Back to Journals » Journal of Inflammation Research » Volume 13
HPV-16 E2/E6 and POU5F1B as Biomarkers to Determine Cervical High-Grade Squamous Lesions and More
Authors Chen L , Dong B, Gao H, Xue H, Pan D , Sun P
Received 1 September 2020
Accepted for publication 26 September 2020
Published 29 October 2020 Volume 2020:13 Pages 813—821
DOI https://doi.org/10.2147/JIR.S278911
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Ning Quan
Lihua Chen,1,2,* Binhua Dong,2,3,* Hangjing Gao,2,3 Huifeng Xue,4 Diling Pan,5 Pengming Sun1– 3
1Department of Gynecology, Fujian Provincial Maternity and Child Hospital, Affiliated Hospital of Fujian Medical University, Fuzhou, People’s Republic of China; 2Fujian Provincial Key Laboratory of Women and Children Major Disease, Fujian Provincial Maternity and Child Hospital, Affiliated Hospital of Fujian Medical University, Fuzhou, People’s Republic of China; 3Laboratory of Gynecologic Oncology, Fujian Provincial Maternity and Child Hospital, Affiliated Hospital of Fujian Medical University, Fuzhou, People’s Republic of China; 4Medical Center of Cervical Disease and Colposcopy, Fujian Provincial Maternity and Child Hospital, Affiliated Hospital of Fujian Medical University, Fuzhou, People’s Republic of China; 5Department of Pathology, Fujian Provincial Maternity and Child Hospital, Affiliated Hospital of Fujian Medical University, Fuzhou, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Pengming Sun
Fujian Provincial Maternity and Child Hospital, Affiliated Hospital of Fujian Medical University, 18 Daoshan Road, Fuzhou 350001, Fujian, People’s Republic of China
Tel +86-591-87558732 (Lab Office)
Fax +86-591-87551247
Email [email protected]
Purpose: Human papillomavirus-16 (HPV-16) is the most carcinogenic HPV genotype. This study aimed to evaluate the clinical value of POU5F1B and HPV-16-E2/E6 by cervical cytology specimens to predict the cervical intraepithelial neoplasia two grade and more (CIN2+).
Methods: Finally, 248 patients with HPV-16 single infection were enrolled. Using cytology specimen by real-time quantitative PCR (qPCR), POU5F1B mRNA and HPV-16-E2/E6 were detected. The relationship of POU5F1B, HPV-16-E2/E6 and CIN2+ were analyzed, and the optimal cut-off values of POU5F1B and HPV-16-E2/E6 to predict CIN2+ were calculated.
Results: The mean HPV-16-E2/E6 decreased significantly with cervical lesions development, especially compared with CIN2+ (p< 0.05). And the POU5F1B demonstrated higher expression in CIN2+ than that of normal cervical tissue and CIN1 (p< 0.05). What is more, POU5F1B was negatively correlated with HPV-16-E2/E6. It demonstrated that the area under the receiver operating characteristic curve (AUC) for POU5F1B (0.9058) was higher than that for HPV-16-E2/E6 (0.8983), and the sensitivity and specificity of POU5F1B in the diagnosis of CIN2+ were higher than HPV-E2/E6. Furthermore, it demonstrated that the POU5F1B had the highest odds ratio (OR= 16.84; 95% CI (8.00– 35.46)) for the detection of CIN 2+.
Conclusion: HPV-16-E2/E6≤ 0.6471 or POU5F1B≥ 1.0310 in cervical exfoliated cells can be used as a reliable predictor of CIN2+. POU5F1B can be used as a new auxiliary biomarker to determine the HPV infection status and a reliable predictor of CIN2+. The expression of POU5F1B≥ 1.0310 had the highest OR for the detection of CIN2+.
Keywords: cervical intraepithelial neoplasia, human papillomavirus type 16, POU5F1B, HPV integration, HPV-E2/E6
Introduction
Cervical cancer is the most common cancer of the lower female genital tract worldwide. Nearly 529,828 newly reported cases and 275,128 deaths were reported yearly.1 China has 98,900 newly diagnosed patients and 30,500 deaths annually, with an increasing trend in China.2 Therefore, identifying of new and reliable biomarkers involved in cervical intraepithelial neoplasia two grade and more (CIN2+) is urgent and highly demanded, predicting the pathogenesis and development of cervical lesions.
