Back to Journals » Clinical Interventions in Aging » Volume 17
Impact of Falls Within 3 Months on the Short-Term Prognoses of Elderly Patients in Intensive Care Units: A Retrospective Cohort Study Using Stabilized Inverse Probability Treatment Weighting
Authors Cheng H , Wang Z , Gu WJ, Yang X, Song S, Huang T , Lyu J
Received 2 September 2022
Accepted for publication 10 November 2022
Published 5 December 2022 Volume 2022:17 Pages 1779—1792
DOI https://doi.org/10.2147/CIA.S387148
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Zhi-Ying Wu
Hongtao Cheng,1 Zichen Wang,2 Wan-Jie Gu,3 Xin Yang,1 Simeng Song,1 Tao Huang,2 Jun Lyu2,4
1School of Nursing, Jinan University, Guangzhou, People’s Republic of China; 2Department of Clinical Research, The First Affiliated Hospital of Jinan University, Guangzhou, People’s Republic of China; 3Department of Intensive Care Unit, The First Affiliated Hospital of Jinan University, Guangzhou, People’s Republic of China; 4Guangdong Provincial Key Laboratory of Traditional Chinese Medicine Informatization, Guangzhou, People’s Republic of China
Correspondence: Jun Lyu, Department of Clinical Research, The First Affiliated Hospital of Jinan University, Guangzhou, People’s Republic of China, Tel +86-20-38680061, Email [email protected]
Background: Falls are a major public health problem in the older adults that can lead to poor clinical outcomes. There have been few reports on the short-term prognoses of older critically ill patients, and so we sought to determine the impact of falls on elderly patients in intensive care units (ICUs).
Patients and Methods: This retrospective study of 4503 patients (aged 65 years or older) analyzed data in the Medical Information Mart for Intensive Care-III critical care database. Of those, 2459 (54.6%) older adults are males, and 2044 (45.4%) older adults are females. Based on information from the medical care record assessment forms, patients were classified into the following two groups based on whether they had a fall within the previous 3 months: falls (n=1142) and nonfalls (n=3361). The primary outcomes of this study were 30- and 90-day mortality. Associations between the results of the Kaplan-Meier (KM) survival analysis, Cox proportional-hazards regression models, and subgroup analysis and its outcomes were analyzed using stabilized inverse probability treatment weighting (IPTW).
Results: KM survival curves with stabilized IPTW indicated that 30- and 90-day survival rates were significantly lower in elderly critically ill patients with a history of falls within the previous 3 months than in those patients without a history of falls (all p< 0.001). Multivariate Cox proportional-hazards regression analysis indicated that 30- and 90-day mortality rates were 1.35 times higher (95% confidence interval [CI]=1.16– 1.57, p< 0.001) and 1.36 times higher (95% CI=1.19– 1.55, p< 0.001), respectively, in elderly critically ill patients with a history of falls within the previous 3 months than in those patients without a history of falls.
Conclusion: Experience of falls within the previous 3 months prior to ICU admission increased the risk of short-term mortality and affected the prognoses of elderly patients. Falls should therefore receive adequate attention from clinical healthcare providers and management decision-makers.
Keywords: accidental falls, older adults, inverse probability treatment weighting, intensive care unit
Introduction
Falls are an unexpected event that cannot be controlled by the individual. They are sudden, involuntary, and unintentional changes in the position of the patient, who fall to the ground or to a plane lower than the original position.1 Falls and post-fall-related injuries are a common and growing public health problem among the older adults.2,3 Studies4–7 have found that one-third of those older adults than 65 years fall and half of those older adults than 80 years fall at least once a year; multiple falls occur in about 4% of the older population and are a common cause of disability and death in this population.8 The high incidence and significant cost of falls in older adults places a heavy economic and disease burden on both the patients themselves and healthcare systems, and is a significant cause of unintentional injury in older adults that can lead to poor clinical outcomes and disruption of the health status.9–11
The US seniors population is projected to increase by 55% between 2015 and 2030,12,13 and is projected to account for one-fifth of the US population, or an estimated 84 million seniors older than 65 years by 2050.14 Although falls are considered preventable,10 as society ages, unintentional falls will become a more-significant healthcare problem with a high incidence in older adults. This will undoubtedly affect the quality of life of patients, increase the cost of care for healthcare providers, and increase the burden on family caregivers.7,15–17 It is therefore important to study the incidence of falls, especially among older adults, and the study of falls and post-fall-related hazards in older adults is of great importance for clinical practice and management decision-making.
Previous scientific literatures that we were aware of have mostly focused their attention on falls among elderly patients in general wards or those living in the community/with family, with fewer studies focusing on the short-term survival of critically ill elderly patients with a history of falls within the previous 3 months. Considering the clinical complexity and serious consequences of history of falls in elderly patients in intensive care units (ICUs), this study explored the relationship between falls and short-term mortality in critically ill elderly patients using a retrospective cohort based on a review of globally shared third-party intensive care data, with the aim of providing guidance for clinical diagnosis and care decisions. Based on previous research18,19 and our clinical experts, we presented a basic hypothesis that older patients with a history of falls in the previous 3 months have a higher mortality rate than those without a history of falls.
