Back to Journals » Open Access Emergency Medicine » Volume 15
Immobilization in Emergency Medical Service – Are CSR and NEXUS-Criteria Considered? A Matched-Pairs Analysis Between Trauma Patients Treated by Onsite EMS Physicians and Patients Treated by Tele-EMS Physicians
Authors Hofstetter P, Schröder H, Beckers SK , Borgs C, Rossaint R, Felzen M
Received 17 September 2022
Accepted for publication 28 March 2023
Published 8 May 2023 Volume 2023:15 Pages 145—155
DOI https://doi.org/10.2147/OAEM.S386650
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Hans-Christoph Pape
Paula Hofstetter,1,2 Hanna Schröder,1,3 Stefan K Beckers,1,3,4 Christina Borgs,1 Rolf Rossaint,1 Marc Felzen1,3,4
1Department of Anesthesiology, University Hospital RWTH Aachen, Aachen, Germany; 2Department of Anesthesiology, Rhein-Maas Klinikum, Würselen, Germany; 3Aachen Institute for Rescue Management & Public Safety, City of Aachen and University Hospital RWTH Aachen, Aachen, Germany; 4Medical Direction of Aachen Fire Department, Aachen, Germany
Correspondence: Marc Felzen, Department of Anesthesiology, University Hospital RWTH Aachen, Pauwelsstrasse 30, Aachen, 52074, Germany, Tel +49 241 8088179, Fax +49 241 82406, Email [email protected]
Background: The NEXUS-low-risk criteria (NEXUS) and Canadian C-spine rule (CSR) are clinical decision tools used for the prehospital spinal clearance in trauma patients, intending to prevent over- as well as under immobilization. Since 2014, a holistic telemedicine system is part of the emergency medical service (EMS) in Aachen (Germany). This study aims to examine whether the decisions to immobilize or not by EMS- and tele-EMS physicians are based on NEXUS and the CSR, as well as the guideline adherence concerning the choice of immobilization device.
Methods: A single-site retrospective chart review was undertaken. Inclusion criteria were EMS physician and tele-EMS physician protocols with traumatic diagnoses. Matched pairs were formed, using age, sex and working diagnoses as matching criteria. The primary outcome parameters were the criteria documented as well as the immobilization device used. The evaluation of the decision to immobilize based on the criteria documented was defined as secondary outcome parameter.
Results: Of a total of 247 patients, 34% (n = 84) were immobilized in the EMS physician group and 32.79% (n = 81) in the tele-EMS physician group. In both groups, less than 7% NEXUS or CSR criteria were documented completely. The decision to immobilize or not was appropriately implemented in 127 (51%) in the EMS-physician and in 135 (54, 66%) in the tele-EMS physician group. Immobilization without indication was performed significantly more often by tele-EMS physicians (6.88% vs 2.02%). A significantly better guideline adherence was found in the tele-EMS physician group, preferring the vacuum mattress (25, 1% vs 8.9%) over the spineboard.
Conclusion: It could be shown that NEXUS and CSR are not applied regularly, and if so, mostly inconsistently with incomplete documentation by both EMS- and tele-EMS physicians. Regarding the choice of the immobilization device a higher guideline adherence was shown among the tele-EMS physicians.
Keywords: immobilization, trauma, emergency medicine, Canadian C-spine rule, NEXUS-criteria, tele-emergency medicine
Introduction
Although the NEXUS-Low-risk criteria (NEXUS) and the Canadian C-spine rule (CSR) have been published almost 20 years ago, and have been adopted into many guidelines worldwide,1,2 the prehospital clearance of the cervical spine and the choice of the immobilization-device are still controversially discussed topics due to the lack of evidence.3–5 The NEXUS-criteria published in 2000 by Hofmann et al and validated for the out-of-hospital spinal clearance in 2000 by Domeier et al include the following five major criteria: the absence of cervical spine tenderness, no focal neurological deficit, normal level of consciousness and the absence of intoxication and distracting painful injury.6,7 In 2001, Stiell et al published the CSR as an alternative clinical decision tool. It defines three high-risk factors (age ≥65 years, dangerous mechanism of injury, paresthesias in the extremities) that require radiological imaging to rule out a spinal fracture. Furthermore, it defines four low-risk factors (sitting position in the ED, ambulatory treatment, delayed onset of neck pain, absence of C-Spine tenderness) that allow a safe assessment of the spine. If the patient can rotate his head 45° left and right, the cervical spine can be cleared without imaging.8 Recent studies show that despite the presence of these criteria, trauma patients are immobilized rather conservatively due to the concern of causing secondary damage to the spine.9,10 It is discussed, if the criteria “distracting injury” leads to unnecessary immobilization, due to the lack of clear evidence about the kind of injury, that should be considered as distracting.11,12
Considering the recent guidelines including the 2016 German trauma guideline,1,2,13 as well as the EMS local standard operating procedures (SOP)14 a spinal immobilization is required if any of the criteria above applies, if none of the criteria applies an immobilization is not required. The NEXUS-criteria and the Canadian C-Spine rule are explicitly cited in both the German guideline and the local SOP. Therefore, assessing the patient for all criteria seems appropriate, especially, if the patient is not immobilized.
