Back to Journals » Clinical Interventions in Aging » Volume 14
Identification of potentially inappropriate medications with risk of major adverse cardiac and cerebrovascular events among elderly patients in ambulatory setting and long-term care facilities
Authors Aguiar JP , Heitor Costa L, Alves da Costa F , Leufkens HGM, Martins AP
Received 25 October 2018
Accepted for publication 11 January 2019
Published 4 March 2019 Volume 2019:14 Pages 535—547
DOI https://doi.org/10.2147/CIA.S192252
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Richard Walker
João Pedro Aguiar,1 Luís Heitor Costa,2 Filipa Alves da Costa,3,4 Hubert GM Leufkens,5 Ana Paula Martins1
1Research Institute for Medicines (iMED.ULisboa), Faculdade de Farmácia, Universidade de Lisboa, Lisboa, Portugal; 2Serviço de Medicina Interna, Centro Hospitalar Psiquiátrico de Lisboa (CHPL), Lisboa, Portugal; 3Centro de Investigação Interdisciplinar Egas Moniz (CiiEM), Instituto Universitário Egas Moniz (IUEM), Caparica, Portugal; 4Faculdade de Farmácia, Universidade de Lisboa, Lisboa, Portugal; 5Division of Pharmacoepidemiology and Clinical Pharmacology, Utrecht Institute for Pharmaceutical Sciences, Utrecht University, Utrecht, the Netherlands
Purpose: Cardiovascular diseases (CVDs) are extremely common among the elderly, but information on the use of potentially inappropriate medications (PIMs) with cardiovascular risk is scarce. We aimed to determine the prevalence of PIMs with risk of cardiac and cerebrovascular adverse events (CCVAEs), including major adverse cardiac and cerebrovascular events (MACCE).
Patients and methods: A cross-sectional study was performed using a convenience sample from four long-term care facilities and one community pharmacy in Portugal. Patients were included if they were aged 65 or older and presented at least one type of medication in their medical and pharmacotherapeutic records from 2015 until December 2017. The main outcome was defined as the presence of PIMs with risk of MACCE and was assessed by applying a PIM-MACCE list that was developed from a previous study. All medications included in this list were assessed for their availability in Portugal.
Results: A total of 680 patients were included. Of those, 428 (63%) were female with a mean age of 78.4±8.1 years. Four-hundred and four (59.4%) patients were taking medications associated with CCVAEs risk (mean =1.7±1.0 drugs/patient), including 264 patients (38.8%) who used drugs with MACCE risk (mean =1.4±0.8 drugs/patient). Fifty percent of patients with a previous history of CVD (n=521) were taking PIMs with risk of CCVAEs, including 30.0% with risk of MACCE.
Conclusion: Our findings show that 50% of patients with previous history of CVD were taking drugs with risk of CCAVEs and 30% with risk of MACCE. More tailored tools for the management of drug therapy in elderly patients with CVD are of major importance in clinical practice.
Keywords: patient safety, therapeutic uses, outcome process assessment (health care), cardiovascular risk, NSAIDs, antipsychotics
Introduction
The elderly are usually fragile and more susceptible to drug-related problems as a result of multimorbidity, polypharmacy, and physiological changes that affect the pharmacokinetics and pharmacodynamics of drugs.1 Therefore, this population is more prone to using medications that can be considered inappropriate.
