Back to Journals » Advances in Medical Education and Practice » Volume 13
Identifying Barriers to the Adoption of Information Communication Technology in Ethiopian Healthcare Systems. A Systematic Review
Authors Tegegne MD , Wubante SM
Received 11 May 2022
Accepted for publication 29 July 2022
Published 5 August 2022 Volume 2022:13 Pages 821—828
DOI https://doi.org/10.2147/AMEP.S374207
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Md Anwarul Azim Majumder
Masresha Derese Tegegne, Sisay Maru Wubante
Department of Health Informatics, Institute of Public Health, College of Medicine and Health Sciences, University of Gondar, Gondar, Ethiopia
Correspondence: Masresha Derese Tegegne, Department of Health Informatics, Institute of Public Health, College of Medicine and Health Sciences, University of Gondar, Gondar, Ethiopia, PO Box 196, Tel +251935474755, Email [email protected]
Background: Ethiopia’s government has planned to digitize the healthcare industry. However, most implementations fail due to various technological and personnel barriers. As a result, this systematic review aimed to comprehensively examine evidence regarding the barriers to adopting information communication technology in the Ethiopian healthcare system.
Methods: This systematic review was conducted by searching the major databases, such as Medline, PubMed, Scopus, Science Direct, Google, Google Scholar, and other online databases. The authors looked for, analyzed, and summarized information about barriers to ICT adoption in the healthcare system. This study included nine articles that described barriers to ICT adoption in the Ethiopian healthcare system.
Results: This systematic review identified 15 barriers to adopting ICT in the healthcare system. The reviewed articles looked into technological barriers to ICT adoption, such as ICT skill, ICT knowledge, a lack of training opportunities, a lack of computer literacy, a lack of computer access, inadequate internet connectivity, and a lack of experience with ICT were cited as barriers to ICT implementation in Ethiopia’s healthcare system. Furthermore, organizational components such as Lack of job satisfaction, Lack of Refreshment training, poor staff initiation, management problem, poor infrastructure, and lack of resources remained barriers to ICT adoption in Ethiopia’s healthcare system.
Conclusion: This review confirmed that lack of training in ICT, poor ICT knowledge, Poor ICT skill, and a lack of computer access were the most common barriers to adopting ICT in the Ethiopian healthcare system. Therefore, it is recommended that the emphasized barriers to ICT adoption be addressed in order to modernize the current Ethiopian healthcare system.
Keywords: barriers, ICT, HIT, healthcare system, Ethiopia
Background
Information and communication technology has the potential to transform every area of the healthcare system.1,2 ICT adoption in the health industry solves critical health data management difficulties and improves the quality of health services.3
There is a considerable burden of sickness and a scarcity of skilled health staff in developing countries.4 These parts of the continents continue to face health problems characterized by the spread of tropical infectious diseases and high infant mortality and maternal mortality.5 As a result, information communication technology is expected to improve health care delivery by fostering a culture of communication and data management.6,7 Additionally, ICT allows health professionals and patients to support primary care and encourage preventive healthcare.8
Evidence suggests that the implementation of e-Health applications such as electronic medical records, telemedicine systems, mobile health apps, and district health information systems has increased in Ethiopia.4,9,10 However, most implementations fail due to technological and personnel barriers.11 Ethiopia’s government has planned to digitize the healthcare industry.12 There are several e-Health projects currently, most of which are suffering sustainability issues.11,13,14 This could be due to several obstacles that prevent target users from adopting health information technology. The individual study showed that lack of ICT infrastructure, expense, technical barriers, a shortage of competent human resources, and a lack of readiness among medical practitioners are obstacles.4,15–20 One frequently proposed technique for closing this gap is to intervene in the barriers before or during the implementation of an e-health system.10 However, to the authors’ knowledge, there has not been comprehensively examined evidence regarding the barriers to adopting health information technology in Ethiopia. As a result, this systematic review aimed to comprehensively examine evidence regarding the barriers to adopting ICT in the Ethiopian healthcare system. The findings of this systematic review will assist health managers and other stakeholders in implementing various e-health initiatives and projects.
Methods
Search Strategy
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses were used to systematically review the available literature (PRISMA) (Table S1).21 The PRISMA flow diagram is also used to visually represent the studies that have been identified, included, and excluded.
