Back to Journals » Clinical Interventions in Aging » Volume 13
Impact of frailty on do-not-resuscitate orders and healthcare transitions among elderly Koreans with pneumonia
Authors Choi JY , Kim SW, Yoon SJ , Kang MG , Kim KI, Kim CH
Received 25 July 2018
Accepted for publication 22 September 2018
Published 1 November 2018 Volume 2018:13 Pages 2237—2245
DOI https://doi.org/10.2147/CIA.S181400
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Richard Walker
Jung-Yeon Choi,1 Sun-wook Kim,1 Sol-Ji Yoon,2 Min-gu Kang,1 Kwang-il Kim,1 Cheol-Ho Kim1
1Department of Internal Medicine, Seoul National University Bundang Hospital, Seongnam 463-707, Republic of Korea; 2Department of Internal Medicine, Kangwon National University Hospital Gangwon-Do 200-722, Republic of Korea
Purpose: Pneumonia poses a significant health risk in aging societies. We aimed to elucidate the determinative value of frailty for do-not-resuscitate (DNR) orders in pneumonia patients.
Patients and methods: This was a retrospective cohort study conducted at the Seoul National University Bundang Hospital (SNUBH) in Korea. Medical records of 431 pneumonia patients, aged 65 years and older, who were admitted between June 2014 and May 2015 were analyzed. Patients were categorized into DNR and no-DNR groups.
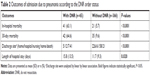
Results: Among the 65 patients (15.1% of pneumonia patients) who completed DNR documents, 24 patients were survived, and 21 patients decided imminent to death (<24 hours before death), with all decisions determined by surrogates. The DNR group tended to be older and frail, with higher rates of renal impairment and malnutrition, and had a lower microbiology detection effort than the no-DNR group. The DNR group used a high number of broad-spectrum antibiotics, experienced high levels of in-hospital (63.1% vs 5.7%, P<0.001) and 30-day (64.6% vs 9.6%, P<0.001) mortality rates, and had prolonged hospital stays (median length of hospital stay, 12 vs 9 days, P=0.020). Frailty was independently associated with DNR status even after adjustment for sepsis, septic shock, and the pneumonia severity index (PSI) score. Frailty also significantly influenced healthcare setting transitions after adjustment for sepsis, septic shock, and the PSI.
Conclusion: We identified the factors associated with DNR orders and their prognoses among elderly Koreans with pneumonia. Frailty was significantly associated with DNR decision and healthcare setting transitions in pneumonia patients.
Keywords: do-not-resuscitate, end-of-life care, frailty index
Introduction
Korea is one of the countries with the highest life expectancies, which poses a significant public health burden. In 2016, pneumonia ranked as the fourth leading cause of death; the mortality rate for pneumonia was 11.6% and 246.8% higher than that in 2015 and 2006, respectively, and a significant proportion of these cases were related to elderly.1 However, few studies have focused on pneumonia treatment in frail, older adults with cognitive and/or physical dysfunction or the prognostic value of frailty in elderly pneumonia patients. The treatment course and the time point at which advance directives should be proposed depend on personal philosophy in valuing independent life and dignity, as well as the ethical decision of patients’ families and physicians. This is an important issue because elderly patients are heterogeneous in terms of overall health, functional capacity, and immunological response. Frailty manifests as a loss of biological reserve among multiple organ systems and vulnerability to possible stress, which reflect physiological age rather than chronological age.2 Various models to identify frailty have been introduced and validated, including the frailty phenotype and frailty index (FI), which calculate the cumulative deficit using 30–40 variables.3–5 FI could be calculated with a simple calculation of the presence of each variable as a proportion of the total. Although some studies have evaluated the association between do-not-resuscitate (DNR) orders and mortality rate, there is a little research on the impact of frailty status on DNR orders in elderly pneumonia patients.6–8
By August 2017, Korea did not have a specific official procedure for DNR documentation. Therefore, several hospitals operate their own guidelines for DNR process and documentation. Seoul National University Bundang Hospital (SNUBH) received consent for the DNR with electronic medical record from the patient’s family by the physician when the patients are in the end-of-life status. From August 2017, with the help of “Law of Determination of Medical Care for Life Prolongation” applied in Korea, depending on the patient’s ability to make decisions and medical conditions, patients or their family members could write “Advanced directive”, “Advanced medical intent”, or “Advanced medical care plan” and could be able to enforce by their family members and one or two doctors.
