Back to Journals » OncoTargets and Therapy » Volume 7
IL-1α -889 C/T polymorphism and cancer susceptibility: a meta-analysis
Authors Cheng D, Hao Y, Zhou W
Received 19 July 2014
Accepted for publication 25 September 2014
Published 10 November 2014 Volume 2014:7 Pages 2067—2074
DOI https://doi.org/10.2147/OTT.S71420
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 5
Editor who approved publication: Dr Jianmin Xu
Daye Cheng, Yiwen Hao, Wenling Zhou
Department of Transfusion, First Hospital of China Medical University, Shenyang, People's Republic of China
Abstract: The -889 C/T polymorphism in the interleukin-1α (IL-1α) gene has been implicated in the risk of cancer, but the results are inconclusive. The present meta-analysis aimed to investigate the association between the -889 C/T polymorphism and cancer risk. A literature search in PubMed, Embase™, Web of Science™, Science Direct®, SpringerLink, EBSCO, Wanfang, and Chinese National Knowledge Infrastructure (CNKI) databases was carried out to identify studies investigating the association between IL-1α -889 C/T polymorphism and cancer risk. The odds ratio (OR) with 95% confidence interval (CI) were used to assess the strength of association. A total of 20 publications, involving 6,782 cases and 7,767 controls, were included in this meta-analysis. Combined analysis revealed a significant association between -889 C/T polymorphism and cancer risk under an allele model (OR =1.12, 95% CI =1.02–1.24, P=0.02), recessive model (OR =1.34, 95% CI =1.06–1.68, P=0.01), and homozygous comparison (OR =1.38, 95% CI =1.10–1.74, P<0.01). Subgroup analysis by ethnicity showed there was significant association between cancer risk and IL-1a -889C/T polymorphism in Asian populations under a recessive model (OR =2.57, 95% CI =1.11–5.98, P=0.03) and homozygous comparison (OR =2.60, 95% CI =1.12–6.04, P=0.03). Moreover, a subgroup analysis was conducted by source of control, and a statistically increased cancer risk was found in the hospital-based group, under a recessive model (OR =1.62, 95% CI =1.03–2.56, P=0.04) and homozygous comparison (OR =1.67, 95% CI =1.04–2.68, P=0.03). This meta-analysis suggests that IL-1α -889 C/T polymorphism contributes to cancer susceptibility. Further large and well-designed studies are needed to confirm this association.
Keywords: neoplasma, biomarker, cytokine, systematic review
Introduction
In recent years, the role for inflammation in tumorigenesis has become more evident. Chronic inflammation, not only facilitates the progression of normal cells to malignancy but also, supports survival of many malignancies through production of proinflammatory cytokines.1,2 Through activation of various downstream effectors, cytokines control the immune and inflammatory milieu to either favor antitumor immunity or enhance tumor progression, and also, have direct effects on cancer cell growth and survival.3,4
Interleukin-1 (IL-1) is a pleiotrophic cytokine that primarily affects inflammatory responses, immune reactivity, and hematopoiesis.5,6 Accumulating evidence has shown that IL-1 is involved in all phases of the malignant process, such as tumorigenesis, tumor invasiveness and progression, as well as activation/suppression of antitumor immunity. The IL-1 cytokine family consists of three members, IL-1α, IL-1β, and IL-1 receptor (IL-1R) antagonist.7 In particular, IL-1α has been suggested to regulate cancer cell invasion and metastasis, inducing invasiveness-promoting factors (ie, matrix metalloproteinases) and adhesion molecules.8,9 In animal models, mice solely deficient in IL-1α exhibit dramatically impaired tumor development and blood vessel growth.10 IL-1α expression has also been found in pancreatic adenocarcinoma,11 colon cancer,12 gastric carcinoma,13 thyroid carcinoma,14 ovarian carcinoma,15 lung carcinoma,16 and adult T-cell leukemia.17 Wolf et al reported that IL-1α contributes to the transcriptional activation of nuclear factor kappaB (NF-κB) and activator protein 1 (AP-1), and promotes cell survival and growth in the head and neck squamous cell carcinoma cell line.18 Xu et al revealed that autocrine IL-1α and paracrine hepatocyte growth factor (HGF) coenhance the metastatic potential of pancreatic cancer cells via both IL-1α and HGF signaling pathways.19 Therefore, IL-1α may be involved in tumor progression.