Previous reports showed that the occurrence of cervical cancer and cervical precancerous lesions is mainly caused by the persistent infection of one or several high-risk human papillomaviruses (HR-HPV).3,4 And HPV-16 dominates 80–90% of all HPV-positive cases.5 However, Nearly 90% of women are likely to get HPV infections during their lifetime; only 10% will develop to persistent HPV infections, and only 1% will progress to cervical cancer.6 Therefore, the poor specificity of the HPV assay results in over-treatment and causes too anxious for patients. Fortunately, the increasing evidence has indicated that HPV integration into the host genome is considered a key step for the development of cervical intraepithelial neoplasia (CIN) and cervical cancer.7 So it is crucial to distinguish cervical lesions based on their progression ability if the biomarker is related to the HPV integration. However, the cause and consequences of HPV integration remain poorly understood.
It is reported that the hinge region of the HPV-E2 gene is unstable.8 It is the most common deletion or breakage site when the HPV DNA integrates into the host genome. And the deletion of the E2 gene makes the oncogenes E6, and E7 genes highly expressed.9–11 Therefore, the E2/E6 ratio has been utilized as surrogate markers to discriminate CIN2+.12–15 However, most published studies with HPV-E2/E6 are based on the cervical tissues by invasive biopsy procedures.
The relationship between HPV-E2/E6 and cervical lesions is still controversial because the Cut-off is different from many studies. Therefore, it expedites to find a new and non-invasive method further to evaluate the relationship between HPV-E2/E6 and cervical lesions. It is reported that POU5F1B, the POU domain five transcriptions factored 1B gene (also known as OCT4-pg1, OTF3C, OTF3P1 and POU5F1P1), had the highest integration frequency when HPV integration happened to use the next-generation sequences (NGS).7 It is located on chromosome 8q24. Current research shows that POU5F1B is a tumor susceptibility gene and expressed highly in some cancer tissues, such as rectal cancer, chronic lymphocytic leukemia, bladder cancer, prostate cancer, and hepatocellular carcinoma.16–18 However, there are a few studies about its expression status and biological function in cervical cancer.
Here, we investigate whether the expressions of POU5F1B and measurement of HPV-E2/E6 are predictive of CIN2+ and if analyses of the cervical cytological specimens non-invasively collected yield sufficiently conclusive results.
Patients and Methods
Patients and Study Design
We analyzed 248 participants with cervical specimens tested positive for HPV-16 single infection from the Fujian Provincial Maternity and Children’s Health Hospital, affiliated hospital of Fujian Medical University from December 2017 to September 2019. The population comes from one of the Fujian Cervical Lesion Screening Cohort (FCLSC), which has more than 120,000 cases involving the community population and hospital population. The populations must meet the following criteria: 1) HPV16 single infection; 2) age above 20 years; 3) sexually active; 4) no history of cervical cancer, CIN, or HIV infection; and 5) did not undergo a cervix surgery or hysterectomy. The Hospital Ethics Committee approved the study (FMCH2017J01232), and all individuals participating in this study provided written informed consent.
Specimen Collection and Management
Exfoliated cervical cells were collected from each participant using a cytobrush. The specimens were collected from the cervical canals. They were gathered in 2-mL vials containing preservation solutions for HPV DNA testing or in 20-mL bottles of ThinPrep® PreservCyt® solution (Hologic, Waltham, MA, USA) cytology examination. The samples for HPV testing need to be stored at −20°C before DNA extraction, and the examples for cytology needs to be stored at 4°C.
