Back to Journals » Clinical Ophthalmology » Volume 14
Hybrid Telehealth Medical Retina Clinic Due to Provider Exposure and Quarantine During COVID-19 Pandemic
Authors Aweidah H , Safadi K, Jotkowitz A, Chowers I, Levy J
Received 9 August 2020
Accepted for publication 3 September 2020
Published 21 October 2020 Volume 2020:14 Pages 3421—3426
DOI https://doi.org/10.2147/OPTH.S276276
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Hamzah Aweidah,1 Khaled Safadi,1 Alan Jotkowitz,2 Itay Chowers,1,* Jaime Levy1,*
1Department of Ophthalmology, Hadassah-Hebrew University Medical Center, Jerusalem, Israel; 2Department of Internal Medicine, Faculty of Health Sciences, Ben-Gurion University of the Negev, Beer-Sheva, Israel
*These authors contributed equally to this work
Correspondence: Jaime Levy
Department of Ophthalmology, Hadassah-Hebrew University Medical Center, Jerusalem, Israel
Email [email protected]
Objective: To present our hybrid telehealth medical retina clinic service with intravitreal injections (IVI) treatment as a safe alternative to in-person visits and examination during COVID-19 pandemic disease.
Methods: Due to exposure to a COVID-19 positive retina fellow, our retina service, in quarantine, evaluated patients’ medical files and retinal scans using a telemedicine approach. A different protocol for patients coming for IVI during the COVID-19 pandemic was established for IVI administration.
Results: During the 14-day quarantine period (between March 18th and March 31st 2020), the hybrid telehealth medical retina clinic performed 523 IVI to 394 patients with a mean age ± SD 70.96 ± 14.4 years. IVI were administered for neovascular age-related macular degeneration in 50.5% of the cases (199 patients), diabetic macular edema in 21.3% (84 patients), retinal vein occlusion in 17.5% (69 patients), and 10.7% for other retinal pathologies (42 patients). No ocular or systemic complications were observed.
Conclusion: During disasters and pandemics, IVI can be provided safely using a hybrid telehealth medical retina clinic approach but only in the appropriate patient and health care system.
Keywords: COVID-19, telemedicine, ophthalmology, intravitreal injections, hybrid telehealth medical retina clinic
Introduction
Severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2), responsible for the pandemic of corona virus disease 2019 (COVID-19) impacted the health systems, governments and the world’s economy. The accompanying possible exposure of health workers to the virus and the social distancing policies required to protect our providers, affiliate staff, and patients has necessitated the need to consider new methods to provide the best treatment without any impact on its quality.
Retina clinics usually accept a high volume of patients with a strict schedule required for office visits and intravitreal injections (IVI) for the treatment of different retinal diseases such as age-related macular degeneration (AMD) and diabetic macular edema (DME).1–4
Neovascular AMD (nAMD) and DME are regularly treated with injections into the eye (intravitreal injections-IVI) every 4 up to 12 weeks according to retinal scan findings using optical coherence tomography (OCT). Consequently, IVI have become the most commonly performed ophthalmic procedure,5 with over 12 million IVI performed worldwide.
The COVID-19 pandemic pushed forward the use of telemedicine for delivering health care.6 Since the declaration of COVID-19 as a national emergency in the United States, the Department of Health and Human Services notified specific health care providers, including ophthalmologists, to serve patients and to communicate with them wherever they are using telehealth services, through remote communications technologies.7,8
In previous complex medical situations telemedicine has been shown to be of great benefit for many conditions9 ranging from hepatitis C management,10 the 2016 Zika virus outbreak in Puerto Rico,11 and education about infectious diseases after the recovery from Hurricane Maria.
As COVID-19 became a pandemic disease,12 there has been a pressing concern regarding medical workforce availability. In the case of COVID-19, healthcare worker's exposure is a primary concern. Known or possible exposure to the virus could put many essential personnel into quarantine. In Israel, health care workers with a possible exposure to a COVID-19 patient are required to complete a 14-day quarantine from the last contact day.