The gene encoding IL-1α is located in chromosome 2q13-21, and there is a single nucleotide polymorphism (SNP) at position -889.20 IL-1α -889 C/T polymorphism has been reported to be associated with an increased cytokine production.21,22 To date, many studies have been published to assess the association between IL-1α -889 C/T polymorphism and cancer susceptibility, but they reported controversial results. A single case-control study may fail to completely demonstrate the complicated genetic relationship because of the small sample size.23 In order to provide strong evidence of the effects of IL-1α -889 C/T polymorphism on cancer susceptibility, we performed a meta-analysis by combining data from numerous published studies.
Methods
Search strategy
A literature search in PubMed, Embase™, Web of Science™, Science Direct®, SpringerLink, EBSCO, Wanfang, and Chinese National Knowledge Infrastructure (CNKI) databases was carried out to identify studies investigating the association between cancer risk and IL-1α -889 C/T polymorphism, without language, time period, or sample size limitations, and covering all papers published up to May 2014. The sets of search terms were as follows: “IL-1, or IL-1α, or IL-1alpha, or interleukin-1A, or IL-1A” and “cancer, or carcinoma, or tumor, or neoplasma” and “polymorphism, or variant, or SNP”.
Inclusion and exclusion criteria
The selection criteria of the retrieved articles in our meta-analysis were as follows: a) case–control studies or cohort studies; b) studies evaluating the association between IL-1α -889 C/T polymorphism and cancer risk; c) identification of cancer patients was confirmed histologically or pathologically; and d) sufficient data available to calculate an odds ratio (OR) with 95% confidence interval (CI). The exclusion criteria of the meta-analysis were: a) case-only studies; b) studies with incomplete data; and c) meta-analyses, letters, reviews, and editorial articles. If more than one study was published by the same author using the same patient population or overlapping case series, the study with the largest size of samples was included.
Data extraction
The following data from included studies were extracted independently by two authors (Cheng and Hao). The following data were collected: name of first author; year of publication; country; ethnicity; cancer types; sources of control; number of cases and controls, and genotype frequency in cases and controls; genotyping methods; P value for Hardy–Weinberg equilibrium; and minor allele frequency. Any disagreement was resolved through discussions by these two authors until consensus was reached.
Sensitivity analysis
Sensitivity analysis was performed by excluding each investigation individually and recalculating the pooled estimates and their corresponding 95% CIs to determine the effect of each study on the summary estimate.
Statistical analysis
The strength of the association between IL-1α -889 C/T polymorphism and cancer risk was estimated by calculating ORs with 95% CIs, based on the genotype frequencies in cases and controls. The pooled ORs were calculated for five models: allele model (T allele vs C allele), dominant model (TT+TC vs CC), recessive model (TT vs TC+CC), homozygous comparison (TT vs CC), and heterozygous comparison (TC vs CC). The chi square-based Q statistic test was employed to test between-study heterogeneity, and heterogeneity was considered significant when P<0.1 for the Q statistic. The fixed effect model was chosen when studies were homogeneous (with P>0.10 for the Q test); otherwise, a random effects model was adopted. The significance of the pooled OR was determined by Z test, and P-value less than 0.05 was considered as statistically significant. Subgroup analyses were carried out to explore the source of heterogeneity among variables, including ethnicity and source of control, respectively. Publication bias was both examined with Begg’s funnel plot24 and Egger’s regression method25 (P<0.05 was considered representative of statistically significant publication bias). All statistics were conducted by using Stata Statistical Software: Release 11.0 (StataCorp, College Station, TX, USA).
Results
Characteristic of eligible studies
The detailed screening process is shown in Figure 1. A total of 311 publications from all databases were reviewed. After a review of titles, abstracts, and articles, 20 studies, with 6,782 cases and 7,767 controls, were included in this meta-analysis.20–22,26–42 Table 1 lists the studies identified and their main characteristics. There were six studies conducted in Asian populations, ten studies in Caucasian populations, and four studies in mixed populations. Population-based controls were performed in eleven studies, and hospital-based controls in nine studies. The genotype distribution of IL-1α -899 C/T polymorphism in the controls was in compliance with Hardy–Weinberg equilibrium, except for in three studies.22,26,33
  | Figure 1 Flow diagram of the study selection process. |
Meta-analysis results
The main results of the meta-analysis of the association between IL-1α -889 C/T polymorphism and cancer risk are shown in Table 2. In the overall analysis, there was significant association between IL-1α -889 C/T polymorphism and cancer risk under an allele model (OR =1.12, 95% CI =1.02–1.24, P=0.02), recessive model (OR =1.34, 95% CI =1.06–1.68, P=0.01), and homozygous comparison (OR =1.38, 95% CI =1.10–1.74, P<0.01), but no significant association was found under other models.
