15
Impact of Laterality on Cumulative Survival in Patients Diagnosed with Retinoblastoma: A Retrospective Cohort Analysis of 1925 Cases in the Surveillance, Epidemiology, and End Results (SEER) Program
Authors Hussain Z
Received 19 December 2020
Accepted for publication 29 January 2021
Published 5 March 2021 Volume 2021:15 Pages 991—1001
DOI https://doi.org/10.2147/OPTH.S298209
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Zain Hussain
Paul L. Foster School of Medicine, Texas Tech University Health Sciences Center, El Paso, TX, USA
Correspondence: Zain Hussain Email [email protected]
Background: Retinoblastoma is an intraocular cancer with potentially severe clinical consequences if left untreated. Diagnostic and clinical management guidelines are strictly dependent on nature of laterality. This analysis aims to characterize the influence of laterality on survival in patients diagnosed with retinoblastoma.
Methods: This retrospective cohort analysis utilized the Surveillance, Epidemiology, and End Results (SEER) program for population-based clinical data from 1975 to 2016, a period of 41 years. Univariable and multivariable Cox regression assessed survival with laterality as the primary independent predictor of mortality. Adjustment for demographical and clinical variables was performed.
Results: N = 1925 patients with a valid cause of death classification. Mean±SD age was 2.35± 2.020 years (range 0– 74). At the time of diagnosis, 819 (42.1%) patients were between 0 and 1 year of age, 469 (24.1%) patients were between 1 and 2 years, 350 (18.0%) patients were between 2 and 3 years, 147 (7.6%) patients were between 3 and 4 years, and 68 (3.5%) patients were between 4 and 5 years of age. The hazard of univariable cause-specific death is 55.6% and 52.9% lower for retinoblastoma patients with left-sided origin and right-sided origin as compared to patients with bilateral origin, respectively (HR = 0.444, CI 0.247– 0.800, p = 0.007; HR = 0.471, CI 0.267– 0.832, p = 0.009). After adjusting for confounding variables, the hazard of other-cause death for retinoblastoma patients is significantly less for left-sided origin (HR = 0.364, CI 0.140– 0.946, p = 0.038) and right-sided origin (HR = 0.190, CI 0.066– 0.549, p = 0.002) as compared to patients with retinoblastomas of bilateral origin.
Conclusion: Prognostication of survival is significantly influenced by the nature of laterality in retinoblastoma. Unilateral retinoblastomas showcase increased promise for long-term cause-specific and other-cause survival compared to cases of retinoblastoma arising from bilateral origin.
Keywords: retinoblastoma, survival, laterality
Introduction
Retinoblastoma is an intraocular cancer with originations from primitive neuroendocrine tissues.1 This malignancy serves the highest incidence of pediatric intraocular cancers with incidences varying from 3.4 to 42.6 cases per million live births.2 It is mostly diagnosed in developed nations.3–5
Remarkable strides in strategic therapeutic implementation of retinoblastomas are discovering the importance of laterality in clinical management guidelines.6 First-line therapy for bilateral retinoblastomas is intravenous chemotherapy (IVC) for prophylaxis against metastasis, secondary recurrences, and authority of intraocular growth.6 One-sided laterality considers alternative treatments, including globe-conserving intra-arterial chemotherapy (IAC).6 Cases of advanced retinoblastomas occurring in third-world countries remain precariously dependent on enucleation for mainstay of therapy.6–8
Although survival of retinoblastoma is shown to correlate with economic development, age at diagnosis, and decade of diagnosis,7,9 survival analyses demonstrating the influence of laterality on mortality are few in number. This SEER analysis highlighted T stage and laterality as the single two covariates significantly influencing survival for overall survival; however, no discrimination for survival in cause-specific and other cause mortality was assessed.10 In addition, incidence rates for diagnoses of retinoblastoma cases seem stable for the past 40 years.9 Interestingly, a retrospective cohort analysis in Jordan at the King Hussein Cancer Center showcased disease stage, laterality, and delay in diagnosis as significant predictors for enucleation.11 To the author’s knowledge, this analysis represents the largest retrospective cohort study comprehensively evaluating the influence of laterality on survival in patients diagnosed with retinoblastoma.
