Back to Journals » Clinical Ophthalmology » Volume 14
Icare Home Tonometer: A Review of Characteristics and Clinical Utility
Authors Liu J , De Francesco T , Schlenker M, Ahmed II
Received 2 October 2020
Accepted for publication 30 October 2020
Published 23 November 2020 Volume 2020:14 Pages 4031—4045
DOI https://doi.org/10.2147/OPTH.S284844
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr Scott Fraser
John Liu,1,2 Ticiana De Francesco,1,2 Matthew Schlenker,1,2 Iqbal Ike Ahmed1,2
1Department of Ophthalmology and Vision Sciences, University of Toronto, Toronto, Ontario, Canada; 2Prism Eye Institute, Oakville, Ontario, Canada
Correspondence: Iqbal Ike Ahmed Tel +1 (905) 456-3937
Email [email protected]
Abstract: The Icare HOME (TA022, Icare Oy, Vanda, Finland) is rebound tonometer recently approved by the US Food and Drug Administration in March 2017 designed for self-measurement of intraocular pressure (IOP). IOP remains a major modifiable risk factor for glaucoma progression; however, IOP measurements typically occur through single office measurements on Goldmann applanation tonometry (GAT) and do not always reveal the complete picture of patient’s IOP patterns and daily fluctuations, which are important for accurate diagnosis and evaluation. Numerous studies have now compared the efficacy of the Icare HOME to that of GAT. The objective of this article is to review the existing literature surrounding the Icare HOME tonometer and its efficacy as a self-tonometer in comparison to GAT. The available literature has shown promising results in its accuracy of measuring IOP but suggests cautious usage in patients with central corneal thicknesses or IOP ranges that are outside of a certain range. This article will also provide details and example cases for when the Icare HOME may be most clinically useful.
Keywords: Icare HOME, Icare, self-tonometry, glaucoma
Background
Management of intraocular pressure (IOP) is the only readily modifiable risk factor known to slow the development and progression of glaucoma and visual disability.1–3 As glaucoma is a leading cause of permanent blindness worldwide,4 efforts to accurately monitor IOP changes over time are of paramount importance. Diurnal variation in intraocular pressure is well recognized; however, most decisions concerning glaucoma therapy are based on single IOP measurements captured at specific moments in office and therefore do not reflect IOP fluctuations over a 24-hour period. Studies have shown that over 75% of single IOP measurements taken between 7am and 9pm tend to miss the highest point of a diurnal curve5 and that a higher peak IOP may be an independent risk factor for progression of glaucoma.6,7 Asrani et al evaluated diurnal IOP fluctuation with home self-tonometry in a group of open-angle glaucoma patients with apparently controlled office IOP. They found that 29% of patients with a progressive visual field loss had IOP peaks compared with 5% of patients with a stable visual field.8
In its truest form, the most accurate measurement of IOP is done through an intracameral transducer. All other measurements are approximations of IOP through the cornea, sclera, or eyelid, including Goldmann applanation tonometry (GAT), which in fact underestimates true intracameral pressure.9 Having said that, GAT continues to be the reference standard in IOP measurement, and all IOP measurement devices are universally calibrated to GAT. However, GAT is only performed in office settings, which prevents clinicians from monitoring IOP changes outside of the office and may make it difficult to assess a pharmaceutical or surgical treatment’s effectiveness. Twenty-four-hour monitoring of IOP of hospitalized patients may provide the most accurate measurements and can reveal higher peaks and wider fluctuation of IOP than those found during office visits. However, this is inconvenient, costly, and impractical for monitoring over longer periods.
With the advent of self-tonometry, 24-hour monitoring at home may become a viable option. The ideal home tonometer would be reliable, user-friendly, portable, and convenient. Although various forms of ocular tonometry exist, rebound tonometry is particularly suited for this role.10 Rebound tonometers have shown to be comparable to GAT in measurement of IOP,11,12 and do not require regular calibration.13 Additionally, they can be adapted into a small portable device that can be used with minimal training and do not require any topical anesthetic. For this reason, rebound tonometry has been typically used for children and uncooperative patients in the past.14,15
The Icare Home (TA022, Icare Oy, Vanda, Finland) is a relatively new rebound tonometer approved by the US Food and Drug Administration in March 2017, specifically designed for self IOP measurements at home.16 This device provides a recording for out-of-office variations in IOP through self-tonometry, as well as electronic documentation of these measurements. As studies investigating the Icare HOME arise, this can inform practitioners regarding the utility of the Icare HOME and its role in the management of glaucoma. The objective of this article is to review the design, efficacy, and clinical utility of the Icare HOME tonometer.
Icare HOME Characteristics
How the Icare HOME Device Works
As a rebound tonometer, the Icare HOME employs the same mechanism in measuring intraocular pressure as the Icare TA01i (Icare Oy, Vanda, Finland), which was the first commercially available rebound tonometer in the United States. The Icare HOME uses a disposable probe roughly 40mm long that is propelled from the tonometer towards the cornea at a speed of 0.25–0.30 meters/second by an electrical-pulse generator that creates a magnetic field via a solenoid.14 The higher the IOP, the shorter the length of time that the probe touches the cornea, and the quicker it rebounds back into the tonometer. The moving speed of the probe back into the device causes a change in the magnetic field, and the tonometer calculates this value into an IOP.14 The device is battery operated and requires two CR123A lithium batteries.17 The Icare HOME has not been validated for a central corneal thickness (CCT) outside the range of 500–600µm and corneal astigmatism >3 dioptre cylinder.
