Back to Journals » Diabetes, Metabolic Syndrome and Obesity » Volume 16
Hyperinsulinemia Impaired Coronary Collateral Circulation in Patients with Chronic Total Coronary Occlusion
Authors Zou X , Chen M, Sun L, Tan Q
Received 27 January 2023
Accepted for publication 16 April 2023
Published 18 May 2023 Volume 2023:16 Pages 1425—1433
DOI https://doi.org/10.2147/DMSO.S402849
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Juei-Tang Cheng
Xiaoyi Zou, Ming Chen, Limin Sun, Qiang Tan
Department of Cardiology, Qinhuangdao First Hospital, Hebei Medical University, Qinhuangdao, Hebei Province, People’s Republic of China
Correspondence: Qiang Tan, Department of Cardiology, Qinhuangdao First Hospital, Hebei Medical University, No. 258 of Wenhua Road, Qinhuangdao, Hebei Province, 066000, People’s Republic of China, Email [email protected]
Background and Objectives: Hyperinsulinemia impaired cardiovascular system and endothelial function in the population. The purpose of this study was to explore the relationship between hyperinsulinemia and coronary collateral circulation in patients with chronic total coronary occlusion.
Methods: Patients with stable angina and at least one total coronary occlusion were enrolled in this study. Collateral grade was determined according to Rentrop’s classification. Patients were divided into a good coronary collateral circulation (CCC) group (grade 2 or 3 collateral vessels, n = 223) and a poor CCC group (grade 0 or 1 collateral vessels, n = 115). Fasting insulin level (FINS) and fasting glucose level (FBS) were measured. Endothelial function evaluated by flow-mediated dilation (FMD).
Results: Serum FINS level was significantly increased in the poor CCC group (P < 0.01). Patients in the poor CCC group had higher levels of FBS, HbA1C, and homeostasis model assessment for insulin resistance (HOMA-IR) than patients in the good CCC group. The poor CCC group also had lower levels of FMD, lower LVEF and higher syntax scores than the good CCC group. Hyperinsulinemia (T3, FINS ≥ 15.22 μIU/mL) increased OR for the incidence of the poor CCC group (OR 2.419, 95% CI 1.780– 3.287) in multivariate analysis. Multivariate logistic regression also revealed that diabetes, HbA1c, HOMA-IR, HDL-C and Syntax score were independent predictors of poor CCC (all P < 0.05).
Conclusion: Hyperinsulinemia is a valuable predictor of poor collateral formation in patients with chronic total coronary occlusion.
Keywords: coronary collateral, hyperinsulinemia, arteriogenesis, endothelial function
A Letter to the Editor has been published for this article.
Introduction
Chronic total coronary occlusion (CTO) refers to a coronary artery occlusion with complete cessation of antegrade blood flow for more than 3 months.1 The presence of CTO could induce myocardial ischemia and increase risk of cardiac mortality.2 Coronary collaterals are collateral anastomosis between major coronary arteries. These collaterals exist in a normal heart from embryogenesis.3 When a major coronary artery is obstructed, the collaterals will open and develop by the mechanism of arteriogenesis.4 Well-developed coronary collateral circulation is a self adaptation mechanism and it can preserve cardiac function, rescue ischemic myocardium and reduce the risk of death in patients with CTO.5
Stimulation of coronary collateral circulation is a potential therapy for patients with severe coronary artery disease who could not receive revascularization. However, many factors restrain collateral development, such as diabetes and metabolic syndrome which are prevalent worldwide.6 Insulin resistance and accompanied hyperinsulinemia are common in these patients.7 Previous researches have indicated that hyperinsulinemia is an independent etiological factor in many diseases, for instance, hypertension, atherosclerosis and diabetes.8,9 Our previous studies also demonstrated that hyperinsulinemia impaired the angiogenesis ability of endothelial progenitor cells and increased adverse cardiovascular events in patients with performed percutaneous coronary intervention (PCI).9,10 However, the association between hyperinsulinemia and collateral development has not been explored.
The aim of this current study is to investigate the association of hyperinsulinemia and collateral circulation in patients with CTO.