It should be taken into account that spinal immobilization is considered, not to be free of risk and can also lead to harm for the patient.4,10
In order to reduce potential harm, when this study was conducted, the national guidelines as the prehospital trauma life support (PHTLS) advocate for the utilization of the vacuum mattress over the spine board for spinal immobilization.1,15
Although many national guidelines1,2,16 as well as PHTLS15 recommend the use of these clinical decision-tools, to date, there are no data illustrating the extent to which these clinical decision-tools are applied by emergency medical service physicians (EMS-physicians). In addition, no surveys could be found on the guideline adherence of EMS physicians concerning the choice of the immobilization device. Furthermore, there is no data for telemedical EMS systems, such as the one, integrated in Aachens EMS system since 2014 as a part of regular prehospital emergency care.17
Therefore, this study examines to what extent the clinically validated7,8 decision-tools recommended by the German national guidelines1 amongst others are being used by EMS physicians and tele-EMS physicians in Aachen, Germany. Moreover, it examines their guideline adherence concerning the immobilization strategy and their choice of the immobilization device, aiming to identify further fields of improvement.
Materials and Methods
This retrospective single-center chart-based cohort study was initiated and conducted at the Department of Anesthesiology, RWTH Aachen University, Aachen, Germany. The study cohort consisted of all patients with traumatic diagnoses treated by the EMS in the city of Aachen between July 2018 and September 2018 and a matched cohort of patients treated by tele-EMS physicians. The study was performed within a quality analysis of the EMS-System and was assessed by the medical faculty’s ethics committee at RWTH Aachen University, Pauwelsstraße 30, 52074 Aachen, Germany (Number of approval: 357/17) as unobjectionable.
Characteristics of Tele-EMS System
The EMS of the city of Aachen consists of paramedic staffed ambulances, as well as EMS-physician staffed vehicles dispatched using a rendezvous-system. Paramedics undergo 3 years of practical and theoretical training. Due to a change in the law, at the time of data collection, there were also emergency paramedics with only 2 years of vocational training. All of them are required to handle the majority of cases independently. Only in the case of potentially life-threatening operations, the EMS physician is additionally dispatched to the scene. EMS-physicians are required to have at least 3 years of clinical practice, of which at least 6 months in anesthesia or intensive care, as well as having taken an 40-hour course in emergency medicine and pre-hospital trauma life support and advanced life support courses. NEXUS and the CSR are part of the practical training of both paramedics and EMS physicians.
Since April 2014, a holistic tele-EMS system is integrated in the EMS of Aachen, complementary to the conventional EMS. It allows transmission of audio communication, pictures or video streams, 12-lead-electrocardiogram and vital signs in real time from inside as well as outside the ambulance to the tele-EMS physician. In contrast to the onsite EMS physician, the tele-EMS physicians are not dispatched by the EMS dispatchers center but either consulted by the paramedics as indicated in the local standard operating procedures or consulted on a voluntary basis whenever considered necessary by the paramedics. The indications for the consultation of the tele-EMS physician include all not primarily life-threatening emergencies, where the expertise of an emergency physician is needed, including the delegation of drug application. It also allows bridging the time to the arrival of the onsite EMS physician. For both conventional- and tele-EMS physician common SOPs are available, defining the necessity of spinal immobilization based on NEXUS and CSR and requiring an evaluation of potential spinal injury based on the mechanism of injury.