The Icare HOME measures approximately 11cm x 8cm x 3cm and weighs roughly 150g. It features a power button on the back panel at the bottom of a panel of LED lights, and a measure button on the top of the device. Notably, the device features adjustable cheek and forehead supports marked at 2mm interval lengths (sizes A1 through to A24 for the forehead, and B1 through to B24 for the cheek). This allows the device to be customizable to a variety of facial anatomy, making it very user-friendly. The tip of the probe must be placed between 4 and 8mm from the centre of the cornea at the start of each measurement. Additionally, the device features three infrared eye sensors that can detect which eye is being measured (right vs left). To assist the user in knowing whether the device is held accurately, the device has an LED probe base light, which shines “green” when the instrument is held properly and ready to begin measuring or “red” when the instrument is not held properly18 (Figure 1).
 |
Figure 1 Icare HOME tonometer with a green light (top panel) that reassures that the device is held properly. |
To measure IOP, the probe is inserted into the probe base, and the device is turned on by holding the power button on the back for three seconds. The probe is then loaded into the probe base and remains magnetically attached so long as the device remains powered on. The user aligns the tonometer in front of their eye and the green, circular probe base light indicates it is ready to begin a measurement. This probe light greatly improves a potential disadvantage of home IOP measurements, which is ensuring adequate positioning and distancing of the probe to the patient’s own eye. IOP measurement can also be affected by the angular position of the probe to the apex of the cornea, the coaxial alignment of the optical axis of the eye, and any gravitational force due to tilting the measurement axis up or down can affect the IOP measurement. Additionally, lid position and orbicularis innervation can also affect the rebound velocity and induce IOP variation. These issues are minimized with usage of the green probe light, which indicates when the Icare HOME is correctly positioned for a more accurate measurement. The user can either press and hold the measurement button for the probe to collect six measurements in a row or press the measurement button briefly six times to collect six measurements one at a time. Once six measurements are taken successfully, the “done” LED light will illuminate on the back panel. The measurement recorded is the mean of four IOP values, excluding the maximum and minimum values of the six measurements taken.10 The patient can then repeat these steps for their fellow eye using the same probe, if necessary. It is important to note that the patient must be upright (not supine) when taking measurements, and the probe base must be positioned at 90° to the patient’s face17 (Figure 2).
 |
Figure 2 Icare HOME correctly positioned at 90° to the patient’s face. |
The Icare HOME does not display its IOP readings on a display for the patient to see immediately. Instead, the device must be connected to a computer with Icare LINK installed or Icare CLINIC cloud-based software (Icare Oy, Vanda, Finland). Through this software, one can access all recorded IOP data indicating the exact time and date of each measurement, the quality of the measurement, and whether the measurement was taken on the right or left eye. Typically, this is done at the eye clinic where a healthcare professional (HCP) can review the results and discuss their relevance to the patient. Restricting this immediate reading of IOP likely helps to reduce potential self-medication and unnecessary patient anxiety.19 Identifying artifacts, outliers, and poor quality measurements should be assessed and interpreted by an HCP. However, it has been argued that allowing patients to view their IOP data may assist them in obtaining better quality measurements.19
All patients must receive training from a certified HCP or delegate prior to using the Icare HOME for self-tonometry based on a set of criteria according to the Icare HOME manufacturer. The criteria to receive certification are the following: a) the first of the three Icare HOME readings taken by the patient and the GAT result measured by the HCP differ by 5mmHg or less; b) the range (max-min) of the three readings taken by the patient is 7mmHg or less; c) the positioning of the tonometer was correct during self-use as determined by the HCP. Only if all three of these conditions are met can a patient be certified to use the Icare HOME to perform self-tonometry. During the training session, the HCP will also “size” the patient and note down their forehead and cheek support measurements on a support position tag, to be kept in the patient’s Icare HOME carrying case. A Patient Guide provided to each patient explains the steps involved in using the device and includes diagrams on how to use the device, along with tips for general troubleshooting.18
Comparison Studies of Icare HOME to GAT
On July 30th, 2020 the search terms “Icare HOME” and “self-tonometry” were used to search the English language literature on PubMed, Google Scholar, and MEDLINE (Ovid). Articles from 2016 onwards were searched. Any study that did not provide data on self-tonometry of the Icare HOME (such as when operated by a partner or healthcare professional) was excluded from this review. Table 1 summarizes eight studies that explore the Icare HOME’s self-tonometry efficacy through comparison to GAT and investigation of its general usability and limitations. Although many studies on the Icare HOME compare other Icare devices in addition to GAT, the focus of this review is primarily on Icare HOME self-tonometry. All mean IOP differences in this review will be reported as GAT-Icare HOME (mean IOP of Icare HOME measurements subtracted from mean IOP of GAT measurements).
 |
Table 1 Summary of Icare HOME Comparison Studies to GAT |
As IOP from tonometry is measured through a patient’s cornea, corneal biomechanics are known to significantly affect the accuracy of IOP measurement with tonometry.20 However, it has also been shown that thin central corneal thickness (CCT) is associated with glaucomatous progression through visual field loss in comparison to a patient with normal CCT values at an equal IOP.21–23 Low corneal hysteresis (CH) is also associated with optic nerve and visual field damage in glaucoma.24,25 Although CCT and CH are sometimes viewed as independent factors for glaucoma progression, their association with inaccurate IOP measurement likely contributes to the increased risk of progression.26 Many of the following studies also explore relationships between corneal biomechanics and their effect on IOP measurements on the Icare HOME in comparison to GAT.
Dabasia et al27 presented one of the first studies to compare the Icare HOME to GAT in 2016. Seventy-six subjects (62 with glaucoma or ocular hypertension, 14 with no glaucoma-related diagnosis) were trained to use the Icare HOME, and 56 (74%) were able to correctly perform self-tonometry after training. They sampled a predominantly elderly population, with a median age of 68 years. Of note, a modified version of the manufacturer’s criteria for patient certification was used, although it still involved a comprehensive assessment of the patient’s ability to use the device. The mean difference in IOP measurements between the GAT and Icare HOME was found to be 0.3mmHg (95% limits of agreement (LOA) −4.6 to 5.2), indicating the Icare HOME slightly underestimated IOP measurements compared to GAT. Overall, 84% of Icare HOME measurements were within and 3mmHg of GAT measurements. It was also found that there was a greater mean IOP difference for CCT<500µm (1.9mmHg) and for CCT>600µm (1.0mmHg). Interestingly, for a CCT between 500 and 600µm, the mean IOP difference was −0.1mmHg, indicating a slight overestimation of IOP measurements for participants with corneal thicknesses that fall within the Icare HOME validated range. Of all subjects who were trained to perform self-tonometry, 84% agreed that the device was easy to use, and 91% agreed that they would use the device at home. No association was found between a subject’s ability to perform self-tonometry and gender, previous or current contact lens wear, hand dexterity, educational level, refractive error, or vertical palpebral aperture.