A potentially inappropriate medication (PIM) is any medication used by a patient that could introduce a significant risk of an adverse drug reaction (ADR), in particular when there is an equally or more effective alternative with lower risk available. In the elderly, ADRs can sometimes be difficult to recognize as they often present with unspecific symptoms (eg, falls, fatigue, and orthostatic hypotension). ADRs are observed 2–3 times more often in the elderly and account for 5%–17% of all hospital admissions.2 A systematic review has found a mean prevalence of ADRs in the elderly of 11% (95% CI: 5.1%–16.8%) and a prevalence of ADRs leading to hospitalization of 10% (95% CI: 7.2–12.8). These authors have also shown that increased comorbid complexity and increased number of medications were significantly associated with an increased risk of ADRs.3 It is estimated that 30%–60% could be prevented.2 A recent study has shown that 45.1% (95% CI: 33.1%–57.2%) of the ADRs leading to hospitalization were preventable.4 In the USA and Canada, the prevalence ranged between 14% and 37.0%;5 in Europe, the prevalence ranged between 23% and 43%.6 Differences found between both continents could be explained by different drug markets, different prescribing patterns, and most importantly, by the tool used to measure prevalence.7
Several tools have been developed to guide prescribing, to maximize the efficacy and safety of therapy, and to minimize the consequences of using PIMs, including costs, hospitalizations, and mortality.8 The Beers criteria (Mark Beers, MD) was the first tool, developed in 1991, and last updated in 2019 by the American Geriatric Society.9,10 Since then, a considerable number of tools have been developed, describing not only PIMs, but also drug–drug and drug–disease interactions.3 Most of these tools are based on explicit criteria, ie, are normally more drug- or disease-oriented and are developed based on literature review, expert opinions, and consensus techniques.3
Cardiovascular diseases ([CVDs] which also include cerebrovascular diseases) such as hypertension, coronary heart disease, congestive heart failure, stroke, and atrial fibrillation are prevalent among the elderly.11 They represent one of the leading causes of death worldwide, with 17.7 million deaths registered in 2015 (31.0% of all-cause mortality).12,13 In Europe, 3.9 million people (45.0% of all-cause mortality) have died from CVDs in 2016.13
Few studies have identified PIMs in patients with CVD. A study conducted in a cardiology service showed that 20% of hospitalized patients were previously exposed to a PIM in the ambulatory setting.14 However, information on PIMs associated with risk of cardiovascular adverse events, especially with major adverse cardiac and cerebrovascular events (MACCE) for elderly is still scarce. Some of these medications can increase the risk of cardiovascular events or even exacerbate underlying conditions. Our previous systematic review showed that there is a restricted number of PIMs described addressing their association with the risk of cardiovascular adverse events.20 Some pharmacotherapeutic groups have been established to be associated with cardiovascular events such as nonsteroidal anti-inflammatory drugs (NSAIDs), antipsychotics, selective calcium channel blockers, and dopaminergic agents. Unfortunately, the prevalence of those PIMs in elderly patients is still unknown.
The primary objective of this study was to assess the prevalence of PIMs with risk of MACCE in the elderly. We then specifically aimed to study the prevalence of PIMs with risk of cardiac and cerebrovascular adverse events (CCVAEs) and to study the presence of these PIMs in patients with previous history of CVD.
Materials and methods
Study design
A descriptive cross-sectional study was conducted, where a convenience sample (based on geographic criteria) of citizens living in long-term care facilities (LTCFs) in the region of Lisboa e Vale do Tejo and the region of Alentejo and independently in their own home (ambulatory) in the region of Lisboa e Vale do Tejo, Portugal were invited to participate. Citizens’ information (including drug use) was collected from two LTCFs in the region of Lisboa e Vale do Tejo and two LTCFs in the other region of Alentejo. While, for individuals who live independently in their own home, citizens’ information was collected from their community pharmacy.
Population and sample
The study population (n=904) consisted of 224 residents and 680 patients from the community pharmacy and the LTCF, respectively. In the LTCF, residents were eligible if they were aged 65 or older and living in the facility until 2017. In the community pharmacy, the study population was calculated based on the minimum legal number of inhabitants per pharmacy (3,500 inhabitants) and on the percentage of elderly living in the district of Cascais in 2016 (19.6%). Moreover, individuals were included if they were aged 65 or older and had their medication history available in the pharmacy database in 2017. We excluded patients if their records were out of date, ie, if there were no sales in 2017.
Outcomes’ definition and measurement
Our previous study focused on a systematic review of 24 PIM-lists, where PIMs associated with CCVAEs and MACCE were identified (Table S1 shows the full list of those PIMs). As the primary outcome, the presence of PIMs with risk of MACCE was defined as PIMs with risk of causing stroke, transient ischemic attack, myocardial infarction, heart failure, and cardiovascular death. A secondary outcome was defined as the presence of PIMs with risk of CCVAEs including the risk of hypertension, orthostatic or postural hypotension, bradycardia, QT prolongation, and cardiac arrhythmias.
Data extraction
Data were extracted for sociodemographics (age and sex), clinical features (number of comorbidities, previous history of CVD, and the presence of dementia), and drug-related characteristics (number of medications and presence of polypharmacy). The previous history of CVD and the presence of dementia were defined according to medication used to treat CVD and dementia, respectively, as a proxy. Polypharmacy was defined as taking five or more medications.15 Information on comorbidities was validated by one member of the research team (JPA) and then confirmed by a physician (LHC). For the records with medical diagnosis, the validation process was performed by comparing the available medical diagnoses with the medication used. When information was insufficient to reach a consensus, data were considered missing.