We hereby present a retrospective cohort study utilizing the Surveillance, Epidemiology, and End Results (SEER) Program to characterize the impact of laterality on survival in patients with retinoblastomas with adjustment for age, sex, SEER registry, race/ethnicity, race origin, grade, ICD-O-3 histology/behavior, diagnostic confirmation, chemotherapy recode (yes, no/unk), radiation sequence, reason no cancer-directed surgery, radiation therapy, insurance recode (2007+), and type of follow-up expected.
Methods
This retrospective cohort analysis characterized the influence of laterality on survival in patients with retinoblastoma via utilization of the Surveillance, Epidemiology, and End Results (SEER) Program. SEER is the only open-source, patient de-identified, publicly accessible database funded by the National Cancer Institute (NCI) and the Centers for Disease Control and Prevention (CDC).12 ThIn addition, SEER contains de-identified population-based data for demographical and clinical variables with additional cancer-based survival trends. The “Incidence – SEER 18 Regs Custom Data (with additional treatment fields), Nov 2018 Sub (1975–2016 varying)” database was utilized within the SEER software. This represents a study period of 41 years.
1946 patient cases of retinoblastoma were selected with the “ICCC site recode ICD-O-3/WHO 2008” classification system using the descriptor term “V Retinoblastoma”. Due to the survival-based nature of this study, all patient cases with unknown causes of death (N = 21) were eliminated, culminating in 1925 retinoblastoma cases for analysis.
To properly diagnose the relationship between laterality and survival in patients with retinoblastoma, univariable and multivariable analysis was performed with adjustment for age, sex, SEER registry, race/ethnicity, race origin, grade, ICD-O-3 histology/behavior, diagnostic confirmation, chemotherapy recode (yes, no/unk), radiation sequence, reason no cancer-directed surgery, radiation therapy, insurance recode (2007+), and type of follow-up expected. Due to the preferential incidence of retinoblastoma occurrences in the pediatric population, age was adjusted in multivariable analysis to yield year-to-year and grouped age outcomes.
Descriptive statistics of demographic and clinical characteristics were presented using means and standard deviations for continuous variables and counts and percentages for categorical variables. Kaplan–Meier plots were produced to visually show the unadjusted differences in survival by laterality. Univariable and multivariable Cox proportional hazard models were fit with laterality as the primary independent predictor. Models were fit for both cause-specific and other cause mortality. Cause-specific models define death in survival models by death by cancer; other cause models define death by causes unrelated to cancer. Proportional hazards assumptions were assessed using log-minus-log plots and time-dependent covariate modeling. Statistical noise and redundance was minimized by grouping variables with too few cases together.
Statistical significance was defined as a p-value ≤ 0.05. All analyses were performed in IBM SPSS Version 26.
Results
Table 1 shows the descriptive statistics of N = 1925 patients with a valid cause of death classification. By definition, all patients had malignant (100%) cancer(s) with nearly all patients receiving active follow-up (99.6%). Mean±SD age was 2.35±2.020 years (range 0–74). At the time of diagnosis, 819 (42.1%) patients were between 0 and 1 year of age, 469 (24.1%) patients were between 1 and 2 years, 350 (18.0%) patients were between 2 and 3 years, 147 (7.6%) patients were between 3 and 4 years, and 68 (3.5%) patients were between 4 and 5 years of age. Laterality was evenly distributed with 28.9% (556) of patients incurring bilateral retinoblastomas, 33.9% (652) incurring left-sided, and 35.6% (686) incurring right-sided retinoblastomas. Diagnostic confirmation via clinical diagnosis only occurred in 29 (1.5%) cases with direct visualization without microscopic confirmation in 193 (10.0%) cases, positive histology in 1541 (80.1%) cases, and radiography without microscopic confirmation in 123 (6.4%) cases. Radiation therapy was received via beam radiation in 191 (9.9%) cases, radioactive implants were received in 22 (1.1%) cases, and 1688 (87.7%) cases either did not receive or are not known to have received radiation therapy. Additional demographical and clinical data are showcased in Table 1.
 |  |  |
Table 1 Baseline Demographical and Clinical Characteristics |
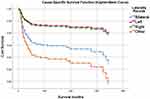
Table 2 shows the univariable Cox regression model results of laterality for both cause-specific survival and other-cause survival models. Univariable results for cause-specific survival show that:
- The hazard of cause-specific death is 55.6% lower for retinoblastoma patients with left-sided origin as compared to patients with bilateral origin (HR = 0.444, CI 0.247–0.800, p = 0.007).