Methods
Study Population
This was a prospective observational study. Between May 2018 and September 2022, patients scheduled for coronary angiography in Qinhuangdao first hospital were recruited. The following were Inclusion criteria: 1) patients at least 18 years old who had coronary artery disease; 2) patients who had at least one total occlusion of a major coronary vessel; 3) the history of coronary occlusion was no less than 3 months. The exclusion criteria of the study: 1) patients with a history of a coronary artery bypass graft; 2) patients with acute myocardial infarction; 3) patients who had taken insulin sensitizer or injected insulin in last three months.
This study complies with the Declaration of Helsinki. Qinhuangdao First Hospital ethics committee has approved this study, and written informed consents were obtained from the enrolled patients.
Clinical Data Collection
Clinical data, such as family history, smoking history, diabetes, hypertension, CCS (Canadian Cardiovascular Society) angina class and medicine history were obtained. CCS class of angina was obtained in all subjects. Overnight fast blood samples were collected. Total cholesterol, triglyceride, low-density lipoprotein cholesterol, high-density lipoprotein, creatinine, homocysteine and fast blood sugar (FBS) were measured. Immunoassay methods (Elecsys1010, Roche) was used to determine fasting insulin (FINS). Insulin resistance was assessed by homeostasis model assessment for insulin resistance (HOMA-IR). The formula is as follows: HOMA-IR (mmol/L×µU/mL) = fasting glucose (mmol/L)×fasting insulin (µU/mL)/22.5.10
Angiography Procedure and Coronary Collaterals Grading
Enrolled patients underwent coronary angiography and the angiographic images were assayed by two interventional cardiologists who did not know other data about the patients. SYNTAX score was obtained based on the findings of the coronary angiography. Coronary collateral circulation (CCC) was evaluated by the Rentrop classification method. 11 The criterias of this method are as follows: grade 0, no filling of contrast; grade one, filling of side branches of collateral with no epicardial perfusion; grade two, partial filling of epicardial artery by collateral; grade three, fully filling of epicardial artery.11 Good coronary collateral circulation (CCC) was delineated as grade two or grade three collateral, poor CCC was delineated as grade 0 or grade one collateral.
Assessment of FMD
An ultrasound system (VIVID 8, GE) was used to assess flow-mediated dilation (FMD). The protocol of FMD measurement followed the methods we established before.12 The value of FMD was expressed as the formula ([{maximum diameter − baseline diameter}/baseline diameter] × 100).12
Statistics Analysis
All data were analyzed by SPSS19. Continuous variables with normal distribution were described as mean ± standard deviation. Non-normal distribution data were described as median and interquartile range. Categorical variables were described by numbers and percentages. One-way ANOVA or the Kruskal–Wallis H-test were used in comparison of the continuous variables. Chi-square test was used in categorical variables.
Multiple logistic regression was performed to estimate the odds ratio (OR) and their 95% confidence intervals (CI) of poor CCC. A probability value <0.05 was considered statistically significant.
Results
Clinical Characteristics of Poor and Good CCC Groups
734 patients had at least one CTO lesion in the 10,328 cases who underwent coronary angiography between May 2018 and September 2022. 521 patients meet the inclusion and exclusion criteria. DATA of FINS were not available in 186 patients. Finally, 335 patients were enrolled in this study (Figure 1) and allocated into the good CCC group or the poor CCC group by Rentrop classification (good.CCC group, Rentrop classification grade two or grade three; poor CCC group, Rentrop classification grade 0 or grade one). The results in Table 1 indicated that both groups had no differences of age, gender, family history, hypertension, prior MI and the use of major medicines. But the poor CCC group had a higher rate of smoking and diabetes. The levels of total cholesterol, triglyceride, low-density lipoprotein cholesterol had no statistical differences in both groups. However, patients in the poor CCC group had higher levels of FBS, FINS, HbA1C, HOMA-IR and lower levels of high-density lipoprotein cholesterol than patients in the good CCC group (P < 0.05). Patients of the poor CCC group also had lower LVEF and higher syntax scores than patients of the good CCC group. Values of FMD were lower in the poor CCC group (5.07 ±4.63%) compared with the good CCC group (7.37 ±5.43%) (P < 0.05). Patients in the poor CCC group also had higher levels of CCS angina class than patients of the good CCC group.