Ethics and confidentiality
The use of patients’ medical and pharmacotherapeutic records was authorized by the clinical directors of all participating institutions. To ensure anonymity, alphanumeric codes were used to identify the patients. All research was conducted following the principles of the Helsinki Declaration. Ethics approval was obtained from Comissão de Ética para a Investigação nas Áreas de Saúde Humana e Bem-Estar da Universidade de Évora (document 14017).
Data analysis
The total number of PIMs, total number of patients using PIMs, and total number of patients using PIMs with previous history of CVD were assessed. The most commonly described PIMs were analyzed and coded by pharmacotherapeutic groups, using the WHO ATC classification system.15
Statistical analysis was performed using IBM SPSS v.24.0. Descriptive statistics were used, where numerical variables were expressed using central tendency and dispersion measures (either as mean and SDs, whichever was applicable) and categorical variables as absolute and relative frequencies. Bivariate statistics were used to compare both settings regarding differences in sociodemographic, clinical, and pharmacotherapeutic features. Chi-squared test and Student’s t-test for independent samples were used, whichever was applicable considering a 95% CI. For numerical variables, normal distribution was also assessed.
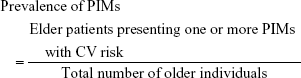
The prevalence of PIMs with the risk of CCVAE or MACCE occurrence was calculated using the following formula:
|
Results
Patients’ characteristics
From the initial 904 elderly patients, 63 were excluded from the LTCF sample and 161 from the community pharmacy sample due to missing data or records which were out of date. The final sample consisted of 680 patients, in which most of them were female (n=428; 62.9%) with a mean age of 78.4±8.1 years (range: 65; 101). Patients had a mean of 3.7±1.8 comorbidities, approximately 77.0% (n=521) presented with a history of CVD, and 10.7% (n=73) also presented with dementia. The total number of medications prescribed was 5,112, with a mean number of medications taken per patient of 7.5±4.2. Table 1 describes the sample’s sociodemographic and clinical features and details the differences by settings.
  | Table 1 Sociodemographic and clinical features of the Portuguese elderly sample |
In LTCF, patients were older than in the ambulatory setting (85.4±6.5 vs 76.7±7.5; P<0.0001). Patients in LTCFs were also more associated with a higher number of comorbidities (4.7 vs 3.5 comorbidities/patient; P<0.0001) and medications used (10.4 vs 6.8 medications/patient; P<0.0001) compared to ambulatory care.
PIMs with risk of CCVAEs
After applying the PIM-list specific for CCVAEs, a total of 682 PIMs were identified from the overall sample. Most of the patients (55.2%) took one PIM with a mean number of 1.7±1.0 PIMs used per patient. The prevalence of PIMs with risk of CCVAEs was 59.4% (n=404) and 47.4% (n=322) of patients had a previous history of CVD.
The prevalence of these PIMs among the elderly in LTCFs was substantially higher when compared to the ambulatory setting (78.1% vs 54.7%; P<0.0001). A similar proportion was observed for patients with a previous history of CVD (63.5% in LTCFs vs 46.6% in ambulatory setting; P<0.0001). These patients were also more prone to using two PIMs when compared to patients from ambulatory setting (33.6% in LTCFs vs 19.1% in ambulatory setting; P=0.001). Table 2 summarizes all previously described data.
In the overall sample, the pharmacotherapeutic groups most commonly found associated with cardiovascular risk of adverse events were: non-steroidal anti-inflammatory drugs ([NSAIDs] n=199; 29.7%); antipsychotics (n=118; 17.6%); thyroid preparations, ie, levothyroxine (n=70; 10.4%); and antidepressants (n=57; 8.5%). Other drug classes were also found to a lower extent: peripheral vasodilators, eg, nicergoline and pentoxifylline (n=33; 4.9%), natural products, eg, gingko biloba (n=25; 3.7%), antiarrhythmics, eg, amiodarone, flecainide, and propafenone (n=19; 2.8%); and cardiac glycosides, eg, digoxin (n=18; 2.7%). Table 3 describes all the pharmacotherapeutic groups with risk of CCVAEs found in the overall sample.
  | Table 3 Most commonly prescribed pharmacotherapeutic groups associated with risk of CCVAEs in both settings |
NSAIDs were mostly used by patients recruited from the community pharmacy (12.7% in LTCFs vs 36.2% in ambulatory setting), as well as thyroid preparations (8.8% in LTCFs vs 11.1% in ambulatory setting). Conversely, antipsychotics (38.7% vs 9.9% in ambulatory setting), dopaminergic agents (3.3% vs 0.6% in ambulatory setting), and cardiac glycosides (6.6% vs 1.2% in ambulatory setting) were more frequently found in patients from LTCFs.
