Back to Journals » Diabetes, Metabolic Syndrome and Obesity » Volume 14
Hyperglycemic Crisis Characteristics and Outcome of Care in Adult Patients without and with a History of Diabetes in Tigrai, Ethiopia: Comparative Study
Authors Gebremedhin G , Enqueselassie F, Yifter H, Deyessa N
Received 10 August 2020
Accepted for publication 14 October 2020
Published 9 February 2021 Volume 2021:14 Pages 547—556
DOI https://doi.org/10.2147/DMSO.S275552
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Juei-Tang Cheng
Getachew Gebremedhin,1 Fikre Enqueselassie1 †, Helen Yifter,2 Negussie Deyessa1
1Department of Community Health and Preventive Medicines, Addis Ababa University, Addis Ababa, Ethiopia; 2Department of Endocrinology, School of Medicine, Addis Ababa University, Addis Ababa, Ethiopia
†Professor Fikre Enqueselassie passed away on October 28th, 2019.
Correspondence: Getachew Gebremedhin Email [email protected]
Objective: To compare hyperglycemic crisis characteristics and outcomes of care in adult patients without and with a history of diabetes in Tigrai, Ethiopia.
Methods: A retrospective record review of diabetes patients, 196 without and 393 with a history of diabetes who had been treated in the medical wards from September 1/2017 to August 31/2018, aged 18 years and above was included. An independent-samples t-test/Mann–Whitney tests, χ2-test, and logistic regression analysis were used to analyze the data using SPSS version 25.0.
Results: Patients without history of diabetes were younger [43.9± 12.6 vs 48.4± 14.9], more rural residents [53.1% vs 30.3%], lower proportion of type 2 diabetes [38.3% vs 53.7%], hyperosmolar hyperglycemic state [15.8% vs 31.8%], with lower mortality rate [8.7% vs 15.5%] compared to with a history of diabetes. A higher mortality reported in rural residents [13.5% vs 3.3%; without vs 21.8% vs 12.8%; with history], and lower urine ketones [1.9± 1.3 vs 2.8± 1.1; without vs 1.6± 1.2 vs 2.2± 1.0; with a history] compared to their counterparts in both patients, respectively. Rural residents [AOR (95% CI); 3.1 (1.8, 5.4)]; medical history of stroke [AOR (95% CI); 2.7 (1.3, 5.6)]; type 2 diabetes [AOR (95% CI); 2.3 (1.1, 4.7)], hyperglycemic hyperosmolar state [AOR (95% CI); 2.4 (1.1, 5.4)]; and with a history of diabetes [AOR (95% CI); 2.0 (1.04, 3.8)] were significantly associated with mortality, but polydipsia [AOR (95% CI); 0.47 (0.27, 0.81)] was preventive.
Conclusion: This finding suggests that rural residents, medical history of stroke, type 2 diabetes, hyperglycemic hyperosmolar state, and with a history of diabetes were independent predictors of mortality while polydipsia was preventive. Therefore, the need for more public health awareness campaigns, screening for people having known risk factors, and expansion of diabetes care services to the primary health care units is a fundamental measure.
Keywords: hyperglycemic crisis, mortality, new-onset, with history, outcome
Plain Language Summary
This study aims to compare hyperglycemic crisis characteristics and outcomes of care in adult patients without and with a history of diabetes in Tigrai, Ethiopia. A retrospective medical chart review of all adult patients aged 18 years and above with a hyperglycemic crisis of 196 without and 393 with a history of diabetes admitted in a medical ward from September 1/2017 to August 31/2018; are included in the study. Patients without a history of diabetes are younger with a mean age of (44 vs 49 years), more rural residents (53.1% vs 30.3%), lower the proportion of type 2 diabetes (38.3% vs 53.7%) and hyperosmolar hyperglycemic state (15.8% vs 31.2%) compared to with a history of diabetes. Mortality is higher in patients with a history of diabetes [15.5% vs 8.7%], rural residents [13.5% vs 3.3%; without, and 21.8% vs 12.8%; with], and with lower urine ketones [1.9± 1.3 vs 2.8± 1.1; without and 1.6± 1.2 vs 2.2± 1.0; with] compared to their counterparts. A 30 days cases of mortality is 3.0, 2.7, 2.3, 2.4, and 2.0 times higher in rural residents, who had a stroke, type 2 diabetes, hyperglycemic hyperosmolar state, and with a history of diabetes, respectively; but reduced by 47% in patients with excessive thirst. In general, rural residents, a history of stroke, type 2 diabetes, hyperglycemic hyperosmolar state, and with a history of diabetes are risk factors for mortality while excessive thirst is preventive. Therefore, the need for more public health awareness campaigns, screening for people having known risk factors, and expansion of services to health centers is a fundamental measure.
