Back to Journals » Clinical Ophthalmology » Volume 8
Hypertensive phase and early complications after Ahmed glaucoma valve implantation with intraoperative subtenon triamcinolone acetonide
Authors Turalba A, Pasquale L
Received 18 March 2014
Accepted for publication 14 May 2014
Published 11 July 2014 Volume 2014:8 Pages 1311—1316
DOI https://doi.org/10.2147/OPTH.S64257
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Angela V Turalba,1,2 Louis R Pasquale1,2
1Department of Ophthalmology, Massachusetts Eye and Ear Infirmary, Boston, MA, USA; 2Department of Ophthalmology, Harvard Medical School, Boston, MA, USA
Objective: To evaluate intraoperative subtenon triamcinolone acetonide (TA) as an adjunct to Ahmed glaucoma valve (AGV) implantation.
Design: Retrospective comparative case series.
Participants: Forty-two consecutive cases of uncontrolled glaucoma undergoing AGV implantation: 19 eyes receiving intraoperative subtenon TA and 23 eyes that did not receive TA.
Methods: A retrospective chart review was performed on consecutive pseudophakic adult patients with uncontrolled glaucoma undergoing AGV with and without intraoperative subtenon TA injection by a single surgeon. Clinical data were collected from 42 eyes and analyzed for the first 6 months after surgery.
Main outcome measures: Primary outcomes included intraocular pressure (IOP) and number of glaucoma medications prior to and after AGV implantation. The hypertensive phase (HP) was defined as an IOP measurement of greater than 21 mmHg (with or without medications) during the 6-month postoperative period that was not a result of tube obstruction, retraction, or malfunction. Postoperative complications and visual acuity were analyzed as secondary outcome measures.
Results: Five out of 19 (26%) TA cases and 12 out of 23 (52%) non-TA cases developed the HP (P=0.027). Mean IOP (14.2±4.6 in TA cases versus [vs] 14.7±5.0 mmHg in non-TA cases; P=0.78), and number of glaucoma medications needed (1.8±1.3 in TA cases vs 1.6±1.1 in the comparison group; P=0.65) were similar between both groups at 6 months. Although rates of serious complications did not differ between the groups (13% in the TA group vs 16% in the non-TA group), early tube erosion (n=1) and bacterial endophthalmitis (n=1) were noted with TA but not in the non-TA group.
Conclusions: Subtenon TA injection during AGV implantation may decrease the occurrence of the HP but does not alter the ultimate IOP outcome and may pose increased risk of serious complications within the first 6 months of surgery.
Keywords: Ahmed valve, hypertensive phase, triamcinolone
Introduction
Glaucoma drainage devices have become a valuable tool in the surgical management of refractory glaucoma. They are effective in reducing intraocular pressure (IOP) and are especially useful in cases where there is high risk of failure for a filtering procedure.1,2 The Ahmed glaucoma valve (AGV) is widely used because of the set internal resistance that obviates the need for modifications to the implant at the time of surgery to prevent postoperative hypotony.
The AGV has been shown to have comparable intermediate-term efficacy with its nonvalved counterpart, the Baerveldt glaucoma implant (BGI), in two prospective randomized clinical trials.3,4 However, the AGV resulted in slightly less IOP lowering compared with the BGI. Insertion of the AGV has been shown to be associated with a hypertensive phase (HP), a period of time in the early postoperative course when the IOP rises.5,6 The development of the HP has been shown to be associated with higher final IOP.6 Although some studies have shown that this early IOP elevation resolves in a subset of patients, in a significant number of patients IOP-lowering medications are required to maintain IOP control in the longer term.6 Encapsulation of the plate early in the postoperative period is thought to be responsible for decreased aqueous flow through the AGV, resulting in this early rise in IOP.7 Tenon’s cysts that are clinically observed in patients after AGV implantation support the notion that distal resistance is the primary mechanism for early IOP elevation.8 There is also evidence to suggest that proinflammatory cytokines are found at higher levels in aqueous of eyes with encapsulated blebs and higher IOP.9 Therefore, wound modulation and anti-inflammatory agents may help minimize this HP.