Subgroup analysis by ethnicity and source of controls was performed in order to determine the source of heterogeneity among the studies and to assess the effect of ethnicity and source of controls on the association between IL-1α -889 C/T polymorphism and cancer risk. Then, stratified analysis by ethnicity showed that a statistically increased cancer risk was found in the Asian population under a recessive model (OR =2.57, 95% CI =1.11–5.98, P=0.03) and homozygous comparison (OR =2.60, 95% CI =1.12–6.04, P=0.03), but there was no significant association between cancer risk and IL-1α -889 C/T in either the Caucasian or mixed population (Table 2, Figure 2). Moreover, a subgroup analysis was conducted by source of control, and a statistically increased cancer risk was found in the hospital-based group, under a recessive model (OR =1.62, 95% CI =1.03–2.56, P=0.04) and homozygous comparison (OR =1.67, 95% CI =1.04–2.68, P=0.03) (Table 2, Figure 3).
  | Figure 2 Meta-analysis for IL-1α -889 C/T polymorphism and cancer susceptibility, based on ethnicity under a recessive model (TT vs TC+CC). |
Sensitivity analysis
Sensitivity analysis was performed to evaluate the stability of the meta-analysis. Statistically similar data were obtained after sequentially excluding each study, indicating that our results were statistically reliable.
Publication bias
Begg’s funnel plot and Egger’s test were performed to assess the publication bias of studies. The shape of Begg’s funnel plot was symmetrical (Figure 4). The statistical results still did not show publication bias by Egger’s test (P=0.923).
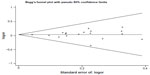  | Figure 4 Funnel plots for publication bias of IL-1α -889 C/T polymorphism and cancer risk in the overall populations under a dominant model. |
Discussion
Cytokines might contribute to tumor development by enhancing angiogenesis and tumor cell adhesions or by interfering with the antitumoral mechanisms of the immune system.43 In recent years, studies have demonstrated that carcinogenesis is associated with altered levels of inflammatory cytokines, which have a substantial impact on numerous biological activities. Common variation in cytokine genes could lead to variation in protein structure, thus affecting the quantity and activity of cytokines.20,44 Knowledge of the genetic variations that influence cancer development is important for assessing cancer risk and identifying preventive strategies.
IL-1α, an important proinflammatory cytokine, plays an important role in tumorigenesis and development.45 IL-1α has been reported to be produced by cancer cell lines derived from carcinomas of the pancreas, lung, ovary, colon, and stomach.19 Of note, some data suggest that IL-1α is less important in carcinogenesis and tumor invasion than IL-1β. Membrane-associated IL-1α seems to increase antitumor immunity and subsequently might contribute to tumor cell eradication.46 Cancer is considered to be a complex and multistep disease that results from interactions between environmental and genetic factors,47 and SNPs are associated with intersubject variation and diversity, and have been recently considered as important genetic factors involved in the development of cancer. Several polymorphisms have been described in IL-1α genes, which probably modulate IL-1α protein production and have been related with the development and severity of cancer.26,48 The most common polymorphism, -889 C/T polymorphism, has been associated with high production of IL-1α.22,49 To date, many studies have investigated the role of the IL-1α -889 C/T polymorphism in different types of cancer. However, the results of these studies remain inconclusive. We, therefore, performed a meta-analysis by pooling 20 eligible studies, including 6,782 cases and 7,767 controls, to clarify this inconsistency and to achieve a more precise estimation of the relationship between IL-1α -889 C/T polymorphism and cancer risk. Our results demonstrated that IL-1α -889 C/T polymorphism was significantly associated with increased overall cancer risk under an allele model (P=0.02), recessive model (P=0.01), and homozygous comparison (P<0.01).