The decrease in workers would limit patient care and put pressure on those that can still provide it in-person. At institutions with telemedicine ability, quarantined physicians can cover those services, freeing up other physicians to perform in-person care. Office-based practices can also employ quarantined physicians to care for patients remotely. The challenge is that other health professionals (nurses, medical assistants, physician's assistants) also contribute to in-person care, and telemedicine cannot replace them all.13
Our ophthalmology department is one of the largest in Israel in which we provide daily medical and surgical treatment for all ophthalmic diseases. The retina specialty is unique in ophthalmology in that a significant percentage of clinic visits involve IVI. The injection procedure itself exposes both the patient and the treating physician to a very close contact of a few inches, far shorter than the recommended social distancing of 6 feet.14 This combined with the current high volume of IVI, poses a significant public health risk for COVID-19 transmission.15 On the other hand, withholding IVI can cause irreversible vision loss in some patients.16,17
Through a unique set of circumstances, on March 18th 2020, one of our retina fellows was diagnosed with COVID-19 and hospitalized. This caused three (two vitreoretinal surgeons (VRs) and one medical retina specialist) out of five of our retina specialists in addition to the only two retina fellows to be placed into a 14-day quarantine. Our department faced a sudden considerable shortage in the retina team, with only one VR and one medical retina specialists for all patients coming with a surgical or medical need.
The objective of this study is to present our hybrid telehealth medical retina clinic used during this period to approach all patients requiring IVI.
Methods
This retrospective observational study adhered to the tenets of the Declaration of Helsinki and the Health Insurance Portability and Privacy Act of 1996 and was approved by the Institutional Review Board of Hadassah Hebrew University Medical Center. No patient informed consent was required.
During the 14-day quarantine period between March 18th and March 31st 2020 (In-COVID), patients scheduled for IVI were called before their visits and assigned to come at specific times during the working hours in order to contend with the capacity and social distancing issues.
At presentation to the clinic, patients were guided immediately to the injection ward where they met the nurses and were told that they will be evaluated using the hybrid telehealth medical retina service and were instructed about the current workflow in the clinic and underwent an initial questionnaire that included questions regarding any change in their visual acuity (VA) or any new ocular complaints (such as: pain, redness, floaters or metamorphopsia) as well as any signs or symptoms of COVID-19.
Following this and according to their answers, patients were distributed to three different OCT devices in separate rooms in which they underwent the OCT images. The OCT images were then transferred to one of the quarantined retinal team by a secured real time remote connection used for the whole team using Microsoft remote desktop application for Microsoft Windows and Apple Macintosh desktops (Microsoft Corporation, Sacramento, CA, Version 10.3.12). Ophthalmologists-at-home were able to get real time access to patients’ medical files, check their previous visits and OCT images as well as the most recent OCT images. A decision for the treatment and follow-up was then filled directly by the ophthalmologists-at-home (first retinal team) to the electronic medical record system of the examined patient and transferred back to the site team. The site team consisted of a nurse that checked the recommendations written for each patient by the ophthalmologists-at-home and transferred that recommendations to a non-retina specialist ophthalmologist who conducted the intraocular injection for those patients according to the first team recommendations.
All patients were advised to seek ophthalmological evaluation in the clinics during the working hours and in the ophthalmology emergency department at any time if any of the following symptoms appear in the eye following IVI: ocular pain, redness, blurred vision, floaters, scotoma or decrease of vision.
The hybrid telehealth visit approach was applied for three groups.
Uninfected Patients with No Ocular and/or VA Complaints
Patients who did not report any change in their VA, have an ocular complaint, or any COVID-19 signs or symptoms got their IVI by the non-retina specialist ophthalmologist with a follow up according to the first team recommendations.
Uninfected Patients with Ocular and/or VA Complaints
If the patient reported any change to their VA or had any ocular complaint but without COVID-19 signs or symptoms; a complete ophthalmological examination was conducted by a non-retina specialist ophthalmologist after acquiring the OCT images. The examination and OCT results were documented in the patient electronic medical record system and were checked by one of the first retinal team who gave the decision for the treatment and follow up recommendations.
Patients Who May Have COVID-19
Patients who reported any signs or symptoms of COVID-19 were checked in a separate distant examination room by a non-retina specialist ophthalmologist with personal protective equipment (PPE) without acquiring OCT images. If the patient reported any change in VA or any other ocular complaint, the examination results were documented in the patient electronic medical record system and checked by one of the first retinal team who gave a real time decision for the treatment and follow up recommendations depending on the current examination results and the previous OCT images the patient had in their last IVI visit.