Introduction
The hyperglycemic crisis is the most common life-threatening acute metabolic-complication, which results in significant morbidity and mortality.1–3 Diabetic ketoacidosis (DKA), and hyperosmolar hyperglycemic state (HHS), are the two most common hyperglycemic crises, where patients requiring intensive treatment and hospitalization.3–5 Both DKA and HHS are extreme metabolic derangements associated with uncontrolled types 1 and 2 diabetes mellitus. DKA is more common in young people with type 1 diabetes (T1D) and HHS is more frequently reported in adult and elderly patients with type 2 diabetes (T2D); however, each type of diabetes may be associated with DKA or HHS. Hyperglycemic crises are a continuum of metabolic derangements that differ in the rapidity of onset, clinical features, the severity of dehydration, and the degree of ketosis.2,3,6–8
The hyperglycemic crisis is becoming a major challenge in the healthcare system; which is usually associated with disability, reduced life expectancy, and has a high cost of treatment.2,7 The annual incidence of the hyperglycemic crisis is estimated to be 9.5 per 1000 persons with diabetes, and there were 207,000 hospitalizations for the hyperglycemic crisis reported in the United States of America (USA) in 2014.9 In the USA, about 43% of the total medical cost for diabetes is spent on hospital inpatient care.10
8A study in Taiwan reported that about one-fourth of hyperglycemic crisis admission was patients without a history of diabetes. Patients without a history of diabetes were younger and less elderly, had better consciousness and renal function, more significant diabetic signs and symptoms, higher blood sugar, a higher proportion of DKA and less proportion of HHS, less opportunity of infection, medical history, and a 30 days cases of mortality.11
In Africa, the hyperglycemic crisis was the main reason for hospital admission of patients with diabetes ranging from about 26% in South Africa to 40% in Nigeria with mortality rates ranging, from 7.5% in South Africa to 34% in Nigeria.12–14 Admissions for HHS, in contrast to DKA, were more common in patients with a new diagnosis of diabetes in South Africa and Ethiopia.2,15 Studies in Ethiopia, 23.6–43% of patients with the hyperglycemic crisis were with new onset of diabetes at admission with a 30 days cases of mortality 4.1%; but 14.6% with a history of diabetes.2,16,17
Although the hyperglycemic crisis is a major challenge in the healthcare system in developing nations, including Ethiopia; but robust data on the hyperglycemic crisis characteristics and outcome of care in patients without and with a history of diabetes is lacking, which will have a crucial input in shifting healthcare priorities and management protocol.
Methods
Study Design, Population and Data Collection
The study conducted in randomly selected six general and one referral hospitals of Tigrai in northern Ethiopia among adult patients aged 18 years and above, who admitted and treated for a hyperglycemic crisis in the medical wards from September 1, 2017, to August 31, 2018. Data extracted from January to March 2019. This study was a hospital-based retrospective record review and all one-year medical records of adult patients aged 18 years and above who had been admitted and treated were included in the review if they met the inclusion criteria. But, adult patients who left against medical advice, referred to other health institutions, and pregnant mothers were excluded from the study.