Liquid-Based Cytology, HPV Genotyping Test
Cytological specimens were blindly reviewed, independent of the other assays’ results, by two experienced cytopathologists. The results were reported following the Bethesda 2001 system.19 If the diagnosis was different, the cervical samples were evaluated again, and a consensus diagnosis was obtained. The PCR-RDB HPV genotyping kit (Yaneng Limited Corporation, Shenzhen, China) can detect 18 HR-HPV types and 5 LR-HPV types. All examination procedures were performed according to the manufacturer’s instructions provided by the kit.20
Histology
Women who were HPV-16 positive with or without abnormal cytological results (with a grade higher than atypical squamous cells of undetermined significance (ASC-US)) need to be referred for colposcopy and punch biopsy. Women with a punch biopsy diagnosis greater than high-grade squamous intraepithelial lesions and more (HSIL) received loop electrosurgical excision procedure cone biopsy (LEEP) or conization by the cold knife. Specimens were fixed in 10% formalin and were routinely processed for paraffin embedding. Then, 4 µm thick histological sections were cut and stained with hematoxylin and eosin using standard methods. According to the 2014 World Health Organization (WHO) Classification of Tumors of the Female Genital Tract, the pathological diagnostic standard is defined.21 An independent expert reviewed all samples with a primary histology result of CIN2+. If the review reading is inconsistent, conduct a second histological review. If two-thirds of the diagnoses are the same, the result is considered the final result.
RT-PCR and Analysis of HPV16-E2/E6
For the HPV DNA extraction, we centrifuge the remaining cervical cells and resuspend them in a digestion solution (10 mmol/L Tris, one mmol/L ethylenediaminetetraacetic acid, 200 μg/mL proteinase K) for 3 hours at 56°C. It was incubated at 95°C for ten minutes to inactivate proteinase K. Real-time quantitative PCR (qPCR) was carried out with modifications in the protocol. E2 PCR was utilized with primer pairs 5′-AGT AAC TGT GGT AGA GGG TCA AG-3′ and 5′-TCA GGA GAG GAT ACT TCG TTG TC-3′, while E6 PCR was performed with primer pairs 5′-CGT GAG GTA TAT GAC TTT GCT TTT C-3′ and 5′-TGT ATT GCT GTT CTA ATG TTG TTC C-3′. And the POU5F1B PCR was reproduced with primer pairs 5′-TGG CAT TCT TAT CCA CAA AGT GA-3′ and 5′-CTG TGA CCG TAT GGC TGT GT-3′. β-globin was applied as an experimental control for sample quality and adequacy during the PCR process. β-globin PCR was reproduced with primer pairs 5′-GCA CCG TCA AGG CTG AGA AC-3′ and 5′-TGG TGA AGA CGC CAG TGG A-3′. Relative levels of ERα and ERRα mRNA were quantified by qPCR and calculated by the 2−ΔΔCT method. According to the PCR results, E2/E6 of cervical cells were calculated to assess HPV integration status. E2/E6 of 1 was regarded as “episome state,” and that ranging from >0 to <1 shown “mixed state”; a ratio of 0 was considered as a “fully integrated state.” The “episomal state” means that HPV is not integrated into the host genome. Conversely, the “fully integrated state” will result in the loss of E2.22
Statistical Analysis
The counting data were analyzed with t-tests, and the measurement data were Chi-square tests. The data were calculated using the IBM SPSS statistical package version 22.0 (IBM Corporation, Armonk, NY, USA). To evaluate the association between the severity of cervical pathology and physical status of HPV integration, linear by linear analysis was performed. Diagnostic accuracy of POU5F1B and E2/E6 ratio for CIN2+ was expressed as the area under the receiver operating characteristic (ROC) curve (AUC). The odd’s ratios (ORs) with 95% confidence intervals (CIs) were used to estimated different risks. In all statistical tests, the differences were considered statistically significant at P-values<0.05
Result
Clinical Presentation and Associations Between Cervical Lesions and Clinicopathological Factors
Analysis of the 248 cervical tissue samples with HPV16 single infection indicated that 53 (21.37%) were normal, 54 (21.77%) were classified as CIN1, 87 (35.08%) were categorized as CIN2/3, and 54 (21.77%) were diagnosed as CC. The clinicopathologic features of the study population are presented in Table 1. The age, cytology, E2/E6 and the POU5F1B were significantly related to cervical lesions. It revealed that older age and abnormal cytology promoted the development of CIN2+. What is more, With the development of cervical lesions, HPV-E2/E6 decreased, but POU5F1B expression increased significantly, especially compared with CIN2+. It suggested that HPV-E2/E6 and POU5F1B could predict the development of CIN2+ lesions (p<0.01).
 |
Table 1 Clinical Characteristics of the Participants of the Study |
We found a significant difference in means of HPV-E2/E6 in four groups (p<0.001, ANOVA test) (Figure 1A and B). No significant difference was found between normal pathology and CIN1 in terms of means of HPV-E2/E6 (p=0.16). In particular, HPV-E2/E6 of CIN2/3 (mean, 0.52) and CC (mean, 0.38) specimens were significantly lower than normal (mean, 1.14) or graded as CIN1 (mean, 1.01) (p<0.05). Furthermore, HPV-E2/E6 of CIN2/3 and CC specimens were significantly different (p<0.05). The relation between HPV-E2/E6 and POU5F1B with cytology was summarized in Figure 1C and D. It revealed that HPV-E2/E6 decreased significantly according to the development of the cytology with a higher ASCUS group, and POU5F1B expression increased significantly in the ASCUS group and higher ASCUS group.