Publications were searched using Online databases: Medline, PubMed, Scopus, Science Direct, Google, Google Scholar, and other online databases until April 5, 2022. Snowballing of the literature was used to find the most relevant study based on the objectives.
Endnote X9 software will be used to retrieve and manage studies found through our database searching strategy. The search phrases included Medical Subject Headings (Mesh), keywords, and free text search queries. We include alternative terms for Barriers and combine them using Boolean operators Search terms as the search terms. Search ((“Barriers” OR “Challenge” OR “Obstacles” OR “Determinants” OR “Factors‘) AND (“ICT” OR “Health information technology” OR “Computer” OR “Digital technology”) AND (“health professional” OR “Medical students”) AND (Ethiopia)).
Eligibility Criteria
This systematic review includes all cross-sectional, analytical cross-sectional research concentrating primarily on ICT adoption in the Ethiopian healthcare system. Full-text publications written in English that were published in peer-reviewed journals or located in the grey literature and were easily accessible are included in this review. However, studies on other electronic systems utilized in healthcare (such as EMR systems or Electronic Health Records (EHRs)), studies published in languages other than English, and studies other than cross-sectional studies, such as case reports, conference reports, national survey reports, and expert opinions, are excluded from this systematic review.
Data Extraction
After identifying eligible articles, two independent reviewers (MDT&SMW) extracted the relevant data using an organized format on Microsoft Excel Spreadsheet. Discrepancies between data extractors have reached a consensus by discussion. We recorded the first author’s last name, year of publication, the study’s setting, study design, study period, and sample si for each included article.
Quality Appraisal
Quality assessment criteria were developed for research that reported the barriers to ICT adoption in the healthcare system. Two separate authors appraised the quality of the study chosen for this review (MDT&SMW). The Joanna Briggs Institute was used to assess the quality of the included studies.22 The final systematic review included five-star or higher articles (Table S2).
Data Analysis
The combined meta-analysis results were not performed in this systematic review. There was significant heterogeneity across the included studies due to differences in the nature of the outcome and study participants. As a result, integrating them would have been methodologically ineffective, and a systematic review of studies on the barriers to adopting ICT was preferable. The barriers were ranked depending on how often they were featured in the studies. In our research, this strategy produced consistent results.
Results
Identified Studies
A total of 1482 records were found through database searching. Seven hundred forty results were exported after duplication. After title and abstract screening, 642 papers were eliminated. Following that, 98 studies were selected for a full-text review. The full-text assessment resulted in the exclusion of 90 articles. Finally, the review included nine studies (Figure 1).
Characteristics of Included Studies
The final systematic review included nine studies conducted in Ethiopia. Except for one study that employed a mixed methodology,20 the reaming eight studies employed a cross-sectional quantitative study. There are also differences across several dimensions; eight studies were conducted in hospital and primary health care settings, and the remaining two were conducted in medicine and health sciences universities. Table 1 illustrates six studies conducted on health professionals, two articles on health sciences students, and one study conducted on the medical record unit personnel.15
 |
Table 1 Characteristics of Included Studies |
Identified Barriers to the Adoption of ICT in the Healthcare Systems
The nine studies included in this review indicated 15 barriers to ICT adoption in the Ethiopian healthcare system (Figure 2). The reviewed articles looked into technological barriers to ICT adoption, such as ICT skill,16,23 ICT knowledge,16,18,23 a lack of training opportunities,4,15–18,20,23,24 a lack of computer literacy,19 a lack of computer access,15,17,19,24 inadequate internet connectivity,19 and a lack of experience with ICT24 were cited as barriers to ICT implementation in Ethiopia’s healthcare system. Furthermore, organizational components such as lack of job satisfaction,17 Lack of Refreshment training,19 poor staff initiation,19 management problems,19 poor infrastructure,19 and lack of resources19 remained barriers to ICT adoption in Ethiopia’s healthcare system.