Materials and Methods
Database
This study was a retrospective cohort study based on a medical intensive care database in the US. The study data were obtained from the Medical Information Mart for Intensive Care-III (MIMIC-III) database.20 This public database, primarily compiled by researchers at the Computational Physiology Laboratory and collaborative research groups of Massachusetts Institute of Technology, contains real medical and nursing care data of inpatients hospitalized at tertiary academic medical centers in Boston (Massachusetts, US). The database system includes all-round diagnoses, and treatment- and nursing-related information, such as demographic application statistics, accurate measurement of bedside vital signs, laboratory test indexes, procedure flows, drug use, caregiver notes, imaging reports, and mortality data (including in-hospital deaths and out-of-hospital follow-ups).21 The database was designed to support various studies in healthcare and is particularly well suited for retrospective cohort study analyses in the area of critical care medicine and nursing because it contains information on out-of-hospital patient deaths. All data are available on the official PhysioNet website (https://mimic.physionet.org/) through extracting the relevant code, and this study is fully reproducible.
Ethics Statement
This study adhered to the provisions of the Declaration of Helsinki, and ethics approval was provided by the Ethics Committee and Institutional Review Board of the First Affiliated Hospital of Jinan University. In addition, we received permission to access the database after completing the “Protecting Human Research Participants” web-based training program from the National Institutes of Health (record ID: 45369280). According to the Health Insurance Portability and Accountability Act (HIPAA), patients in MIMIC-III were de-identified by removing sensitive information and obfuscated their admission year. Accordingly, the need for informed consent was waived. One of the authors (Hongtao Cheng) completed required online training and signed related agreement before accessed the restricted databased.22 Data storage and evaluation were performed by different teams, and all information was approved by the Massachusetts Institute of Technology (Cambridge, MA) and Beth Israel Deaconess Medical Center (Boston, MA). Therefore, this study was an analysis of the third party anonymized publicly available database with pre-existing institutional review board (IRB) approval.
Study Population
In this study, the history of falls within the previous 3 months was the primary classification, considering whether the patient had fallen within 3 months as the primary exposure factor. This information was extracted from the MIMIC-III database using the “chartevents” form with code 227341. It was obtained from the admission or previous health history of critically ill patients assessed by nurses or other clinical workers. Based on the fall histories of the patients, we could easily divide the study population into two study cohorts: one group of those who had fallen within the previous 3 months and another group who had not. The group of older adults who had fallen within the previous 3 months may include two subgroups of patients in this study: those admitted to ICU due to fall-related injuries and those admitted to ICU for reasons other than fall-related injuries.
The 17,523 unique patients whose care assessment information had a history of falls within the previous 3 months (“itemid”=227341) were selected by reviewing their existing event record forms in the MIMIC-III database. The exclusion criteria were patients (i) <65 years old, (ii) with an ICU stay of <1 day (including those who died at their ICU admission), (iii) not admitted to the ICU for the first time, and (iv) with missing height or weight records. Ultimately, 4503 patients were enrolled in the study (Figure 1). Data were collected from the MetaVision data collection system. This database recorded detailed patient admissions during 2008–2012, and all patients within were followed up for a minimum of 90 days.
 |
Figure 1 Inclusion and exclusion flowchart of the study. |
Data Extraction
This study used Structured Query Language23 to extract the following data from the MIMIC-III database: age, sex, race, ICU length of stay (LOS), body mass index (BMI), Sequential Organ Failure Assessment (SOFA) score,24 Glasgow Coma Scale (GCS) score,25 Acute Physiology Score-III (APS-III),26 Braden Scale (BS) score,27 prothrombin time (PT), use of vasopressin and mechanical ventilation, renal replacement therapy (RRT), and comorbidities including sepsis, metastatic cancer, congestive heart failure, water-electrolyte disturbances, and renal failure. The database also includes information on patient deaths (in-hospital, 30-day, and 90-day deaths), liver diseases, paralysis, coagulopathy, diabetes, hypertension, and depression. The database is privacy-protected for the elderly, and the age of patients older than 89 years is listed as 300 years. We replaced these values with a median age of 91.5 years for these patients. The critical-illness-related scores were extracted on the first day of ICU admission. As for the laboratory test indicators, we chose the mean values on the first day of ICU admission. These extracted variables were considered covariates in the data analysis, and we adjusted them using stabilized inverse probability treatment weighting (IPTW), multivariate models, and subgroup analyses. We extracted all variables with no more than 15% missing values, and used the multiple interpolation (MI) method to process missing data.28
Outcomes
The primary outcomes of interest in this study were 30- and 90-day all-cause mortality rates. Survival times were obtained by subtracting the ICU admission time (“intime”) of the patients from their date of death (“dod”). Patients who survived at the end of the follow-up period (30 or 90 days) or with an ICU stay longer than 30 or 90 days were defined as the 30- or 90-day review; otherwise patients were defined as having a mortality status. The secondary outcomes were patient in-hospital mortality and prolonged ICU length of stay. ICU length of stay was calculated by the difference between ICU discharge time (“outtime”) and ICU admission time (“intime”). There is currently no universally accepted definition of a prolonged ICU length of stay.29 In the present study, patients with an ICU length of stay longer than 6.0 days (corresponding to the 75th percentile of the ICU length of stay in the sample) were defined as having an prolonged ICU length of stay.