A retrospective comparison of EMS physician and tele-EMS physician protocols concerning immobilization in consideration of NEXUS6 and the CSR8 as commonly used clinical decision tools was performed.
All paper-based EMS physician protocols between 01.07.2018 and 31.12.2018 were screened concerning traumatological diagnoses. All protocols with documented traumatic diagnoses or injuries were included, except for interhospital transports. The entire information extracted from these protocols was entered anonymously into a database (Open Clinica, LLC, Waltham, Massachusetts, USA).
Tele-EMS physician protocols entered digitally into a checklist-based software (TM-Doku, Umlaut telehealthcare, Aachen, Germany) were screened and all protocols with a traumatic diagnose were extracted. Matched pairs were formed to address possible differences between the two study groups. To allow the forming of matched pairs, screening protocols from 01.07.2018 to 30.09.2020 was necessary. The matching criteria were the working diagnosis and the patients age and sex. In order to find the maximum amount of matching pairs, an age difference of 24 months was allowed within the pairs, whereas the working diagnose and sex had to be identical. Three patients were excluded since no appropriate match could be found (Figure 1).
 |
Figure 1 Flowchart of inclusion and exclusion of EMS- and tele-EMS protocols. |
Primary and Secondary Outcome Parameter
The primary outcome parameters were the documentation of the NEXUS- and CSR-Criteria, as well as the choice of immobilization device. To obtain this information, the free text boxes of the matched EMS physician and tele-EMS physician protocols were analyzed regarding the documentation NEXUS and CSR. On top of that, the information concerning the choice of immobilization device was retrieved from the protocols.
The secondary outcome parameter was the evaluation of appropriate or inappropriate application of NEXUS and CSR concerning the decision to immobilize or not immobilize the patient. It was reviewed, whether not immobilizing the spine was decided based on documented criteria, or if clearance of the spine was explicitly documented otherwise. Items documented in the protocol by default such as age and Glasgow Coma Scale (GCS), were not considered, as a specific query in favor of spinal clearance was not to be assumed here.
Statistics
The data entry as well as descriptive statistics were performed with Microsoft Excel (©2016 Microsoft, Redmond, Washington, USA, Version 25.17). Numerous analyses were performed using Microsoft Excel pivot tables (©2016 Microsoft, Redmond, Washington, USA, Version 25.17). Conjunctions and negations were used to map indicated or non-indicated spinal immobilization in relation to all variables and to form sums. Patient characteristics are presented in tables, summarizing normal distributed variables by mean ± standard deviation. To find differences between the two groups, a two-sided Fisher's exact test was performed. Analyzing the documentation of individual NEXUS-criteria and CRS-Items, Pearson Chi2-test was used. Significance testing was performed with GraphPad Prism 9 (GraphPad Software, San Diego, California, USA). A p-value below 0.05 was considered statistically significant.
Results
In this study, 250 out of 3082 EMS physician and 956 out of 9169 tele-EMS physician protocols met the inclusion criteria. A total of 247 matched pairs could be formed (Figure 1). The epidemiological data of the patients included is shown in Table 1.
 |
Table 1 The Epidemiological Data of the Patients Before and After Matching |
The assignment of several working diagnoses by the EMS-physician was possible. The distribution of the main diagnoses as matching criterion as well as the secondary diagnoses is shown in Table 2. The tele-EMS physician- as well as the EMS physician protocols allow giving multiple diagnoses. The main diagnoses in both groups are identical, since they were used as a matching criterion, the secondary diagnoses vary in both groups.
 |
Table 2 The Main and Secondary Diagnoses Given by EMS- and Tele-EMS Physicians. Assigning Multiple Working Diagnoses Was Possible |
Documentation of NEXUS- and CSR-Criteria
There was no significant difference in the number of documentation of NEXUS criteria in one of the two groups. The criteria of CSR were documented incompletely more often in the EMS physician group (79.4%) compared to tele-EMS physician group (53.8%) with significant difference (p < 0.001). Reversely, complete documentation occurred more often in the tele-EMS physician group (39.3%) compared to the EMS physician group (20.6%, p < 0.001) (Figure 2). The exact distribution of the individual criteria of NEXUS and CSR are shown in Table 3. In addition to the standard documented criteria (age and GCS), the most frequently documented criteria were “painful distracting injury” and “dangerous mechanism of accident”. The least frequently documented criteria were “paresthesia in the extremities” and “possible active neck rotation of 45°”.