In order to explore a potential source of heterogeneity, we also performed subgroup analysis based on ethnicity. We found the significant association of IL-1α -889 C/T polymorphism with cancer risk only in the Asian population, under a recessive model (P=0.03) and homozygous comparison (P=0.03). Our results also revealed that no statistically significant risk was observed in Caucasian and mixed populations, under all genetic models. Moreover, in the subgroup analysis by source of control, we found a statistically increased cancer risk in the hospital-based group, under a recessive model (P=0.04) and homozygous comparison (P=0.03), but not in the population-based group. Hospital-based controls were randomly selected cancer-free patients from the same hospital as the cancer patients during the same period, and they might be from a related disease population and not the general population. Selection bias could not be avoided.
The findings in this meta-analysis should be interpreted with caution because of several limitations. First, in the subgroup analysis by ethnicity, the included studies were mainly in Asians and Caucasians, and future study should evaluate the association between IL-1α -889 C/T polymorphism and cancer risk in different ethnicities, especially in Africans. Second, the meta-analysis was limited by a relatively small number of available studies. It is difficult to perform subgroup analysis for every type of cancer. Third, only published studies in the selected databases were included in this meta-analysis. It is possible that some studies that were not included in these databases or some unpublished studies with null results were not identified, and this may have biased our results. Fourth, gene–gene and gene–environment interactions may play important roles in the function of IL-1α -889C/T polymorphism, but the effect was not addressed in our meta-analysis, due to unavailable data.
Conclusion
To the best of our knowledge, this is the first meta-analysis to assess the relationship between IL-1α -889 C/T polymorphism and cancer risk. Our results demonstrated that IL-1α -889 C/T polymorphism was associated with increased risk of cancer. Further stratification by ethnicity or source of control indicated that the association between IL-1α -889 C/T polymorphism and cancer was restricted to the Asian population and the hospital-based group. More studies with large sample size are needed to further assess the associations described above.
Disclosure
The authors report no conflicts of interest in this work.
References
Qin Y, Ekmekcioglu S, Liu P, et al. Constitutive aberrant endogenous interleukin-1 facilitates inflammation and growth in human melanoma. Mol Cancer Res. 2011;9(11):1537–1550. | |
Schottenfeld D, Beebe-Dimmer J. Chronic inflammation: a common and important factor in the pathogenesis of neoplasia. CA Cancer J Clin. 2006;56(2):69–83. | |
Grivennikov SI, Greten FR, Karin M. Immunity, inflammation, and cancer. Cell. 2010;140(6):883–899. | |
Cataisson C, Salcedo R, Hakim S, et al. IL-1R-MyD88 signaling in keratinocyte transformation and carcinogenesis. J Exp Med. 2012;209(9):1689–1702. | |
Dinarello CA. Blocking IL-1 in systemic inflammation. J Exp Med. 2005;201(9):1355–1359. | |
Apte RN, Voronov E. Interleukin-1 – a major pleiotropic cytokine in tumor-host interactions. Semin Cancer Biol. 2002;12(4):277–290. | |
Shao J, Sheng H. Prostaglandin E2 induces the expression of IL-1alpha in colon cancer cells. J Immunol. 2007;178(7):4097–4103. | |
Andersen K, Maelandsmo GM, Hovig E, Fodstad O, Loennechen T, Winberg JO. Interleukin-1 alpha and basic fibroblast growth factor induction of matrix metalloproteinases and their inhibitors in osteosarcoma cells is modulated by the metastasis associated protein CAPL. Anticancer Res. 1998;18(5A):3299–3303. | |