Mudie et al28 conducted a study with a larger population of 171 eligible participants, all of whom were glaucoma patients or suspected glaucoma patients. Participants were trained using the exact manufacturer’s criteria to use the Icare HOME, and 127 (74%) were successful. Of the 44 who were not certified, 7 withdrew due to time concerns, while 10 were not certified due to difficulty using the device, and 27 were unable to obtain Icare HOME measurements within 5mmHg to GAT. The participants had a mean age of 62 years. The mean difference in IOP measurements was found to be −0.33mmHg (SD 3.11mmHg). Interestingly, this study found that the Icare HOME slightly overestimated IOP compared to GAT, which contrasts to most other comparison studies. Overall, 91.3% of the Icare HOME measurements agreed within 5mmHg of GAT. This study only included patients with CCT thickness between 500 and 600µm, and no association between CCT and agreement of Icare HOME and GAT measurements were identified within that range. It also stratified accuracy by lower and higher IOP ranges and found that at lower IOP ranges (6–16mmHg), the Icare HOME device underestimated IOP by more than 7.5mmHg in 1 of 60 participants, and at higher IOP ranges (>23mmHg), it overestimated IOP by more than 7.5mmHg in 1 of 67 participants. This may be a result of the fact that corneal rigidity increases with increasing IOP in a non-linear fashion.29 At a lower IOP, the cornea is less stiff and thus rebound velocity is reduced and IOP is underestimated. At a higher IOP, the stiffer cornea will allow for a quicker rebound velocity on the rebound tonometer and will produce a relative overestimation of IOP. The reliability of Icare HOME was assessed by calculating an overall Coefficient of Variation (COV) of 7.02 from two measurements, compared to a COV of 5.9 from two measurements using GAT. The intraclass correlation coefficient (ICC) for the Icare HOME was 0.91 (95% confidence interval (CI) 0.89–0.94). No significant difference in IOP measurements was found when participants used their nondominant hand. Unique to their study, Mudie et al assessed participant comfort and safety with the Icare HOME by grading corneal staining with fluorescein dye and a discomfort score from 0 to 100. It was found that for 91% of patients (116/127), corneal staining remained the same before and after certification, and the average discomfort score increased insignificantly from 6.2 to 7.1 before and after certification, ranging from 0 to 80.
Noguchi et al30 provided a unique perspective and investigated the importance of diurnal measurements and the relative differences between the Icare HOME and GAT depending on time of day. This study assessed 43 healthy young participants with a mean age of 28.3 ± 4.7 years. Due to the younger population sampled, this may have underestimated the IOP relative to the population that the Icare HOME is targeted for. Younger eyes have been shown to have significantly different corneal biomechanical properties with lower corneal rigidity.31 A lower corneal rigidity would reduce the rebound velocity of the Icare HOME and thus underestimate IOP in comparison to GAT. The Icare HOME and GAT were compared 6 times a day every 2 hours from 0800h to 1800h. No certification process was outlined to determine who was eligible to use the Icare HOME. Similar diurnal IOP curves were observed between Icare HOME and GAT; however, the IOP values were significantly lower for the Icare HOME than for GAT at 1200h, 1600h, and 1800h. The mean overall difference in IOP measurements between Icare HOME and GAT at all time points was 1.03mmHg (95% LOA −3.91 to 5.98). There was a weak but significant (P = 0.038) tendency for the Icare HOME to overestimate the IOP in eyes having higher IOP values (>18mmHg) and underestimate the IOP in those having lower IOP values (<18mmHg). An intraclass correlation coefficient was calculated at 0.812 (95% CI 0.713–0.886) for Icare HOME self-tonometry. Additionally, 39.5% of participants described handling the Icare HOME as “easy to use”, 46.5% described it as “normal”, and 13.9% described it as “difficult to use.” Of note, this study postulated that IOP measurements are lower in the Icare HOME due to two reasons. Firstly, accommodation occurs when subjects must confirm the ring signal lit up as “green”, and it is known that accommodation reduces IOP. Secondly, when the eye accommodates, the eyeball rotates inwards slightly and the Icare HOME probe touches the temporal cornea; it has been shown previously that when the probe touches the cornea at an angle of 10 or 20 degrees towards the visual axis, IOP decreased by approximately 2mmHg.
Termuhlen et al32 compared Icare HOME and GAT with a population of 154 patients; 101 with a diagnosis of glaucoma, and 53 patients without a glaucoma diagnosis. There was no mention of a certification or training process. Because this study focused more on the difference between ophthalmologist-operated Icare HOME compared to patient-operated Icare HOME (self-tonometry), it did not explicitly provide a mean difference in IOP between self-tonometry with Icare HOME and GAT. However, the mean IOP for GAT was 15.9mmHg and the mean IOP for Icare HOME was 14.9mmHg, which is a difference of 0.9mmHg. The CCT of participants ranged from 407 to 685µm, and a linear regression demonstrated that the Icare HOME tended to overestimate IOP at higher CCT ranges, and underestimate IOP at lower CCT ranges relative to GAT. To note, the measurements used for the CCT comparison were from physician-operated Icare HOME measurements, not self-tonometry. Similar to previous studies, within lower ranges of IOP, the Icare HOME was found to underestimate IOP, whereas at higher IOP levels it overestimated IOP in comparison to GAT. This study compared patient satisfaction between usage of the Icare HOME and the Icare ONE, concluding that the Icare HOME scored significantly better.
Tagaki et al33 examined 130 participants in various glaucoma or suspected glaucoma patients. The mean age was 57.5 ± 13.1 years. They also demonstrated an average overestimation of IOP with Icare HOME compared to GAT, just like Mudie et al, the mean difference was −0.70mmHg (95% LOA −3.07 to 4.46mmHg), which is the only other study other than Mudie et al to report an overestimation of Icare HOME compared to GAT. In this study, participants did not receive a formal certification process according to Icare HOME certification criteria; instead, it was stated that 128 participants (98%) were able to correctly perform self-tonometry within 30 minutes, and the 2 that could not be excluded from the study. However, this study only included patients with a visual acuity of 20/25 or better. This study found a 10% increase in CCT predicted a 1.2% increase in difference in IOP between Icare HOME and GAT. A negative correlation between IOP difference and age was shown (with Icare HOME more likely to underestimate IOP at older ages), and a positive correlation between IOP difference and corneal astigmatism was shown (with Icare HOME more likely to overestimate IOP with greater astigmatism). To note, the associations with CCT, age, and astigmatism were found when the Icare HOME was operated by an ophthalmologist. Again, this study also mentioned that the Icare HOME underestimated IOP measurements in lower ranges of IOP, and overestimated IOP measurements in higher ranges of IOP when compared to GAT.