PIMs with risk of MACCE
From the 682 PIMs identified, more than a half (n=378) were associated with risk of MACCE. A mean number of 1.4±0.8 PIMs were used per patient, with the majority of them using between one and two PIMs (92.4%). In the overall sample, the prevalence of PIMs with risk of MACCE was 38.8% (n=264), and 29.7% (n=202) of patients also had a previous history of CVD (Table 2).
The prevalence of these PIMs among the elderly was substantially higher in LTCFs compared to the ambulatory setting (51.8% vs 35.5%, respectively; P<0.0001). A similar proportion was observed for patients with a previous history of CVD (40.1% in LTCFs vs 27.1% in ambulatory setting; P=0.003).
NSAIDs (n=199; 53.1%) and antipsychotics (n=118; 31.5%) were the most prevalent drug classes in the overall sample. However, antipsychotics were mostly used by patients in LTCFs, and NSAIDs by patients from the ambulatory setting. To a lower extent, antidepressants (eg, venlafaxine), selective calcium channel blockers with mainly vascular effects (eg, nifedipine) were also identified. The individual drugs most commonly found in each group were: quetiapine (n=48; 40.7%); ibuprofen (n=46; 23.1%); diclofenac (n=43; 21.6%); melperone (n=19; 16.1%); cyamemazine (n=13; 11.0%); etoricoxib (n=20; 10.0%); and naproxen (n=20; 10.0%). Table 4 summarizes all the PIMs with risk of MACCE identified in the overall sample and by setting.
No differences were found in the distribution of pharmacotherapeutic groups. In patients with previous history of CVD, 91.7% (LTCFs =22/ambulatory =24) were using nifedipine, 81.0% (17/21) venlafaxine, 77.0% (10/13) estrogen, 76.7% (69/90) antipsychotics, and 76.1% (118/155) NSAIDs.
One of the subpopulations where antipsychotics should be avoided is the demented elderly patient. From the 73 demented patients, more than half (n=39; 53.4%) were taking antipsychotics. This value was even higher if we only restricted the analysis to LTCFs: 88% (22/25). Conversely, a lower proportion of patients in primary care used antipsychotics (n=17; 35.4%). In addition, the type of antipsychotics selected also seemed to be influenced by setting, where second-generation antipsychotics were more widely found in the ambulatory setting, whilst first-generation antipsychotics were most common in LTCFs.
Discussion
This study enabled the possibility of assessing the prevalence of PIMs with risk of CCVAEs and MACCE in an elderly Portuguese sample and, to the best of our knowledge this is the first study focusing on this topic in Europe. Inappropriate prescribing is more likely to occur in the elderly, since this subpopulation is generally using more medications to treat several chronic conditions. In this study, patients presented an average of 3.7±1.8 comorbidities and were taking on average 7.5±4.2 medications. The majority of these patients were taking PIMs with CCVAE risk (59.4%) and almost half of them were associated with MACCE risk. It is well-known that CVDs are frequently found in the elderly and are an important cause of morbidity and mortality in these patients. Thus, in patients with a previous history of CVD, the prevalence of PIM use was also high. A previous study focusing on the identification and quantification of PIMs with MACCE risk, using tools addressing inappropriate prescribing, was used to assess the prevalence of these medications in our sample. This list was driven by a previous systematic review that included 24 of the tools currently available (eg, Beers criteria, START/STOPP criteria, and Zhan criteria). Different studies, in different health care settings, have also investigated the prevalence of PIMs, but did not focus on a specific negative outcome. In Portugal, da Costa et al (2016) used different criteria to assess the prevalence of PIMs in elderly residents in nursing homes. They found that using Beers criteria, Beers criteria adapted to Portugal and START/STOPP criteria, the prevalence of PIMs was 85.1%, 60.3%, and 75.4%, respectively. These patients had an average age of 84.7±6.35 years and a mean of 4.1±2.14 comorbidities.16 Another study, conducted by Nyborg et al (2017), showed that the prevalence of PIMs in Norwegian elderly was 43.8%, using the Norwegian General Practice Nursing Home (NORGEP-HN) criteria.17 In the outpatient setting, in the USA, the prevalence of PIMs was 23.3% and 16.2% using the Beers criteria and Zhan criteria, respectively.18
The elderly tend to present with multiple chronic conditions, which increases the odds of using multiple medications. Many patients in this study had a previous history of CVDs and 10% also presented with dementia. The most commonly prescribed pharmacotherapeutic groups were NSAIDs and antipsychotics. NSAIDs are known to be associated with exacerbation of heart failure and to cause major cardiac events like stroke and myocardial infarction. Among NSAIDs, selective cyclooxygenase-2 (COX-II) inhibitors (eg, etoricoxib and celecoxib) are associated with an increased risk of myocardial infarction.19 In this study, 15.5% of patients took selective COX-II inhibitors. The 2015 Beers criteria alert for the potentially inappropriate prescribing of antipsychotics in patients with dementia. This pharmacotherapeutic group is known to be associated with an increased risk of stroke.10 Even though not many demented patients were found in our sample, almost 77.0% of them were taking antipsychotics. These medications were commonly used in patients in LTCFs, where more frail elderly patients can be found, and are normally used in combination with other high-risk medications for cardiovascular events, such as dopaminergic agents or antidepressants.