Some studies have focused on the factors influencing life-prolonging medical treatment or DNR orders for terminally ill patients.9,10 DNR decisions tend to be taken by surrogates, as they are usually determined in the late stages of an illness when patients are unconscious or death is imminent.9,11 We tried to evaluate the decisive clinical characteristics, as well as anthropometric and laboratory findings, in particular frailty, associated with determining DNR orders among older Korean patients with pneumonia in a teaching hospital. We compared initial antibiotic choices, bacteriological findings, clinical courses, and prognoses between patients with and without DNR orders. The impact of frailty on healthcare setting transition in elderly pneumonia patients was also evaluated.
Patients and methods
Patient selection
This retrospective cohort study was conducted at the SNUBH that has 1,300 beds. Patients aged 65 years or older admitted for pneumonia between June 2014 and May 2015 were included in this study. Pneumonia was defined as a inflammatory condition of the lung proven by at least simple chest X-ray with definite fever (>38.0°C). Patients were excluded if they were initially admitted for reasons other than pneumonia or treated with antibiotics for more than 3 days before admission to maintain the homogeneity of the study population and to exclude the possibility of bias due to prehospital treatment.
Patients were categorized into the DNR group and no-DNR groups. The DNR group was defined as the presence of an electronically formatted DNR document during the hospitalization period. Baseline patient characteristics including age, sex, height, weight, comorbidities, and area of residence before admission were collected from electronic medical records, retrospectively. Severity of pneumonia was assessed using the CURB-65 score and pneumonia severity index (PSI) Score at admission.12,13 The conventional definition for sepsis was used as previously described, and septic shock was defined as using vasopressors during the hospitalization period.14 The study protocol was reviewed and approved by the institutional review board (IRB) of the SNUBH, which waived the requirement for informed consent if it is impossible to get the informed consent of the subjects who admitted several years ago, there is no reason to estimate the rejection of the subjects’ consent, and the risk to the subjects is extremely low even if the consent is waived (IRB No, B-1608/357-105). Research data were stored in a password-protected file and kept in a locked laboratory. The data will be maintained for 3 years from the end of research and will be destroyed in accordance with the relevant laws.
Study outcomes
The primary objective of this study was to identify the decisive factors associated with DNR orders in older patients with pneumonia. Baseline characteristics including comorbidities; demographic, anthropometric, and laboratory data; severity indices; and initial antibiotic choice were compared between the DNR group and no-DNR group. The secondary objective was to identify the impact of frailty on healthcare setting transitions (transitioning from care in the home to care in the hospital or a nursing home).
Microbiological diagnoses were performed using sputum, blood, bronchial washing, and pleural effusion. Microbial detection effort was defined as conducting a sputum examination and/or a urinary antigen test. Pneumococcal pneumonia was diagnosed in combination with a positive urinary antigen test. The presence of Mycoplasma pneumoniae was diagnosed only when there were significant findings in a single serum or paired serum test. Drug-resistant bacteria included Pseudomonas aeruginosa, methicillin-resistant Staphylococcus aureus (MRSA), Acinetobacter sp., and extended-spectrum β-lactamase-producing bacteria Enterobacteriaceae.
Discharge sites were categorized as home, a nursing home, and transitional care or long-term care facilities. Survival outcomes were collected by the Ministry of Security and Public Administration on November 4, 2017. Surrogates’ DNR decisions and time differences between in-hospital mortality and the DNR order were also described.
Frailty index
We constructed the FI using a cumulative deficit model including symptoms, signs, abnormal laboratory values, disease status, and disabilities.15 The FI, calculated retrospectively by J-YC as the ratio of deficits present out of the total number of possible deficits at admission, provides a continuous score, ranging from total fitness (0) to total frailty (1).