The sample size calculated using a double population proportion formula with the assumption of 4.1% and 14.6% mortality rates in patients without and with a history of diabetes, respectively,2 a power of 90% and confidence interval of 95% and a ratio of patients with history diabetes to without a history of diabetes is 2. Then, the required sample size was 137 patients without a history of diabetes and 274 patients with a history of diabetes. But, finally, all medical records of patients (196 without and 393 with a history of diabetes) with hyperglycemic crisis who were admitted and treated between September 1, 2017, to August 31, 2018, in the six general hospitals and Ayder Comprehensive specialized hospital were included.
Data were abstracted using a uniform data abstraction format prepared to gather relevant data from the medical records both from paper copy file and e file/smart care/. The data were abstracted from 196 patients without a history of diabetes and 393 patients with a history of diabetes with DKA and HHS. By Nurse and public health experts recruited for data abstraction. Data collectors and supervisors trained for one day on how to retrieve, and abstract relevant data from the medical records. The data abstraction format was pretested in 60 adult medical records two weeks before the actual data abstraction period.
Operational Definitions
Type 1 diabetes: When the patient presented with FBS ≥ 126 mg/dl or RBS ≥ 200 mg/dl plus classic symptoms excessive urination, excessive thirst, and unexplained weight loss.
Type 2 diabetes: When the patient presented with FBS ≥ 126 mg/dl or RBS ≥ 200 mg/dl plus other symptoms such as excess body weight, physical inactivity, unhealthy diet, and family history of diabetes.18,19
Diabetic Ketoacidosis (DKA): DKA was defined as admission blood glucose >250 mg/l and urine dipstick ketone level ≥ +2.2
Hyperosmolar Hyperglycemic State (HHS): HHS was defined as blood glucose >600 mg/dL, alteration in mental status, and mild or absent ketonuria.2
Level of consciousness: Based on the Glasgow Coma Scale (GSC); the level of consciousness is classified as better consciousness (mild) when GSC ≥ 13; Moderate level of consciousness when GSC is 9 to 12; Severe altered level of consciousness when the GSC ≤ 8.
Without a history of diabetes: Patients who denied and had no medical record of diabetes and diagnosed for the first time with fasting blood sugar (FBS) ≥ 126 mg/dl, or repeated random blood sugar (RBS) ≥ 200 mg/dl plus fatigue, polyuria, polydipsia, and other symptoms.11
Definition of End-Point: We used 30-day mortality as the primary end-point. People who survived at least 30 days whether or not they were still hospitalized were considered ‘survivors’ for this analysis. We used 30-day mortality as the primary end-point because the hospital stay of 98.8% of patients was within 30 days in the present study. Also, 30 days is a universally acceptable endpoint for outcome studies.11
Data Analysis
Data entered and analyzed using SPSS version 25.0 for Windows. Continuous data presented as the median and interquartile range (IQR) [25th; 75th percentiles] and means ± Standard Deviation (SD). Comparisons between two groups made using either an independent-samples t-test (assuming a normal distribution) or Mann–Whitney/Wilcoxon tests (assuming non-normality) of the continuous variables.
The nominal variables presented as absolute frequencies and proportions, and the χ2-test or a Fisher’s exact test was used for categorical variables. The association between the exposure and outcome variables was determined using a logistic regression model with 95% confidence intervals (CI). Significance was set at p < 0.05 (two-tailed) to extract variables effective in a model.
Ethical Statement
The ethical statement protocol was approved by the Institution Review Board (IRB) of Addis Ababa University-College of Health Sciences (AAU-CHS), following the Helsinki Declaration, and a waiver letter was obtained. Besides, written permission was obtained from the health bureau of the Tigrai Regional State after submitting the protocol and explaining the purpose of the study. For the sake of privacy and confidentiality, all charts used in this research were kept private and confidential; where data were password protected and filled checklists were kept locked in a cabinet. No information other than for this study purpose was collected from the patient charts, including personal identifiers.