- The hazard of cause-specific death is 52.9% lower for retinoblastoma patients with right-sided origin as compared to patients with bilateral origin (HR = 0.471, CI 0.267–0.832, p = 0.009).
- Figure 1 showcases univariable cause-specific Kaplan–Meier plot.
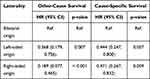 |
Table 2 Univariable Cox Regression Results |
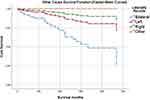
Univariable results for other-cause survival show that:
- The hazard of other-cause death is 63.2% lower for retinoblastoma patients with left-sided origin as compared to patients with bilateral origin (HR = 0.368, CI 0.179–0.756, p = 0.007).
- The hazard of other-cause death is 81.1% lower for retinoblastoma patients with right-sided origin as compared to patients with bilateral origin (HR = 0.189, CI 0.077–0.465, p < 0.001).
- Figure 2 showcases univariable other cause Kaplan–Meier plot.
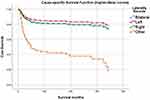
Table 3 shows the multivariable Cox regression results of age for both cause-specific survival and other-cause survival models. Multivariable results for cause-specific survival show that:
- The Log rank (Mantel-Cox) test demonstrated multivariable cause-specific survival distributions stratified by laterality are significantly different (p < 0.001).
- After adjusting for confounding variables, the hazard of cause-specific death for retinoblastoma patients with bilateral origin is significantly different for those aged 1–4 years (HR = 1.850, CI 1.030–3.324, p = 0.040) compared to those aged 0–1 years.
- After adjusting for confounding variables, the hazard of cause-specific death for retinoblastoma patients with left-sided origin (HR = 0.870, CI 0.402–1.879, p < 0.722) and right-sided origin (HR = 1.008, CI 0.501–2.031, p < 0.981) is not significantly different compared to patients with retinoblastomas with bilateral origin.
- When partitioning the age variable to a year-to-year basis, adjusted cause-specific distributions in patients with retinoblastomas of bilateral origin demonstrated increased mortality in patients aged 2 (HR = 2.564, CI 1.233–5.329, p = 0.012) compared to patients aged less than 1 year.
- Figure 3 showcases multivariable cause-specific survival functions.
 |
Table 3 Multivariable Cox Regression Results |
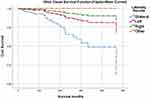
Multivariable results for other cause survival show that:
- The Log rank (Mantel-Cox) test demonstrated multivariable other-cause survival distributions stratified by laterality are significantly different (p < 0.001).
- After adjusting for confounding variables, the hazard of other-cause death for retinoblastoma patients is significantly less for left-sided origin (HR = 0.364, CI 0.140–0.946, p = 0.038) and right-sided origin (HR = 0.190, CI 0.066–0.549, p = 0.002) as compared to patients with retinoblastomas of bilateral origin.
- After adjusting for confounding variables, the hazard of other-cause death for retinoblastoma patients with bilateral origin is significantly less for those who obtained cancer-directed surgery (HR = 0.226, CI 0.068–0.749, p = 0.015) versus those who were not recommended cancer-directed surgery.
Outcomes of multivariable analysis are portrayed in Table 4.
- Figure 4 showcases multivariable cause-specific survival functions.
 |
Table 4 Multivariable Survival Analysis |
Discussion
This study utilized the national SEER database to procure 1925 patients diagnosed with retinoblastomas with a valid cause of death. Our findings highlight the influence of laterality on cause-specific and other cause of death in patients diagnosed with retinoblastomas. To the author’s knowledge, this study is only one of few assessing the influence of laterality on survivorship in those with retinoblastoma. Unilateral retinoblastomas preferentially showcase protective measures against mortality compared to retinoblastomas of bilateral origin. More specifically, our univariable analysis demonstrates a 55.6% reduction in cause-specific mortality and a 52.9% reduction in other cause mortality, as compared to patients with bilateral retinoblastomas. Adjustment for demographical and clinical variables, such as age, sex, race/ethnicity, grade, ICD-O-3 histology/behavior, diagnostic confirmation, chemotherapy recode (yes, no/unk), radiation sequence, reason no cancer-directed surgery, radiation therapy, insurance recode (2007+), and type of follow-up expected were performed. With adjustment, our other cause mortality model maintained a strong stance for preferentiality of survival in patients with left- and right-sided retinoblastomas with an acknowledged 63.6% and 81.0% reduction, respectively, as compared to patients with dual-sided retinoblastomas. Significant differences in survival are observed in unilateral versus bilateral cases of retinoblastoma. In addition, our cohort analysis showcases that retinoblastomas demonstrate no appreciable differences in survival between left-sided and right-sided cohorts. This is observable via KM curves for cause-specific unadjusted and adjusted models.