Statistical Analysis
Characteristics of baseline information for all patients (aged 65 years or older) were grouped according to whether the patient had experienced a fall during the previous 3 months. Continuous variables that conformed to a normal distribution were expressed as mean and SD values, while other continuous variables were expressed as medians with 25th–75th percentiles. Differences between groups were determined using independent-sample t-tests or Wilcoxon rank-sum tests for continuous variables, and chi-square tests for qualitative variables. The balance between the cohort populations in this study was assessed by standardized differences in all baseline covariates, with a threshold of >0.1 indicating an imbalance.30
Kaplan-Meier (KM) survival analysis and Cox proportional-hazards regression models were used to compare the correlations between 30- and 90-day mortality rates in the two patient groups. A Log rank test was used to compare the survival distributions of the two groups, with p<0.05 indicating a significant difference. To adjust for baseline patient characteristics between the two groups to make them comparable between the two study populations, a stabilized IPTW method was used for balance.31 This method is based on propensity scores and statistically adjusts the weights of all observed subjects (exposed and unexposed groups combined) as a “standard population” to control for population differences between groups as much as possible.32 The weighting is adjusted statistically for differences between groups. The weighting in the present study was performed according to the algorithm proposed by Hernan et al33 which is a modification of the calculation method of Robins et al.34 Hernan et al added the treated and untreated rates of the entire study population to the formula to obtain stable weights, and the calculated dummy population was comparable to the actual population, and stabilized IPTW could reduce the occurrence of false positives. To control for potential confounders, hazard ratios (HR) and 95% confidence intervals (CIs) were calculated using multifactorial Cox regression and inverse-probability-weighted posterior Cox regression. Multifactorial logistic regression and inverse-probability-weighted posterior logistic regression were used to analyze the association between fall history within the previous 3 months and the secondary outcomes of in-hospital mortality and prolonged ICU length of stay. A multifactorial logistic regression model was used, and potential confounders were selected as the covariates for the regression model.
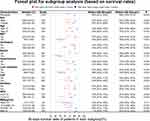
A subgroup analysis was performed in this study to analyze 90-day survival under all subgroups for eleven variables: sex, age, treatment and medication (RRT and mechanical ventilation use), comorbidities (sepsis, hypertension, liver diseases, congestive heart failure and diabetes), critical-illness-related rating scales (GCS), and BMI.
All data were statistically analyzed and processed using R software (version 4.2.0, https://www.r-project.org/). MI was performed using the “mice” package, descriptive analysis and comparison of differences between groups were performed using the “tableone” package, stabilized IPTW was performed using the “IPWsurvival” package, KM survival analysis and Cox proportional-hazards regression model were performed using the “survival” package, and multifactor logistic regression analysis was performed using the “rms” package. Probability values of p<0.05 were considered statistically significant.
Results
Baseline Data of the Study Population
This study selected 4503 patients (aged 65 years or older) for whom comprehensive information was available. Of those, 2459 (54.6%) older adults are males, and 2044 (45.4%) older adults are females. The population was divided into two groups according to whether they had fallen within the previous 3 months: falls (n=1142) and nonfalls (n=3361). Before weighting, baseline information was unbalanced between the two groups in terms of age, sex, GCS score, BMI, APSIII, mechanical ventilation, sepsis, congestive heart failure, hypertension, paralysis, renal failure, liver diseases, water-electrolyte disturbances, and depression (p<0.05). Older adults with a history of falls in the previous three months were older than those not (79.21 years vs 76.57 years, p<0.001). After correcting these covariates using stabilized IPTW, baseline levels were comparable between the two patient groups. There were no significant differences (p>0.05) and the standardized mean difference was <0.1 in both groups (Table 1 and Figure 2).
 |
Table 1 Baseline Characteristics of the Study Population |
Primary and Secondary Outcomes
The population in this study had in-hospital, 30-day, and 90-day all-cause mortality rates of 14.3%, 17.7%, and 23.7%, respectively. The median length of ICU stay was 3 days (25th percentile=1.7 days, 75th percentile=6 days). The results of chi-square and nonparametric tests indicated that there were significant differences (p<0.05) in in-hospital, 30-day, and 90-day all-cause mortality rates, and ICU length of stay between two groups (Table 2). Patients aged 65 years or older with a history of falls in the previous three months had higher in-hospital, 30-day, and 90-day all-cause mortality rates, and ICU length of stay than those not. In addition, chi-square tests indicated that females had a higher mortality rate at 90 days after a fall compared with males in this study (25.8% vs 21.9%, p=0.002) (Supplementary Table 1).
 |
Table 2 Baseline Characteristics of the Primary/Secondary Study Outcomes |
Kaplan-Meier Survival Analysis
KM survival curves indicated differences in the survival probability between older critically ill patients (aged 65 years or older) with a history of falls within the previous 3 months and those without a history of falls (p<0.001). The probabilities of 30-day (Figure 3A) and 90-day (Figure 3B) survival were lower older critically ill patients (aged 65 years or older) with a history of falls than in those without a history of falls. Using stabilized IPTW to correct the KM survival curves, the results remained consistent with the original population, with the differences remaining significant (p<0.001). Older critically ill patients (aged 65 years or older) with a history of falls had lower survival probabilities at both 30 and 90 days (Figure 3C and D).