Results
Of the 1082 hyperglycemic crisis-related admissions, only 589 (54.4%) of them met the inclusion criteria for DKA or HHS. Out of those patients with a hyperglycemic crisis, 196 (33.3%) patients without a history of diabetes, and 393 (66.7%) patients with a history of diabetes were included in the study (Figure 1).
 |
Figure 1 Flow diagram of analyzed events and comparing clinical characteristics of patients without and with a history of diabetes. |
The distribution of socio-demographic and clinical characteristics differs between those patients without and with a history of diabetes. Those patients without a history of diabetes were comparatively younger than those with a history of diabetes with a mean (±SD) age of [43.9±12.6 vs 48.4±14.8 years; p<0.001], and also they were less elderly [3.6% vs 15.8%; p< 0.001]. Similarly, patients without a history of diabetes were more rural residents [53.1% vs 30.3%; p<0.001] compared to patients with a history of diabetes. Regarding to the clinical characteristics of hyperglycemic crisis, patients without a history of diabetes had relatively higher proportion of classic signs and symptoms of diabetes [vomiting (69.4% vs 36.4%; p<0.001), polyuria (75.5% vs 59.0%; p<0.001), polydipsia (83.7% vs 74.8%; p=0.015), fruit breath odor (84.2% vs 72.3%; p=0.001), and weight loss (79.6% vs 64.1%; p<0.001)]. Whilst, patients with a history of diabetes had a comparatively higher proportion of medical history of Chronic Kidney Disease (10.7% vs 1.5%; p<0.001), Cardiovascular diseases (31.3% vs 13.8%; p<0.001), and stroke (12.5% vs 5.6%; p=0.014); compared to their counterparts. Besides, patients with a history of diabetes had comparatively a higher proportion of Type 2 diabetes, hyperosmolar hyperglycemic state, and a 30 days cases of mortality rate (53.7% vs 38.3%; p<0.001), (31.8% vs 15.8%; p<0.001), and (15.5% vs 8.7%; p=0.02) compared to patients without a history of diabetes, respectively. Likewise, comparatively, patients with a history of diabetes had a higher median of baseline blood pressure readings in mmHg than patients without a history of diabetes. However; patients with a history of diabetes had relatively lower mean baseline body urine ketones (2.1± 1.1 vs 2.7± 1.1; p<0.001) in mg/dl compared to their counterparts, respectively, (Table 1).
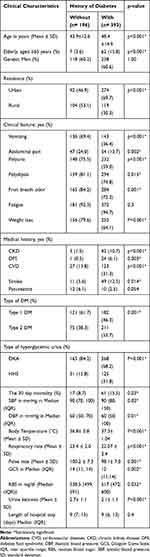 |
Table 1 Comparison of Clinical Characteristics of Adult Patients with a Hyperglycemic Crisis without and with a History of Diabetes in a Resource-Poor Community |
As Table 2 showed, comparatively a higher proportion of mortality was observed in rural residents than urban residents in both patients without and with a history of diabetes (13.5% vs 3.3%; p= 0.023), and (21.8% vs 12.8%; p= 0.03); respectively. In patients with a history of diabetes, a higher proportion of mortality was observed in patients who did not presented with polyuria (21.1% vs 11.6%; p=0.016), polydipsia (23.2% vs 12.9%; p=0.022), fruit breath odor (26.6% vs 11.3%; p<0.001), and weight loss (22.0% vs 11.9%; p=0.012) compared to patients who had on admission. Whereas, in patients without a history of diabetes, a higher proportion of mortality was observed in patients who had not fruit breath odor on admission (25.8% vs 5.5%; p= 0.001) compared to those who had the presentation on admission. In both patients without and with a history of diabetes, a higher proportion of mortality was observed in patients who had a medical history of Chronic Kidney Diseases, Cardiovascular diseases, and stroke than without a medical history. Similarly, 30 days of cases mortality was higher in Type 2 diabetes patients than type 1 diabetes (16.0% vs 4.1%; p= 0.009) and (22.3% vs 7.7%; p<0.001) in both patients without and with a history of diabetes, respectively. Besides, patients with HHS had comparatively a higher proportion of mortality than patients with DKA (29.0% vs 4.8%; p< 0.001) and (27.2% vs 10.1%; p<0.001) in both patients without and with a history of diabetes, respectively. Similarly, in both patients without and with a history of diabetes; lower mean baseline urine ketones (1.9± 1.3 vs 2.8± 1.1; p=0.008); and (1.64± 1.2 vs 2.2± 1.04; p=0.002) was statistically significantly associated with a 30 days cases of mortality, respectively. Also, in patients with a history of diabetes a higher median blood pressure in mmHg (p<0.01), and RBS in mg/dl (p= 0.003) readings at baseline was statistically significantly associated with a 30 days cases of mortality.