 |
Table 1 Clinical and Angiographic Characteristics of Poor and Good CCC Groups. |
 |
Figure 1 Study flowchart (figure title) Flowchart of enrolled patients. |
FINS Level and Coronary Collateral Circulation
The subjects were allocated into T1, T2, or T3 groups by tertiles of FINS level (T1, low-insulin group: FINS < 7.91 μIU/mL; T2, medium-insulin group: 7.91 μIU/mL ≤ FINS < 15.22 μIU/mL; T3, high-insulin group: FINS ≥ 15.22 μIU/mL). The results in Table 2 show that the clinical characteristics had no statistical differences among the three groups. Triglyceride, HOMA-IR, and BMI were higher in the high insulin group than the other groups. Patients in the high insulin group had lower Rentrop grades of collateral circulation and lower levels of FMD than patients in other groups (Figure 2).
 |
Table 2 Comparison of Clinical and Angiographic Characteristics According to FINS Status |
Predictors of Coronary Collateral Circulation
Table 3 shows the results of multivariate logistic regression for the association between the incidence of poor CCC and tertiles of FINS. Being a category variable, hyperinsulinemia (T3, FINS ≥15.22 μIU/mL) raised OR for the incidence of poor CCC (OR 2.419, 95% CI 1.780–3.287) in multivariate analysis.
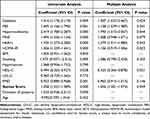 |
Table 3 Logistic Regression |
In univariate analysis, the FINS level was associated with poor CCC (95% CI 1.056–1.134, P < 0.05). However, in multivariate analysis, the association between FINS level and poor CCC had no statistical significance (OR 1.008, 95% CI 0.948–1.071, P = 0.079).
Multivariate regression also revealed that diabetes (OR 1.407, 95% CI 1.033–2.667), HbA1c (OR 1.379, 95% CI 1.011–1.880), HOMA-IR (OR 1.136, 95% CI 0.919–1.406), HDL-C (OR 0.425, 95% CI 0.206–0.878) and SYNTAX score (OR 1.036, 95% CI 1.001–1.073) were independent factors of poor CCC (all P < 0.05).
Discussion
The main finding of this study is that a higher fasting insulin concentration was associated with poor coronary collateral circulation. Hyperinsulinemia impaired endothelial function and collateral development in patients with chronic total coronary occlusion.
Coronary collateral circulation is a channel of artery to artery connection in the heart. Because of their tiny caliber, collateral arteries could not offer enough blood flow in their native state.13,However, well-developed collateral circulation protected ischemic myocardium and reduced cardiovascular death in severe stenosis of the coronary artery. Previous studies have demonstrated that metabolic diseases, such as diabetes and metabolic syndrome restrained collateral formation in patients with coronary heart disease.11,14 In an observational study which included 1653 patients with CTO, Liu et al found that MetS was inversely correlated with coronary collateral growth.1 A meta-analysis which included 18 studies and 4746 enrolled patients, revealed that diabetes inhibited formation of coronary collaterals (OR = 0.50, 95% CI: 0.38–0.67, p = 0.00001).13
A normal level of insulin plays a protective role in the cardiovascular system. However, hyperinsulinemia can cause a variety of diseases.15,16 The traditional view believed that hyperinsulinemia was secondary to insulin resistance. Recently, a new concept suggested that hyperinsulinemia is primary and causes insulin resistance.15 Until now, there was no research to explore the influence of hyperinsulinemia on coronary collateral circulation. In the current study, we, for the first time, found that hyperinsulinemia impaired collateral development in patients with CTO. It is recognized that angiogenesis and arteriogenesis are both involved in collateral development. Angiogenesis refers to the formation of capillaries from existing vessels to expand the microvascular system.13 However, angiogenesis could not provide enough blood flow to the ischemic area. Arteriogenesis is an adaptive remodeling of existing collateral arteries. Unlike angiogenesis, arteriogenesis results in an increased flow capacity of the artery.17 The mechanism of collateral development is complex. Several cytokines and factors involved in this process include vascular endothelial growth factor, nitric oxide, shear forces, inflammation and endothelial progenitor cells (EPCs).18–20 EPCs play a vital role in angiogenesis and collateral formation. Flores-Umanzor et al found that patients with Rentrop grade 3 collateral circulation exhibited higher EPC activity at baseline and at 1-year follow-up compared with those who had poor collateral circulation.21 In a previous cell-culture based study, we found that hyperinsulinemia decreased proliferation and tube formation abilities of EPCs by disturbing the balance of the PI3K/ AKT/eNOS pathway and p38 MAPK pathway.8 The results of this study indicate that hyperinsulinemia impaired endothelial function is evaluated by FMD. Mackesy et al’s study demonstrated that hyperinsulinemia induced oxidative stress and inflammation in macrophages and endothelial cells.22 Mahmoud et al found that hyperinsulinemia increased endothelin-1 protein expression and impaired vasodilation of human skeletal muscle arterioles.23 The mechanism underlying the association of hyperinsulinemia and poor collateral circulation has not been elucidated, But the above investigation proposes that endothelial dysfunction, inflammation and cytokine secretion may take part in it.
