Back to Journals » Therapeutics and Clinical Risk Management » Volume 12
How does hospitalization affect continuity of drug therapy: an exploratory study
Authors Blozik E , Signorell A, Reich O
Received 25 March 2016
Accepted for publication 11 June 2016
Published 22 August 2016 Volume 2016:12 Pages 1277—1283
DOI https://doi.org/10.2147/TCRM.S109214
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Garry Walsh
Eva Blozik,1–3 Andri Signorell,1 Oliver Reich1
1Department of Health Sciences, Helsana Group, Zürich, Switzerland; 2Department of Primary Medical Care, University Medical Centre Hamburg-Eppendorf, Hamburg, 3Department of Medicine, University Medical Centre Freiburg, Freiburg im Breisgau, Germany
Introduction: Transitions between different levels of health care, such as hospital admission and discharge, pose a significant threat to the quality and continuity of medication therapy. This study aims to explore the role of hospitalization on medication changes as patients are transferred from and back to ambulatory care.
Methods: Secondary analysis of claims data from Swiss residents with basic health insurance at the Helsana Group was performed. We evaluated medication invoices of patients who were hospitalized in a Swiss private hospital group in the year 2013. Medication changes were defined as discontinuation, new prescription, or change in the Anatomical Therapeutic Chemical (ATC) Classification System level 4, which is equivalent to a change in the chemical/therapeutic/pharmacological subgroup. Multiple Poisson regression analysis was applied to evaluate whether medication change was predicted by socioeconomic or clinical patient characteristics or by a system factor (physician dispensing of medication allowed in canton of residence).
Results: We investigated a total of 10,123 hospitalized patients, among whom a mean number of 3.85 (median 3.00) changes were identified. Change most frequently affected antihypertensives, analgesics, and antirheumatics. If patients were enrolled in a managed care plan, they were less likely to undergo changes. If a patient resided in a canton, in which physicians were allowed to dispense medication directly, the patient was more likely to experience change.
Conclusion: There is considerable change in medication when patients shift between ambulatory and inpatient health care levels. This interruption of medication continuity is in part desirable as it responds to clinical needs. However, we hypothesize that there is also a significant proportion of change due to unwarranted factors such as financial incentives for change of products.
Keywords: medication, prescribing, safety, hospital, admission, discharge
Background
Transitions between different levels of health care, such as hospital admission and discharge, pose a significant threat to the quality and continuity of medication therapy. Previous research has shown that extensive changes in patients’ drug regimens were made during their hospital stays, and almost equally extensive changes were undertaken after the patients were transferred back into the care of their general practitioners.1–3 In a study based on a prescription database, it was found that hospitalization markedly influenced medical therapy in ambulatory care.4 When medication regimens are constantly modified and updated associated with a patient’s hospitalization, these modifications might increase the risk for nonadherence, polypharmacy, cost, and poor outcomes among elderly patients.5–7
This study aims to explore medication changes related to hospitalizations within the Swiss health care setting. Using Swiss health insurance claims data, medication invoices can be tracked as patients are transferred from and back to ambulatory care. This study describes medication changes by relevant therapeutic subgroups. Furthermore, we explore socioeconomic, clinical, and health system factors that may contribute to medication changes.
Methods
Data source and study population
This is a retrospective analysis of anonymized individual-level health care claims data from the leading health insurance group (Helsana Group) in Switzerland currently covering ~1.2 million individuals with nationwide mandatory health insurance coverage (~15% of Swiss residents). The core business of the Helsana Group is basic (compulsory) health insurance according to the Swiss Federal Health Insurance Act. Persons with basic health insurance insured with Helsana come from all regions of Switzerland and cover all socioeconomic and clinical groups. We performed a secondary analysis including all adult persons who were hospitalized in a Swiss private hospital group in the year 2013 and who were enrolled with Helsana basic health insurance in the 6 months preceding and following the hospitalization. The private hospital group includes 16 private hospitals distributed across the country but with a concentration of hospital beds in the canton of Zürich. These hospitals were all included in the hospital list of the canton where the hospital is situated, so that all insured persons with basic health insurance had primary access to those hospitals.