Pronin et al34 assessed 100 patients with diagnosed glaucoma or ocular hypertension with a mean age of 67.5 years. A total of 73% (73/100) of participants successfully were certified to use the Icare HOME. Participants spent a mean of 20.3 minutes to learn how to perform self-tonometry, and those who were unsuccessful in being certified were significantly older and had significantly worse visual acuity. There was no association found between successful certification and handedness. The mean difference in IOP (GAT-care HOME) was 2.66mmHg, which is on the higher end of underestimations of the Icare HOME from this review. This may be due to the fact that this studied only included confirmed glaucoma or ocular hypertension patients. These patients have been shown to have significantly lower CCTs and corneal hysteresis, which can result in a reduction in rebound velocity of the Icare HOME tonometer, resulting in significant underestimation of IOP in comparison to GAT. It was found that only 56% of Icare HOME measurements were within 5mmHg of GAT. Thinner CCT was associated with lower IOP measurements with Icare HOME. This same association was also noted for measurements with GAT, although not as strong. Questionnaire data revealed that 71% of participants felt the Icare HOME was easy to use, and 92% stated they would be happy to perform self-tonometry in the future. This study also found there was excellent agreement between measurements obtained with self-tonometry and measurements obtained by clinicians on the Icare HOME, with an ICC of 0.903.
Brown et al35 conducted a study focused more on corneal properties on IOP, but used Icare HOME self-tonometry measurements in comparison to the GAT. Of the 100 glaucoma or ocular hypertension patients with a mean age of 67.5 ± 10.9 years, 73% were successfully trained to use the Icare HOME. The mean IOP difference (GAT-Icare HOME) was 2.66mmHg (SD 3.13mmHg), identical to the larger difference found by Pronin et al. The mean IOP difference was significantly associated with CCT, with eyes with thinner CCT having a smaller IOP difference between Icare HOME and GAT. As this study focused more on corneal properties, it found that in univariable analyses, IOP measurements taken by Icare HOME were significantly associated with CCT, as well as corneal hysteresis (CH) and corneal resistance factor (CRF). However, in multivariable analyses, CH and CRF were significantly associated with CCT, but CCT was no longer significant. This indicates that CH and CRF are more important in determining accuracy of IOP measurement than CCT.
Cvenkel et al36 assessed 117 suspected glaucoma, open-angle glaucoma, or ocular hypertension participants, of which 96 participants (82%) fulfilled requirements for certification. The mean age of participants was 57.4 ± 14.9 years. This mean amount of time taken for participants to obtain three reliable measurements and obtain certification was 14.2 minutes. This was positively correlated with age, but not with gender or visual acuity. The mean IOP difference (GAT-Icare HOME) was 1.2mmHg (SD 2.4mmHg, 95% LOA −3.4 to 5.9mmHg). Overall, all Icare HOME readings were within 5mmHg of GAT in 93.8% (90/96) of patients. It was noted that the Icare HOME underestimated IOP at thinner CCT compared to thicker CCT, with a decrease in mean difference of 0.16mmHg for every 10µm thicker of CCT based on regression analysis. Survey data showed that 78.5% (93) of participants felt self-tonometry was easy to use, with 80.6% (75/93) participants stating they would use the device at home.
In summary, comparison studies of Icare HOME self-tonometry to GAT reveal that the mean difference in IOP (GAT-Icare HOME) ranged from −0.7mmHg to 2.66mmHg, and that ≥73% of participants were consistently successful in being certified or trained to use the device. Across most studies, there was an underestimation of IOP by Icare HOME when measuring in lower IOP ranges, and an overestimation of IOP by Icare HOME when measuring in higher IOP ranges. Studies also supported the overall user-friendliness and participant willingness to use the Icare HOME for self-tonometry at home through survey data. Although a few studies showed a correlation of increasing IOP difference between Icare HOME and GAT with an increase in CCT, the exact correlation between CCT and mean IOP difference was inconsistent and variable, potentially due to the variability of inclusion criteria for CCT values of participants. Further investigation may be required to deduce the exact relationship between CCT and accuracy of Icare HOME readings. To note, Brown et al discussed that biomechanical properties of the cornea such as corneal hysteresis and corneal resistance factor are more important factors in determining how the cornea will influence IOP measurement, which are not necessarily correlated with CCT, especially in eyes weakened with disease.35
A few discrepancies between studies are noted from this review. Firstly, the exact Icare HOME manufacturer criteria were not consistently used to train participants; some studies did not mention at all how they trained or certified patients (Noguchi et al and Termuhlen et al), while others (Dabasia et al and Takagi et al) modified the certification criteria to train participants. Takagi et al also only included patients with a visual acuity of 20/25 or better, which may have contributed to its high success rate of 98%. As a result, the success rate in adopting the Icare HOME among participants should be interpreted with caution in these studies. Additionally, masking of the investigator reading the Icare HOME measurements and performing GAT measurements was inconsistent, with certain studies leaving the investigator unmasked to both readings (Termuhlen et al) Frequency and number of IOP measurements taken were also inconsistent amongst studies. Some studies did not report how many IOP recordings were taken per participant with Icare HOME and GAT (Pronin et al and Brown et al), while other studies reported 1 measurement (Termuhlen et al) and 3 measurements (Dabasia et al, Mudie et al, Takagi et al, and Cvenkel et al). Only Noguchi measured diurnal fluctuations throughout the day (every 2 hours from 0800h to 1800h) with both Icare HOME and GAT, and thus had the largest number of readings per participant to compare both devices. Finally, amongst studies that assessed CCT, the devices used for determining CCT varied. Some studies used an Accutome Pachpen (Dabasia et al), while others used a DGH Technology Pachmate (Cvenkel et al).