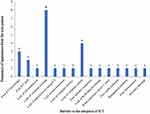 |
Figure 2 Identified barriers to the adoption of ICT in the Ethiopian healthcare system. |
Figure 2 displays the fifteen barriers from the nine papers that were chosen, along with their frequency of occurrence. As a result, lack of training in ICT, poor ICT knowledge, Poor ICT skill, and a lack of computer access were all common barriers in at least two studies. Almost all articles mention the lack of computer training as one of the most common barriers to adopting ICT in the healthcare system. Lack of computer access was also seen in nearly half of the research covered in this systematic review. Poor ICT knowledge and skill were again the most common underlying barrier, appearing in three and two research, respectively, out of nine included studies (Figure 2).
Discussion
Health information technologies encompass various strategies to deliver high-quality patient care. An academic study into the factors influencing the adoption of HIT in Ethiopia has been scattered, leaving researchers with limited comprehensive knowledge of the challenges to HIT implementation. No prior review has specifically examined or synthesized the evidence on the significant barriers that affect HIT adoption in the Ethiopian health care system. This systematic review contributes to this field by critically evaluating and synthesizing existing research on HIT adoption barriers, which may help identify significant HIT implementation barriers.
To accomplish the objectives of this systematic review, we compiled empirical data on 15 barriers to adopting HIT in the Ethiopian healthcare system. Residing in rural areas, older age groups, lack of training in ICT, poor ICT knowledge, Poor ICT skill, a lack of computer access, and a low education level were prevalent Obstacles in at least two research studies.
A lack of computer training was one of the most frequently reported barriers to ICT adoption in the healthcare sector. According to a study conducted in Canada, lack of computer training is a recognized barrier to ICT adoption in a healthcare context.25 In a study conducted in Australia, barriers, and facilitators to using e-Health technology confirms that training and education are barriers to HIT adoption.26 Furthermore, similar studies on the obstacles to EMR adoption in Ethiopia supported the conclusion that computer training is one of the contributing variables to the clinical information system adoption.27 This suggested that the government should prioritize computer education when adopting HIT in Ethiopia. Therefore, it is essential to include computer training as a key component of successful HIT adoption.
Computer inaccessibility was highlighted in over half of the papers analyzed as a significant barrier to ICT adoption in the Ethiopian healthcare system. This finding is consistent with earlier studies,28–30 which found that a lack of computer access is the main barrier preventing healthcare workers from adopting health information technology. A study conducted in developing nations also supports our findings that lack of computer hardware and software is one of the challenges in adopting health information technology.31 Similarly, according to a study conducted in Ghana, a lack of ICT infrastructure hinders the implementation of information and communication technology in the health setting.32 This shows that for the Ethiopian healthcare system to successfully implement health information technologies, the ministry of health should increase the accessibility of digital technology in the healthcare setting.
The present study also found that poor knowledge and skill in ICT were also the identified barriers to the successful adoption of health information technology. A study in Pakistan found that implementing health information technology in underdeveloped nations is hindered by a lack of ICT expertise and skills.31 Similar research has identified ICT skill and knowledge as the most crucial factor to consider in implementing the health information technology.33,34 As skill is the main factor in ICT adoption in healthcare,35 interventions are required to improve health professionals’ knowledge and use of ICT. This demonstrates the necessity for specialized training to enhance the ICT skills and knowledge of healthcare staff to enable efficient use of ICT within the healthcare system.4 Therefore, it is suggested that it is desirable to improve health practitioners’ ICT knowledge and skills before introducing health information technology.
Conclusion and Recommendation
This study identified 15 barriers to adopting ICT in the Ethiopian healthcare system. The review confirmed that lack of training in ICT, poor ICT knowledge, Poor ICT skill, and a lack of computer access were the most common barriers to adopting ICT in the Ethiopian healthcare system. These findings will assist health managers and other stakeholders in implementing various ICT programs and projects in the Ethiopian healthcare system. This evidence can advance our understanding of the potential barriers and suggested solutions for ICT adoption in the Ethiopian healthcare system. As a result, It is recommended that the specific barriers to ICT adoption in the Ethiopian health system be addressed in order to innovate health care delivery. Using this data, researchers can investigate reported barriers in diverse contexts and nations. Future studies should focus on identifying barriers that prevent the implementation of e-health services like Telemedicine, M-health, and comparable ones in the Ethiopian healthcare system.