The system of mandatory health insurance in Switzerland
All people residing in Switzerland are required to purchase basic health insurance on a private market of health insurance, which is regulated by federal bodies. In order to protect those with poor health, health insurers are obliged to offer basic insurance to everyone and to charge the same premium to every individual irrespective of age or health status. The basic health insurance package includes all ambulatory or hospital medical treatment deemed appropriate, medically effective, and cost-effective. Supplementary hospital insurance in Switzerland is purchased if individuals wish further comfort of a semiprivate or private ward or treatment in another canton for personal reasons. Basic obligatory health insurance covers the expenses of public and private hospitals when they are listed on the cantonal list of hospitals published as defined by the canton of residence.
However, the insured person pays a part of the cost of health care in the form of an annual deductible cost (called a “franchise”) ranging from CHF 300 to a maximum of CHF 2,500 as chosen by the insured person and a charge of 10% of the costs up to CHF 700 per year. Currently, there are 57 insurance companies providing basic health coverage in Switzerland, and they offer a range of different premiums and types of health plans from which Swiss residents are free to choose.8
Managed care models are alternative insurance models for mandatory health insurance under which the insured persons agree to always first consult a specific type of health care provider (ie, a group practice, a fixed family doctor, or a telemedicine center). The aim of the models is to increase coordination of health care provision, to support networking of health care providers, and to reduce inefficiency. Depending on the model, insured persons can benefit from a premium reduction of up to 25%.9
Measurements
Characteristics of our sample comprised age, sex, health plan coverage (high deductible class, ie, 1,500, 2,000, or 2,500 as compared to the standard deductible of 300 or 500 Swiss francs [CHF], managed care option, and availability of supplementary private hospital insurance). We explored medication invoices in four-quarter years related to the first hospitalization of an individual in 2013: Q1 (pre-prehospitalization quarter year), Q2 (prehospitalization quarter year), Q3 (posthospitalization quarter year), and Q4 (quarter year following posthospitalization). We considered all medications reimbursed, irrespective of whether they were supplied by a community pharmacy, a mail-order pharmacy, or a physician if physician dispensing (PD) was allowed. As a prerequisite for reimbursement by basic health insurance, medications had to be prescribed by a physician. This means that over-the-counter medications are not included in our database.
We explored medication change between Q2 and Q3. Medication change was defined as discontinuation, new prescription, or change in the Anatomical Therapeutic Chemical (ATC) Classification System level 4, which is equivalent to a change in the chemical/therapeutic/pharmacological subgroup.10 Neither the changes in the doses of drugs nor the substitution of a generic drug was recorded as a change because the available data format of medication invoices was limited with respect to these parameters. This means that the definition of change in this study did not include substitutions of expensive drugs by identical, less costly medical compounds (ie, generic drugs). Temporary drug changes during hospital stays were not recorded, because our aim was to investigate the follow-up of the medications after discharge. Rehospitalizations of the same year were not included, so that an individual was included not more than once.
In Switzerland, physicians (irrespective of their specialization) dispense drugs directly to their patients (PD), which is allowed in some cantons but prohibited in others.11 We checked whether an individual resided in a canton, in which PD was allowed (Basel Landschaft, Solothurn, Appenzell Innerrhoden, Appenzell Ausserrhoden, Glarus, Luzern, Obwalden, Nidwalden, Sankt Gallen, Schwyz, Thurgau, Uri, and Zug) to include this system factor in the analysis.
Statistical analysis
Descriptive statistics were used to describe the socioeconomic characteristics of the study population. The sum of all medication changes was calculated, differentiated for discontinuations (negative numbers for change), new prescriptions (positive numbers for change), and total change (absolute sum of negative and positive changes). Medication information was clustered using subgroups of medications highly relevant for primary care.12 These subgroups were analgesics (ATC code N02), antibiotics (J01), antidiabetics (A10), antihypertensives including diuretics, beta blockers, calcium channel blockers, renin–angiotensin antagonists (C02, C03, C07, C08, C09), antirheumatics (M01, M02), antithrombotics (B01), cardiac therapy (C01), lipid lowering drugs (C10), drugs for obstructive airway diseases (R03), drugs for treatment of bone diseases (M05), drugs for acid-related disorders including antidiarrheals, intestinal anti-inflammatory/anti-infective agents (A02, A07), psychoanaleptics (N06), and psycholeptics (N05).