The Physical Status of HPV Integration in Cytological Samples
The results of the physical status of HPV integration in 248samples revealed that the proportion of episome, mixed, and fully integrated state was 22.58%, 75.40%, and 2.02%, respectively (Figure 2A). The episomal status of HPV was found in 62.3% (33 of 53) of normal pathology but 1.9% (1 of 54) in SCC, whereas the fully integrated form of HPV was noted in 7.48% (4 of 54) of SCC but not found in normal pathology and CIN1.
Prediction of HPV-E2/E6 and POU5F1B for ≥CIN2
To predict CIN2+ lesions, ROC analyses of HPV-E2/E6 and POU5F1B mRNA were performed. HPV-E2/E6 and POU5F1B mRNA were evaluated individually (Figure 2A). We observed that AUC for POU5F1B mRNA (0.9058) was higher than that for HPV-E2/E6 (0.8983) (Figure 2B). Also, an optimal cut-off of POU5F1B mRNA was 1.0310, and an optimal cut-off of HPV-E2/E6 was 0.6471. The sensitivity of HPV-E2/E6 for women with CIN2+ was 80.35%, and specificity was 88.79%. The sensitivity and specificity of the combination of POU5F1B mRNA in the differential diagnosis of CIN2+ was 82.98% and 90.65%, respectively (Table 2). The PPV of the POU5F1B mRNA was significantly higher than HPV-E2/E6 (92.13% vs77.87%). There are similar results in the CIN3+.
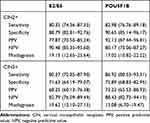 |
Table 2 Diagnostic Accuracy of the Rate of E2/E6 and POU5F1B for the Detection of CIN 2+ and CIN 3+ |
HPV-E2/E6 and POU5F1B is a Predictive Factor for the Detection of CIN 2+
As shown in Table 3, the independent factors associated with the diagnosis of high-grade CIN were identified in the multiple logistic regressions. It is demonstrated that the positivity for POU5F1B had the highest OR (OR= 16.84; 95% CI (8.00–35.46)), as well as the following: HPV-E2/E6 (OR = 3.43; 95% CI (1.07–9.53)) and TCT (OR = 1.72; 95% (1.46–2.04)).
 |
Table 3 Independent Predictors for Detection of CIN2+ Lesions |
Discussion
This study indicated that cervical cytology samples with over-expression of POU5F1B and a decreased HPV-E2/E6 showed significant association with CIN2+. Hence, our study may provide information with a new and possible biomarker to predict the pathogenesis and development of CIN2+ with fewer invasive methods.
Co-test screening with cytology and HPV test has been routinely used for cervical screening. However, the subjective interpretation of cytology is associated with a high degree of variability,23 which depends on the quality of the laboratory, experience of the cytologist, adequacy of the sample, and technique of fixation.24 It is reported that the sensitivity of HR-HPV testing is higher, and the negative predictive value (NPV) is better.25 HPV detection needs to balance clinical sensitivity and specificity and maximizes the protection of low-risk populations and discrimination of high-risk groups but avoids over-treatment and causing too much anxiety. This study aims to evaluate the biomarker concerning the HPV integration to predict the CIN2+.