Cox Proportional-Hazards Regression
This study used Cox proportional-hazards regression models to compare the 30- and 90-day all-cause mortality rates of the two patient groups (aged 65 years or older). Univariate Cox regression analysis (Table 3) indicated that the HRs for 30- and 90-day mortality in older critically ill patients with a history of falls within the previous 3 months were 1.83 (95% CI=1.59–2.12) and 1.86 (95% CI=1.64–2.11), respectively, which differed significantly from those of older critically ill patients without a history of falls (both p<0.001), demonstrating that a history of falls within the previous 3 months is a risk factor for short-term mortality in critically ill elderly patients. Potential confounding factors included age, sex, race, BMI, SOFA score, GCS score, Braden score, APSIII, RRT, vasopressin use, ventilation use, PT, sepsis, metastatic cancer, congestive heart failure, water-electrolyte disturbances, renal failure, liver diseases, paralysis, coagulopathy, hypertension, diabetes, and depression. Statistical analysis indicated that compared with elderly critically ill patients without a history of falls within the previous 3 months, the HRs for 30- and 90-day mortality in those with a history of falls within the previous 3 months were 1.35 (95% CI=1.16–1.57) and 1.36 (95% CI=1.19–1.55), respectively, after correcting for these confounders (both p<0.001).
 |
Table 3 HRs/ORs (95% CIs) for Primary/Secondary Study Outcomes |
We also used a stabilized IPTW method to verify the stability of the findings by calculating a stable weight to put into the model using R software. The weighted results indicated that the HRs for 30- and 90-day mortality in elderly critically ill patients with a history of falls within the previous 3 months were 1.52 (95% CI=1.30–1.78) and 1.54 (95% CI=1.34–1.76), respectively, compared with those patients without a history of falls (both p<0.001). The findings were consistent with the Cox multivariate adjusted-covariate analysis. The results demonstrated that a history of falls within the previous 3 months is an independent risk factor for poor short-term prognosis in critically ill elderly patients.
Logistic Regression Analysis
This study used a logistic regression analysis model to compare the in-hospital mortality and prolonged ICU stays of the two patient groups (aged 65 years or older). Univariate logistic regression analysis (Table 3) indicated that the ORs of in-hospital mortality and prolonged ICU stay in elderly critically ill patients with a history of falls within the previous 3 months compared with those without a history of falls were 1.77 (95% CI=1.48–2.11) and 1.56 (95% CI=1.34–1.81), respectively (both p<0.001), demonstrating that a history of falls within the previous 3 months is a significant risk factor for in-hospital death and prolonged ICU stay in critically ill older patients. Potential confounding factors were controlled for using multifactorial logistic regression. After correcting for confounders, the analysis indicated that the ORs for in-hospital mortality and prolonged ICU stay in critically ill elderly patients with a history of falls within the previous 3 months compared with those without were 1.54 (95% CI=1.24–1.91) and 1.84 (95% CI=1.54–2.21), respectively (both p<0.001). We also used a stabilized IPTW method to verify the stability of these findings. The weighted results indicated that the ORs of in-hospital mortality and prolonged ICU stay in elderly critically ill patients with a history of falls within the previous 3 months compared with those without were 1.58 (95% CI=1.33–1.89) and 1.85 (95% CI=1.60–2.14), respectively (both p<0.001). These findings were consistent with those of the logistic multivariate adjusted-covariate analysis. The results demonstrated that a history of falls within the previous 3 months is an independent risk factor for in-hospital death and prolonged ICU stay in critically ill elderly patients.
Subgroup Analysis
Patients in both groups were further analyzed according to sex, age, treatment and medication (RRT and mechanical ventilation use), comorbidities (sepsis, hypertension, liver diseases, congestive heart failure and diabetes), critical-illness-related rating scales (GCS), and BMI. KM survival analysis was used to compare the 90-day survival probabilities of the two study groups according to different subgroups, and the results were presented as forest plots. The forest plots provided a clear and concise summary of the differences in 90-day survival rates for the populations in each subgroup. For 90-day survival, there was no significant difference in survival between the two populations when RRT was used, sepsis was present, liver diseases were present, and the BMI was <18.5 kg/m2 (Figure 4). We found an interesting fact that the 90-day survival rates were higher in overweight or obese elderly critically ill patients than in underweight individuals. In addition, for all older adults, multivariate Cox proportional-hazards regression analysis indicated that compared with underweight older patients, the HRs for overweight and obese (90-day mortality) in older adults were 0.71(95% CI=0.53 – 0.95, p=0.021) and 0.69 (95% CI=0.51 – 0.94, p=0.017), respectively (Supplementary Table 2).
Discussion
Considering that falls are strongly associated with short-term prognoses in critically ill elderly patients, this study conducted a retrospective population-based cohort study of 4503 critically ill patients (aged 65 years or older) selected from a large intensive care database and investigated the effect of a history of falls within the previous 3 months on short-term prognoses and ICU length of stay in these patients. Stabilized inverse-probability-weighted KM curves indicated that the in-hospital and 30- and 90-day mortality rates were significantly higher in elderly patients who had fallen in the previous 3 months than in those who had not fallen. After correcting for potential confounders, multifactorial Cox proportional-hazards regression analysis indicated that compared with elderly critically ill patients without a history of falls, the HRs for 30- and 90-day mortality in those patients with a history of falls within the previous 3 months were 1.35 (95% CI=1.16–1.57, p<0.001) and 1.36 (95% CI=1.19–1.55, p<0.001), respectively. Multifactorial logistic regression analysis indicated that the ORs of in-hospital mortality and prolonged ICU stay in elderly critically ill patients with a history of falls within the previous 3 months compared with those without a history of falls were 1.54 (95% CI=1.24–1.91, p<0.001) and 1.84 (95% CI=1.54–2.21, p<0.001), respectively.