 |
Table 3 The Documentation of Individual NEXUS- and CSR-Criteria by EMS- and Tele-EMS Physicians |
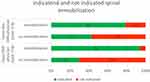
Indicated and Not Indicated Spinal Immobilization
Of the 247 patients in the EMS physician group, 34% (n = 84) of patients were immobilized and 32.79% (n = 81) of patients in the tele-EMS physician group.
The decision to immobilize or not according to NEXUS- or CSR-criteria was correctly implemented in 127 (51.42%) patients in the EMS physician group and in 135 (54.66%) in the tele-EMS physician group (Figure 3). No significant difference could be found between both groups (p=0.528).
The tele-EMS physician group performed immobilization without indication significantly more often with 17 (6.88%) cases than the emergency physician group with 5 (2.02%) cases (p=0.0146).
A total of 115 (46, 56%) patients in the EMS physician group and 95 (38, 46%) patients in the tele-EMS physician group were not immobilized, although neither a spinal clearance according to NEXUS nor according to the CSR was documented. The comparison of the two groups was not significant (p = 0.0837).
Choice of Immobilization Device
With reference to the choice of immobilization device, a significantly more frequent use of the vacuum mattress by the tele EMS-physicians and a significantly more frequent use of the spineboard by the conventional emergency physicians (p < 0.001) was found with an almost identical total number of immobilizations. In the tele-EMS physician group, the vacuum mattress was used in 62 cases, which corresponds to 77.5% of all spinal immobilizations. In contrast, the vacuum mattress was only used in 25.6% of all spinal immobilizations performed by EMS physicians.
The exact distribution of the devices used for immobilization of the spine as well as other splinting or immobilization methods is shown in Table 4.
 |
Table 4 The Immobilization and Splinting Devices Used by EMS and Tele-EMS Physicians in Comparison |
Discussion
This study compares the documentation of the NEXUS- and CSR criteria and the related correct or incorrect indication for immobilizing the spine between the EMS- and tele-EMS physicians.
It could be shown that the common clinical decision tools are not used by the EMS physicians as well as the tele-EMS physicians on a regular basis. If applied, the documentation of criteria is mostly incomplete. Based on the criteria documented, it could be shown that in both groups only around half of the patients were correctly immobilized/not immobilized following NEXUS or CSR guidelines. A significant difference between EMS- and tele-EMS physicians could not be found. Concerning the choice of the immobilization device, a significantly more frequent application of the vacuum mattress could be found in the tele-EMS physician group and hereby a significantly better guideline adherence.
Documentation of NEXUS- and CSR-Criteria
Comparing the number of NEXUS- and CSR-criteria documented as applicable with the study by Ala et al shows that a possible cervical spine rotation of 45° was documented remarkably more often, with 72% of the patients.18 In addition, a dangerous mechanism of accident and spinal midline tenderness were documented more frequently there, whereas all other criteria were documented more frequently in the present study. This suggests that the NEXUS-criteria seem to be much more common among the emergency physicians than the CSR.
The mostly incomplete documentation not only seems critical in all patients where immobilization has been waived, since the guidelines1,2,13 require immobilization when at least one of the criteria is found to be positive, but it is also essential in order to prevent over-immobilisation which can cause severe harm to the patients.4,10
Indicated and Not Indicated Spinal Immobilization
The number of non-indicated immobilisations with 5% in the EMS physician- and 17% in the tele-EMS physician group corresponds well with the results of the study by Muhr et al, who were able to demonstrate 11.7% non-indicated immobilisations with an immobilisation protocol based on NEXUS and CSR.19 However, with 46.56% in the EMS physician group and 38.46% in the tele-EMS physician group, the present study shows a significantly higher rate of patients who were not immobilised despite the spine not being cleared considering the criteria documented compared to the study by Paterek et al (0.3%).20 This does not take into account patients in whom no spinal clearance was documented because the clinical presentation and the accident mechanism did not provide any indication of a spinal injury and thus no indication for immobilisation.