Steroids are potent anti-inflammatory agents that may help treat the HP and improve IOP control after AGV implantation. Intravitreal triamcinolone acetonide (TA) has been used in AGV implantation for patients with neovascular glaucoma and has been shown to lower mean IOP in the first month after surgery. However, TA did not alter intermediate-term success or complications with AGV implantation in this cohort.10 On the other hand, topical steroids were associated with a higher rate of the HP compared with topical nonsteroidal agents in another study.11
Subtenon TA is an established route of administering steroid locally for cases of macular edema and uveitis.12 It may be a more practical route of administration of steroid compared with intravitreal injections in patients with refractory glaucoma. Although complication rates are low with intravitreal injections, there is potential risk of prolonged IOP elevation, endophthalmitis, retinal detachment, and intraocular hemorrhage.13 We hypothesize that subtenon TA injection is a safe and effective adjunct to AGV implantation that may blunt the HP and improve postoperative IOP control.
Methods
The Massachusetts Eye and Ear Human Subjects Committee approved this retrospective study. To test our hypothesis that TA improves the HP after AGV implantation, we retrospectively reviewed consecutive adult cases of AGV implantation by a single surgeon (LRP), and analyzed postoperative data for the first 6 months. A series of consecutive pseudophakic patients with uncontrolled glaucoma necessitating AGV implantation received subtenon TA at the time of surgery from 2009 to 2010. All pseudophakic patients receiving an AGV during the study period received subtenon TA with no specific clinical indications for the TA. A historical comparison group consisted of consecutive pseudophakic patients who had AGV implantation without subtenon TA from 2007 to 2008. Patients who received a pediatric AGV (model FP8) or had any concurrent eye surgery were excluded from the analysis.
In both groups, insertion of the AGV (using the FP7 model in all cases except in three cases where the S2 model was used) was performed in either the superotemporal or inferotemporal quadrant via a fornix-based conjunctival flap. Inferior placement of the AGV was performed in cases where there was an existing superior glaucoma drainage device or if there was conjunctival scarring superiorly that precluded placement in that quadrant. The AGV was routinely primed with balanced salt solution prior to insertion, and dehydrated donor pericardium or irradiated split thickness corneal grafts were used for scleral reinforcement. A total of 0.5 mL of subtenon TA (40 mg/mL) was injected adjacent to the site of the AGV insertion at the completion of the case. Postoperatively, all patients were placed on routine topical broad-spectrum antibiotics and topical steroids (prednisolone acetate 1% four times daily tapered over a 4-week period).
Primary outcomes include IOP and number of glaucoma medications, and secondary outcomes include postoperative complications and visual acuity. IOP measurements and glaucoma medications were collected from all postoperative visits within 6 months of surgery for each patient. The peak IOP for each patient was defined as the highest IOP measurement recorded during this time period. For data not available at a given time point, that patient was censored in the analysis for that time point. We selected our definition of the HP based on definitions used in the literature.5,6 The HP is defined as an IOP measurement of greater than 21 mmHg (with or without medications) during the 6-month postoperative period that was not a result of tube obstruction, retraction, or malfunction. Tube and valve function was determined postoperatively by examining the AGV and, if needed, needling the bleb with a 30-gauge needle to evaluate aqueous egress and subsequent IOP lowering to suggest proper valve function. Given the retrospective nature of this study, the initiation of IOP-lowering medications was not standardized postoperatively, so we opted to use an IOP-based definition that does not account for medication use. We assessed the number of IOP-lowering medications used pre- and postoperatively, as well as timing and number of needlings performed in a separate analysis. For secondary outcomes, events considered as serious early complications include endophthalmitis, hypotony requiring intervention, reoperation, tube erosion, and vision loss to light or no light perception within the 6-month postoperative period. Any patients requiring reoperation for uncontrolled IOP were censored from data analysis after reoperation.
Quantitative data are expressed as mean ± standard deviation, and qualitative data are presented as percentages. To compare the TA and non-TA groups, an unpaired t-test was used for quantitative data and a chi-square test was used for qualitative data. t-tests were two-tailed, and P-values less than 0.05 were considered to be statistically significant.
Results
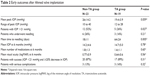
The two groups were similar in all baseline characteristics, and the most common diagnoses in both groups were open angle glaucoma and neovascular glaucoma (Table 1). More patients in the non-TA group developed the HP compared with the TA group (52% versus [vs] 26%, P=0.027) (Table 2). When we included only the patients who received a model FP7 Ahmed valve (N=39) in a secondary analysis, there was still a statistically significant difference between the two groups (52% vs 25%, P=0.020). The mean peak IOP postoperatively was higher in the non-TA group (26±14 mmHg) compared with the TA group (19.4±3.9 mmHg), but this trend did not meet statistical significance (P=0.059) (Table 2). Although this retrospective study was not designed to determine exact timing of the HP phase, the patients in the comparison group appeared to develop the HP earlier than patients in the TA group (mean days to HP were 20 in the non-TA group vs 90 in the TA group, P=0.004). Mean IOP and number of glaucoma medications used were similar in both groups at every time point, except at month 1, when the non-TA group used a higher number of medications compared with the TA group (0.9 vs 0.2 medications, P=0.03) (Table 3). More patients underwent needling in the non-TA group (26%) compared with the TA group (16%), but this did not meet statistical significance. Those who underwent needling in the TA group had it performed later compared with the non-TA group (average of 64 days vs 18 days, P=0.005). This is consistent with the seemingly delayed onset of the HP in the TA group compared with the non-TA group. Rates of success (defined as IOP <21 mmHg and at least a 20% decrease from preoperative IOP) were similar in both groups (87% in the comparison group and 89% in the TA group) at 6 months (Table 2). Mean visual acuity was similar in both groups at month 6 (Table 2).