For patients without any change in VA or ocular complaints, that was documented in the patient electronic medical record system, the first retinal team gave the decision for the treatment and follow up recommendations depending on the previous OCT images the patient had. If the recommendation was to give IVI, that was done in the same examination room by the non-retina specialist ophthalmologist with the PPE.
New Patients
Patients on a first visit to the retina clinic were checked and evaluated by one of the two retina specialists. They underwent the required retinal images then treated accordingly.
The results of the IVI during the two week In-COVID period were analyzed and compared to a two week period before the COVID-19 outbreak in Israel, between January 1st and January 14th 2020 (Pre-COVID).
Results
During the COVID-19 period (In-COVID), 394 patients were treated with IVI by the use of the hybrid telehealth medical retina clinic. 49.3% males and 50.7% females. The mean age ± SD was 70.96 years ± 14.4 (range; 28–95 years). Of the 394 patients, 50.5% (199 patients) were diagnosed with nAMD, 21.3% (84 patients) with DME, 17.5% (69 patients) with Retinal Vein Occlusion (RVO) with cystoid macular edema and 10.7% (42 patients) with other retinal pathologies including myopic choroidal neovascularization, polypoidal choroidal vasculopathy and punctate inner choroidopathy. 31.7% of the patients (n=125) received injections in the right eye, 35.5% (n=140) received injections in the left eye while 32.8% (n=129) received injections in both eyes. The total number of injections was 523 (Table 1).
 |
Table 1 Demographic Features |
The mean In-COVID VA by the Logarithm of the Minimum Angle of Resolution (LogMAR ± SD) was 0.6 ± 0.6. Monthly injections protocol was used in 56.1% of cases (221 patients) while the treat-and-extend protocol was used in 43.9% (173 patients). The mean ± SD central subfield thickness (CST) was 318.13 ± 107.47 microns (Table 2).
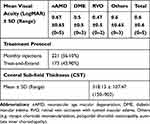 |
Table 2 Clinical Features |
During the In-COVID period, 523 IVI were performed. Among them, 59.8% were bevacizumab (Avastin), 30.6% were aflibercept (Eylea) and 9.6% were ranibizumab (Lucentis) (Table 3).
 |
Table 3 Treatment in Pre-COVID and In-COVID Periods |
During the Pre-COVID period, 607 patients (86% of the scheduled patients) came to our retina clinic, according to their scheduled appointment, to receive their planned IVI. The total number of IVI was 705 and included 67.4% of bevacizumab, 23.8% of aflibercept and 8.8% of ranibizumab (Table 3).
During the In-COVID period, 35% of the scheduled patients did not show up for their appointment to receive IVI vs. 14% for the Pre-COVID period. The overall number of patients coming for IVI has been reduced by COVID-19, but the number of injections related to the number of patients remained overlapping (Table 3).
Discussion
We report the use of a telemedicine approach to evaluate, treat and schedule appointments for all patients requiring IVI in our retina clinic during the In-COVID period. During the 14-day quarantine period, the hybrid telehealth medical retina clinic performed 523 IVI to 394 patients.
During this pandemic, everyone became remote and underserved, this raised the question: can in-person visits and examination become the second, third, or even last option for meeting retina clinic patient's needs? Fortunately, nowadays we work in an environment with highly advanced technology, making telehealth mainstream.
Telemedicine has been used in ophthalmology in different aspects including mainly the screening and diagnosis of diabetic retinopathy,18 but also the diagnosis of retinopathy of prematurity (ROP) by using trained non-expert personnel to capture images and transfer data to remote ophthalmologists,19 as well as in glaucoma and other eye diseases.20
Teleophthalmology has been previously described in patients with AMD requiring IVI.21,22 Local ophthalmologists were able to examine and acquire macular OCT imaging on those patients and send this information, electronically, to the overseeing retina specialist, who recommended the treatment with IVI and allowed patients to continue their overall eye care with their local ophthalmologist.