Nguyen M, Corless CL, Kräling BM, et al. Vascular expression of E-selectin is increased in estrogen-receptor-negative breast cancer: a role for tumor-cell-secreted interleukin-1 alpha. Am J Pathol. 1997;150(4):1307–1314. | |
Voronov E, Shouval DS, Krelin Y, et al. IL-1 is required for tumor invasiveness and angiogenesis. Proc Natl Acad Sci U S A. 2003;100(5):2645–2650. | |
Tjomsland V, Bojmar L, Sandström P, et al. IL-1α expression in pancreatic ductal adenocarcinoma affects the tumor cell migration and is regulated by the p38MAPK signaling pathway. PLoS One. 2013;8(8):e70874. | |
Matsuo Y, Sawai H, Ma J, et al. IL-1alpha secreted by colon cancer cells enhances angiogenesis: the relationship between IL-1alpha release and tumor cells’ potential for liver metastasis. J Surg Oncol. 2009;99(6):361–367. | |
Tomimatsu S, Ichikura T, Mochizuki H. Significant correlation between expression of interleukin-1alpha and liver metastasis in gastric carcinoma. Cancer. 2001;91(7):1272–1276. | |
Zeki K, Nakano Y, Inokuchi N, et al. Autocrine stimulation of interleukin-1 in the growth of human thyroid carcinoma cell line NIM 1. J Clin Endocrinol Metab. 1993;76(1):127–133. | |
Li BY, Mohanraj D, Olson MC, et al. Human ovarian epithelial cancer cells cultures in vitro express both interleukin 1 alpha and beta genes. Cancer Res. 1992;52(8):2248–2252. | |
Nakane T, Szentendrei T, Stern L, Virmani M, Seely J, Kunos G. Effects of IL-1 and cortisol on beta-adrenergic receptors, cell proliferation, and differentiation in cultured human A549 lung tumor cells. J Immunol. 1990;145(1):260–266. | |
Shirakawa F, Tanaka Y, Oda S, Eto S, Yamashita U. Autocrine stimulation of interleukin 1 alpha in the growth of adult human T-cell leukemia cells. Cancer Res. 1989;49(5):1143–1147. | |
Wolf JS, Chen Z, Dong G, et al. IL (interleukin)-1alpha promotes nuclear factor-kappaB and AP-1-induced IL-8 expression, cell survival, and proliferation in head and neck squamous cell carcinomas. Clin Cancer Res. 2001;7(6):1812–1820. | |
Xu D, Matsuo Y, Ma J, et al. Cancer cell-derived IL-1α promotes HGF secretion by stromal cells and enhances metastatic potential in pancreatic cancer cells. J Surg Oncol. 2010;102(5):469–477. | |
Ioana Braicu E, Mustea A, Toliat MR, et al. Polymorphism of IL-1alpha, IL-1beta and IL-10 in patients with advanced ovarian cancer: results of a prospective study with 147 patients. Gynecol Oncol. 2007;104(3):680–685. | |
Sengüven B, Oygür T. Investigation of interleukin-1 alpha and interleukin-6 expression and interleukin-1 alpha gene polymorphism in keratocystic odontogenic tumors and ameloblastomas. Med Oral Patol Oral Cir Bucal. 2011;16(4):e467–e472. | |
Grimm C, Berger I, Tomovski C, et al. A polymorphism of the interleukin-1 receptor antagonist plays a prominent role within the interleukin-1 gene cluster in vulvar carcinogenesis. Gynecol Oncol. 2004;92(3):936–940. | |
Tein JY, Coxe S, Cham H. Statistical power to detect the correct number of classes in latent profile analysis. Struct Equ Modeling. 2013;20(4):640–657. | |
Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. 1994;50(4):1088–1101. | |
Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–634. | |
Abazis-Stamboulieh D, Oikonomou P, Papadoulis N, Panayiotidis P, Vrakidou E, Tsezou A. Association of interleukin-1A, interleukin-1B and interleukin-1 receptor antagonist gene polymorphisms with multiple myeloma. Leuk Lymphoma. 2007;48(11):2196–2203. | |
Bushley AW, Ferrell R, McDuffie K, et al. Polymorphisms of interleukin (IL)-1alpha, IL-1beta, IL-6, IL-10, and IL-18 and the risk of ovarian cancer. Gynecol Oncol. 2004;95(3):672–679. | |
Foster CB, Lehrnbecher T, Samuels S, et al. An IL6 promoter polymorphism is associated with a lifetime risk of development of Kaposi sarcoma in men infected with human immunodeficiency virus. Blood. 2000;96(7):2562–2567. | |
Ennas MG, Moore PS, Zucca M, et al. Interleukin-1B (IL1B) and interleukin-6 (IL6) gene polymorphisms are associated with risk of chronic lymphocytic leukaemia. Hematol Oncol. 2008;26(2):98–103. | |