Multiple Poisson regression analysis was applied to evaluate whether medication change (total change) was predicted by socioeconomic or clinical patient characteristics or by a system factor (PD allowed in canton of residence). Socioeconomic factors included age, sex, high annual deductible, membership in a managed care plan, and availability of supplementary private hospital insurance. The number of ATC codes represented clinical factors in the following two ways: the number of ATC in Q1 (pre-prehospitalization quarter year) was used as a marker for the baseline morbidity of the patient and the number of ATC in Q2 (prehospitalization quarter year) reflected the acute burden of disease related to the hospitalization. To consider any other (cultural) differences between the patient populations across the Swiss cantons, canton of residence was adjusted in the analysis. A two-sided P-value <0.05 was considered statistically significant. All statistical analyses were performed using R, Version 3.2.0 (R Foundation for Statistical Computing, Vienna, Austria).
Ethics
The analysis complied with the Swiss Federal Law on data protection. All data were anonymized and de-identified prior to the performed analysis to protect the privacy of patients, physicians, and hospitals. According to the national ethical and legal regulation, an ethical approval was not needed because the data were retrospective, pre-existing, and de-identified. Since data was anonymized, no consent of patients was required. Therefore, the authors deemed that ethical approval and consent weren’t necessary.
Results
Sample
We analyzed a total of 10,123 hospitalized persons. Of those 5,908 (58.4%) were female. The analytic study sample had a mean age of 63.3 (standard deviation 16.8 years). The majority of persons chose the lowest (obligatory) deductible of 300 CHF (N=6,374, 63%). About half of the analyzed persons purchased supplementary hospital insurance including semiprivate or private ward or treatment in another canton not covered by basic insurance (4,954, 48.9%). In all, 41.6% (4,215) persons were members of a managed care insurance plan that trades off lower premiums for reduced choice and more care coordination.
Medications
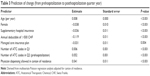
Medication invoices were highly prevalent in hospitalized persons (8,687/10,123, 86%). The mean number of different medications (ATC codes) started at 5.6 medications, peaked in the prehospitalization quarter year (6.8), slightly decreased in the posthospitalization quarter year (6.6), and then returned to its initial value in the quarter year following the posthospitalization period (Table 1).
  | Table 1 The number of ATC codes by quarter year (N=10,123) |
Change
Hospitalized persons experienced a mean number of 3.85 changes. Of 10,123 analyzed persons, only 774 (7.6%) did not have any change between the pre- and the posthospitalization quarter year.
Table 2 depicts use and changes in medication in the posthospitalization quarter as compared to the prehospitalization quarter year. Results are stratified for user status in the prehospitalization quarter year. The variance across medication subgroups was relatively low. Persons who had drugs for treatment of bone diseases or obstructive airway diseases were slightly more likely to receive more drugs than other patient subgroups, such as persons receiving antirheumatics or antihypertensives.
  | Table 2 Use and change of medication in the posthospitalization quarter year as compared to prehospitalization quarter year |
The mean number of additional medications persons received in Q3 as compared to Q2 was 2.03. New prescriptions most frequently included antihypertensives, analgesics, and antirheumatics. The number of additional medications in users and nonusers was approximately similar for analgesics, antirheumatics, and psycholeptics, which means that the probability for change in these subgroups was almost independent of preceding therapy with such substances. The number of additional medications in prior users was much higher than in nonusers for long-term therapies of chronic diseases, such as antidiabetics, cardiac therapy, antiasthmatics, and psychoanaleptics. For antithrombotics, statins/fibrates, and antacids, the number of additional medications was higher for prior nonusers as compared to prior users. The probability for prior nonusers to get new users of antidiabetics, cardiac therapy, antiasthmatics, and antiosteoporotics was low.