Our FI comprised 46 characteristics from the electronic medical record system, such as comorbidities, functional abilities, signs and symptoms, laboratory values, and socioeconomic status. Comorbidities included dementia, malignancy, heart failure, cerebrovascular/cardiovascular diseases, liver diseases, and renal diseases. Functional abilities comprised activity limitation, movement limitation, communication ability, awareness state, response to pain, visual impairment, and hearing impairment. Signs and symptoms comprised pain, appetite, sleep disorder, skin condition, orientation of time, person, place, defecation disorder, urinary symptoms, and symptoms of multiple organ systems (respiratory/circulatory/gastrointestinal/neurologic/sensory). Laboratory values comprised hemoglobin, total protein, total cholesterol, and albumin levels. Socioeconomic status comprised education level, marital status, and institutionalization (reside in nursing home, transitional care facility, or any long-term care center) before admission. Additional items included current smoking or drinking status and body mass index (BMI). The cutoff value for frailty (FI≥0.35) was defined using the clinical frailty scale from another study.4,16
Statistical analyses
Statistical analyses were performed using SPSS version 21.0 (IBM Corporation, Armonk, NY, USA). Continuous variables were expressed as mean (SD) or median (interquartile range [IQR]) for variables not normally distributed. Continuous variables were compared using an unpaired t-test. Categorical variables are represented as number (proportion), and the Chi-squared or Fisher’s exact test was used to compare proportions.
Patients admitted two or more times between June 2014 and May 2015 were analyzed separately. ORs were used as a summary measure for the relationship between selected variables and DNR status with logistic regression analysis. The adjustment was made with variables such as age, sex, BMI, comorbidities, residence before admission, and disease severity. Models 1, 2, 3, and 4 were adjusted for sepsis, septic shock, the PSI, and intensive care unit (ICU) admission, respectively. All calculated P-values were two tailed; P<0.05 was considered statistically significant.
Results
Baseline demographics and clinical characteristics of the study population
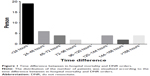
A total of 512 patients and 541 admission cases were enrolled, of whom 29 patients who were admitted twice within the study period were analyzed separately. Fifty-eight admission cases, comprising 57 patients with a diagnosis of pneumonia but who were not admitted for pneumonia and 52 admission cases, comprising 52 patients who were treated with antibiotics for ≥3 days before admission, were excluded from the study. Accordingly, the data from 403 patients and 431 admission cases were used in the analysis, and 69.1% (298 cases) were male with a median age (IQR) of 78 (73–84) years. Among them, 165 cases were institutionalized (admitted at hospital or long-term care facility) before admission to treat pneumonia. The median length of hospital stay (IQR) was 9 (6–15) days. Sixty-five (15.1%) patients made DNR decisions within the hospitalization period. Sixty-two (14.4%) patients died in the hospital. Of the patients in the DNR group who died during the admission period (n=41), the median time between in-hospital mortality and the DNR order (IQR) was 32 (4–107) hours. A total of 165 (38.3%) patients were institutionalized before the admission, and 231 (53.6%), 73 (16.9%), and 65 (15.1%) patients were discharged home, a transitional hospital, and a nursing home, respectively. The median FI (IQR) was 0.34 (0.24–0.43); by using an FI of ≥0.35, 215 (49.9%) patients were defined as having frailty.
Identification of the factors involved in the DNR decision and prognoses of patients in the DNR group
Analyzed data on the relationship among patients’ comorbidities, demographic and laboratory data, frailty and pneumonia severity, and the presence of a DNR order are presented in Table 1. Patients in the DNR group were older and tended to have lower levels of protein, albumin, and cholesterol and higher levels of blood urea nitrogen (BUN) and creatinine. The DNR group needed a vasopressor to maintain blood pressure more frequently and had a higher degree of confused consciousness and severe pneumonia, as defined by the PSI score or CURB-65 score. The FI and prevalence of frailty were higher in the DNR group. Concentrations of C-reactive protein or white blood cells and incidences of comorbidity did not differ between the groups.