Strength and Limitations
This systematic review contributes to this field by critically evaluating and synthesizing existing research on HIT adoption barriers, which may help identify significant HIT implementation barriers. This study has certain drawbacks. The significant limitation is that only a few studies were discovered despite the authors’ exhaustive search. This could be related to the lack of investigation into Ethiopia’s health information technology adoption.
Abbreviations
MRU, medical record unit; ICT, information communication technology; HIT, health information technology; e-Health, electronic health; PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analyses; EMR, electronic medical record.
Data Sharing Statement
The data analyzed during the current meta-analysis and supplementary information are available in the manuscript.
Acknowledgments
We want to express our gratitude to all of the studies’ authors included in this systematic review.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis, and interpretation, or in all these areas; took part in drafting, revising, or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted, and agree to be accountable for all aspects of the work.
Funding
There is no funding to report.
Disclosure
The authors declare that they have no competing interests.
References
1. Lucas H. Information and communications technology for future health systems in developing countries. Soc Sci Med. 2008;66(10):2122–2132. doi:10.1016/j.socscimed.2008.01.033
2. Jacobson LE, Labrique AB. Information communication technology and health. Foundation Glob Health Sci Pract. 2018;217:1–4.
3. Reid PP, Compton WD, Grossman JH, Fanjiang G. Information and communications systems: the backbone of the health care delivery system. In: Building a Better Delivery System: A New Engineering/Health Care Partnership. National Academies Press (US); 2005.
4. Alwan K, Ayele TA, Tilahun B. Knowledge and utilization of computers among health professionals in a developing country: a cross-sectional study. JMIR Human Factors. 2015;2(1):e4184. doi:10.2196/humanfactors.4184
5. Boutayeb A. The double burden of communicable and non-communicable diseases in developing countries. Trans R Soc Trop Med Hyg. 2006;100(3):191–199. doi:10.1016/j.trstmh.2005.07.021
6. Sukums F, Mensah N, Mpembeni R, Kaltschmidt J, Haefeli WE, Blank A. Health workers’ knowledge of and attitudes towards computer applications in rural African health facilities. Glob Health Action. 2014;7(1):24534. doi:10.3402/gha.v7.24534
7. Dzenowagis J, Kernen G. Connecting for health: global vision, local insight: report for the World Summit on the Information Society; 2005:36.
8. Dery S, Vroom F-C, Godi A, Afagbedzi S, Dwomoh D. Knowledge and use of information and communication technology by health sciences students of the University of Ghana. Ghana Med J. 2016;50(3):180–188. doi:10.4314/gmj.v50i3.10
9. Dagnaw GA, Tsigie S. Current stat of the art digital literacy in Ethiopia: article review. Studies. 2019;5(9):2454–8499.
10. Shiferaw KB, Tilahun BC, Endehabtu BF. Healthcare providers’ digital competency: a cross-sectional survey in a low-income country setting. BMC Health Serv Res. 2020;20(1):1–7. doi:10.1186/s12913-020-05848-5
11. Fraser HS, Blaya J. Implementing medical information systems in developing countries, what works and what doesn’t.
12. Tilahun B, Gashu KD, Mekonnen ZA, et al. Strengthening the national health information system through a capacity-building and mentorship partnership (CBMP) programme: a health system and university partnership initiative in Ethiopia. Health Res Policy Syst. 2021;19(1):1–11. doi:10.1186/s12961-021-00787-x
13. Luna D, Otero C, Marcelo A. Health informatics in developing countries: systematic review of reviews contribution of the IMIA working group health informatics for development. Yearb Med Inform. 2013;22(01):28–33. doi:10.1055/s-0038-1638829
14. Azubuike MC, Ehiri J. Health information systems in developing countries: benefits, problems, and prospects. J R Soc Promot Health. 1999;119(3):180–184. doi:10.1177/146642409911900309
15. Meseret M, Tesfu M, Alemayehu M, Abebe Y. Knowledge and attitude towards ICT among medical record unit workers, Northwest Ethiopia, 2018: institutional based cross-sectional study. Int J Wirel Commun Mob Comput. 2020;8(1):1. doi:10.11648/j.wcmc.20200801.11
16. Woreta SA, Kebede Y, Zegeye DT. Knowledge and utilization of information communication technology (ICT) among health science students at the University of Gondar, North Western Ethiopia. BMC Med Inform Decis Mak. 2013;13(1):1–7. doi:10.1186/1472-6947-13-31
17. Mohammed E, Andargie G, Meseret S, Girma E. Knowledge and utilization of computer among health workers in Addis Ababa hospitals, Ethiopia: computer literacy in the health sector. BMC Res Notes. 2013;6(1):1–8. doi:10.1186/1756-0500-6-106
18. Tsigie SE, Dagnaw GA. Knowledge and utilization of information communication technologies (ICTs) among Health Professionals at Debretabor Referral Hospital, Northwest Ethiopia. Int J. 2021;10:2.
