Back to Journals » Journal of Blood Medicine » Volume 11
Idiopathic Hypereosinophilia and Venous Thromboembolism: Is There a Pathophysiological or Clinical Link? Description of an Intriguing Clinical Case
Authors Di Micco P, scudiero O, Scudiero O , Lombardo B , Lodigiani C
Received 29 August 2019
Accepted for publication 29 October 2019
Published 28 February 2020 Volume 2020:11 Pages 73—76
DOI https://doi.org/10.2147/JBM.S229074
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Martin H Bluth
Pierpaolo Di Micco,1 Olga Scudiero,2,3 Barbara Lombardo,2,3 Corrado Lodigiani4
1Department of Internal Medicine and Emergency Room, Fatebenefratelli Hospital of Naples, Naples, Italy; 2Dipartimento di Medicina Molecolare e Biotecnologie Mediche, Università degli Studi di Napoli “Federico II”, Napoli, Italia; 3CEINGE-Biotecnologie Avanzate, Napoli, Italia; 4Thrombosis and Hemorrhagic Center, Humanitas Research Hospital and Humanitas University, Rozzano, Italy
Correspondence: Corrado Lodigiani
Thrombosis and Hemorrhagic Center, Humanitas Research Hospital and Humanitas University, Rozzano, Italy
Email [email protected]
Abstract: Thrombosis events usually occur after prolonged bedrest, pregnancy, hormonal therapy, recent surgery and in the presence of inherited or acquired thrombophilia. However, several other diseases are often associated with thrombosis although their frequency is not easily estimated. Eosinophilia is one of these conditions. From a clinical viewpoint it is very difficult to understand which conditions might lead to a thrombotic event because the underlying pathophysiological mechanisms are different. Here, we report a case of idiopathic hypereosinophilia associated to venous thromboembolism without any other associated prothrombotic condition.
Keywords: venous thromboembolism, deep vein thrombosis, hypereosinophilia, allergy
Background
Several clinical conditions associated with chronic hypereosinophilia are already known. The most common are Churg–Strauss syndrome (CSS), hypereosinophilic syndrome (HES), and chronic eosinophilic leukemia (CEL), all associated with an excess of eosinophilic cells in bone, in peripheral tissues, vessels, bone marrow or other connective tissues.1–3 Clinical manifestations of chronic eosinophilia are usually associated with local degranulation of eosinophilic cells inducing local and\or systemic inflammation; in these cases the number of eosinophilic cells is always more than 12% on a total WBC count of 10,000 mm3.4 Beside local or systemic inflammation or allergy, other complications such as thrombosis of small or large vessels may appear in these patients.5 Thrombotic complications may occur in several regions and venous thromboembolism (VTE) is one of the most common clinical thrombotic complications associated with hypereosinophilia.5,6
Little is known from a pathophysiological point of view concerning the generation of a prothrombotic condition induced by hypereosinophilia but other environmental prothrombotic risk factors may occur in each patient with hypereosinophilia as far as a possible association with inherited thrombophilia or hormonal treatment or pregnancy or recent hypomobility or recent surgery.7
We report a clinical case in which an adult without personal and familial history of VTE but with chronic hypereosinophilia developed a sudden VTE without association with further environmental thrombotic risk factors, suggesting a possible direct link between hypereosinophilic conditions and venous thromboembolism.
Case History
BA a 60 year old man was referred to the ER because of a sudden pain to his left leg that began nearly 24–30 h before and did not improve after full doses of NSAIDs (ie ibuprofen 1200 mg daily). At physical examination of the left leg revealed a moderate swelling and clinical signs of Homann and Payr were present so inferring a suspicion of deep vein thrombosis (DVT). His anamnesis revealed chronic hypertension and hypercholesterolemia treated with lisinopril 20 mg daily and atorvastatin 10 mg daily; no previous thrombotic event (ie atherothrombosis or VTE) or recent hypomobilization or recent surgery were detected. While past anamnesis revealed history of skin allergy without significant complications or recurrences by more than 15 years; in order to confirm this last condition the use of last anti-allergic medication was referred more than 15 years before. Increase of sweating was not referred to by the patient as weight loss in last three months.
Ultrasound vascular scan of leg was performed and revealed a proximal DVT. Hemodynamic signs were good with blood pressure 130/70 mmHg, ECG in sinus rhythm and pulse oximetry 97% in normal breath (without any type of oxygen administration); therefore, because systemic symptoms as dyspnea or syncope or chest pain were not mentioned by the patient, pulmonary angio-CT scan of lung was not required.
A treatment based on low molecular weight heparin, enoxaparin, (100 U/kg twice daily) was started and followed after one week by a direct oral anticoagulant administration, edoxaban 60 mg daily for long-term treatment.