Clinically Relevant Take-Home Points
A review of these studies suggests a few clinically relevant points, which can inform clinicians when deciding when it would be advisable to rely on Icare HOME self-tonometry measurements. Firstly, with such a varied population sampled across studies but with a consistent majority of participants being certified to use Icare HOME, it appears that feasibility of the Icare HOME is not significantly affected by population demographic. As noted by Dabasia et al, handedness, gender, education level, contact lens wear, refractive error, and vertical palpebral aperture do not appear to affect usage of the Icare HOME. However, tremor and arthritis in elderly participants were mentioned by Dabasia et al as hindrances to successfully performing self-tonometry in 2 participants. Secondly, CCT appears to affect Icare HOME readings in an inconsistent manner. It is therefore no surprise that the manufacturer criteria states that the Icare HOME is only validated to be used in patients with a CCT between 500 and 600nm. Although it has long been recognized that CCT measurements affect GAT readings, they appear to be even more affected with Icare HOME readings. Further, it appears that a “mid-range” IOP is ideal for the most reliable IOP readings. Mudie et al stratified participants into three IOP groups: 6.1mmHg to 16mmHg, >16mmHg to <23mmHg, and ≥23mmHg while Noguchi et al analyzed IOP ranges in two groups: >18mmHg and <18mmHg. Both studies indicated that participants in the groups with higher IOPs were more likely to have IOP overestimated with Icare HOME readings and the groups with lower IOPs were more likely to have IOP underestimated. A thorough analysis involving how the reliability of Icare HOME readings are affected along the continuum of IOP ranges was not discussed in any study and warrants further investigation. Nevertheless, it would be reasonable to suggest that the Icare HOME is most accurate in the “middle ranges” of roughly 16mmHg to 23mmHg. Participants in this IOP group did not have any differences greater than 7.5mmHg between Icare HOME readings and GAT according to Mudie et al. To note, a study conducted by Huang et al (not included in this review due to lack of self-tonometry data) adapted an equation to calculate the upper limit of expected Icare HOME IOP measurements with respect to in-office GAT measurements based on a linear regression model.28 This could assist clinicians in identifying clinically relevant IOP elevations from the Icare HOME. Future studies on the Icare HOME could aim to employ a similar regression model to correct for high/low IOP ranges and CCT values.
Clinical Utility of the Icare HOME
The value of Icare HOME tonometry lies more so in monitoring patients at risk due to diurnal variations in IOP rather than its alternative use as a tonometer with similar accuracy to GAT. As a result, we will discuss how the Icare HOME can be most useful in clinical practice. A few published studies have demonstrated the clinical utility of the Icare HOME. Cvenkel et al provided the Icare HOME to patients with glaucoma or ocular hypertension and found that eyes with significantly higher average IOP, peak IOP, and higher IOP fluctuation as measured on the Icare HOME were the eyes that showed progression in glaucoma (defined as significant visual field deterioration or optic nerve head/retinal nerve fiber layer changes), despite stable in-office IOP measurements.36 Additionally, Awadalla et al found that a significant reduction in mean IOP after selective laser trabeculoplasty could be detected when providing Icare HOME devices to patients after their procedure.37 These studies demonstrate the Icare HOME’s role in obtaining an accurate IOP profile to assist in treatment decision-making, which complement similar findings from our own practice.
In our practice, patients are trained by a healthcare professional before renting the device and usually take the tonometer home for 5–7 days. We encourage our patients to continue their usual daily life routine and try to obtain as many measurements as possible with measurements taken during one overnight period. We also suggest patients to log activities when using Icare HOME to potentially correlate readings to certain activities (ie, awake or sleeping, drop administration, physical activity, and meals). By obtaining consistent measurements over a period of 5–7 days, we are able to identify daily trends that can help to exclude artifacts or outliers.
As IOP – particularly peak IOP – is considered an important variable in glaucoma risk, target IOPs are often based on this measure. Conceivably, home tonometry should then be performed for all glaucoma patients at diagnosis and after therapeutic interventions. However, for practical reasons, we recommend it most useful to perform Icare HOME in patients who present with reasonable in office IOP, but with uncertainty as to if their disease is controlled. This uncertainty could arise from significant visual field progression, optic nerve head and retinal nerve fiber layer changes, or anything that raises suspicion from a clinician’s own judgment.
We find that certain types of glaucoma could particularly benefit with additional IOP monitoring with the Icare HOME – particularly those with pigment dispersion glaucoma, suspects of angle-closure glaucoma, and normal-tension glaucoma (NTG). As Icare HOME users are asked to provide us with a diary of their activities and glaucoma medication routine while monitoring their IOP with Icare HOME, this can assist in detecting whether the IOP spike is related to physical exertion in pigment dispersion glaucoma cases. When dealing with patients with progressive NTG, a better understanding of the patient’s overall IOP profile can help us to identify how important the IOP-dependent factors are, which can help to decide target IOP when operating on these patients. We are able to more confidently decide if we should aim for single-digit IOPs with a tight therapeutic window just above hypotony (ie, 6–8mmHg) or target IOPs around 12mmHg while ensuring we keep peak IOPs also at this level. The findings of an elevated peak IOP on diurnal testing may reduce the need (and risk) of aiming for extremely aggressive sub-physiologic IOPs and address fluctuations more so with surgery, while a low peak IOP would tilt us to be more aggressive with the choice of surgical procedure. Considering the wide range of IOP fluctuation in some angle closure and angle closure suspect patients, the use of Icare HOME tonometry in these eyes can provide useful insight into disease control and timing of intervention. Finally, we have also begun using the Icare HOME to monitor postoperative IOP control, as it can be very reassuring for both physicians and patients to know how well a patient is doing after a surgical intervention. Overall, the Icare HOME tonometer adds an extra tool to our diagnostic armamentarium.