 |
Table 2 Comparision of Hospital Management and Clinical Outcomes Adult Patients with a Hyperglycemic Crisis without and with a History of Diabetes in a Resource-Poor Community |
On the multivariate logistic regression model (Table 3), independent predictors of a 30 days case of mortality were a rural residents [AOR=3.1, 95% CI 1.8, 5.4], patients with a medical history of stroke [AOR=2.7, 95% CI 1.3, 5.6], type 2 diabetes [AOR=2.3, 95% CI (1.1, 4.7)], hyperosmolar hyperglycemic state [AOR=2.4, 95% CI (1.1, 5.4)], and patients with history of diabetes [AOR=2.0, 95% (CI 1.04, 3.8)]; while presentation with polydipsia on admission was preventive [AOR= 0.47, 95% CI 0.27, 0.81]; (Table 3).
 |
Table 3 Potential Risks of Hyperglycemic Crisis-Related Mortality Among Patients without and with a History of Diabetes in a Resource-Poor Community |
Discussion
In this study, patients without a history of diabetes had a higher proportion of classic signs and symptoms of diabetes. Whilst, the proportion of Type 2 diabetes, hyperosmolar hyperglycemic state, and medical history of chronic diseases were higher among those patients with a history of diabetes. Also, the mortality rate was comparatively higher in those patients with a history of diabetes. A higher proportion of mortality was observed in patients from rural. Similarly, higher a 30 days case of mortality was reported among those patients with T2D, HHS, a lower mean of urine ketones, had a medical history of chronic kidney disease, cardiovascular disease, and stroke. Rural residence patients, type 2 diabetes, hyperglycemic hyperosmolar state, had a medical history of stroke, and history of diabetes were independent predictors of mortality while had polydipsia on admission was preventive.
In the current findings, although patients without a history of diabetes had better consciousness compared to with a history of diabetes, but had more pronounced signs and symptoms for hyperglycemic crisis (vomiting, abdominal pain, polyuria, polydipsia, fruity breath odor, and body weight loss) compared to patients with a history of diabetes; which is in line with findings in Taiwan.11 We believe that it could be due to two-third of the patients without a history of diabetes had type 1 diabetes that presents with these classic signs and symptoms of diabetes mellitus.18,19
In the current study, comparatively a higher proportion of the hyperglycemic crisis among rural residents in patients without a history of diabetes than those with a history of diabetes. This is due to people living in rural areas have increased treatment gaps, less access to health care services, and long-distance travel to health services. On the other hand, somewhat a greater proportion of hyperglycemic crisis among urban residents in patients with a history of diabetes compared to those patients without a history of diabetes. This might be due to poor compliance, unaffordability of insulin medicine, and inaccessibility of anti-diabetes medicines. We suggest expansion diabetes care services to the primary health care units, integrate diabetes screening in the health extension packaging programs, and providing diabetes self-care management education.
Furthermore, DKA was more common in patients without a history of diabetes (84.7%), while HHS is more pronounced in patients with a history of diabetes. As a result, a higher mortality rate is reported in patients with a history of diabetes. This finding contradicts a study conducted in other parts of Ethiopia2 but consistent with findings from Taiwan and South Africa.11,15 The higher incidence of DKA in patients without a history of diabetes may be related to a relatively younger age and more than half of the patients are from rural residents which could be associated with poverty.20,21
The overall 30 days case of hyperglycaemic crisis-related mortality is 13.2%; which is higher than studies in Colombia, China, Taiwan, and other parts of Ethiopia that reported mortality rates ranging from 2.27 to 10.6%;1,2,11,22 but lower than 20% mortality in Nigeria.23 The disparity might be due to differences in inpatient management protocol of hyperglycemic crisis, inadequate laboratory investigations at presentation, insufficient laboratory monitoring during treatment to monitor patient response, and also the absence of routine annual checkup policy for NCDs- in Ethiopia. Besides a delayed diagnosis of T2D, and then present for medical attention after developing diabetes complications.