The event appeared as a nonprovoked VTE (ie not associated with common risk factor as recent hypomobility or recent surgery) so a full screening of potential underlying causes of VTE was ruled out. Inherited thrombophilia was looked for and tested negative such as acquired thrombophilia with antiphospholipid antibodies testing (Table 1); occult malignancy was excluded after a screening based on chest X-ray, colonoscopy, abdominal ultrasound scan, cerebral CT scan. Abdominal and thoracic CT scan was planned one week after and did not reveal any type of pathology nor lymphadenomegaly or splenomegaly.
 |
Table 1 Thrombophilia Screening of the Studied Patient |
General blood samples did not reveal any type of alteration of kidney or liver functions but a hypereosinophilia was detected with levels of 1800 mm3 (20% of total white blood cell count).
The presence of hypereosinophilia was also investigated and because the recent screening for occult malignancy performed for the occurrence of nonprovoked VTE, a secondary hypereosinophilia to solid malignancy was excluded too.
Yet, because the old anamnesis of skin allergy, eosinophils levels were checked again confirming at different times their increased levels; in this way further tests to specify the cause of this asymptomatic blood abnormality were planned and blood samples to detect plasma levels of IgE were planned and tested negative (Table 2); usually increased levels of IgE, in fact, are present when a reaction toward common antigens is present Similarly, autoimmunity markers were looked for in order to evaluate a possible underlying Churg–.Strauss syndrome or Wegener‘s disease without any evidence (Table 2). Fecal research of parasites associated with hypereosinophilia as Ascaris lumbricoides or pinworms had negative results. Lymphocyte clusters were tested in order to exclude an infective or autoimmune latent disorder but levels of CD4 and CD8 were not increased (Table 2).
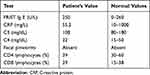 |
Table 2 Main Clinical Conditions Associated with to Eosinophilia Tested in the Described Patient |
An echocardiogram was planned in order to detect restrictive endomyocardial fibrosis or other intracardiac damages as pericarditis or valves’ damage due to the increase of eosinophil cells but without any evidence.
Finally bone marrow aspiration to reveal potential abnormalities as myeloid malignancy or clonal alteration present in clonal idiopathic eosinophilia were also tested without evidence; for this reason, a further test as platelet-derived growth factor receptor (PDGFR) or fibroblast growth factor 1 (FGR1) rearrangements were not considered.
So the only alteration associated with idiopathic DVT was the hypereosinophilia and the only complication of chronic eosinophilia was the sudden DVT. Because hypereosinophilia is not considered a cause of provoked venous thromboembolism the patient was assigned to a long-term treatment of one year of anticoagulant drug as far as unprovoked venous thromboembolism with a direct oral anticoagulant, edoxaban 60 mg daily and associated to a low dose of steroids per os as prednisone 0.3 mg\kg with improvements on eosinophilic count (ie reduction of 10–15%).
Discussion
Incidence and prevalence of hypereosinophilic syndromes are still not well known. In the majority of cases males seem to be more affected, in particular, in middle age, but case series have been reported in all decades of life.4
Clinical signs and symptoms may be different and may appear as contemporaneous features or at different times. Usually, skin symptoms such as urticaria or eczema or digestive symptoms such as nausea, vomiting, and diarrhea or respiratory symptoms such as asthma are the most common symptoms described by patients, but thromboses are not rare, comprising 20% or more of affected patients.5,6 These symptoms may also be present in clonal eosinophilia and may be associated with peripheral nervous dysfunctions or thromboembolic complications.8
Venous thromboembolism is the one of the most commonly described thromboses in hypereosinophilia and it may influence long-term treatment and prognosis of hypereosinophilic patients.5,6
Several pathophysiological mechanisms have been described in the last decades to explain the hypercoagulable state induced by hypereosinophilia that may lead to thrombosis. Of course the most commonly known has been related to chronic inflammation as in the Churg–Strauss vasculitis that may cause a real thromboangiitis.1
However, other clinical forms of hypereosinophilia may be associated with thrombosis by other noninflammatory pathways.