  | Table 1 Baseline demographic and ocular characteristics |
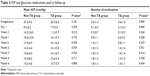  | Table 3 IOP and glaucoma medications used at follow-up |
The rate of serious complications was similar in both groups, but the nature of complications differed between the groups. In the non-TA group, serious complications included reoperation for uncontrolled IOP in two patients and vision loss from light perception to no light perception in one patient. No tube erosions or cases of endophthalmitis were noted in the non-TA group in the 6-month postoperative period.
In the TA group, penetrating keratoplasty for corneal decompensation was performed in one patient postoperatively at month 5. None of the patients in the TA group required reoperation for uncontrolled IOP in the 6-month postoperative period. The second serious complication noted in the TA group was tube erosion at month 2 in a patient with an inferotemporal tube who had no intraoperative complications with conjunctival dissection and closure. This patient was treated with tube explantation and transscleral cyclophotocoagulation. The third serious complication in the TA group was a case of bacterial endophthalmitis associated with an inferotemporal tube. The patient had two prior trabeculectomies with solid superior blebs that were not cystic in morphology. The patient presented with significant intraocular inflammation, but no tube erosion, 6 weeks after surgery and was treated with vitreous biopsy, intravitreal injection of antibiotics, and tube explantation. The infection was confirmed with vitreous cultures that grew out methicillin-sensitive Staphylococcus aureus. The infection resolved, but the patient was noted to have significant scleral thinning in the inferotemporal quadrant where the Ahmed valve was initially implanted.
Discussion
Our study suggests that intraoperative subtenon TA injection with AGV implantation decreases occurrence of the HP. The TA group had lower mean peak IOP overall, though this did not reach statistical significance, probably due to the wide variability in peak IOP in both groups. The lower rate of the HP in the TA group is potentially a result of wound-modulating and anti-inflammatory properties of steroids. Indirect evidence supporting this comes from observations made in the patients who received TA. The patient with the tube erosion in the TA group developed the erosion over the inferior tube early in the postoperative course (2 months). Tube erosions have been noted to occur in up to 8.3% of patients with inferior AGV,14 but the mean time to initial tube erosion has been reported to be 21.5 months.15 The patient with bacterial endophthalmitis in the TA group did not have tube erosion but was noted to have notable scleral thinning at and around the site of the explanted tube shunt. Endophthalmitis is fairly uncommon after glaucoma drainage device implantation (1.7% in superotemporal AGV16 and 2.5% in inferior AGV14). Although the scleral thinning is likely a direct sequela of the infection in this case, any additional adverse effect of the TA in this setting is unclear. These unusual early complications suggest that TA may be exerting a potent local effect on the tissues.
Although the TA group did have more inferiorly placed tubes compared with the control group (42% in TA vs 26% in controls, P=0.10), this did not reach statistical significance. However, it is worth noting that the patients with the early tube erosion and endophthalmitis in the TA group both had the AGV implanted in the inferotemporal quadrant. Though none of the non-TA cases with inferior tubes developed early serious complications, inferior placement of glaucoma drainage devices has been shown to be associated with more complications, in general.14,17,18 Based on our findings, we caution against use of adjunctive subtenon steroids in an inferiorly placed AGV, because of the potentially additive risks.