In this study, a lower mortality rate in patients without a history of diabetes than patients with a history of diabetes is reported. Many diabetes patients might die undiagnosed and before access to diabetes treatment particularly in rural areas. This finding is still higher than studies in other parts of Ethiopia, China, and Taiwan.2,11,22 This disparity might be due to a delayed diagnosis of T2D and then present for medical attention after developing diabetes complications. And also; the absence of inpatient management protocol, and insufficient laboratory monitoring during treatment to monitor patient response in the studied hospitals. The researchers suggest the expansion of reliable diabetes care services to the primary health care units and integrating diabetes in the health extension packaging. Furthermore, the inpatient management protocol of the hyperglycemic crisis has to be equipped with adequate laboratory investigations and sufficient laboratory monitoring during treatment to monitor patient response. Also, routine annual checkup policies for NCDs, including diabetes have to be implemented.
In this finding, more than three times higher a 30 days cases of mortality among rural patients than urban; which is consistent with a study in China.22 This higher mortality in rural patients might be people living in rural areas have less access to diabetes screening and preventive services. Besides, long-distance travel to health care services, and have increased treatment gaps. Likewise, these individuals are unaware of their glycemic state and then present for medical attention after developing diabetes complications and worsening of the conditions. Therefore, the need for more public health awareness campaigns about diabetes, and the expansion of diabetes care services to the primary health care units particularly in the rural areas is a fundamental measure.
The findings of this study revealed that lower mortality is reported in patients who had classic signs and symptoms of diabetes (vomiting, polydipsia, polyuria, fruity breath odor, and body weight loss) than those who had not on admission. Mortality is reduced by 47% in patients who had polydipsia on admission. Nevertheless, delayed recognition of hyperglycemic symptoms in T2D and ignorance of diabetes complications might lead to mortality.11,22 Public health awareness campaigns have to be made to increase health-seeking behavior to make annual checkups and the classic symptoms of diabetes.
In both patients, a higher proportion of mortality is reported in patients who had a medical history of chronic kidney disease, cardiovascular disease, and stroke compared to patients who had not. Patients who had a medical history of stroke are 2.7 times as great as the likelihood of mortality those who had not a medical history of the stroke on admission. This study is consistent with the study in Taiwan.11,22 Medical attention after developing diabetes complications, absence of integrated inpatient management protocol of hyperglycemic crisis and co-morbidity, and inadequate laboratory monitoring during treatment to monitor patient response might be the reasons for higher mortality.
In this study, patients with type 2 diabetes, and hyperosmolar hyperglycemic state had more than two folds higher mortality than patients with type 1 diabetes, and DKA respectively. A higher 30 days cases of mortality are observed in patients with a lower mean of urine ketones which is common T2D and HHS in both patients without and with a history of diabetes. This higher mortality might be due to delayed diagnosis of T2D and ignorance of diabetes complications which results in severe dehydration and neurologic deficit that can lead to death. We recommend more public health awareness campaigns and diabetes screening for people with known risk factors.
Furthermore, two folds higher a 30 days of cases mortality in patients with a previous history of diabetes than without a history of diabetes; which is parallel with a study in Taiwan.11 Long-standing hyperglycemia due to poorly controlled diabetes and ignorance of diabetes complications might be the reason for the higher mortality.