We assume patients in LTCFs seem to have a higher risk of MACCE occurrence because of a higher prevalence of PIMs’ use, in addition, a higher prevalence of medications with higher odds of drug–drug and drug–disease interactions was found. Additionally, these elderly patients have more comorbidities and use more medications increasing the cardiovascular risk for future events. These findings suggest that more attention should be paid to tertiary care to optimize medication, by reducing the use of these drugs.
The high prevalence of PIMs with the risk of CCVAEs and MACCE may suggest that interventions targeted at medication misuse need to be further developed and implemented into practice. However, we should keep in mind that the existing criteria, in most cases, do not explicitly assess patient-related indicators (eg, weight, cardiac disturbances, and patients with high cardiovascular risk score) or drug-related indicators (eg, route of administration, dosage, and frequency of exposure). A good example is levothyroxine. This drug does not have an alternative suggested in the lists and sometimes is considered as potentially inappropriate, given the risk for cardiac arrhythmias. This is surely a drawback in practice if we consider the likelihood of a clinician basing his decisions on such lists. Perhaps more complex and tailored indicators should be developed to target high-risk patients where the PIMs identified are indeed potentially inappropriate for that specific individual. A possible example of an intervention could be the familiarization or even the inclusion of these last indicators in an information and technology strategy to foster de-prescribing during the medication review process, where full clinical and laboratory details would be embedded in the software.
Limitations
This study has some limitations. First, to assess drug use in the ambulatory setting, we reported community pharmacy data which limited our ability to extract accurate information on patients’ comorbidities, and consequently the capacity to judge drug–disease interactions. Second, the number of comorbidities, the previous history of CVD, and the presence of dementia were based on the analysis of the pharmacotherapeutic regimen of each patient available in the community pharmacy and LTCF. We therefore believe that comorbidities are more likely to be underreported and some misclassification bias could also be present. However, to minimize this bias, we have assessed comorbidities as a group (history of CVD or dementia), instead of using individual diagnoses from both settings. Third, we had incomplete information on all drug-related variables in both settings, which did not allow for the extraction of the frequency of exposure. Finally, although we had a good sample size, the results should only be generalized to elderly patients included in those regions (restricted to both settings) and not nationwide.
Conclusion
More than half of the elderly included in our sample were using PIMs with risk of CCVAEs, and approximately 40% of those were associated with risk of MACCE. About half of patients with a previous history of CVD took PIMs. The most commonly used PIMs with risk of MACCE were NSAIDs and antipsychotics, which accounted for almost half of the total drugs assessed in this sample. Future interventions and more tailored tools for the management of drug therapy in elderly patients with CVD are of major importance.
Acknowledgments
The authors would like to acknowledge the LTCFs and the community pharmacy for all the work in data extraction and for their participation in this study. The authors would also like to thank Fundação para a Ciência e a Tecnologia, I.P. (FCT), Ministério da Ciência e da Tecnologia, Portugal for the PhD Grant to João Pedro Aguiar (SFRH/BD/132785/2017).
Disclosure
The authors report no conflicts of interest in this work.