Eshghyar N, Nikbin B, Amirzargar A, Dehghani Nazhvani A, Shakiba Y. Gene polymorphism of interleukin-1 alpha and beta in keratocystic odontogenic tumors. J Oral Pathol Med. 2012;41(9):697–701. | |
Grimm C, Watrowski R, Baumühlner K, et al. Genetic variations of interleukin-1 and -6 genes and risk of cervical intraepithelial neoplasia. Gynecol Oncol. 2011;121(3):537–541. | |
Wang HM. Relationship between interleukin-1 gene cluster gene polymorphism and susceptibility to cervical cancer [D]. Liaoning: Dalian Medical University. 2005. | |
Hefler LA, Grimm C, Lantzsch T, et al. Interleukin-1 and interleukin-6 gene polymorphisms and the risk of breast cancer in Caucasian women. Clin Cancer Res. 2005;11(16):5718–5721. | |
Hoeft B, Becker N, Deeg E, Beckmann L, Nieters A. Joint effect between regular use of non-steroidal anti-inflammatory drugs, variants in inflammatory genes and risk of lymphoma. Cancer Causes Control. 2008;19(2):163–173. | |
Hou L, El-Omar EM, Chen J, et al. Polymorphisms in Th1-type cell-mediated response genes and risk of gastric cancer. Carcinogenesis. 2007;28(1):118–123. | |
Rothman N, Skibola CF, Wang SS, et al. Genetic variation in TNF and IL10 and risk of non-Hodgkin lymphoma: a report from the InterLymph Consortium. Lancet Oncol. 2006;7(1):27–38. | |
Sáenz-López P, Carretero R, Cózar JM, et al. Genetic polymorphisms of RANTES, IL1-A, MCP-1 and TNF-A genes in patients with prostate cancer. BMC Cancer. 2008;8:382. | |
Snoussi K, Strosberg AD, Bouaouina N, Ben Ahmed S, Chouchane L. Genetic variation in pro-inflammatory cytokines (interleukin-1beta, interleukin-1alpha and interleukin-6) associated with the aggressive forms, survival, and relapse prediction of breast carcinoma. Eur Cytokine Netw. 2005;16(4):253–260. | |
Yang ZH, Dai Q, Zhong L, Zhang X, Guo QX, Li SN. Association of IL-1 polymorphisms and IL-1 serum levels with susceptibility to nasopharyngeal carcinoma. Mol Carcinog. 2011;50(3):208–214. | |
Zheng L, Yin J, Wang L, et al. Interleukin 1B rs16944 G>A polymorphism was associated with a decreased risk of esophageal cancer in a Chinese population. Clin Biochem. 2013;46(15):1469–1473. | |
Bai L, Yu H, Wang H, Su H, Zhao J, Zhao Y. Genetic single-nucleotide polymorphisms of inflammation-related factors associated with risk of lung cancer. Med Oncol. 2013;30(1):414. | |
Qu YL, Yu H, Chen YZ, et al. Relationships between genetic polymorphisms in inflammation-related factor gene and the pathogenesis of nasopharyngeal cancer. Tumour Biol. Epub June 22, 2014. | |
Nash MA, Ferrandina G, Gordinier M, Loercher A, Freedman RS. The role of cytokines in both the normal and malignant ovary. Endocr Relat Cancer. 1999;6(1):93–107. | |
Hirschhorn JN, Lohmueller K, Byrne E, Hirschhorn K. A comprehensive review of genetic association studies. Genet Med. 2002;4(2):45–61. | |
Voronov E, Dotan S, Krelin Y, et al. Unique versus redundant functions of IL-1α and IL-1β in the tumor microenvironment. Front Immunol. 2013;4:177. | |
Apte RN, Dotan S, Elkabets M, et al. The involvement of IL-1 in tumorigenesis, tumor invasiveness, metastasis and tumor-host interactions. Cancer Metastasis Rev. 2006;25(3):387–408. | |
Xu J, Yin Z, Cao S, et al. Systematic review and meta-analysis on the association between IL-1B polymorphisms and cancer risk. PLoS One. 2013;8(5):e63654. | |
Endres S, Cannon JG, Ghorbani R, et al. In vitro production of IL 1 beta, IL 1 alpha, TNF and IL2 in healthy subjects: distribution, effect of cyclooxygenase inhibition and evidence of independent gene regulation. Eur J Immunol. 1989;19(12):2327–2333. | |
Dominici R, Cattaneo M, Malferrari G, et al. Cloning and functional analysis of the allelic polymorphism in the transcription regulatory region of interleukin-1 alpha. Immunogenetics. 2002;54(2):82–86. |
 © 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.