Nevertheless, the present study had several limitations. The first limitation, the data were obtained retrospectively from patient charts, where clinical presentations or records might not have been completely documented. Some patients may have been excluded due to a lack of data for analysis. The second limitation, data were not validated, which could have led to misclassification of type hyperglycemic crisis, though the overlaps do not affect the present study results. Third, the study is limited to include important diagnostic criteria for the classification of hyperglycemic crises due to the study is conducted in general hospitals with a lack of advanced laboratory setups. Fourth, the study is limited to medical wards, and do not include patients against medical advice, pregnant mothers, and patients referred to other hospitals. Fifth, this was a single- Regional State study, where findings from our database might not be generalizable to the entire national hospitals, but it can generalize for hospitals in Tigrai.
Conclusions
Comparatively a higher 30 days cases of mortality in patients with a history of diabetes compared to patients without a history of diabetes. Moreover, a higher proportion of mortality is rural residents in both patients. Also, mortality was higher among patients with type 2 diabetes and hyperosmolar hyperglycemic state in both patients. Rural residents, Type 2 diabetes, hyperosmolar hyperglycemic state, had a medical history of stroke, and with a history of diabetes were independent predictors of 30 days cases of mortality; while polydipsia was preventive. We suggest regular check-ups and screening for NCDs and more public health awareness campaigns. We also recommend expanding diabetes care services to the primary health care units and integrate diabetes screening in the health extension packaging programs. Furthermore, improving the inpatient management protocol of hyperglycemic crisis and equipped advanced laboratory investigations.
Abbreviations
AAU-CHS, Addis Ababa University-College of Health Sciences; DBP, CKD, chronic kidney disease; Diastolic blood pressure; DFS, diabetic foot syndrome; DKA, diabetic ketoacidosis; DM, diabetes mellitus; GCS, Glasgow Coma Scale; HEs, hyperglycemic emergencies; HHS, hyperosmolar hyperglycemic state; IRB, Institution Review Board; IQR, Interquartile ranges; T1D; type 1 diabetes; T12D; type 2 diabetes SD, standard deviation; SBP, systolic blood pressure; SD, Standard Deviation.
Data Sharing Statement
All data about the findings are presented in this paper. However, the data can be obtained from the corresponding author at any time on reasonable request.
Acknowledgments
The sudden death of Professor Fikre Enquo Selassie is really painful and hurting. He was not only a good professor of epidemiology and biostatistics but also, he had a unique human entity to his family, students, and staff. It pains me to notify you that, professor Fikre, left for his heavenly abode on October 28, 2019, on account of sudden death. Professor Fikre was vigorously involved in all activities of the study from the proposal development to manuscript approval for publication. The authors express their gratitude to the Addis Ababa University for its financial support to conduct this study. Additionally, we would like to express our heartfelt thanks to the selected public hospitals’ administrative bodies, staff, data collectors and supervisors, and the Tigrai Regional Health Bureau office for granting access to these data.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Chaithongdi N, Subauste JS, Koch CA, Geraci SA. Diagnosis and management of hyperglycemic emergencies. Hormones. 2011;10(4):250–260.
2. Desse TA, Eshetie TC, Gudina EK. Predictors and treatment outcome of hyperglycemic emergencies at Jimma University Specialized Hospital, southwest Ethiopia. BMC Res Notes. 2015;8. doi:10.1186/s13104-015-1495-z
3. Corwell B, Knight B, Willis GC. Current diagnosis and treatment hyperglycemic emergencies. Emerg Med Clin North Am. 2014;32:437–452.
4. Builes-montaño CE, Chavarriaga A, Ballesteros L, et al. Characteristics of hyperglycemic crises in an adult population in a teaching hospital in Colombia. J Diabetes Metab Disord. 2018;17(2018):143–148. doi:10.1007/s40200-018-0353-7
5. Chang L, Lin L, Tsai M, How C. Association between hyperglycaemic crisis and long-term major adverse cardiovascular events: a nationwide score-matched, cohort study. BMJ Open. 2016;6(8):e012233. doi:10.1136/bmjopen-2016-012233
6. Nkpozi MO, Ezeani IU, Korubo IF, Chinenye S, Jumbo AUC. The outcome of hyperglycemic emergencies in a tertiary hospital, South East, Nigeria. Sahel Med J. 2019;22:47–54.