In this study, 78.50% >ASC-US showed CIN2+, which was higher than that reported in our previous study.26 Higher progression for CIN2+ among >ASC-US may be explained by the effect of specific HPV genotypes such as HPV16 during infection. Moreover, of all HR-HPV genotypes, HPV-16 showed the strongest oncogenic capacity for cervical cancer development. Similarly, with our results, many studies reported that HPV-16 was significantly associated with a higher incidence of CIN2/3 in LSIL.27
HPV-16 persistent infection has been attributed partially to its oncogenic potency and is proposed to be regarded as a reliable marker for cervical precancerous lesion progression.28 Although the mechanism that causes HPV-16, persistent infection is not clear, it has been associated with HPV integration into the human genome.29 HR-HPV E2, E6 and E7 proteins play an important role in the suppressing and activating of HPV promoters.30,31 The expression levels of these proteins can affect HPV integration.32 The E2 protein plays various roles, such as promoting apoptosis,33 causing DNA breaks and chromosomal instability during mitosis9 and inhibiting the expression of E6 and E7 proteins.34,35 HPV E6 and E7 genes are transcriptions start sites for most HPV types, and they play a key role in the viral transformation and cell carcinogenesis. A previous study has pointed out that HPV integration results in deleting of the open reading frame (ORF) of the E2 gene and releases its inhibitory on E6 and E7gene.36 The elimination of E2 expression leads to augmented transcription of E6 and E7 oncogenes and is thought to confer a selective growth advantage to the infected cell, which presented the full integrated state. In a word, the function of E2 seems to depend on their relative ratio to E6. Thus, determining of the relative quantities of E2 genes (or PCR products) and their respective rates to E6 could estimate the HPV integration degree. Therefore, the information about the level of integration of HPV DNA with a host genome could be important and probably useful in the prognosis of cervical cancer’s progression and outcome.
This study demonstrated that HPV-E2/E6 evaluated by qPCR with the cervical cytological specimen is predictive of CIN2+ and allows discrimination of cancer from cervical precursors (Figure 1). We also found that HPV-E2/E6 had an optimal cut-off of 0.6471 to predict the CIN2+. Thus, the measurement of HPV-E2/E6, which represents the integration status of HPV16 in cervical cancer, may be useful for normal and low-grade lesions (CIN1) from high-grade lesions (CIN2+). It showed that HPV16-E2/E6 was significantly distinct according to the severity of cervical lesions and was regarded as a surrogate marker for HPV integration in cervical tissues. In accordance with our results, Cricca M and Lorenzi A also revealed similar conclusions.12,15 As we had known, it takes a long process from the HPV infection to the occurrence of cervical lesions, so the HPV integration status from the episome to the fully integrated is a dynamic process. However, currently, there is no consensus to distinguishing the status of the episome, mixed and fully integrated. Yoshinouchi M defined HPV-E2/E6 of 1 as “episome state,” whereas that is ranging from >0 to <1 as “mixed state”; HPV-E2/E6 of 0 as “fully integrated state”.14 Based on the Manawapat A,s result, HPV-E2/E6 of 1 is regarded as “episome state,” whereas that is ranging from >0 to <1 is considered as a “mixed state”; HPV-E2/E6 of 0 indicated “fully integrated state”.37
Recently, Hu et al.,7 using sequencing, reported frequent HPV integration sites in genes such as POU5F1B. So we hypothesis that POU5F1B can be used as an auxiliary indicator with HPV-E2/E6 to predict the CIN2+lesions. POU5F1B is involved in many important biological processes. Multiple studies have shown that POU5F1B plays a role as a tumor oncogene in the progression of various cancers. Bellanger S et al38 revealed that POU5F1B was amplified in gastric cancer and promoted the invasion phenotype of gastric cancer cells. Steger G et al39 found that the expression of POU5F1B was significantly up-regulated in human hepatocellular carcinoma tissues and promoted the proliferation of hepatocellular carcinoma by activating the AKT gene. The mechanism of POU5F1B is not clear. Senapati R et al40 hypothesized that POU5F1B might be used as a microRNA sponge to competitively regulate the microRNA of OCT4A by regulating the expression of OCT4 protein. In our study, we demonstrated that POU5F1B mRNA was significantly increased with the development of the cervical lesions, especially in the CIN2+. And it is an optimal cut-off of 1.0310 to predict the CIN2+. What is more, the sensitivity, specificity and PPV are superior to HPV E2/E6 to predict the CIN2+/CIN3+ lesions. Furthermore, the POU5F1B has the highest OR (16.84) (95% CI 8.00–35.46) using multiple logistic regressions to detect CIN 2+.