Limitations
There were some limitations in the study. First, the number of enrolled patients was relatively small. Second, we did not explore whether decreasing insulin level could restore collateral flow. We still need further investigations to testify this hypothesis.
Conclusions
The results of this study demonstrated that hyperinsulinemia is associated with poorly developed collateral circulation in patients with CTO. Hyperinsulinemia might impair endothelial function and collateral formation in patients with severe coronary artery disease. The findings of this study indicate that reducing hyperinsulinemia can be a candidate of therapeutic target for patients with ischemic cardiovascular diseases.
Abbreviation
MI, myocardial infarction; TC, cholesterol; TG, triglyceride; LDL-C, low density lipoprotein-cholesterol; HCY, homocysteine; HDL-C, high-density lipoprotein cholesterol; FBS, fasting blood sugar; FINS, fasting insulin; BMI, body mass index; HOMA-IR, homeostasis model assessment for insulin resistance; LVEF, left ventricular ejection fraction; LVD, left ventricular diameter; LA, left atrial diameter; CCS, Canadian Cardiovascular Society; FMD, flow-mediated dilation; CI, confidence interval.
Ethics Approval
Ethics committee approved this work and patients provided their written informed consent.
Funding
This study was funded by S&T program of Hebei (20377756D), Hebei Chinese medical technology project (2020377) and Hebei medical technology project (20231833).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Liu T, Wu Z, Liu J, Lv Y, Li W. Metabolic syndrome and its components reduce coronary collateralization in chronic total occlusion: an observational study. Cardiovasc Diabetol. 2021;20(1):104. doi:10.1186/s12933-021-01297-4
2. van Veelen A, Claessen BEPM, Houterman S, et al. PCI Registration Committee of the Netherlands Heart Registration. Incidence and outcomes of chronic total occlusion percutaneous coronary intervention in the Netherlands: data from a nationwide registry. Neth Heart J. 2021;29(1):4–13. doi:10.1007/s12471-020-01521-y
3. Wu WT, Lin TH, Hsu PC, Lai WT, Sheu SH. Prediction for coronary collateral development. Acta Cardiol Sin. 2022;38(1):27–28. doi:10.6515/ACS.202201_38(1).20211208A
4. Das S, Goldstone AB, Wang H, et al. A unique collateral artery development program promotes neonatal heart regeneration. Cell. 2019;176(5):1128–1142. doi:10.1016/j.cell.2018.12.023
5. Jamaiyar A, Juguilon C, Dong F, et al. Cardioprotection during ischemia by coronary collateral growth. Am J Physiol Heart Circ Physiol. 2019;316(1):H1–H9. doi:10.1152/ajpheart.00145.2018
6. Xun P, Wu Y, He Q, He K. Fasting insulin concentrations and incidence of hypertension, stroke, and coronary heart disease: a meta-analysis of prospective cohort studies. Am J Clin Nutr. 2013;98(6):1543–1554. doi:10.3945/ajcn.113.065565
7. Yaghootkar H, Scott RA, White CC, et al. Genetic evidence for a normal-weight “metabolically obese” phenotype linking insulin resistance, hypertension, coronary artery disease, and type 2 diabetes. Diabetes. 2014;63:4369–4377. doi:10.2337/db14-0318
8. Tan Q, Li Y, Li X, Zhang S. Hyperinsulinemia impairs functions of circulating endothelial progenitor cells. Acta Diabetol. 2019;56(7):785–795. doi:10.1007/s00592-019-01314-9
9. Tan Q, Chen M, Hao J, Wei K. Impact of hyperinsulinemia on long-term clinical outcomes of percutaneous coronary intervention in patients without diabetes who have acute myocardial syndrome. Diabetes Metab Syndr Obes. 2021;7(14):3949–3957. doi:10.2147/DMSO.S318852
10. Tan Q, Zhang S, Li Y. Circulating endothelial progenitor cells were decreased in patients with metabolic syndrome. Clin Lab. 2018;64(10):1679–1683. doi:10.7754/Clin.Lab.2018.180427
11. Reto BM, Seiler C. The Human Coronary Collateral Circulation, Its Extracardiac Anastomoses and Their Therapeutic Promotion. Int J Mol Sci. 2019;20(15):3726. doi:10.3390/ijms20153726.