The present results are similar to those of many previous studies,3,35–37 although the subjects of those studies were elderly in general wards or the community. The possible reason for the results were that falls can lead to fractures, soft tissue injuries, brain injuries, and hip fractures, which can greatly affect the physical and mental health of older adults.38–40 Anxiety and fear after a fall can reduce the physical mobility of older adults, restricting their range of motion and decreasing their quality of life and self-confidence in their activities of daily living.41 For critically ill patients, previous research42–44 found that early mobilization could improve the patient’s respiratory function, increase central and peripheral blood perfusion, promote muscle metabolism, and also boost the patient’s confidence in overcoming the disease. Anxiety and fear after a fall can impact on early mobilization of patients, which may be related to a high mortality. In addition, due to the special clinical characteristics of the older adults,45,46 the combined effects of various underlying diseases, physical and mental changes associated with aging, medication use, and the unfamiliar environment of ICUs can result in even a relatively minor fall having serious clinical consequences for the patient, resulting in poor short-term prognoses and prolonged ICU stays.
Quantifying fall mortality rates in different subgroups of the population can help to identify the medical care needs of these populations and to develop appropriate prevention programs for specific target groups. A subgroup analysis was therefore performed on the two patient groups in this study. Previous studies11,47,48 have found that more females than males die from falls. We also drew the same conclusion: females had a higher mortality rate at 90 days after a fall compared with males (25.8% vs 21.9%, p=0.002). This may be related to the larger amount of sex hormones and higher incidence of osteoporosis in female patients. The results of the subgroup analysis indicated that 90-day survival was less likely in the falls group than in the nonfalls group in both males (67% vs 81%, p<0.001) and females (65% vs 78%, p<0.001). This findings suggests that clinical practitioners need to pay equal attention to male and female patients who experience falls in the previous three months. We divided the study population into four categories according to patient BMI:49 underweight (BMI <18.5 kg/m2), normal weight (18.5 ≤BMI < 25 kg/m2), overweight (25 ≤BMI < 30 kg/m2), and obese (BMI >30 kg/m2). The 90-day survival rates were higher in overweight or obese elderly critically ill patients than in underweight individuals. A possible reason is that critically ill patients have accelerated fat mobilization and reduced fat stores when fat becomes the main source of energy in the body during stressful conditions such as trauma, and overweight patients can use their stored fat to resist this adverse effect.50 The present study also found a lower GCS score (≤12) on the first day of ICU admission in patients who fell compared with those who did not, which suggests a lower 90-day survival rate (53% vs 73%, p<0.001). This finding could help medical caregivers to identify high-risk patients.
There have been extensive reports of fall prevention measures for elderly patients, such as exercise, balance training, and multicomponent interventions.51–53 Notably, in our study, patient fall histories were collected through nurses or other clinical workers asking patients or family members. Critical care clinicians need to pay extra attention to the assessment and collection of patient admission information; even though these tasks are simple and basic, they are still have significant clinical implications. A good health assessment helps to provide a comprehensive and holistic understanding of the condition of a patient, provides a basis for developing individualized care plans and interventions, and can minimize the adverse effects of falls on the short-term prognoses of critically ill elderly patients.
Falls of the older adults are one of the primary geriatric syndromes and clear indicators of fragility in the older adult population.54 Previous studies reported that every year, an estimated 30–40% of older adults (aged 65 years or older) will fall at least once.54–56 In our cohort, 25.4% (1142/3361) of the older adults had a history of falls within the previous 3 months, which is somewhat different from the data. This is mainly because we focused on whether fell occurred in older adults within the previous 3 months before ICU admission. Considering the clinical complexity and the different proportion of falls in the older population, we used a stabilized (inverse probability treatment weighting) IPTW method to control for potential confounders. IPTW is a method used to account for missing and selection bias due to non-random selection of observations or non-random absence of population information. The method can modify the analysis by weighting the study population, so that it has the probability of being selected. Stabilized IPTW could also reduce the occurrence of false positives.
This study was based on a large and diverse population in the MIMIC-III database, but there were several limitations. Firstly, the study was based on data of inpatients treatment at tertiary academic medical centers in Boston. Therefore, we would expect the intensity of treatment and the complexity of management of patients in these centers to be higher than in other secondary (nontertiary) or non-academic hospitals in the US, which limits the generalizability of the conclusions. Moreover, such sample may not be representative of ICU populations in other countries, and extrapolation should be cautious. Secondly, the patients were divided into two groups according to their preadmission status based on the exposure factor of the history of falls within the previous 3 months, and because this was a retrospective study of a public database, it was inevitably limited by the extent to which the database could be used, and there were unmeasured confounding factors in the study, such as the patient’s MORSE Fall Risk Factor Assessment Scale.57 We did not assess the physical restraint on patients during their ICU stay or other factors such as their dietary nutrition, which may have led to bias in the study findings. Thirdly, we obtained mortality data from the MIMIC-III database. However, these data only included the date of death from the hospital or Social Security Administration statistics, calculated as all-cause patient mortality, and we were unable to analyze deaths due to specific diseases. Fourthly, the lack of any information in this database related to the outcomes of physical function and functional status of critically ill survivors after hospital discharge limited our ability to determine the final level of psychosocial adjustment and quality of life for patients, factors that could also potentially affect survival.58 Finally, it is of great significance that being aware of considering older adults with history of falls within the previous 3 months. Except for this period, older adults who fall may be omitted, and the full impact of history of falls on outcomes is unclear. Further prospective study are needed to verify the findings. Despite these limitations, this study explored the association between history of falls and short-term mortality of older adults in intensive care units. Utilizing this knowledge will help to advance clinical practices in improving the care of older adults with a history of falls in the previous three months in intensive care units.