7. You JH, Song SO, Park SH, et al. Trends in hyperglycemic crisis hospitalizations and in- and out-of-hospital mortality in the last decade based on Korean National Health Insurance Claims Data Data source. Endocrinol Metab. 2019;34:275–281. doi:10.3803/EnM.2019.34.3.275
8. Anthanont P, Thana Khawcharoenporn TT. Incidences and outcomes of hyperglycemic crises: a 5-year study in a tertiary care center in Thailand. J Med Assoc Thai. 2012;95(8):995–1002.
9. Centers for Disease Control and Prevention. National diabetes statistics report, 2014 estimates of diabetes and its burden in the epidemiologic estimation methods. Natl Diabetes Stat Rep. 2014:1–12.
10. American Diabetes Association. Economic costs of Diabetes in the US in 2012. Diabetes care. 2013;36(4):1033–1046.
11. Chou W, Chung M, Wang H, Chen J, Chen W, Guo H. Clinical characteristics of hyperglycemic crises in patients without a history of diabetes. J Diabetes Investig. 2014;5(6):657–662.
12. Ogbera AO, Awobusuyi J, Unachukwu C, Fasanmade O. Clinical features, predictive factors, and outcome of hyperglycaemic emergencies in a developing country. BMC Endocr Disord. 2009;9(9):1–5. doi:10.1186/1472-6823-9-9
13. Chb DJPMB, Bch VCBMB, Chb NSLMB, Ma SC. Hyperglycaemic emergency admissions to a secondary-Level hospital — an unnecessary financial burden Hyperglycaemic emergency admissions to a secondary-level hospital – an unnecessary financial burden. J Endocrinol Metab Diabetes S Afr. 2014;9677.
14. Olugbemide O, Bankole I, Akhuemokhan K, Adunbiola P. Original article clinical profile and outcome of hyperglycaemic emergencies at a rural hospital in southern Nigeria. African J Diabetes Med. 2017;25(2).
15. Ekpebegh CO, Akinrinmade A, Badri M, Levitt NS. Hyperglycaemic crisis in the Eastern Cape province of South Africa: high mortality and association of hyperosmolar ketoacidosis with a new diagnosis of diabetes. S Afr Med J. 2010;100(12):822–826.
16. Bedaso A, Oltaye Z, Geja E, Ayalew M. Diabetic ketoacidosis among adult patients with diabetes mellitus admitted to the emergency unit of Hawassa university comprehensive specialized hospital. BMC Res Notes. 2019;12:137.
17. Abegaz M, Mekonnen GA, Gebreyohannes EA, Gelaye A. Treatment outcome of diabetic ketoacidosis among patients attending a general hospital in north-west Ethiopia: a hospital-based study. BioRxiv. 2018:441964.
18. Atlas IDF. IDF Diabetes Atlas; 2019.
19. American Diabetes Association. Standards of Medical Care in diabetes — 2020. J Clin Appl Res Educ Diabetes Care. 2020;43(supplement 1).
20. Balcha SA, Phillips DIW, Trimble ER. Type 1 diabetes in a resource-poor setting: malnutrition related, malnutrition modified, or just diabetes? Curr Diab Rep. 2018;18(47):2–7. doi:10.1007/s11892-018-1003-7
21. Fekadu S, Yigzaw M, Alemu S, et al. Insulin-requiring diabetes in Ethiopia: associations with poverty, early undernutrition, and anthropometric disproportion. Eur J Clin Nutr. 2010;64(10):1192–1198. doi:10.1038/ejcn.2010.143
22. Bragg F, Holmes MV, Iona A, et al. Association between diabetes and cause-specific mortality in Rural and Urban Areas of China. JAMA. 2017;317(3):280–289. doi:10.1001/jama.2016.19720
23. Ogbera AO, Fasanmade OA, Chinenye S, Akinlade A. Characterization of lipid parameters in diabetes mellitus – a Nigerian report. Int Arch Med. 2009;2(19):1–7. doi:10.1186/1755-7682-2-19
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