Only five (7.7%) patients in the DNR group (n=65) were discharged home and 41 (63.1%) patients died during the admission period, whereas 223 (60.9%) patients in the no-DNR group (n=366) were discharged home and 21 (5.7%) patients died. Both in-hospital (63.1% vs 5.7%, P<0.001) and 30-day mortality rates after discharge (64.6% vs 9.6%, P<0.001) were significantly higher in the DNR group; the length of hospital stay was also longer in this group (median length of hospital stay, 12 vs 9 days, P=0.020; Table 2).
A multiple logistic regression analysis was conducted to determine the association between frailty and the presence of DNR orders, adjusted for age, sex, BMI, comorbidities, institutionalization before admission, and disease severity (sepsis or septic shock or PSI or ICU admission; Table 3). The ORs for the impact of frailty on DNR decisions were 3.559 (95% CI, 1.754–7.219, P<0.001), 2.486 (95% CI, 1.199–5.155, P=0.014), 2.629 (95% CI, 1.259–5.488, P=0.010), and 2.654 (95% CI, 1.301–5.412, P=0.007) after disease severity was adjusted for sepsis, septic shock, PSI, and ICU admission, respectively.
Bacteriological findings, initial choice of antibiotics, and effort in identifying pathologic bacteria
MRSA, Klebsiella sp., Acinetobacter sp., and Candida sp. were more frequently detected in the DNR group, as these were drug-resistant bacteria. The number of patients with unknown bacteriology was higher in the no-DNR group.
As for the initial choice of antibiotics, the rate of monotherapy use did not significantly differ. The frequency of monotherapy using piperacillin/tazobactam was higher in the DNR group, whereas combination therapy with β-lactams and macrolides was more common in the no-DNR group. The frequency with which initial antibiotics were chosen as antipseudomonal or anti-MRSA agents did not differ between the groups. Although the microbial detection effort was high in both groups, a higher rate of positive efforts in detecting bacteria were observed in the no-DNR group (98.6% vs 93.8%, P=0.033; Table 4).
Proxy decision making and time taken to propose DNR decisions
None of the patients with a DNR order provided written informed consent for the DNR by themselves. Surrogates were predominantly patients’ sons or daughters (86.2%) with other proxies including spouses (6.2%) and other family members (7.7%).
Of the 41 patients with a DNR order at the time of death, the DNR order was written within the last 24 hours of life for 19 (46.3%) patients, 2–3 days prior to death for 10 (24.4%) patients, 3–7 days prior to death for 8 (19.6%) patients, and >7 days prior to death for 4 (9.8%) patients. The distribution of the time differences between mortality and the DNR order is shown in Figure 1.
Impact of frailty on healthcare transitions after pneumonia treatment in elderly adults
The impact of frailty on healthcare setting transitions was analyzed among the 266 patients who lived at home before their admission due to pneumonia. Two hundred eight patients were discharged home after treatment of pneumonia; however, 23 and six patients were discharged to transitional care hospitals and nursing facilities, respectively. The multiple logistic regression analysis to identify the impact of frailty on healthcare setting transitions adjusted for age, sex, BMI, comorbidities, institutionalization before admission, and disease severity (sepsis or septic shock or PSI) is shown in Table 3. The ORs for the impact of frailty on healthcare setting transitions were 6.189 (95% CI, 2.142–17.882, P<0.001), 2.251 (95% CI, 1.110–4.566, P=0.025), 3.965 (95% CI, 1.279–12.288, P=0.017), and 5.553 (95% CI, 1.877–16.430, P=0.002) after disease severity was adjusted for sepsis, septic shock, PSI, or ICU admission, respectively.
Discussion
This study described factors impacting physicians’ decisions in proposing DNR and the impact of frailty on healthcare setting transitions in elderly Korean pneumonia patients. Physicians were more likely to propose DNR when the patients were older or frail and had low albumin, protein, and cholesterol levels, high BUN and creatinine levels, confused mental status, and severe pneumonia. Patients who had a DNR order were more likely to have higher in-hospital mortality or 30-day all-cause mortality.