Comparing the indicated and non-indicated immobilisations of EMS- and tele-EMS physicians shows that more patients were immobilised by the tele-EMS physicians without indication, but also fewer patients were not immobilised despite indication than by the EMS physicians. A general superiority of one of the two groups could not be shown. A possible explanation for this is that the tele-EMS physicians are more likely to decide in favour of immobilisation due to the lack of presence at scene, or that the patients were already immobilised by the ambulance service before the tele-EMS physician was consulted.
Choice of Immobilization Device
Concerning the choice of immobilization device (spineboard vs vacuum mattress) a significantly better guideline adherence by the tele-EMS physician could be shown. So far, this has not been clearly demonstrated for other diagnoses for the tele-EMS physician.21,22 Possible explanations are the checklist-based documentation system used by the tele-EMS physician as well as the required higher qualification and more longstanding experience of the tele-EMS physicians compared to the EMS physicians, since the tele-EMS physicians are all board-certified anesthesiologists and are required to have performed a minimum of 400–500 conventional EMS missions. In comparison, the conventional German EMS physicians are only required to.23,24 Another possible cause is the better general overview of the situation and less subjective time pressure on the part of the tele-EMS physicians, as s/he is not physically on scene. The superiority of the tele-EMS physicians does not apply to the use of the decision tools examined. Both EMS physicians and tele-EMS physicians rely on their clinical judgement, presumably due to a lack of explicit training in this regard. Increased training, especially of conventional EMS physicians on this topic is relevant, as it has been shown by Bandiera et al25 that CSR works significantly better for evaluating the need for spinal immobilisation than unstructured physician assessment.
The poor documentation of NEXUS and CSR by both EMS physicians and tele-EMS physicians can be attributed, at least in parts, to the poor documentation quality of the protocols, which has already been shown by Ernst et al for the EMS physician protocols in Aachen.26 In a simulation study, Bergrath et al were able to show that, especially in the simulated polytrauma scenario, documentation quality suffered under the dynamic situation.27 In this study, both groups showed a high number of undocumented criteria; in contrast to Brokmann et al,22 a better documentation of the collected parameters by the tele-EMS physicians could not be shown. This might be because the CSR- and NEXUS-criteria are not included in the tele-EMS physicians checklist-based documentation system.
In summary, the focus of further training for emergency physicians should in future be on the disadvantages of non-indicated immobilisation, ie, it is not a case of: If in doubt, immobilise. In addition, an integration of the criteria of NEXUS and CSR on the paper-based protocols as well as in the tele-EMS physician documentation system should be carried out so that these can be queried in the form of a checklist.
Limitations of the Study
This is a monocentric, retrospective analysis of emergency physician protocols. This study did not investigate whether the EMS physicians and tele-EMS physicians actually applied the NEXUS-criteria and the CSR in order to decide whether to immobilize the spine or not, but it only used the criteria documented in the protocols free text boxes as a surrogate for the application of the criteria.
Neither the paper-based EMS physician protocol nor the checklist-based tele-EMS physician protocol have explicit fields for ticking the criteria of NEXUS and CSR, and the spinal clearance, so that in both cases this information must be explicitly indicated by the emergency physicians in the free text. Due to the poor documentation quality of the protocols, especially the history and physical examination,26 it must be assumed that more examinations were performed to decide on the need for spinal immobilisation than are documented on the protocols.
The use of matched-pairs analysis may result in a biased selection of tele-EMS physician protocols with a greater focus on more severely injured patients, so that, although both groups are comparable to each other, this study might only reflect the totality of traumatological tele-EMS physicians missions to a limited extent. On top of that, the two matched groups might not be completely comparable due to the fact that the EMS physicians were dispatched to scene, while the tele-EMS physicians were required by the EMS personnel.
Although NEXUS and CSR are part of the German trauma guideline as well as Aachens local EMS SOPs, the EMS physicians awareness of these clinical decision tools remains unclear. This could lead to more unnecessary spinal immobilizations and should therefore be addressed in further studies.
Due to the monocentric study design, the generalizability of the results found remains unclear. It could be assumed that due to the standardized German EMS-protocols, the documentation deficits probably caused by the lacking boxes for documenting NEXUS and CSR are likely to also appear in other areas. Whether the other findings are generalizable remains to be proven.