Although the rate of the HP was lower in the TA group, the mean IOP and number of glaucoma medications used at 6 months were similar in both groups. The 6-month IOP outcomes and success rates we report for both groups are comparable with previously published results on the AGV.2–4 Compared with cohorts in prospective studies comparing AGV with BGI, our cohort had slightly lower mean IOP (14.2 mmHg in the non-TA group and 14.7 mmHg in the TA group compared with 15.7 mmHg and 16.7 mmHg in the Ahmed Baerveldt Comparison Study3 and Ahmed Versus Baerveldt Study4 trials, respectively) on a similar average number of medications at 6 months. Prior studies using antimetabolites and antivascular endothelial growth factor agents as adjuncts to Ahmed valve implantation similarly found no difference in final outcomes with adjunctive treatment.19–22
Although a prospective evaluation of postoperative IOP would be needed to better characterize the timing of the HP, it is interesting that the HP appeared to occur sooner in the non-TA group compared with the TA group. The delayed HP in patients in the TA group may reflect the diminishing effect of the subtenon TA over time. The unchanged IOP and medication outcomes at 6 months between the two groups may reflect the loss of effect of TA over time or inadequate dosing of the medication. Improved drug delivery systems that would potentiate longer-term release of wound-modulating agents may be needed to see a difference in longer-term outcomes. One of the weaknesses of our study is the short follow-up period, which does not allow us to address outcomes beyond 6 months. The primary aim of this study is to describe the safety and early effects of TA on the HP, which, by definition, occurs within the first 6 months of surgery. As our findings do not support the use of subtenon TA at Ahmed valve implantation, longer follow-up is not needed.
Although this is the first published report of the early outcomes of subtenon TA during AGV implantation, this study has other limitations. The retrospective, nonrandomized design of this study makes it prone to bias and unintended differences between the two groups. Although not statistically significant, the higher proportion of inferior AGVs in the TA group suggests that the TA group may have had subjects with more complex ophthalmic disease requiring inferior tube implantation. However, both groups had similar mean preoperative IOP, visual acuity, number of prior ocular surgeries, and preoperative glaucoma medications at baseline (Table 1). The postoperative medication regimen was also not standardized for all the patients. IOP-lowering medications were started at the discretion of the surgeon and not at a preset IOP level. Although the mean number of medications was similar between groups for most time points, the threshold to start these medications may have differed and may be another uncontrolled factor. Evidence showing that intraocular cytokine levels are related to IOP provides a basis for judicious IOP control after glaucoma drainage device implantation.9 If better IOP control in the early postoperative period decreases the risk of the HP, then a lower threshold in starting IOP-lowering medications postoperatively may influence final outcomes.
Another limitation to this study is the method of delivering TA. There was reflux of medication noted in some cases, so a precise dosing of TA was likely not achieved. The ideal dose and mode of delivery have yet to be determined. Microfilms are being developed to carry various types of ocular medications and may be a more standardized method to deliver steroids at the time of surgery.23,24 More study is needed to evaluate the ideal delivery of adjunctive steroids during AGV implantation to prevent encapsulation with its attendant poor hydraulic conductivity of aqueous humor. The use of fibrin glue at the time of AGV implantation may also help minimize intra- and postoperative inflammation, and may be another avenue to explore in preventing the HP.25
Conclusion
In conclusion, we do not advocate the use of intraoperative subtenon TA as an adjunctive measure to prevent the HP phase, especially for inferior AGV implantation. Given the comparable mean IOP between TA and non-TA cases at 6 months, and the development of endophthalmitis in a TA case, other measures to address the HP should be employed. Short-term measures such as bleb needling and the introduction of glaucoma medicines seem to represent a safer approach to address the HP.
Disclosure
Dr Pasquale was supported by a Harvard Medical School Ophthalmology Distinguished Scholar Award and the Harvard Glaucoma Center of Excellence. The authors report no conflicts of interest in this work.