In this study, a DNR decision was taken for 15.1% of the patients with pneumonia. The DNR rate was lower compared to that observed in previous studies conducted in the USA, Canada, and Japan (28.5%–32.6%).17,18 However, DNR rates could vary among institutes or hospitals due to the absence of standardized decision-making processes in the case of pneumonia and differing policies. One study noted that patients from hospital A were 50% more likely to have DNR orders than those from hospital B; in addition, the practice patterns also varied substantially among specialists.19
The prevalence of frailty in this study was 49.9%, and the mean frailty indices were 0.325 in men and 0.353 in women. The prevalence of frailty was higher than that observed in other studies on community-dwelling elderly adults.16 However, the prevalence of frailty was comparable with that observed in studies on patients with atrial fibrillation (48.2%) or non-ST segment elevation myocardial infarction (48.5%).20,21 In our study, the FI was significantly correlated with chronological age (P<0.001 by the Spearman’s rank correlation coefficient) and negative health outcomes such as in-hospital mortality (4.6% vs 24.2%, P<0.001) and 30-day mortality (7.4% vs 28.4%, P<0.001). The variables used in the FI were deficits associated with health status and increasing prevalence with age. The fact that our FI could predict mortality after adjustment for chronological age or pneumonia severity suggest that our FI may represent patients’ actual frailty status to an extent.
In Korea, official legal systems have not been formulated for advanced directives or DNR orders for pneumonia patients. In 1997, a court convicted a family for murder and a hospital for assisting in the crime for removing ventilation from a comatose patient after head trauma. Due to this, and the absence of legislation to defend such legal charges, physicians may hesitate in taking a DNR decision even for patients where reversibility of the condition is very low or absent. Although there was no statistical significance, the proportion of patients with cancer or congestive heart failure was higher in the DNR group; this could be attributed to the fact that malignancies or heart failure are considered irreversible by the public. Therefore, physicians might be more comfortable taking DNR decisions in such patients. In Korea, owing to the aging of the population and increase in the mortality rate associated with pneumonia (5.9% of all deaths), especially among older adults, end-of-life decisions for pneumonia must be discussed by patients, their family members, and physicians. Decisions should then be formally legalized.
Physicians tend to select broad-spectrum antibiotics for the treatment of patients with DNR orders. Piperacillin/tazobactam therapy was selected more frequently for patients with DNR orders, whereas β-lactam+macrolide was chosen more frequently for those without. Broad-spectrum antibiotics were used based on patients’ pneumonia severity or place of residence before admission, irrespective of the DNR status. This result was identical to that observed in another study.18 However, efforts to identify the etiology of microbiology were not as conscientious in the DNR group as in the no-DNR group. This could be due to guardians’ preferences or the physicians’ reluctance to perform invasive procedures, such as catheter aspiration, which could distress patients.
Patients in the DNR group had nearly an eightfold increase in the in-hospital mortality rate and over a sixfold increase in the 30-day mortality rate (64.6% vs 9.6%). Length of hospital stay was also longer in the DNR group. Most patients (93.8%) with DNR orders and 77.3% of those without DNR orders were in risk groups IV and V, respectively, based on the PSI score. This result shows that the patients with DNR orders had a higher severity of pneumonia at baseline. Among patients in the same risk group, mortality rate was much higher in the DNR group (3.9% vs 65.2% in category IV and 11.5% vs 63.2% in category V). It may be assumed that DNR orders proposed by physicians and approved by family members based on comprehensive medical conditions and frailty.
We found that DNR decisions were made by a surrogate, and over two-thirds of these decisions were written on the the day of passing or a day before. This may be attributed to cultural factors, such as the fact that older adults may be hesitant to be informed of their poor prognoses and also due to the presence of acute critical illnesses that were associated with confused mentality in 36.7% of the cases at admission. Delayed DNR decision making observed in this study is in concordance with that noted in another study that focused on identifying the timing of DNR orders for patients with imminent death.9,11 Family members may provide assistance to physicians in articulating patients’ values and their preferred end-of-life care when patients are unable to express themselves; previous studies showed that patients with a family member present were more likely to have a DNR order.22 However, Tsevat et al23 also found that proxies cannot guide the health values of elderly hospitalized patients accurately, and the majority (68.6%) of very old elderly patients were willing to give up at most 1 month of 12 in exchange for excellent health. For these reasons, efforts must be made to speak to very old adults about their health values when they are still healthy and able to understand advanced directives.