The proteolytic actions induced by eosinophil granules may activate the kallikrein system and so the clotting cascade by factor XII activation; the factor XII activation, increasing the activation of other proteases of clotting system, induces hypercoagulable state.9 Protease systems, in particular, matrix metalloproteinases are also involved in cleavage of extracellular matrix proteins that also participate in myocardial remodelling during cardiac diseases as heart failure and\or pulmonary hypertension.10,11 Moreover, this pathway is also overexpressed by the cytokine network and the balance protease-antiprotease is able to hyperactivate clotting system per se.11
Furthermore, the eosinophil activation and degranulation increases the release of eosinophil cationic protein that is able to bind heparin and modulate thrombomodulin so reducing the physiological anticoagulation mechanisms and so increasing the prothrombotic state in hypereosinophilia.12,13
The reported case is intriguing because the involvement of the skin system and the evidence of strong chronic hypereosinophilia and the systemic involvement with clinical symptoms such as deep vein thrombosis. However, although associated with comorbidity as hypereosinophilia this kind of DVT could be considered nonprovoked DVT because it is not associated with typical risk factors such as recent surgery, cancer, hypomobility, ongoing pregnancy, or hormonal treatment.7 Moreover, classic inherited or acquired thrombophlic abnormalities were not detected either. These evaluations are needed to establish the duration of the antithrombotic treatment and may also influence the prognosis of this nonprovoked DVT associated with clinical conditions in which a thrombotic event may be detected.14
Consent Statement
The authors certify that the described patient gave us a specific written informed consent and the agreement to publish his clinical experience and his case details.
Disclosure
Prof. Dr. Corrado Lodigiani reports personal fees from Bayer Health Care, Boehringer Ingheleim, NovoNordisk, and Daiichi Sankyo, outside the submitted work. The authors report no other conflicts of interest in this work.
References
1. Katerenchuk IP, Tkachenko LA, Yarmola TI, et al. Churg–Strauss syndrome: clinical case and its feautures. Wiad Lek. 2019;72(4):723–726.
2. Bychkov VG, Zolotukhin VM, Khadieva ED, et al. Hypereosinophilic syndrome, cardiomyopathies, and sudden cardiac death in superinvasive opisthorchiasis. Cardiol Res Pract. 2019;4836948.
3. Iriyama N, Takahashi H, Naruse H, et al. A novel fusion gene involving PDGFRB and GCC2 in a chronic eosinophilic leukemia patient harboring t(2;5)(q37;q31). Mol Genet Genomic Med. 2019;7(4):e0059. doi:10.1002/mgg3.591
4. Leru PM. Eosinophilic disorders: evaluation of current classification and diagnostic criteria, proposal of a practical diagnostic algorithm. Clin Transl Allergy. 2019;9:36. doi:10.1186/s13601-019-0277-4
5. Wallace KL, Elias MK, Butterfield CL, Weiler L. Hypereosinophilic syndrome and thrombosis: a retrospective review. J Allergy Clin Immunol. 2013;131(Supplement):441. doi:10.1016/j.jaci.2012.12.1105
6. Li D, Xu L, Lin D, Jiang S, Feng S, Zhu L. Acute pulmonary embolism and deep vein thrombosis secondary to idiopathic hypereosinophilic syndrome. Respir Med Case Rep. 2018;25:213–215. doi:10.1016/j.rmcr.2018.09.006
7. Gharaibeh L, Albsoul-Younes A, Younes N. Evaluation of VTE prophylaxis in an educational hospital: comparison between the institutional guideline (Caprini 2006) and the ACCP guideline (Ninth edition). Clin Appl Thromb Hemost. 2016;22(7):627–632. doi:10.1177/1076029615575344
8. Tefferi A, Gotlib J, Pardanani A. Hypereosinophilic syndrome and clonal eosinophilia: point-of-care diagnostic algorithm and treatment update. Mayo Clin Proc. 2010;85(2):158–164. doi:10.4065/mcp.2009.0503
9. Naito T, Hayashi H, Kashiwada T, et al. Pulmonary embolism and deep vein thrombosis in eosinophilic granulomatosis with polyangiitis successfully treated with rivaroxaban. Respir Med Case Rep. 2018;25:33–35. doi:10.1016/j.rmcr.2018.05.008
10. Neto Neves EM, Sousa Santos SO, Ferraz KC, et al. Matrix metalloproteinase inhibition attenuates right ventricular dysfunction and improves responses to dobutamine during acute pulmonary thromboembolism. J Cell Mol Med. 2013;17:1588–1597.
11. Querques F, Cantilena B, Cozzolino C,et al. Angiotensin I receptor stimulates osteoprogenitor proliferation throug TGFß-mediated signaling. J Cell Physiol. 2015;230:1466–1474.
12. Mukai HY, Ninomiya H, Ohtani K, Nagasawa T, Abe T. Major basic protein binding to thrombomodulin potentially contributes to the thrombosis in patients with eosinophilia. Br J Haematol. 1995;90(4):892–899. doi:10.1111/j.1365-2141.1995.tb05211.x
13. Torrent M, Nogués MV, Boix E. Eosinophil cationic protein (ECP) can bind heparin and other glycosaminoglycans through its RNase active site. J Mol Recognit. 2011;24(1):90–100. doi:10.1002/jmr.1027
14. Di Micco P, Lodigiani C. Idiopathic Venous Thromboembolism (VTE) and its association to rare molecular clotting abnormalities. Health Sci J. 2018;12:e15. doi:10.21767/1791-809X
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