Conclusions
It could be shown that NEXUS and CSR as clinical decision tools for spinal immobilisation are not regularly applied, and if so, mostly only incompletely documented by both the EMS- and tele-EMS physicians of the city of Aachen, as there are no specific guidelines in this regard. With regard to the choice of the immobilisation device, however, a clearly higher guideline adherence of the tele-EMS physician compared to the conventional EMS-physician was shown.
Data Sharing Statement
The datasets analyzed during the current study are not publicly available due to the fact that the datasets are municipal property and can therefore not be published online under open access agreements. However, the datasets are available on reasonable request and with the permission of the municipal authorities.
Ethics Approval and Consent to Participate
The study was assessed by the medical faculty’s ethics committee at RWTH Aachen University, Pauwelsstraße 30, 52074 Aachen, Germany (Number of approval: 357/17) as unobjectionable. The ethics committee, the university research board (Center for Translational and Clinical Research), and data protection officers granted the analysis of the data for quality assurance purposes and waived the requirement of informed consent from patients.
Acknowledgments
We thank Michèle Twomey for the language editing and Markus Kirch for his technical support during the data analysis.
Author Contributions
All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data. PH wrote the entire manuscript, all other authors took part in revising it critically for important intellectual content; agreed to submit to the current journal; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
Funding
The present study did not receive any external funding.
Disclosure
The authors declare that they have no competing interests.
References
1. Unfallchirurgie DGf. S3-Leitlinie Polytrauma/ Schwerverletzten-Versorgung [German National Polytrauma Guideline]. Prof. Dr. med. Bertil Bouillon; 2016.
2. Kornhall DK, Jorgensen JJ, Brommeland T, et al. The Norwegian guidelines for the prehospital management of adult trauma patients with potential spinal injury. Scand J Trauma Resusc Emerg Med. 2017;25(1):2. doi:10.1186/s13049-016-0345-x
3. Kwan I, Bunn F, Roberts IG. Spinal immobilisation for trauma patients. Cochrane Database Syst Rev. 2001;(2). doi:10.1002/14651858.CD002803
4. Abram S, Bulstrode C. Routine spinal immobilization in trauma patients: what are the advantages and disadvantages? Surgeon. 2010;8(4):218–222. doi:10.1016/j.surge.2010.01.002
5. Baez AA, Schiebel N. Evidence-based emergency medicine/systematic review abstract. Is routine spinal immobilization an effective intervention for trauma patients? Ann Emerg Med. 2006;47(1):110–112. doi:10.1016/j.annemergmed.2005.09.008
6. Hoffman JR, Mower WR, Wolfson AB, Todd KH, Zucker MI. Validity of a set of clinical criteria to rule out injury to the cervical spine in patients with blunt trauma. National Emergency X-Radiography Utilization Study Group. N Engl J Med. 2000;343(2):94–99. doi:10.1056/NEJM200007133430203
7. Domeier RM, Swor RA, Evans RW, et al. Multicenter prospective validation of prehospital clinical spinal clearance criteria. J Trauma. 2002;53(4):744–750. doi:10.1097/00005373-200210000-00021
8. Stiell IG, Wells GA, Vandemheen KL, et al. The Canadian C-spine rule for radiography in alert and stable trauma patients. JAMA. 2001;286(15):1841–1848. doi:10.1001/jama.286.15.1841
9. Connor D, Greaves I, Porter K, Bloch M. Pre-hospital spinal immobilisation: an initial consensus statement. Emerg Med J. 2013;30(12):1067–1069. doi:10.1136/emermed-2013-203207
10. Larson S, Delnat AU, Moore J. The use of clinical cervical spine clearance in trauma patients: a literature review. J Emerg Nurs. 2018;44(4):368–374. doi:10.1016/j.jen.2017.10.013
11. Dahlquist RT, Fischer PE, Desai H, et al. Femur fractures should not be considered distracting injuries for cervical spine assessment. Am J Emerg Med. 2015;33(12):1750–1754. doi:10.1016/j.ajem.2015.08.009
12. Rose MK, Rosal LM, Gonzalez RP, et al. Clinical clearance of the cervical spine in patients with distracting injuries: it is time to dispel the myth. J Trauma Acute Care Surg. 2012;73(2):498–502. doi:10.1097/TA.0b013e3182587634
13. National Clinical Guideline Council. National institute for health and care excellence: guidelines. In: Spinal Injury: Assessment and Initial Management. London: National Institute for Health and Care Excellence (NICE); 2016. Copyright © National Clinical Guideline Centre, 2016.