Disasters and pandemics pose unique challenges to health care delivery as physicians in every specialty find themselves working at an exceptional moment. They are the forefront of a fast-moving process that forces them to accommodate to try to provide the best medical service to their patients. The unfortunate occurrence of a pandemic is an opportunity to set up an infrastructure for providing the best retinal care using teleophthalmology with hybrid telehealth visits. For COVID-19, social distancing, at variable stringency levels, is likely to stay around for months or even years,23 and different diagnostic and therapeutic approaches used during COVID-19 times may change traditional ones.
Though our hybrid telehealth visits are not expected to solve all the medical retinal diseases, they are well suited for scenarios in which infrastructure remains intact and clinicians are available to see patients. During the In-COVID period, 35% of the scheduled patients for IVI did not show up for their appointment vs. 14% for the Pre-COVID period. The overall number of patients coming for IVI has been reduced by COVID-19, but the number of injections related to the number of patients remained overlapping, evidencing that the use of the hybrid telehealth medical retina clinic maintained the continuity of IVI with preservation of vision.
The main limitations of our report are its retrospective nature and the short period of evaluation. The time to get all retina images and patient’s files remotely and at a hospital computer at the retinal clinics could not be compared. Patients’ satisfaction and comparison with regular follow-up in clinics could not be determined. The changes in the intraocular pressure (IOP), cataract or new peripheral retinal abnormalities could not be obtained with the use of this model.
In conclusion, a successful hybrid retinal telemedicine service requires an advanced health systems network with excellent communication and the ability to share electronic data seamlessly. Telemedicine may offer a safe alternative to traditional office visits but only in appropriate patient and health care systems,24 and can help to prevent treatment delay-related damage for maculopathies. This approach may be applied to other areas in ophthalmology such as oculoplastics,25 neuro-ophthalmology,26 and pediatrics ophthalmology,27 in which many of these examinations can be performed externally and also in other fields in medicine such as radiology, cardiology, pathology and emergency services during the COVID-19 pandemic.
Patient and Public Involvement Statement
Patients or the public were not involved in the design, or conduct, or reporting, or dissemination plans of our research.
Disclosure
No financial support was received for the preparation of the article. The authors report no conflicts of interest for this work.
References
1. Flaxel CJ, Adelman RA, Bailey ST, et al. Age-related macular degeneration preferred practice pattern®. Ophthalmology. 2020;127(1):PP1–P65. doi:10.1016/j.ophtha.2019.09.024
2. Friedman DS, O’Colmain BJ, Muñoz B, et al. Prevalence of age-related macular degeneration in the United States. Arch Ophthalmol. 2004;122(4):564–572. doi:10.1001/archopht.122.4.564
3. Flaxel CJ, Adelman RA, Bailey ST, et al. Diabetic retinopathy preferred practice pattern®. Ophthalmology. 2020;127(1):P66–P145. doi:10.1016/j.ophtha.2019.09.025
4. Harris MI, Flegal KM, Cowie CC, et al. Prevalence of diabetes, impaired fasting glucose, and impaired glucose tolerance in U.S. adults: the Third National Health and Nutrition Examination Survey, 1988–1994. Diabetes Care. 1998;21(4):518–524.
5. Berkowitz ST, Sternberg P, Feng X, Chen Q, Patel S. Analysis of anti-vascular endothelial growth factor injection claims data in US medicare part B beneficiaries from 2012 to 2015. JAMA Ophthalmol. 2019;137(8):921–928. doi:10.1001/jamaophthalmol.2019.1971
6. Bashshur R, Doarn CR, Frenk JM, Kvedar JC, Woolliscroft JO. Telemedicine and the COVID-19 pandemic, lessons for the future. Telemed E Health. 2020;26(5):571–573. doi:10.1089/tmj.2020.29040.rb
7. Ophthalmology AA of. Academy, federal agencies issue new telehealth guidance in light of COVID-19. 2020. Available from: https://www.aao.org/eye-on-advocacy-article/academy-federal-agencies-issue-telehealth-guidance.
8. Department of Health and Human Services (HHS). Notification of enforcement discretion for telehealth remote communications during the COVID-19 Nationwide Public Health Emergency. 2020. Available from: https://www.hhs.gov/hipaa/for-professionals/special-topics/emergency-preparedness/notification-enforcement-discretion-telehealth/index.html.