As a result of the continuous efforts to find cervical markers, p16 immunostaining positivity and an increase in Ki-67 expression may predict a higher risk progression in low-grade lesions.41,42 However, the indirect correlations of the combined markers have limitations to explain the progression or regression of cervical lesions. To solve this limitation, we utilized the expression of POU5F1B, which is the most frequent HPV integration sites in POU5F1B genes when HPV integration into the host genome.
As we knew, these are a few studies to test and verify the utility of the viral marker of HPV integration. We utilized POU5F1B mRNA and integration methods such as HPV-E2/E6 for the diagnosis of CIN2+ lesions. The accuracy of the identification of CIN2+-was increased in the POU5F1B mRNA versus measurement of HPV-E2/E6 (AUC=0.9058 vs AUC=0.8983). There are some limitations to our research. First, the size of the specimens was not big enough. For a more accurate evaluation, increasing the sample size may be necessary for future studies. Second, in our study, we did not further study the mechanism of the POU5F1B of promoting the development of cervical lesions, which is worth further studying.
In conclusion, our results demonstrate that POU5F1B expression increased, and HPV-E2/E6 decreased in cervical cytology are strongly related to a higher grade of cervical lesions. We advocate cervical cytology from non-invasive procedures and combined measurement of POU5F1B and HPV-E2/E6 as a suitable method to predict CIN2+. Our results may offer a sound basis for the accurate cytological diagnosis of cervical pre-malignancy and cancer in future transitionally research.
Ethics Approval and Consent to Participate
The study was approved by the Hospital Ethics Committee (FMCH2017J01232) and complied with the Declaration of Helsinki. All individuals participating in this study provided written informed consent.
Acknowledgments
The authors want to thank the Fujian Province Cervical Lesions Screening Cohorts Investigators for planning and conducting the trial and providing the biological specimens and data to the present study. Above all, they are grateful to the patients who made this study possible.
Author Contributions
All authors contributed to data analysis, drafting or revising the article, have agreed on the journal to which the article will be submitted, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Funding
The study was supported by grants from the Fujian Provincial Maternity and Children’s Hospital Technology Innovation Project (grant no. YCXM-19-01) and Fujian Provincial Health and Family Planning Commission Innovation Project (2019-CX-7).
Disclosure
The authors declare that they have no competing interests.
References
1. Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68(6):394–424. doi:10.3322/caac.21492
2. Chen W, Zheng R, Baade PD, et al. Cancer statistics in China, 2015. CA Cancer J Clin. 2016;66(2):115–132. doi:10.3322/caac.21338
3. Muñoz N, Bosch FX, de Sanjosé S, et al. Epidemiologic classification of human papillomavirus types associated with cervical cancer. N Engl J Med. 2003;348(6):518–527. doi:10.1056/NEJMoa021641
4. Bouvard V, Baan R. A review of human carcinogens—part B: biological agents. Lancet Oncol. 2009;10(4):321–322. doi:10.1016/S1470-2045(09)70096-8
5. Villiers EM, Fauquet C, Broker TR, Bernard HU, Hausen H. Classification of papillomaviruses. Virology. 2004;324(1):17–27. doi:10.1016/j.virol.2004.03.033
6. Sasagawa T, Takagi H, Makinoda S. Immune responses against human papillomavirus (HPV) infection and evasion of host defense in cervical cancer. J Infect Chemother. 2012;18(6):807–815. doi:10.1007/s10156-012-0485-5
7. Hu Z, Zhu D, Wang W, et al. Genome-wide profiling of HPV integration in cervical cancer identifies clustered genomic hot spots and a potential microhomology-mediated integration mechanism. Nat Genet. 2015;47(2):158–163. doi:10.1038/ng.3178
8. McNicol P, Paraskevas M, Guijon F. Variability of polymerase chain reaction-based detection of human papillomavirus DNA is associated with the composition of vaginal microbial flora. J Med Virol. 1994;43(2):194–200. doi:10.1002/jmv.1890430218