In the future we plan to conduct a multicenter prospective cohort study to collect patient information as comprehensively as possible in order to obtain more accurate results to better guide clinical diagnoses and care practices.
Conclusion
We have conducted a retrospective analysis based on the MIMIC-III critical care database to determine the impact of a history of falls within the previous 3 months on critically ill elderly patients, taking into account the specificity of the critical care setting and patients. The inverse-probability-weighted KM survival analysis indicated that older critically ill patients with a history of falls within the previous 3 months had significantly higher in-hospital and 30- and 90-day mortality rates than those without a history of falls (all p<0.001). Multifactorial Cox proportional-hazards regression analysis indicated that 30- and 90-day mortality rates were 1.35 times higher (95% CI=1.16–1.57, p<0.001) and 1.36 times higher (95% CI=1.19–1.55, p<0.001), respectively, in older critically ill patients with a history of falls within the previous 3 months than in those without a history of falls. Subgroup analyses were used to summarize the differences in 90-day survival between the two patient groups according to different subgroups. These findings will inform clinical management and decision-making.
Data Sharing Statement
MIMIC-III database analyzed in this study is available on the PhysioNet repository.
Funding
The study was supported by Guangdong Provincial Key Laboratory of Traditional Chinese Medicine Informatization (2021B1212040007).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Lamb SE, Jørstad-Stein EC, Hauer K, Becker C. Development of a common outcome data set for fall injury prevention trials: the prevention of falls network Europe consensus. J Am Geriatr Soc. 2005;53(9):1618–1622. doi:10.1111/j.1532-5415.2005.53455.x
2. Hu G, Baker SP. An explanation for the recent increase in the fall death rate among older Americans: a subgroup analysis. Public Health Rep. 2012;127(3):275–281. doi:10.1177/003335491212700307
3. Padrón-Monedero A, Damián J, Pilar Martin M, Fernández-Cuenca R. Mortality trends for accidental falls in older people in Spain, 2000–2015. BMC Geriatr. 2017;17(1):276. doi:10.1186/s12877-017-0670-6
4. Hornbrook MC, Stevens VJ, Wingfield DJ, Hollis JF, Greenlick MR, Ory MG. Preventing falls among community-dwelling older persons: results from a randomized trial. Gerontologist. 1994;34(1):16–23. doi:10.1093/geront/34.1.16
5. Hausdorff JM, Rios DA, Edelberg HK. Gait variability and fall risk in community-living older adults: a 1-year prospective study. Arch Phys Med Rehabil. 2001;82(8):1050–1056. doi:10.1053/apmr.2001.24893
6. Sherrington C, Fairhall NJ, Wallbank GK, et al. Exercise for preventing falls in older people living in the community. Cochrane Database Syst Rev. 2019;1(1):Cd012424. doi:10.1002/14651858.CD012424.pub2
7. Swift CG, Iliffe S. Assessment and prevention of falls in older people--concise guidance. Clin med. 2014;14(6):658–662. doi:10.7861/clinmedicine.14-6-658
8. Liu-Ambrose T, Davis JC, Best JR, et al. Effect of a home-based exercise program on subsequent falls among community-dwelling high-risk older adults after a fall: a randomized clinical trial. JAMA. 2019;321(21):2092–2100. doi:10.1001/jama.2019.5795
9. Haagsma JA, Olij BF, Majdan M, et al. Falls in older aged adults in 22 European countries: incidence, mortality and burden of disease from 1990 to 2017. Inj Prev. 2020;26(Supp 1):i67–i74. doi:10.1136/injuryprev-2019-043347
10. Ye P, Er Y, Wang H, et al. Burden of falls among people aged 60 years and older in mainland China, 1990–2019: findings from the Global Burden of Disease Study 2019. Lancet Public Health. 2021;6(12):e907–e918. doi:10.1016/S2468-2667(21)00231-0
11. Burns ER, Stevens JA, Lee R. The direct costs of fatal and non-fatal falls among older adults - United States. J Safety Res. 2016;58:99–103. doi:10.1016/j.jsr.2016.05.001
12. Stevens JA, Corso PS, Finkelstein EA, Miller TR. The costs of fatal and non-fatal falls among older adults. Inj Prev. 2006;12(5):290–295. doi:10.1136/ip.2005.011015
13. Shumway-Cook A, Ciol MA, Hoffman J, Dudgeon BJ, Yorkston K, Chan L. Falls in the medicare population: incidence, associated factors, and impact on health care. Phys Ther. 2009;89(4):324–332. doi:10.2522/ptj.20070107
14. Wiener JM, Tilly J. Population ageing in the United States of America: implications for public programmes. Int J Epidemiol. 2002;31(4):776–781. doi:10.1093/ije/31.4.776