A current market analysis of the literature supports these findings with genetic influences underpinning the development of unilateral versus bilateral retinoblastomas and treatment modalities specific to either qualities of unilaterality or bilaterality, irrespective of left-sided versus right-sided laterality. Interestingly, while rare trilateral diagnoses have been reported in the literature, the SEER database does not observe these specificities within the encoded laterality variables.
While several studies have established significant survival associations between laterality and mortality,9–11 this study represents the largest retrospective cohort analysis of 1925 patients evaluating this association. In addition, of the few studies that attempt to evaluate this association, even fewer evaluate cause-specific and other cause survival models.9–11 Interestingly, this study demonstrated a nearly 1900% increase in risk of hazards of overall death for bilateral versus unilateral cases of retinoblastoma.10 In contrast, our cause-specific analysis finds a 125% and 112% increase in bilateral cases of retinoblastoma as compared to left- and right-sided cases, respectively. Bifurcation of survival models in cause-specific and other cause models allows greater discrimination of true survival from death by cancer itself versus causes of death not related to cancer diagnosis.
Currently defined mechanisms postulating genetic etiologies shed light on deciphering why unilateral retinoblastomas may prognosticate increased propensity of survival. Prediction of improved clinical outcomes in children is dependent upon cogent identification of RB1 mutations,13,14 which was found in 86% of patients with sporadic bilateral retinoblastomas or those carrying a positive family history of retinoblastoma.15 Cumulative mortality from hereditary retinoblastoma survivors showcased increased mortality from consequent malignancies (25.5%, CI 20.8% to 30.2%) compared to nonhereditary retinoblastoma survivors (1.0%, CI 0.2% to 1.8%),13 indicating genetic inheritance of relevant markers reduces survivorship compared to those with sporadic retinoblastomas.14 Interestingly, while our current understanding of the RB1 mutation demonstrates preferential positive prediction of bilaterality,16 this study showcased findings of germline abnormalities in 11% of sporadic unilateral retinoblastoma, indicating no preclusion of genetic testing in the presence of unilaterality.15 This 2019 survival analysis showcased that out of 924 patients with nonhereditary retinoblastoma, none incurred bilateral origin.14 By extension, through the unilateral nature of nonhereditary retinoblastomas, survivorship increases.14
Preferred choice of therapeutic strategy for retinoblastoma is partially dependent on nature of laterality.6,16 Clinical guidelines highlight preferentiality for intravenous chemotherapy with intermediate consideration for intra-arterial chemotherapy and periocular chemotherapy for bilateral retinoblastomas.6 In contrast, unilateral retinoblastomas demonstrate increased responsiveness to intra-arterial chemotherapy; however, intermediate or minimal consideration for intravenous, periocular, and intravitreal chemotherapy remains.6 Interestingly, our study highlighted a reduction in hazards by 77.4% in patients diagnosed with retinoblastoma of bilateral origin who received cancer-directed surgery compared to patients who were not recommended cancer-directed surgery.
Unique limitations exist for survival studies based on SEER-extracted data. Despite formal diagnoses of a variety of cancers in public hospital systems, patients may seek treatment from clinicians in private practices, which largely do not share patient data with public hospital systems. Due to this discrepancy, patients may be designated with no receipt of treatment (radiation therapy, chemotherapy, surgical excision, etc.) in the SEER database, despite the likelihood of receipt of treatment from private clinicians. In addition, this study removed patients (N = 21) from analysis due to no listed cause of death. The outcomes of this study are strengthened by the sample size, number of survivors, and extraction of clearly interpretable data by virtue of the SEER classification system.
Conclusion
Our retrospective cohort study highlights the positive influence of laterality on cause-specific and other cause survivorship in patients diagnosed with unilateral retinoblastoma compared to patients with bilateral retinoblastoma. Cancer-directed surgery in patients diagnosed with retinoblastoma of bilateral origin demonstrates increased survival compared patients who were not recommended cancer-directed surgery. An improved understanding of the underlying genetic mechanisms related to the retinoblastoma gene, chromosomal aberrations, and epigenetic alterations may shed light on this association; however, additional studies evaluating the unilateral influence of laterality on survival may be needed.