19. Asemahagn M. Challenges of ICTs utilization among health professionals: the case of public hospitals in Addis Ababa, Ethiopia. SM J Public Health Epidemiol. 2015;1(3):1012.
20. Adane M, Lessa L, Shiferaw S. Knowledge, attitude and utilization of information communication technologies (ICTs) in an Ethiopian Medical Teaching Hospital. NesglobalOrg. 2010;10:105–110.
21. PRISMA. PRISMA Checklist 2021. Available from: http://prisma-statement.org/PRISMAStatement/Checklist.
22. Institute JB. Critical appraisal tools. Available from: https://jbi.global/critical-appraisal-tools.
23. Hailegebreal S, Sedi TT, Belete S, et al. Utilization of information and communication technology (ICT) among undergraduate health science students: a cross-sectional study. BMC Med Educ. 2022;22(1):1–7. doi:10.1186/s12909-022-03296-9
24. Seboka BT, Yilma TM, Birhanu AY. Factors influencing healthcare providers’ attitude and willingness to use information technology in diabetes management. BMC Med Inform Decis Mak. 2021;21(1):1–10. doi:10.1186/s12911-021-01398-w
25. Kavandi H, Jaana M. Factors that affect health information technology adoption by seniors: a systematic review. Health Soc Care Community. 2020;28(6):1827–1842. doi:10.1111/hsc.13011
26. Wilson J, Heinsch M, Betts D, Booth D, Kay-Lambkin F. Barriers and facilitators to the use of e-health by older adults: a scoping review. BMC Public Health. 2021;21(1):1–12. doi:10.1186/s12889-021-11623-w
27. Yehualashet DE, Seboka BT, Tesfa GA, Demeke AD, Amede ES. Barriers to the adoption of electronic medical record system in Ethiopia: a systematic review. J Multidiscip Healthc. 2021;14:2597. doi:10.2147/JMDH.S327539
28. Lee HW, Ramayah T, Zakaria N. External factors in hospital information system (HIS) adoption model: a case on Malaysia. J Med Syst. 2012;36(4):2129–2140. doi:10.1007/s10916-011-9675-4
29. Qureshi S. Creating a Better World with Information and Communication Technologies: Health Equity. Taylor & Francis; 2016:1–14.
30. Zayyad MA, Toycan M. Factors affecting sustainable adoption of e-health technology in developing countries: an exploratory survey of Nigerian hospitals from the perspective of healthcare professionals. PeerJ. 2018;6:e4436. doi:10.7717/peerj.4436
31. Anwar F, Shamim A, Khan S. Barriers in adoption of health information technology in developing societies. Int J Adv Comput Sci Appl. 2011;2(8):40–45.
32. Addo K, Agyepong PK. The effects of information and communication technology on health service delivery at Tafo Government Hospital. E Health Telecommun Syst Network. 2020;9(3):33–48. doi:10.4236/etsn.2020.93003
33. Salahuddin L, Ismail Z. Classification of antecedents towards safety use of health information technology: a systematic review. Int J Med Inform. 2015;84(11):877–891. doi:10.1016/j.ijmedinf.2015.07.004
34. De Leeuw JA, Woltjer H, Kool RB. Identification of factors influencing the adoption of health information technology by nurses who are digitally lagging: in-depth interview study. J Med Internet Res. 2020;22(8):e15630. doi:10.2196/15630
35. Dias C, Escoval A. Narrowing the skills gap for innovation: an empirical study in the hospital sector. JMIR Human Factor. 2014;1(1):e3598. doi:10.2196/humanfactors.3598
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