Examples from Practice
Utility of the Icare HOME is best demonstrated through examples where usage of the Icare HOME led to diagnoses or clinical findings that would have otherwise been missed. The following five clinical cases arise from our practice where information from the Icare HOME was critical in altering decisions for glaucoma management. Although some of these cases demonstrate changes in IOP demonstrated on Icare HOME before and after a surgical or medical intervention, it should also be noted that procedures such as a trabeculectomy as well as IOP-lowering medications can affect corneal biomechanics and alter true changes in IOP measurement.38,39
Case 1
A sixty-year-old Caucasian male with mild pigmentary glaucoma presented with a suspicion of glaucomatous progression in visual fields despite apparently “controlled” IOP in the mid-teens for 7 years. This patient had no visual symptoms related to physical exertion. IOP monitoring with Icare HOME tonometer showed significant peak IOP fluctuations up to 32mmHg in the right eye and 43mmHg in the left eye (Figure 3). Glaucoma tests were repeated, and visual field progression was confirmed despite maximal glaucoma medical therapy with good compliance. Trabeculectomy was performed in the right eye, and a gonioscopy-assisted trabeculotomy (GATT) was performed for the left eye. Six months after both surgeries, the patient had apparently reasonable IOP control (right 6mmHg, left 12mmHg). However, a dramatic visual field progression in the left eye was noticed, and IOP monitoring with Icare HOME was again performed.
 |
Figure 3 Case 1 Preoperative Icare HOME Results. |
Postoperative Icare HOME monitoring showed great IOP improvement for the right eye with no significant IOP variation. Interestingly, for the left eye, the highest IOP registered was over 40mmHg with significant IOP fluctuation (Figure 4), despite the apparently reasonable IOP control in the office. Medical treatment was attempted; however, a trabeculectomy was ultimately performed in the left eye as well.
 |
Figure 4 Case 1 Postoperative Icare HOME Results. |
Case 2
A 55-year-old female presented with advanced, progressive, NTG in her right eye. Over the past four years, in-office IOPs had remained in the low teens in both eyes as the Optical Coherence Tomography (OCT) and Visual Fields (VF) continued to deteriorate in the right eye only with the left eye remaining stable. The patient participated in a sleep study and 24-hour blood pressure monitoring with results unremarkable. Icare HOME was then prescribed to the patient and confirmed significant peak IOP fluctuations up to 20mmHg with a standard deviation of 3.5 in the right eye (Figure 5). The left eye also showed some peak IOP elevation, although less than the right eye and was non-progressive with similar office IOP readings.
 |
Figure 5 Case 2 Preoperative Icare HOME Results. |
A subconjunctival micro-invasive surgical implant was successfully placed in the patient’s right eye. A postoperative Icare HOME evaluation revealed a much lower peak IOP following surgery (Figure 6) on no glaucoma medication and at three months the postoperative IOP remained controlled between 5 and 10mmHg.
 |
Figure 6 Case 2 Postoperative right eye Icare HOME Results. |
Case 3
A 61-year-old female with advanced open-angle glaucoma in both eyes was referred for surgical management. Her left eye had a complicated course after trabeculectomy surgery with resultant chronic hypotony and poor vision, while right eye had advanced visual field loss and over the last 3 years was felt to be progressing despite in-office IOP measurements in the low teens on 4 classes of medications. Both non-IOP and IOP-related factors for progression were considered, and the Icare HOME tonometer was prescribed for one week (Figure 7).
 |
Figure 7 Case 3 Preoperative Icare HOME Results. |
Icare HOME demonstrated IOP fluctuations with a high of 20mmHg in the morning. Risks and benefits of any procedure with the likely chance of further progression were considered. The decision to proceed with a subconjunctival micro-invasive glaucoma surgery was made and successfully performed. Over the course of the year after surgery, IOP was controlled with pressures between 6 and 8mmHg and on no glaucoma drops.
Case 4
A 61-year-old male with advanced glaucoma, worse in the left eye than right eye presented with IOP in the high teens, approaching the low twenties pre-treatment. Additionally, there had been visual field progression over the last 2 years with central fixation loss while on 3 glaucoma medications in both eyes. The Icare HOME tonometer was prescribed to obtain a more accurate assessment of IOP control. Results indicated IOP fluctuations into the thirties in both eyes (Figure 8).
 |
Figure 8 Case 4 Preoperative Icare HOME Results. |
Subconjunctival micro-invasive glaucoma surgery was then performed in the left eye to achieve better IOP control. Postoperative Icare HOME results showed minimal IOP fluctuations in the left eye while the right eye still showed significant IOP elevations (Figure 9). The patient is currently off glaucoma medications and at a one year postoperative follow up showed a controlled IOP between 7 and 11mmHg. The right eye has recently undergone the same procedure with similar early results (Figure 10).
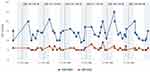 |
Figure 9 Case 4 Postoperative Icare HOME Results (after surgery on left eye). |
 |
Figure 10 Case 4 Postoperative Icare HOME Results (after surgery on right eye). |
Case 5
A 67-year-old female presented with moderate normal pressure glaucoma in both eyes. Over the past eight years, in-office IOPs had remained in the low teens in both eyes as the OCT and VF continued to deteriorate in the right eye. A workup for non-IOP mechanisms of optic neuropathy, including 24-hour blood pressure monitoring and a sleep study was done, with unremarkable results. The Icare HOME tonometer was prescribed to obtain additional IOP monitoring. Results indicated low peak IOP with the highest IOP of 12 and the lowest of 5 in the right eye (Figure 11). As the peak IOP was low, we decided to be more aggressive with the surgical procedure’s choice. A trabeculectomy was performed in the right eye aiming for single-digit IOPs with a tight therapeutic window just above hypotony. For the left eye, progression was not obvious and was decided to continue observation with glaucoma medications.
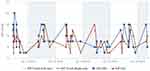 |
Figure 11 Case 5 Preoperative Icare HOME Results. |
Conclusion
At the time of writing this article, the COVID-19 pandemic has significantly changed healthcare delivery worldwide with physical distancing measures necessitating a rapid shift to virtual delivery of clinical care. As a result, home tonometers such as the Icare HOME would prove an invaluable resource by allowing clinicians to maintain follow-up for glaucoma patients without the need to physically see them in their clinics. With the electronic storage of IOP data within the device, integration into a clinic’s electronic medical record would allow for streamlined virtual data collection. Additionally, the Icare HOME provides an additional tool in providing healthcare access for rural and remote areas, who may no longer need to travel far as frequently to visit an eye care specialist.