12. Li Y, Tan Q, Guo Y, et al. The influence of exercise training on endothelial function, serum irisin and inflammatory markers in the elderly with metabolic syndrome. Clin Lab. 2021;67(3). doi:10.7754/Clin.Lab.2020.200446
13. Pei J, Wang X, Xing Z. Traditional cardiovascular risk factors and coronary collateral circulation: a meta-analysis. Front Cardiovasc Med. 2021;8:743234. doi:10.3389/fcvm.2021.743234
14. Janssen JA. Hyperinsulinemia and its pivotal role in aging, obesity, type 2 diabetes, cardiovascular disease and cancer. Int J Mol Sci. 2021;22(15):7797. doi:10.3390/ijms22157797
15. Sbraccia P, D’Adamo M, Guglielmi V. Is type 2 diabetes an adiposity-based metabolic disease? From the origin of insulin resistance to the concept of dysfunctional adipose tissue. Eat Weight Disord. 2021;26:2429–2441. doi:10.1007/s40519-021-01109-4
16. Sabra M, Karbasiafshar C, Aboulgheit A, Raj S, Abid MR, Sellke FW. Clinical application of novel therapies for coronary angiogenesis: overview, challenges, and prospects. Int J Mol Sci. 2021;22(7):3722. doi:10.3390/ijms22073722
17. Melincovici CS, Boşca AB, Şuşman S, et al. Vascular endothelial growth factor (VEGF) - key factor in normal and pathological angiogenesis. Rom J Morphol Embryol. 2018;59(2):455–467.
18. Chen Z, Haus JM, Chen L, et al. CCL28-induced CCR10/eNOS interaction in angiogenesis and skin wound healing. FASEB J. 2020;34(4):5838–5850. doi:10.1096/fj.201902060R
19. Adali MK, Buber I, Sen G, Yilmaz S. Relationship between systemic immune-inflammation index and coronary collateral circulation in patients with chronic total occlusion. Arq Bras Cardiol. 2022;119(1):69–75. doi:10.36660/abc.20210414
20. Mackesy DZ, Goalstone ML. Insulin augments tumor necrosis factor-alpha stimulated expression of vascular cell adhesion molecule-1 in vascular endothelial cells. J Inflamm. 2011;8:34–38. doi:10.1186/1476-9255-8-34
21. Flores-Umanzor EJ, Ortega-Paz L, Cepas-Guillen PL, et al. Endothelial progenitor cell function in patients with coronary chronic total occlusion and its relationship with collateral circulation. J Invasive Cardiol. 2021;33(10):E809–E816.
22. Mackesy DZ, Goalstone ML. Extracellular signal-regulated kinase-5: novel mediator of insulin and tumor necrosis factor α-stimulated vascular cell adhesion molecule-1 expression in vascular cells. J Diabetes. 2014;6(6):595–602. doi:10.1111/1753-0407.12132
23. Mahmoud AM, Szczurek MR, Blackburn BK, et al. Hyperinsulinemia augments endothelin-1 protein expression and impairs vasodilation of human skeletal muscle arterioles. Physiol Rep. 2016;4(16):e12895. doi:10.14814/phy2.12895
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