Frailty is known to be related to institutionalization or short- and long-term outcomes in hospitalized older adults.24 Our study also found that frailty was associated with healthcare setting transitions to institutions from home after adjustment for age, comorbidities, and pneumonia severity. Even though patients’ age, comorbidities, and pneumonia severity are important clinical factors to determine whether elderly pneumonia patients need intensive or conservative treatment, assessment of physiologic vulnerabilities unique to the elderly, such as frailty, should also be considered to determine the discharge site because function to maintain independent living of frailty elderly could deteriorate after pneumonia treatment.
Our study has some limitations. First, due to the retrospective design, we were unable to identify cases where physicians proposed DNR orders but surrogates rejected them, as well as those where patients decided their DNR preferences before admission; we also could not determine the interphysician factors involved in DNR decision making. A previous study demonstrated that physicians who majored in pulmonary or critical care more frequently suggested DNRs.25 In addition, because patients without close relatives/surrogates could not decide the DNR on their behalf concerned about legal disputes, the DNR decision before the enactment of the relevant statute infringed self-determination. Second, since our study population was reviewed retrospectively and data were collected from only one tertiary hospital, selection bias could not be ruled out, limiting the generalizability of the findings. In addition, eventhough the importance of aspiration pneumonia is further emphasized in frail elderly, we could not identify whether patients had aspiration event or aspiration tendency before pneumonia admission accurately. Third, among the 19 patients who indicated the comment on the use of vasopressors in the DNR document, 3 of 9 non-septic shock patients and 2 of 10 septic shock patients wanted to use vasopressors. Therefore, DNR decision on septic shock (need for the vasopressors to maintain blood pressure) could be influenced as a confounding factor. Also, we failed to adjust the updated definition of sepsis because we targeted patients from 2014 to 2015 and most of them have missing data to calculate Sequential Organ Failure Assessment (SOFA) score.26 Finally, the data on frailty status and pneumonia severity were attained in a cross-sectional manner, and therefore, the FI obtained in our study could be influenced by pneumonia severity and the factors adjusted in this study would not sufficiently reflect the confounding of the frailty status.
Conclusion
We demonstrated clinical and demographical factors in determining DNR orders (older age; frailty; high levels of BUN and creatinine; low levels of protein, albumin, and cholesterol; and severe pneumonia) in elderly pneumonia patients who required admission to the hospital. Although several pneumonia guidelines, depending on the patients’ area of residence when they developed pneumonia, have been released, there is a lack of guidelines for the management of elderly pneumonia patients who have multiple comorbidities and frailty and whose treatment options are limited. There remains a need for more evidence on the comprehensive and effective management of elderly pneumonia patients, inclusive of end-of-life care, as well as their family members and physicians.
Acknowledgment
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author contributions
All authors participated in designing the study concept, statistical analysis, data analysis, and interpretation and drafted the manuscript. They agree to be accountable for all aspects of the work in ensuring that the accuracy or integrity of any part of the work is appropriately investigated. All authors have read and revised and approved this manuscript.
Disclosure
The authors report no conflicts of interest in this work.