9. Blachon S, Bellanger S, Demeret C, Thierry F. Nucleo-cytoplasmic shuttling of high risk human Papillomavirus E2 proteins induces apoptosis. J Biol Chem. 2005;280(43):36088–36098. doi:10.1074/jbc.M505138200
10. Schneider-Maunoury S, Croissant O, Orth G. Integration of human papillomavirus type 16 DNA sequences: a possible early event in the progression of genital tumors. J Virol. 1987;61(10):3295–3298. doi:10.1128/JVI.61.10.3295-3298.1987
11. Dyson N, Howley PM, Münger K, Harlow E. The human papilloma virus-16 E7 oncoprotein is able to bind to the retinoblastoma gene product. Science. 1989;243(4893):934–937. doi:10.1126/science.2537532
12. Cricca M, Morselli-Labate AM, Venturoli S, et al. Viral DNA load, physical status and E2/E6 ratio as markers to grade HPV16 positive women for high-grade cervical lesions. Gynecol Oncol. 2007;106(3):549–557. doi:10.1016/j.ygyno.2007.05.004
13. Lukaszuk K, Liss J, Wozniak I, Emerich J, Wójcikowski C. Human papillomavirus type 16 status in cervical carcinoma cell DNA assayed by multiplex PCR. J Clin Microbiol. 2003;41(2):608–612. doi:10.1128/JCM.41.2.608-612.2003
14. Gradíssimo Oliveira A, Delgado C, Verdasca N, Pista A. Prognostic value of human papillomavirus types 16 and 18 DNA physical status in cervical intraepithelial neoplasia. Clin Microbiol Infect. 2013;19(10):E447–50. doi:10.1111/1469-0691.12233
15. Lorenzi A, Rautava J, Kero K, et al. Physical state and copy numbers of HPV16 in oral asymptomatic infections that persisted or cleared during the 6-year follow-up. J Gen Virol. 2017;98(4):681–689. doi:10.1099/jgv.0.000710
16. Panagopoulos I, Möller E, Collin A, Mertens F. The POU5F1P1 pseudogene encodes a putative protein similar to POU5F1 isoform 1. Oncol Rep. 2008;20(5):1029–1033.
17. Zhao S, Yuan Q, Hao H, et al. Expression of OCT4 pseudogenes in human tumours: lessons from glioma and breast carcinoma. J Pathol. 2011;223(5):672–682. doi:10.1002/path.2827
18. Kastler S, Honold L, Luedeke M, et al. POU5F1P1, a putative cancer susceptibility gene, is overexpressed in prostatic carcinoma. Prostate. 2010;70(6):666–674.
19. Wang CC, Huai L, Zhang CP. Study on expression of PTEN gene and its pseudogene PTENP1 in acute leukemia and correlation between them. Chin J Hematol. 2012;33(11):896–901.
20. Scarola M, Comisso E, Pascolo R, et al. Epigenetic silencing of Oct4 by a complex containing SUV39H1 and Oct4 pseudogene lncRNA. Nat Commun. 2015;6:7631. doi:10.1038/ncomms8631
21. Chen L, Sun MJ, Shi HY, He Q, Liu DG. Association of human papillomavirus L1 capsid protein with koilocytosis, expression of p16, and Ki-67, and its potential as a prognostic marker for cervical intraepithelial neoplasia. Anal Quant Cytopathol Histpathol. 2013;35(3):139–145.
22. Waxman AG, Chelmow D, Darragh TM, Lawson H, Moscicki AB. Revised terminology for cervical histopathology and its implications for management of high-grade squamous intraepithelial lesions of the cervix. Obstet Gynecol. 2012;120(6):1465–1471. doi:10.1097/AOG.0b013e31827001d5
23. Verma I, Jain V, Kaur T. Application of bethesda system for cervical cytology in unhealthy cervix. J Clin Diagn Res. 2014;8(9):OC26–OC30.
24. Sun P, Song Y, Ruan G, et al. Clinical validation of the PCR-reverse dot blot human papillomavirus genotyping test in cervical lesions from Chinese women in the Fujian province: a hospital-based population study. J Gynecol Oncol. 2017;28(5):e50. doi:10.3802/jgo.2017.28.e50
25. Reich O, Regauer S, Marth C, et al. Precancerous lesions of the cervix, vulva and vagina according to the 2014 WHO classification of tumors of the female genital tract. Geburtshilfe Frauenheilkd. 2015;75(10):1018–1020. doi:10.1055/s-0035-1558052
26. Yoshinouchi M, Hongo A, Nakamura K, et al. Analysis by multiplex PCR of the physical status of human papillomavirus type 16 DNA in cervical cancers. J Clin Microbiol. 1999;37(11):3514–3517. doi:10.1128/JCM.37.11.3514-3517.1999
27. Bhatla N, Maheswari ND. HPV screening for cervical cancer in rural India: do we have an answer? Natl Med J India. 2009;22(4):183–184.