14. Graw. Gemeinsames Kompendium Rettungsdienst 2020 [Regional EMS standard operating procedures]. 2020. German.
15. Deutschland P PHTLS Europe Research Group. Stellungnahme zum Themenkomplex “Immobilisation von Traumapatienten” [Statement on the topic of “Immobilisation of Trauma Patients” by the National Board of PHTLS Germany]. 2015. German.
16. Council NMD. National Model EMS Clinical Guidelines. Council NMD; 2019.
17. Felzen M, Brokmann JC, Beckers SK, et al. Improved technical performance of a multifunctional prehospital telemedicine system between the research phase and the routine use phase - an observational study. J Telemed Telecare. 2017;23(3):402–409. doi:10.1177/1357633X16644115
18. Ala A, Shams Vahdati S, Ghaffarzad A, Mousavi H, Mirza-Aghazadeh-Attari M. National emergency X-radiography utilization study guidelines versus Canadian C-spine guidelines on trauma patients, a prospective analytical study. PLoS One. 2018;13(11):e0206283. doi:10.1371/journal.pone.0206283
19. Muhr MD, Seabrook DL, Wittwer LK. Paramedic use of a spinal injury clearance algorithm reduces spinal immobilization in the out-of-hospital setting. Prehosp Emerg Care. 1999;3(1):1–6. doi:10.1080/10903129908958895
20. Paterek E, Isenberg DL, Schiffer H. Characteristics of trauma patients with potential cervical spine injuries underimmobilized by prehospital providers. Spine. 2015;40(24):1898–1902. doi:10.1097/BRS.0000000000001149
21. Bergrath S, Müller M, Rossaint R, Beckers SK, Uschner D, Brokmann JC. Guideline adherence in acute coronary syndromes between telemedically supported paramedics and conventional on-scene physician care: a longitudinal pre-post intervention cohort study. Health Informatics J. 2019;25(4):1528–1537. doi:10.1177/1460458218775157
22. Brokmann JC, Rossaint R, Müller M, et al. Blood pressure management and guideline adherence in hypertensive emergencies and urgencies: a comparison between telemedically supported and conventional out-of-hospital care. J Clin Hypertens. 2017;19(7):704–712. doi:10.1111/jch.13026
23. Brokmann JC, Felzen M, Beckers SK, et al. Telemedizin: potenziale in der Notfallmedizin. Anasthesiol Intensivmed Notfallmed Schmerzther. 2017;52(2):107–117. doi:10.1055/s-0042-108713
24. Felzen M, Hirsch F, Brokmann JC, Rossaint R, Beckers SK. Anforderungs- und Qualifikationsprofil an den Notarzt in der Telenotfallmedizin. Notfall + Rettungsmedizin. 2018;21(7):590–597. doi:10.1007/s10049-018-0443-6
25. Bandiera G, Stiell IG, Wells GA, et al. The Canadian C-spine rule performs better than unstructured physician judgment. Ann Emerg Med. 2003;42(3):395–402. doi:10.1016/S0196-0644(03)00422-0
26. Ernst ME. Dokumentationsqualität im Notarztdienst der Stadt Aachen - Eine retrospektive Analyse der Notfallprotokolle und Einsatzdaten eines Jahres nach Einführung der DIVI MIND 3 Notarzteinsatzprotokolle [Documentation quality in the emergency physician service of the city of Aachen - A retrospective analysis of emergency protocols and deployment data one year after the introduction of the DIVI MIND 3 emergency physician deployment protocols]. Aachen: Rheinisch-Westfälische Technische Hochschlue Aachen; 2020.
27. Bergrath S, Rörtgen D, Skorning M, et al. Notärztliche Einsatzdokumentation in der Simulation [Emergency mission documentation in simulated care. Video-based error analysis]. Anaesthesist. 2011;60(3):221–229. German. doi:10.1007/s00101-010-1790-y
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.