References
Suzman R, Beard J. Global health and aging. NIH Publ. 2011;1(4):273–277. | ||
Brahma DK, Wahlang JB, Marak MD, Ch Sangma M. Adverse drug reactions in the elderly. J Pharmacol Pharmacother. 2013;4(2):91. | ||
Alhawassi TM, Krass I, Bajorek BV, Pont LG. A systematic review of the prevalence and risk factors for adverse drug reactions in the elderly in the acute care setting. Clin Interv Aging. 2014;9:2079–2086. | ||
Schmiedl S, Rottenkolber M, Szymanski J, et al. Preventable ADRs leading to hospitalization – results of a long-term prospective safety study with 6,427 ADR cases focusing on elderly patients. Expert Opin Drug Saf. 2018;17(2):125–137. | ||
Morin L, Laroche ML, Texier G, Johnell K. Prevalence of potentially inappropriate medication use in older adults living in nursing homes: a systematic review. J Am Med Dir Assoc. 2016;17(9):862.e1–862.e9. | ||
Tommelein E, Mehuys E, Petrovic M, Somers A, Colin P, Boussery K. Potentially inappropriate prescribing in community-dwelling older people across Europe: a systematic literature review. Eur J Clin Pharmacol. 2015;71(12):1415–1427. | ||
Komagamine J. Prevalence of potentially inappropriate medications at admission and discharge among hospitalised elderly patients with acute medical illness at a single centre in Japan: a retrospective cross-sectional study. BMJ Open. 2018;8(7):e021152. | ||
Barnes PJ. Mechanisms of development of multimorbidity in the elderly. Eur Respir J. 2015;45(3):790–806. | ||
Beers MH, Ouslander JG, Rollingher I, et al. Explicit criteria for determining inappropriate medication use in nursing home residents. UCLA division of geriatric medicine. Arch Intern Med. 1991;151(9):1825–1832. | ||
By the 2019 American Geriatrics Society Beers Criteria® Update Expert Panell. American Geriatrics Society 2019 Updated AGS Beers Criteria® for Potentially Inappropriate Medication Use in Older Adults. J Am Geriatr Soc. Epub 2019 Jan 29. | ||
By the American Geriatrics Society 2019 Beers Criteria Update Expert Panel. American Geriatrics Society 2019 Updated AGS Beers Criteria® for Potentially Inappropriate Medication Use in Older Adults. J Am Geriatr Soc. Epub 2019 Jan 29. | ||
Moher D, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement (Chinese edition). J Chin Integr Med. 2009;7(9):889–896. | ||
European Commission. Eurostat database. 2015. Available from: https://ec.europa.eu/eurostat/data/database. Accessed May 14, 2018. | ||
Sheikh-Taha M, Dimassi H. Potentially inappropriate home medications among older patients with cardiovascular disease admitted to a cardiology service in USA. BMC Cardiovasc Disord. 2017;17(1):1–6. | ||
World Health Organisation (WHO). Guidelines for ATC Classification and DDD Assignment. Oslo: WHO Collaborating Centre for Drug Statistics Methodology; 2003. | ||
da Costa FA, Periquito C, Carneiro MC, Oliveira P, Fernandes AI, Cavaco-Silva P. Potentially inappropriate medications in a sample of Portuguese nursing home residents: does the choice of screening tools matter? Int J Clin Pharm. 2016;38(5):1103–1111. | ||
Nyborg G, Brekke M, Straand J, Gjelstad S, Romøren M. Potentially inappropriate medication use in nursing homes: an observational study using the NORGEP-NH criteria. BMC Geriatr. 2017;17(1):1–11. | ||
Buck MD, Atreja A, Brunker CP, et al. Potentially inappropriate medication prescribing in outpatient practices: prevalence and patient characteristics based on electronic health records. Am J Geriatr Pharmacother. 2009;7(2):84–92. | ||
Trelle S, Reichenbach S, Wandel S, et al. Cardiovascular safety of non-steroidal anti-inflammatory drugs: Network meta-analysis. BMJ. 2011;342:c7086. | ||
Aguiar JP, Brito AM, Martins AP, Leufkens H, Costa FA. Potentially Inappropriate Medications with risk of Cardiovascular Adverse Events in the Elderly: a systematic review of tools addressing inappropriate prescribing”. Journal of Clinical Pharmacy and Therapeutics. 2019. |
Supplementary material
    | Table S1 Potentially inappropriate medications with risk of cardiovascular adverse events in the elderly |
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.