15. Tricco AC, Thomas SM, Veroniki AA, et al. Comparisons of interventions for preventing falls in older adults: a systematic review and meta-analysis. JAMA. 2017;318(17):1687–1699. doi:10.1001/jama.2017.15006
16. Stenhagen M, Ekström H, Nordell E, Elmståhl S. Accidental falls, health-related quality of life and life satisfaction: a prospective study of the general elderly population. Arch Gerontol Geriatr. 2014;58(1):95–100. doi:10.1016/j.archger.2013.07.006
17. Scuffham P, Chaplin S, Legood R. Incidence and costs of unintentional falls in older people in the United Kingdom. J Epidemiol Community Health. 2003;57(9):740–744. doi:10.1136/jech.57.9.740
18. Liu SW, Obermeyer Z, Chang Y, Shankar KN. Frequency of ED revisits and death among older adults after a fall. Am J Emerg Med. 2015;33(8):1012–1018. doi:10.1016/j.ajem.2015.04.023
19. Majdan M, Mauritz W. Unintentional fall-related mortality in the elderly: comparing patterns in two countries with different demographic structure. BMJ Open. 2015;5(8):e008672. doi:10.1136/bmjopen-2015-008672
20. Johnson AE, Pollard TJ, Shen L, et al. MIMIC-III, a freely accessible critical care database. Sci Data. 2016;3:160035. doi:10.1038/sdata.2016.35
21. Yang J, Li Y, Liu Q, et al. Brief introduction of medical database and data mining technology in big data era. J Evid Based Med. 2020;13(1):57–69. doi:10.1111/jebm.12373
22. Xu J, Tong L, Yao J, et al. Association of sex with clinical outcome in critically ill sepsis patients: a retrospective analysis of the large clinical database MIMIC-III. Shock. 2019;52(2):146–151. doi:10.1097/SHK.0000000000001253
23. Wu WT, Li YJ, Feng AZ, et al. Data mining in clinical big data: the frequently used databases, steps, and methodological models. Military Med Res. 2021;8(1):44. doi:10.1186/s40779-021-00338-z
24. Lambden S, Laterre PF, Levy MM, Francois B. The SOFA score-development, utility and challenges of accurate assessment in clinical trials. Critical Care. 2019;23(1):374. doi:10.1186/s13054-019-2663-7
25. Teasdale G, Maas A, Lecky F, Manley G, Stocchetti N, Murray G. The glasgow coma scale at 40 years: standing the test of time. Lancet Neurol. 2014;13(8):844–854. doi:10.1016/S1474-4422(14)70120-6
26. Knaus WA, Draper EA, Wagner DP, Zimmerman JE. APACHE II: a severity of disease classification system. Crit Care Med. 1985;13(10):818–829. doi:10.1097/00003246-198510000-00009
27. Bergstrom N, Braden BJ, Laguzza A, Holman V. The braden scale for predicting pressure sore risk. Nurs Res. 1987;36(4):205–210. doi:10.1097/00006199-198707000-00002
28. Morris TP, White IR, Royston P. Tuning multiple imputation by predictive mean matching and local residual draws. BMC Med Res Methodol. 2014;14:75. doi:10.1186/1471-2288-14-75
29. Huang YC, Huang SJ, Tsauo JY, Ko WJ. Definition, risk factors and outcome of prolonged surgical intensive care unit stay. Anaesth Intensive Care. 2010;38(3):500–505. doi:10.1177/0310057X1003800314
30. Austin PC. Some methods of propensity-score matching had superior performance to others: results of an empirical investigation and Monte Carlo simulations. Biom J. 2009;51(1):171–184. doi:10.1002/bimj.200810488
31. Austin PC, Stuart EA. Moving towards best practice when using inverse probability of treatment weighting (IPTW) using the propensity score to estimate causal treatment effects in observational studies. Stat Med. 2015;34(28):3661–3679. doi:10.1002/sim.6607
32. Xu S, Ross C, Raebel MA, Shetterly S, Blanchette C, Smith D. Use of stabilized inverse propensity scores as weights to directly estimate relative risk and its confidence intervals. Value Health. 2010;13(2):273–277. doi:10.1111/j.1524-4733.2009.00671.x
33. Hernán MA, Brumback B, Robins JM. Marginal structural models to estimate the causal effect of zidovudine on the survival of HIV-positive men. Epidemiology. 2000;11(5):561–570. doi:10.1097/00001648-200009000-00012
34. Robins JM, Hernán MA, Brumback B. Marginal structural models and causal inference in epidemiology. Epidemiology. 2000;11(5):550–560. doi:10.1097/00001648-200009000-00011
35. Hagiya H, Koyama T, Zamami Y, et al. Fall-related mortality trends in older Japanese adults aged ≥65 years: a nationwide observational study. BMJ open. 2019;9(12):e033462. doi:10.1136/bmjopen-2019-033462
36. Wu H, Mach J, Le Couteur DG, Hilmer SN. Fall-related mortality trends in Australia and the United Kingdom: implications for research and practice. Maturitas. 2020;142:68–72. doi:10.1016/j.maturitas.2020.07.008