In summary, the Icare HOME has demonstrated excellent potential to transform the traditional approach to glaucoma diagnosis and management. Our review indicates that the Icare HOME is reasonably similar to GAT measurements, easy to use, and well accepted by patients. Preliminary examples have demonstrated ways in which the Icare HOME can be used clinically to guide and customize glaucoma management. Continued strict review of the Icare HOME’s accuracy, feasibility, areas for improvement, as well as potential for future applications is important in adapting this technology widely.
Abbreviations
IOP, intraocular pressure; GAT, Goldmann applanation tonometry; CCT, central corneal thickness; NTG, normal-tension glaucoma; OCT, optical coherence tomography; VF, visual fields.
Ethics
This article was exempt from approval from the Trillium Health Partners Research Ethics Board as no intervention on human participants occurred. The authors all adhered to the Declaration of Helsinki.
Consent for Publication
Informed consent for publication was obtained from patients for the clinical cases.
Author Contributions
All authors made a significant contribution to the work reported, whether in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
Dr John Liu reports grants from iCare USA Inc., during the conduct of the study. Dr Ticiana De Francesco reports grants from iCare USA Inc., during the conduct of the study. Dr Matthew Schlenker reports grants from iCare USA Inc., during the conduct of the study; personal fees from Abbvie, Thea-Labtician, Santen, and Zeiss, grants and personal fees from Alcon, Bausch Health, and J&J, outside the submitted work. Dr Iqbal (Ike) Ahmed reports personal fees from Aequus, grants from Aerie Pharmaceuticals, Camras Vision, Glaukos, Ivantis, New World Medical, and Santen, grants and speakers honoraria from Alcon, Allergan, and Johnson and Johnson, speakers honoraria for Carl Zeiss Meditec, MST Surgical, and MundiPharma, consulting from Akorn, consulting from ArcScan, consulting from Bausch Health, consulting from Beaver Visitec, consulting from Beyeonics, consulting from CorNeat Vision, consulting from Ellex, consulting from ELT Sight, consulting from Elutimed, consulting from Equinox, consulting from Genentech, consulting from Gore, consulting from InjectSense, consulting from Iridex, consulting from iStar, consulting from KeLoTec, consulting from LayerBio, consulting from Leica Microsystems, consulting from Long Bridge Medical, consulting from MicroOptx, consulting from Mynosys, consulting from Ocular Instruments, consulting from Ocular Therapeutix, consulting from Omega Ophthalmics, consulting from PolyActiva, consulting from Sanoculis, consulting from Science Based Health, consulting from Sight Sciences, consulting from Smartlens, consulting from Stroma, consulting from Thea Pharma, consulting from ViaLase, consulting from Vizzario, outside the submitted work. The authors report no other potential conflicts of interest for this work.
References
1. Heijl A. Reduction of intraocular pressure and glaucoma progression: results from the early manifest glaucoma trial. Arch Ophthalmol. 2002;120(10):1268. doi:10.1001/archopht.120.10.1268
2. The advanced glaucoma intervention study (AGIS): 7. the relationship between control of intraocular pressure and visual field deterioration. Am J Ophthalmol. 2000;130(4):429–440. doi:10.1016/S0002-9394(00)00538-9
3. Canadian Glaucoma Study: 3. Impact of risk factors and intraocular pressure reduction on the rates of visual field change. Arch Ophthalmol. 2010;128(10):1249. doi:10.1001/archophthalmol.2010.196
4. Tham Y-C, Li X, Wong TY, Quigley HA, Aung T, Cheng C-Y. Global prevalence of glaucoma and projections of glaucoma burden through 2040. Ophthalmology. 2014;121(11):2081–2090. doi:10.1016/j.ophtha.2014.05.013
5. Jonas JB, Budde W, Stroux A, Oberacher-Velten IM. Single intraocular pressure measurements and diurnal intraocular pressure profiles. Am J Ophthalmol. 2005;139(6):1136–1137. doi:10.1016/j.ajo.2004.12.012
6. Konstas AGP, Irkec MT, Teus MA, et al. Mean intraocular pressure and progression based on corneal thickness in patients with ocular hypertension. Eye. 2009;23(1):73–78. doi:10.1038/sj.eye.6702995
7. Zeimer RC, Wilensky JT, Gieser DK, Viana MAG. Association between intraocular pressure peaks and progression of visual field loss. Ophthalmology. 1991;98(1):64–69.
8. Asrani S, Zeimer R, Wilensky J, Gieser D, Vitale S, Lindenmuth K. Large diurnal fluctuations in intraocular pressure are an independent risk factor in patients with glaucoma. J Glaucoma. 2000;9(2):134–142.
9. McCafferty S, Levine J, Schwiegerling J, Enikov ET. Goldmann applanation tonometry error relative to true intracameral intraocular pressure in vitro and in vivo. BMC Ophthalmol. 2017;17(1):215.
10. Nakakura S. Icare rebound tonometers: review of their characteristics and ease of use. OPTH. 2018;12:1245–1253. doi:10.2147/OPTH.S163092
11. Gao F, Liu X, Zhao Q, Pan Y. Comparison of the iCare rebound tonometer and the Goldmann applanation tonometer. Exp Ther Med. 2017;13(5):1912–1916. doi:10.3892/etm.2017.4164
12. Iliev ME, Goldblum D, Katsoulis K, Amstutz C, Frueh B. Comparison of rebound tonometry with Goldmann applanation tonometry and correlation with central corneal thickness. British J Ophthalmol. 2006;90(7):833–835. doi:10.1136/bjo.2005.089870
13. iCare TECHNICAL SERVICES [Internet]. Icaretonometer. Available from: https://www.icaretonometer.com/technical-repair-services/.
14. Lambert SR, Melia M, Buffenn AN, Chiang MF, Simpson JL, Yang MB. Rebound tonometry in children. Ophthalmology. 2013;120(4):e21–7. doi:10.1016/j.ophtha.2012.09.058
15. Flemmons MS, Hsiao Y-C, Dzau J, Asrani S, Jones S, Freedman SF. Home tonometry for management of pediatric glaucoma. Am J Ophthalmol. 2011;152(3):470–478.e2. doi:10.1016/j.ajo.2011.03.001
16. iCare USA. Icare USA Receives FDA Clearance for Icare HOME Tonometer [Internet]. Eyewire News; 2017. Available from: https://eyewire.news/articles/fda-cleared-icare-home-iop-self-monitoring/.