9. Lurie N, Carr BG. The role of telehealth in the medical response to disasters. JAMA Intern Med. 2018;178(6):745–746. doi:10.1001/jamainternmed.2018.1314
10. Arora S, Thornton K, Murata G, et al. Outcomes of treatment for hepatitis C virus infection by primary care providers. N Engl J Med. 2011;364(23):2199–2207. doi:10.1056/NEJMoa1009370
11. American Academy of Pediatrics EP. 2016 zika virus outbreak in puerto rico. Available from: https://www.aap.org/en-us/professional-resources/practice-transformation/echo/Pages/default.aspx.
12. WHO. Novel coronavirus situation report situation report 22. February, 2020.
13. Hollander JE, Carr BG. Virtually perfect? Telemedicine for COVID-19. N Engl J Med. 2020;382(18);1–3.
14. CDC. Healthcare facilities: managing operations during the COVID-19 pandemic. 2020. Available from: https://www.cdc.gov/coronavirus/2019-ncov/hcp/guidance-hcf.html.
15. Corradetti G, Corvi F, Nguyen TV, Sadda SVR. Management of neovascular age-related macular degeneration during the COVID-19 pandemic. Ophthalmol Retina. 2020;4(8):757–759. doi:10.1016/j.oret.2020.05.015
16. Soares RR, Mellen P, Garrigan H, et al. Outcomes of eyes lost to follow-up with neovascular age-related macular degeneration receiving intravitreal anti-vascular endothelial growth factor. Ophthalmol Retina. 2019;4(2):134–140. doi:10.1016/j.oret.2019.07.010
17. Shmueli O, Chowers I, Levy J. Current safety preferences for intravitreal injection during COVID-19 pandemic. Eye. 2020;34(7):1165–1167. doi:10.1038/s41433-020-0925-x
18. Horton MB, Brady CJ, Cavallerano J, et al. Practice guidelines for ocular telehealth-diabetic retinopathy, third edition. Telemed J E Health. 2020;26(4):495–543. doi:10.1089/tmj.2020.0006
19. Murakami Y, Jain A, Silva RA, Lad EM, Gandhi J, Moshfeghi DM. Stanford University network for diagnosis of retinopathy of prematurity (SUNDROP): 12-month experience with telemedicine screening. Br J Ophthalmol. 2008;92(11):1456–1460. doi:10.1136/bjo.2008.138867
20. Hark LA, Adeghate J, Katz LJ, et al. Philadelphia telemedicine glaucoma detection and follow-up study: cataract classifications following eye screening. Telemed E Health. 2019;00(00):1–9. doi:10.1089/tmj.2019.0170
21. Starr MR, Barkmeier AJ, Engman SJ, Kitzmann A, Bakri SJ. Telemedicine in the management of exudative age-related macular degeneration within an integrated health care system. Am J Ophthalmol. 2019;208:206–210. doi:10.1016/j.ajo.2019.03.021
22. Brady CJ, Garg S. Telemedicine for age-related macular degeneration. Telemed E Health. 2020;26(4):565–568. doi:10.1089/tmj.2020.0011
23. Adam D. Special report: the simulations driving the world’s response to COVID-19. Nature. 2020;580(7803):316–318. doi:10.1038/d41586-020-01003-6
24. Saleem SM, Pasquale LR, Sidoti PA, Tsai JC. Virtual ophthalmology: telemedicine in a COVID-19 Era. Am J Ophthalmol. 2020;216:237–242. doi:10.1016/j.ajo.2020.04.029
25. Kang S, Thomas PBM, Sim DA, Parker RT, Daniel C, Uddin JM. Oculoplastic video-based telemedicine consultations: COVID-19 and beyond. Eye. 2020;34(7):1193–1195. doi:10.1038/s41433-020-0953-6
26. Lai KE, Ko MW, Rucker JC, et al. Tele-neuro-ophthalmology during the age of COVID-19. J Neuroophthalmol. 2020:292–304. doi:10.1097/wno.0000000000001024
27. Areaux RG, de Alba Campomanes AG, Indaram M, Shah AS. Your eye doctor will virtually see you now: synchronous patient-to-provider virtual visits in pediatric tele-ophthalmology. J Am Assoc Pediatr Ophthalmol Strabismus. 2020. doi:10.1016/j.jaapos.2020.06.004
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