References
Korean Statistics [homepage on the Internet]. Korean Statistical Information Service. Cause of Death Statistics; 2016. Available from: http://kostat.go.kr/portal/korea/kor_nw/2/6/1/index.board?bmode=read&aSeq=363268. Accessed 22 September, 2017. | ||
Clegg A, Young J, Iliffe S, Rikkert MO, Rockwood K. Frailty in elderly people. Lancet. 2013;381(9868):752–762. | ||
Fried LP, Tangen CM, Walston J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci. 2001;56(3):M146–M157. | ||
Rockwood K, Song X, Macknight C, et al. A global clinical measure of fitness and frailty in elderly people. CMAJ. 2005;173(5):489–495. | ||
Searle SD, Mitnitski A, Gahbauer EA, Gill TM, Rockwood K. A standard procedure for creating a frailty index. BMC Geriatr. 2008;8:24. | ||
Mehta AB, Cooke CR, Douglas IS, Lindenauer PK, Wiener RS, Walkey AJ. Association of early do-not-resuscitate orders with unplanned readmissions among patients hospitalized for pneumonia. Ann Am Thorac Soc. 2017;14(1):103–109. | ||
Walkey AJ, Weinberg J, Wiener RS, Cooke CR, Lindenauer PK. Association of do-not-resuscitate orders and hospital mortality rate among patients with pneumonia. JAMA Intern Med. 2016;176(1):97–104. | ||
Lo YT, Wang JJ, Liu LF, Wang CN. Prevalence and related factors of do-not-resuscitate directives among nursing home residents in Taiwan. J Am Med Dir Assoc. 2010;11(6):436–442. | ||
Oh DY, Kim JH, Kim DW, et al. CPR or DNR? End-of-life decision in Korean cancer patients: a single center’s experience. Support Care Cancer. 2006;14(2):103–108. | ||
Kim DY, Lee KE, Nam EM, et al. Do-not-resuscitate orders for terminal patients with cancer in teaching hospitals of Korea. J Palliat Med. 2007;10(5):1153–1158. | ||
Bailey FA, Allen RS, Williams BR, et al. Do-not-resuscitate orders in the last days of life. J Palliat Med. 2012;15(7):751–759. | ||
Fine MJ, Auble TE, Yealy DM, et al. A prediction rule to identify low-risk patients with community-acquired pneumonia. N Engl J Med. 1997;336(4):243–250. | ||
Lim WS, van der Eerden MM, Laing R, et al. Defining community acquired pneumonia severity on presentation to hospital: an international derivation and validation study. Thorax. 2003;58(5):377–382. | ||
Bone RC, Balk RA, Cerra FB, et al. Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. The ACCP/SCCM Consensus Conference Committee. American College of Chest Physicians/Society of Critical Care Medicine. Chest. 1992;101(6):1644–1655. | ||
Clegg A, Bates C, Young J, et al. Development and validation of an electronic frailty index using routine primary care electronic health record data. Age Ageing. 2016;45(3):353–360. | ||
Jung HW, Kim SW, Ahn S, et al. Prevalence and outcomes of frailty in Korean elderly population: comparisons of a multidimensional frailty index with two phenotype models. PLoS One. 2014;9(2):e87958. | ||
Marrie TJ, Fine MJ, Kapoor WN, Coley CM, Singer DE, Obrosky DS. Community-acquired pneumonia and do not resuscitate orders. J Am Geriatr Soc. 2002;50(2):290–299. | ||
Oshitani Y, Nagai H, Matsui H. Rationale for physicians to propose do-not-resuscitate orders in elderly community-acquired pneumonia cases. Geriatr Gerontol Int. 2014;14(1):54–61. | ||
Hakim RB, Teno JM, Harrell FE, et al. Factors associated with do-not-resuscitate orders: patients’ preferences, prognoses, and physicians’ judgments. SUPPORT Investigators. Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatment. Ann Intern Med. 1996;125(4):284–293. | ||
Kim SW, Yoon SJ, Choi JY, et al. Clinical implication of frailty assessment in older patients with atrial fibrillation. Arch Gerontol Geriatr. 2017;70:1–7. | ||
Ekerstad N, Swahn E, Janzon M, et al. Frailty is independently associated with short-term outcomes for elderly patients with non-ST-segment elevation myocardial infarction. Circulation. 2011;124(22):2397–2404. | ||
Tschann JM, Kaufman SR, Micco GP. Family involvement in end-of-life hospital care. J Am Geriatr Soc. 2003;51(6):835–840. | ||
Tsevat J, Dawson NV, Wu AW, et al. Health values of hospitalized patients 80 years or older. HELP Investigators. Hospitalized Elderly Longitudinal Project. JAMA. 1998;279(5):371–375. | ||
Chong E, Ho E, Baldevarona-Llego J, et al. Frailty in hospitalized older adults: comparing different frailty measures in predicting short- and long-term patient outcomes. J Am Med Dir Assoc. 2018;19(5):450–457. | ||
Kelly WF, Eliasson AH, Stocker DJ, Hnatiuk OW. Do specialists differ on do-not-resuscitate decisions? Chest. 2002;121(3):957–963. | ||
Singer M, Deutschman CS, Seymour CW, et al. The third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA. 2016;315(8):801–810. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.