37. Galet C, Zhou Y, Eyck PT, Romanowski KS. Fall injuries, associated deaths, and 30-day readmission for subsequent falls are increasing in the elderly US population: a query of the WHO mortality database and National Readmission Database from 2010 to 2014. Clin Epidemiol. 2018;10:1627–1637. doi:10.2147/CLEP.S181138
38. Timler D, Dworzyński MJ, Szarpak Ł, Gaszyńska E, Dudek K, Gałązkowski R. Head trauma in elderly patients: mechanisms of injuries and CT findings. Adv Clin Exper Med. 2015;24(6):1045–1050. doi:10.17219/acem/27565
39. Ryan S, Ward M, Vaughan D, et al. Do safety briefings improve patient safety in the acute hospital setting? A systematic review. J Adv Nurs. 2019;75(10):2085–2098. doi:10.1111/jan.13984
40. Bergen G, Stevens MR, Burns ER. Falls and fall injuries among adults aged ≥65 years - United States, 2014. MMWR Morb Mortal Wkly Rep. 2016;65(37):993–998. doi:10.15585/mmwr.mm6537a2
41. Hallford DJ, Nicholson G, Sanders K, McCabe MP. The association between anxiety and falls: a meta-analysis. J Gerontol B Psychol Sci Soc Sci. 2017;72(5):729–741. doi:10.1093/geronb/gbv160
42. Doiron KA, Hoffmann TC, Beller EM. Early intervention (mobilization or active exercise) for critically ill adults in the intensive care unit. Cochrane Database Syst Rev. 2018;3(3):Cd010754. doi:10.1002/14651858.CD010754.pub2
43. Vanhorebeek I, Latronico N, Van den Berghe G. ICU-acquired weakness. Intensive Care Med. 2020;46(4):637–653. doi:10.1007/s00134-020-05944-4
44. Tipping CJ, Harrold M, Holland A, Romero L, Nisbet T, Hodgson CL. The effects of active mobilisation and rehabilitation in ICU on mortality and function: a systematic review. Intensive Care Med. 2017;43(2):171–183. doi:10.1007/s00134-016-4612-0
45. Daubney ME, Culham EG. Lower-extremity muscle force and balance performance in adults aged 65 years and older. Phys Ther. 1999;79(12):1177–1185. doi:10.1093/ptj/79.12.1177
46. Grimmer M, Riener R, Walsh CJ, Seyfarth A. Mobility related physical and functional losses due to aging and disease - A motivation for lower limb exoskeletons. J Neuroeng Rehabil. 2019;16(1):2. doi:10.1186/s12984-018-0458-8
47. Ensrud KE, Ewing SK, Taylor BC, et al. Frailty and risk of falls, fracture, and mortality in older women: the study of osteoporotic fractures. J Gerontol a Biol Sci Med Sci. 2007;62(7):744–751. doi:10.1093/gerona/62.7.744
48. LeBoff MS, Greenspan SL, Insogna KL, et al. The clinician’s guide to prevention and treatment of osteoporosis. Osteop Int. 2022;33:1–54.
49. Flegal KM, Kit BK, Orpana H, Graubard BI. Association of all-cause mortality with overweight and obesity using standard body mass index categories: a systematic review and meta-analysis. JAMA. 2013;309(1):71–82. doi:10.1001/jama.2012.113905
50. Schetz M, De Jong A, Deane AM, et al. Obesity in the critically ill: a narrative review. Intensive Care Med. 2019;45(6):757–769. doi:10.1007/s00134-019-05594-1
51. Sherrington C, Michaleff ZA, Fairhall N, et al. Exercise to prevent falls in older adults: an updated systematic review and meta-analysis. Br J Sports Med. 2017;51(24):1750–1758. doi:10.1136/bjsports-2016-096547
52. Hopewell S, Adedire O, Copsey BJ, et al. Multifactorial and multiple component interventions for preventing falls in older people living in the community. Cochrane Database Syst Rev. 2018;7(7):Cd012221. doi:10.1002/14651858.CD012221.pub2
53. El-Khoury F, Cassou B, Charles MA, Dargent-Molina P. The effect of fall prevention exercise programmes on fall induced injuries in community dwelling older adults: systematic review and meta-analysis of randomised controlled trials. BMJ. 2013;347:f6234. doi:10.1136/bmj.f6234
54. Ates Bulut E, Soysal P, Isik AT. Frequency and coincidence of geriatric syndromes according to age groups: single-center experience in Turkey between 2013 and 2017. Clin Interv Aging. 2018;13:1899–1905. doi:10.2147/CIA.S180281
55. Ambrose AF, Paul G, Hausdorff JM. Risk factors for falls among older adults: a review of the literature. Maturitas. 2013;75(1):51–61. doi:10.1016/j.maturitas.2013.02.009
56. Joo H, Wang G, Yee SL, Zhang P, Sleet D. Economic burden of informal caregiving associated with history of stroke and falls among older adults in the US. Am J Prev Med. 2017;53(6s2):S197–s204. doi:10.1016/j.amepre.2017.07.020
57. Baek S, Piao J, Jin Y, Lee SM. Validity of the Morse Fall Scale implemented in an electronic medical record system. J Clin Nurs. 2014;23(17–18):2434–2440. doi:10.1111/jocn.12359
58. Gazibara T, Kurtagic I, Kisic-Tepavcevic D, et al. Falls, risk factors and fear of falling among persons older than 65 years of age. Psychogeriatrics. 2017;17(4):215–223. doi:10.1111/psyg.12217
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.