28. Soost HJ, Lange HJ, Lehmacher W, Ruffingkullmann B. The validation of cervical cytology. sensitivity, specificity and predictive values. Acta Cytol. 1991;35(1):8.
29. Zazove P, Reed BD, Gregoire L, Ferenczy A, Gorenflo DW, Lancaster WD. Low false-negative rate of PCR analysis for detecting human papillomavirus-related cervical lesions. J Clin Microbiol. 1998;36(9):2708–2713. doi:10.1128/JCM.36.9.2708-2713.1998
30. Kang Y, Sun P, Mao X, Dong B, Ruan G, Chen L. PCR-reverse dot blot human papillomavirus genotyping as a primary screening test for cervical cancer in a hospital-based cohort. J Gynecol Oncol. 2019;30(3):e29. doi:10.3802/jgo.2019.30.e29
31. Khan MJ, Castle PE, Lorincz AT, et al. The elevated 10-year risk of cervical precancer and cancer in women with human papillomavirus (HPV) type 16 or 18 and the possible utility of type-specific HPV testing in clinical practice. J Natl Cancer Inst. 2005;97(14):1072–1079. doi:10.1093/jnci/dji187
32. Schiffman M, Herrero R, Desalle R, et al. The carcinogenicity of human papillomavirus types reflects viral evolution. Virology. 2005;337(1):76–84. doi:10.1016/j.virol.2005.04.002
33. Kulmala SM, Syrjänen SM, Gyllensten UB, et al. Early integration of high copy HPV16 detectable in women with normal and low grade cervical cytology and histology. J Clin Pathol. 2006;59(5):513–517. doi:10.1136/jcp.2004.024570
34. Lin BY, Makhov AM, Griffith JD, Broker TR, Chow LT. Chaperone proteins abrogate inhibition of the human papillomavirus (HPV) E1 replicative helicase by the HPV E2 protein. Mol Cell Biol. 2002;22(18):6592–6604. doi:10.1128/MCB.22.18.6592-6604.2002
35. Woo YL, van den Hende M, Sterling JC, et al. A prospective study on the natural course of low-grade squamous intraepithelial lesions and the presence of HPV16 E2-, E6- and E7-specific T-cell responses. Int J Cancer. 2010;126(1):133–141. doi:10.1002/ijc.24804
36. van Poelgeest MI, Nijhuis ER, Kwappenberg KM, et al. Distinct regulation and impact of type 1 T-cell immunity against HPV16 L1, E2 and E6 antigens during HPV16-induced cervical infection and neoplasia. Int J Cancer. 2006;118(3):675–683. doi:10.1002/ijc.21394
37. Chojnacki M, Melendy T. The HPV E2 transcriptional transactivation protein stimulates cellular DNA polymerase epsilon. Viruses. 2018;10(6):321. doi:10.3390/v10060321
38. Bellanger S, Tan CL, Nei W, He PP, Thierry F. The human papillomavirus type 18 E2 protein is a cell cycle-dependent target of the SCFSkp2 ubiquitin ligase. J Virol. 2010;84(1):437–444. doi:10.1128/JVI.01162-09
39. Steger G, Corbach S. Dose-dependent regulation of the early promoter of human papillomavirus type 18 by the viral E2 protein. J Virol. 1997;71(1):50–58. doi:10.1128/JVI.71.1.50-58.1997
40. Senapati R, Senapati NN, Dwibedi B. Molecular mechanisms of HPV mediated neoplastic progression. Infect Agent Cancer. 2016;11:59.
41. Manawapat A, Stubenrauch F, Russ R, Munk C, Kjaer SK, Iftner T. Physical state and viral load as predictive biomarkers for persistence and progression of HPV16-positive cervical lesions: results from a population based long-term prospective cohort study. Am J Cancer Res. 2012;2(2):192–203.
42. Hayashi H, Arao T, Togashi Y, et al. The OCT4 pseudogene POU5F1B is amplified and promotes an aggressive phenotype in gastric cancer. Oncogene. 2015;34(2):199–208.
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