References
Gedde SJ, Schiffman JC, Feuer WJ, Herndon LW, Brandt JD, Budenz DL; for the Tube versus Trabeculectomy Study Group. Treatment outcomes in the tube versus trabeculectomy (TVT) study after five years of follow-up. Am J Ophthalmol. 2012;153(5):789–803. | ||
Huang MC, Netland PA, Coleman AL, Siegner SW, Moster MR, Hill RA. Intermediate-term clinical experience with the Ahmed glaucoma valve implant. Am J Ophthalmol. 1999;127(1):27–33. | ||
Budenz DL, Barton K, Feuer WJ, et al; for the Ahmed Baerveldt Comparison Study Group. Treatment outcomes in the Ahmed Baerveldt comparison study after 1 year of follow-up. Ophthalmology. 2011;118(3): 443–452. | ||
Christakis PG, Kalenak JW, Zurakowski D, et al. The Ahmed Versus Baerveldt Study: one-year treatment outcomes. Ophthalmology. 2011; 118(11):2180–2189. | ||
Ayyala RS, Zurakowski D, Smith JA, et al. A clinical study of the Ahmed glaucoma valve implant in advanced glaucoma. Ophthalmology. 1998; 105(10):1968–1976. | ||
Nouri-Mahdavi K, Caprioli J. Evaluation of the hypertensive phase after insertion of the Ahmed glaucoma valve. Am J Ophthalmol. 2003;136(6): 1001–1008. | ||
Thieme H, Choritz L, Hofmann-Rummelt C, Schloetzer-Schrehardt U, Kottler UB. Histopathologic findings in early encapsulated blebs of young patients treated with the Ahmed glaucoma valve. J Glaucoma. 2011;20(4):246–251. | ||
Gedde SJ, Panarelli JF, Banitt MR, Lee RK. Evidence-based comparison of aqueous shunts. Curr Opin Ophthalmol. 2013;24(2):87–95. | ||
Freedman J, Iserovich P. Pro-inflammatory cytokines in glaucomatous aqueous and encysted Molteno implant blebs and their relationship to pressure. Invest Ophthalmol Vis Sci. 2013;54(7):4851–4855. | ||
Teixeira SH, Doi LM, Freitas Silva AL, et al. Silicone Ahmed glaucoma valve with and without intravitreal triamcinolone acetonide for neovascular glaucoma: randomized clinical trial. J Glaucoma. 2012;21(5): 342–348. | ||
Yuen D, Buys Y, Jin YP, Alasbali T, Smith M, Trope GE. Corticosteroids versus NSAIDs on intraocular pressure and the hypertensive phase after Ahmed glaucoma valve surgery. J Glaucoma. 2001;20(7):439–444. | ||
Byun YS, Park YH. Complications and safety profile of posterior subtenon injection of triamcinolone acetonide. J Ocul Pharm Ther. 2009; 25(2):159–162. | ||
Jager RD, Aiello LP, Patel SC, Cunningham ET Jr. Risks of intravitreous injection: a comprehensive review. Retina. 2004;24(5):676–698. | ||
Pakravan M, Yazdani S, Shahabi C, Yaseri M. Superior versus inferior Ahmed glaucoma valve implantation. Ophthalmology. 2009;116(2): 208–213. | ||
Huddleston SM, Feldman RM, Budenz DL, et al. Aqueous shunt exposure: a retrospective review of repair outcome. J Glaucoma. 2013;22(6): 433–438. | ||
Al-Torbak AA, Al-Shahwan S, Al-Jadaan I, et al. Endophthalmitis associated with the Ahmed glaucoma valve implant. Br J Ophthalmol. 2005;89(4):454–458. | ||
Rachmiel R, Trope GE, Buys YM, Flanagan JG, Chipman ML. Intermediate-term outcome and success of superior versus inferior Ahmed Glaucoma Valve implantation. J Glaucoma. 2008;17(7):584–590. | ||
Geffen N, Buys YM, Smith M, et al. Conjunctival complications related to Ahmed glaucoma valve insertion. J Glaucoma. 2014;23(2): 109–114. | ||
Costa VP, Azuara-Blanco A, Netland PA, Lesk MR, Arcieri ES. Efficacy and safety of adjunctive mitomycin C during Ahmed glaucoma valve implantation. Ophthalmology. 2004;111(6):1071–1076. | ||
Alvarado JA, Hollander DA, Juster RP, Lee LC. Ahmed valve implantation with adjunctive mitomycin C and 5-fluorouracil: long-term outcomes. Am J Ophthalmol. 2008;146(2):276–284. | ||
Ma KT, Yang JY, Kim JH, et al. Surgical results of Ahmed valve implantation with intraoperative bevacizumab injection in patients with neovascular glaucoma. J Glaucoma. 2012;21(5):331–336. | ||
Desai RU, Singh K, Lin SC. Intravitreal ranibizumab as an adjunct for Ahmed valve surgery in open-angle glaucoma: a pilot study. Clin Experiment Ophthalmol. 2013;41(2):155–158. | ||
Ang M, Yan P, Zhen M, Foo S, Venkatraman S, Wong T. Evaluation of sustained release of PLC-loaded prednisolone acetate microfilm on postoperative inflammation in an experimental model of glaucoma filtration surgery. Curr Eye Res. 2011;36(12):1123–1128. | ||
Ponnusamy T, Yu H, John VT, Ayyala RS, Blake DA. A novel antiproliferative drug coating for glaucoma drainage devices. J Glaucoma. Epub 2013 Apr 29. | ||
Quaranta L, Riva I, Floriani IC. Outcomes of using a sutureless bovine pericardial patch graft for Ahmed glaucoma valve implantation. Eur J Ophthalmol. 2013;23(5):738–742. |
 © 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.