17. Icare HOME. Icare HOME Patient Guide [Internet]. Icare Finland Oy; 2019. Available from: https://www.icaretonometer.com/wp-content/uploads/2020/05/200122_Icare_HOME_Patient_Guide_TA022-035-EN-4.0_LOW.pdf.
18. Icare HOME: instruction manual for health care professionals [Internet]. Icare Finland Oy; 2014. Available from: http://www.icaretonometer.com/wp-content/uploads/2014/06/Icare_HOME_instruction_manual_TA022-036_EN-3-1_lo.pdf.
19. Cvenkel B, Velkovska MA, Jordanova VD. Self-measurement with Icare HOME tonometer, patients’ feasibility and acceptability. Eur J Ophthalmol. 2020;30(2):258–263. doi:10.1177/1120672118823124
20. Costin BR, Fleming GP, Weber PA, Mahmoud AM, Roberts CJ. Corneal biomechanical properties affect Goldmann applanation tonometry in primary open-angle glaucoma. J Glaucoma. 2014;23(2):69–74. doi:10.1097/IJG.0b013e318269804b
21. Kotecha A, Elsheikh A, Roberts CR, Zhu H, Garway-Heath DF. Corneal thickness- and age-related biomechanical properties of the cornea measured with the ocular response analyzer. Invest Ophthalmol Vis Sci. 2006;47(12):5337. doi:10.1167/iovs.06-0557
22. Iester M, Mete M, Figus M, Frezzotti P. Incorporating corneal pachymetry into the management of glaucoma. J Cataract Refract Surg. 2009;35(9):1623–1628.
23. Kass MA. The ocular hypertension treatment study: a randomized trial determines that topical ocular hypotensive medication delays or prevents the onset of primary open-angle glaucoma. Arch Ophthalmol. 2002;120(6):701. doi:10.1001/archopht.120.6.701
24. Deol M, Taylor DA, Radcliffe NM. Corneal hysteresis and its relevance to glaucoma. Curr Opin Ophthalmol. 2015;26(2):96–102. doi:10.1097/ICU.0000000000000130
25. Medeiros FA, Meira-Freitas D, Lisboa R, Kuang T-M, Zangwill LM, Weinreb RN. Corneal hysteresis as a risk factor for glaucoma progression: a prospective longitudinal study. Ophthalmology. 2013;120(8):1533–1540. doi:10.1016/j.ophtha.2013.01.032
26. Medeiros FA, Weinreb RN. Is corneal thickness an independent risk factor for glaucoma? Ophthalmology. 2012;119(3):435–436. doi:10.1016/j.ophtha.2012.01.018
27. Dabasia PL, Lawrenson JG, Murdoch IE. Evaluation of a new rebound tonometer for self-measurement of intraocular pressure. Br J Ophthalmol. 2016;100(8):1139–1143. doi:10.1136/bjophthalmol-2015-307674
28. Mudie LI, LaBarre S, Varadaraj V, et al. The Icare HOME (TA022) Study. Ophthalmology. 2016;123(8):1675–1684. doi:10.1016/j.ophtha.2016.04.044
29. Tonnu P-A. The influence of central corneal thickness and age on intraocular pressure measured by pneumotonometry, non-contact tonometry, the Tono-Pen XL, and Goldmann applanation tonometry. British J Ophthalmol. 2005;89(7):851–854. doi:10.1136/bjo.2004.056622
30. Noguchi A, Nakakura S, Fujio Y, et al. A pilot evaluation assessing the ease of use and accuracy of the new self/home-tonometer icarehome in healthy young subjects. J Glaucoma. 2016;25(10):835–841. doi:10.1097/IJG.0000000000000457
31. Vitályos G, Kolozsvári BL, Németh G, et al. Effects of aging on corneal parameters measured with Pentacam in healthy subjects. Sci Rep. 2019;9(1):3419. doi:10.1038/s41598-019-39234-x
32. Termühlen J, Mihailovic N, Alnawaiseh M, Dietlein TS, Rosentreter A. Accuracy of measurements with the iCare HOME rebound tonometer. J Glaucoma. 2016;25(6):533–538. doi:10.1097/IJG.0000000000000390
33. Takagi D, Sawada A, Yamamoto T. Evaluation of a new rebound self-tonometer, Icare HOME: comparison with Goldmann applanation tonometer. J Glaucoma. 2017;26(7):613–618. doi:10.1097/IJG.0000000000000674
34. Pronin S, Brown L, Megaw R, Tatham AJ. Measurement of intraocular pressure by patients with glaucoma. JAMA Ophthalmol. 2017;135(10):1030. doi:10.1001/jamaophthalmol.2017.3151
35. Brown L, Foulsham W, Pronin S, Tatham AJ. The influence of corneal biomechanical properties on intraocular pressure measurements using a rebound self-tonometer. J Glaucoma. 2018;27(6):511–518. doi:10.1097/IJG.0000000000000948
36. Cvenkel B, Atanasovska Velkovska M. Self-monitoring of intraocular pressure using Icare HOME tonometry in clinical practice. OPTH. 2019;13:841–847. doi:10.2147/OPTH.S198846
37. Awadalla MS, Qassim A, Hassall M, Nguyen TT, Landers J, Craig JE. Using Icare HOME tonometry for follow‐up of patients with open‐angle glaucoma before and after selective laser trabeculoplasty. Clin Experiment Ophthalmol. 2020;48(3):328–333. doi:10.1111/ceo.13686
38. Pakravan M, Afroozifar M, Yazdani S. Corneal biomechanical changes following trabeculectomy, phaco-trabeculectomy, ahmed glaucoma valve implantation and phacoemulsification. J Ophthalmic Vis Res. 2014;9(1):7–13.
39. Radcliffe N, Berdahl J, Ibach M, Schweitzer J, Levine J, McCafferty S. Improved efficacy of topical latanoprost 0.005% demonstrated by corneal biomechanical correcting modified Goldmann prism. OPTH. 2020;14:2245–2253. doi:10.2147/OPTH.S264055
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