Disclosure
The author reports no conflict of interest in this work.
References
1. Choe C, Bacal DA, O’Brien JM, et al. Retinoblastoma. AAO EyeWiki; June 4, 2020. Available from: https://eyewiki.aao.org/Retinoblastoma.
2. Broaddus E, Topham A, Singh AD. Incidence of retinoblastoma in the USA: 1975–2004. Br J Ophthalmol. 2008;93(1):21–23. doi:10.1136/bjo.2008.138750
3. Jenkinson H. Retinoblastoma: diagnosis and management—the UK perspective. Arch Dis Child. 2015;100(11):1070–1075. doi:10.1136/archdischild-2014-306208
4. Park SJ, Woo SJ, Park KH. Incidence of retinoblastoma and survival rate of retinoblastoma patients in Korea using the Korean national cancer registry database (1993–2010). Invest Ophthalmol Vis Sci. 2014;55(5):2816–2821. doi:10.1167/iovs.14-14078
5. Marees T, van Leeuwen FE, de Boer MR, Imhof SM, Ringens PJ, Moll AC. Cancer mortality in long-term survivors of retinoblastoma. Eur J Cancer. 2009;45(18):3245–3253. doi:10.1016/j.ejca.2009.05.011
6. Shields CL, Fulco EM, Arias JD, et al. Retinoblastoma frontiers with intravenous, intra-arterial, periocular, and intravitreal chemotherapy. Eye. 2013;27(2):253–264. doi:10.1038/eye.2012.175
7. Rodriguez-Galindo C, Wilson MW, Chantada G, et al. Retinoblastoma: one world, one vision. Pediatrics. 2008;122(3):e763–70. doi:10.1542/peds.2008-0518
8. Kivelä T. The epidemiological challenge of the most frequent eye cancer: retinoblastoma, an issue of birth and death. Br J Ophthalmol. 2009;93(9):1129–1131. doi:10.1136/bjo.2008.150292
9. Fernandes AG, Pollock BD, Rabito FA. Retinoblastoma in the United States: a 40-year incidence and survival analysis. J Pediatr Ophthalmol Strabismus. 2018;55(3):182–188. doi:10.3928/01913913-20171116-03
10. Andreoli MT, Chau FY, Shapiro MJ, Leiderman YI. Epidemiological trends in 1452 cases of retinoblastoma from the surveillance, epidemiology, and end results (SEER) registry. Can J Ophthalmol. 2017;52(6):592–598. doi:10.1016/j.jcjo.2017.05.012
11. Al-Nawaiseh I, Jammal HM, Khader YS, Jaradat I, Barham R. Retinoblastoma in Jordan, 2003–2013: ocular survival and associated factors. Ophthalmic Epidemiol. 2014;21(6):406–411. doi:10.3109/09286586.2014.967781
12. Surveillance, Epidemiology, and End Results (SEER) Program. SEER*stat database: incidence – SEER 18 regs custom data (with additional treatment fields), Nov 2018 Sub (1975–2016 varying)-linked to county attributes – total U.S., 1969–2016 Counties, National Cancer Institute, DCCPS, Surveillance Research Program, based on the November 2018 submission. Available from: www.seer.cancer.gov.
13. Yu CL, Tucker MA, Abramson DH, et al. Cause-specific mortality in long-term survivors of retinoblastoma. J Natl Cancer Inst. 2009;101(8):581–591. doi:10.1093/jnci/djp046
14. Kleinerman RA, Tucker MA, Sigel BS, Abramson DH, Seddon JM, Morton LM. Patterns of cause-specific mortality among 2053 survivors of retinoblastoma, 1914–2016. J Natl Cancer Inst. 2019;111(9):961–969. doi:10.1093/jnci/djy227
15. Brichard B, Heusterspreute M, De Potter P, et al. Unilateral retinoblastoma, lack of familial history and older age does not exclude germline RB1 gene mutation. Eur J Cancer. 2006;42(1):65–72. doi:10.1016/j.ejca.2005.07.027
16. Gregersen PA, Olsen MH, Urbak SF, et al. Incidence and mortality of second primary cancers in Danish patients with retinoblastoma, 1943–2013. JAMA Netw Open. 2020;3(10):e2022126. doi:10.1001/jamanetworkopen.2020.22126
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.