Users of analgesics, antibiotics, antirheumatics, and cardiac therapy had the highest chance for discontinuation of such medications. These subgroups correspond to those groups in which the highest total changes (absolute values of discontinuations and new prescriptions) were identified.
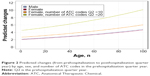
Figure 1 shows how the number of changes between Q2 and Q3 differs between younger adults and elderly persons. Change was more frequent in the elderly population in all but one medication subgroups (antirheumatics). For antihypertensives, antithrombotics, and psycholeptics, there is substantially more change in elderly as compared to younger adults.
  | Figure 1 Number of changes (from prehospitalization to posthospitalization quarter year) by age group and medication subgroup. |
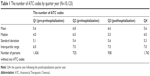
Prediction of change
Multivariate Poisson regression analysis revealed that the most important predictor of change is the number of ATC codes a person receives prior to the hospitalization (Table 3). Both the number of ATC codes in the prehospitalization quarter year (as a marker for severity of the current health problem leading to hospitalization) and the number of ATC codes in the pre-prehospitalization quarter year (as a marker of “baseline” morbidity) affect change independent from each other. However, the number of ATC codes in the prehospitalization quarter year showed the largest effect estimate: a coefficient of 0.052 means that every additional ATC codes a person received had a mean of 5.2% more changes. Thus, a person with ten medications had ~0.5 changes more than a person without medications. This is a small but clinically relevant figure. In contrast, the influence of the number of ATC codes in the pre-prehospitalization quarter year was only about one-tenth (0.006).
Socioeconomic wealth as measured by the availability of supplementary hospital insurance and high deductible class was both independently and inversely associated with change. Female patients were less likely to experience change than male patients. The probability of change increased with increasing age (0.008 changes with every year). This correlates with ~3.2 changes in a 70-year-old patient as compared to a 30-year-old patient.
The model of care provision also influenced the likelihood of change. If patients were enrolled in a managed care plan, they were less likely to undergo changes with the effect estimate of 3% being small although statistically significant. The probability of change was also influenced by the system level. If a person resided in a canton in which physicians were allowed to dispense medication directly, he or she experienced 4% additional medication changes.
To illustrate the clinical relevance of the results of the Poisson regression analysis, Figure 2 depicts predicted changes for men and women with comparable insurance status (both without managed care option, without supplementary hospital insurance, and low deductible) and comparable health status (five ATC both in the pre-pre- and in the prehospitalization quarter year), residing in a canton where PD of medication was allowed. For example, according to our estimation, men with 60 years of age undergo ~3.3 changes, women slightly less (3.2). The figure shows that the impact of number of ATC in the prehospitalization quarter year increases with increasing age. When a 60-year-old women experiences 4 changes, a 80-year-old women undergoes 4.7 changes when having ten ATC codes in the prehospitalization quarter year.
Discussion
There is considerable change in medication when patients shift between ambulatory and inpatient health care levels. This change can be quantified: hospitalized persons experience a mean number of 3.85 changes, and this phenomenon affects virtually all hospitalized patients.
In general, change is plausible and appropriate if it responds to clinical needs. If a person receives a large number of medications for therapy of multiple morbidities, it is more likely that a health problem leading to hospitalization requires medication change.
In addition, medication changes in response to an acute illness might be no longer relevant after stabilization in primary care. However, there is evidence suggesting that there is also a significant proportion of change due to unwarranted factors.
First, change was predicted by nonclinical patient characteristics. Change was less frequent in patients who purchased supplementary hospital insurance and who chose a high annual deductible. Both characteristics are markers for socioeconomic wealth which – when controlling for morbidity – should not be correlated with medication continuity. Our results suggest that there might be an unwarranted socioeconomic gradient related to the choice of medication.
Change was also more frequent in cantons, in which PD of medication was allowed. This is a clear indicator that financial incentives might trigger change of products, as clinical arguments for change are very likely to be evenly distributed across cantons irrespective of whether or not the cantons provide the opportunity for physicians in private practices to sell medication. Previous studies indicated that PD is associated with increased cost and quality deficits.11,13,14 This study provides further evidence that PD may lead to undesirable effects.
In addition, change was less frequent in patients enrolled in managed care health plans. Those models are intended to reduce inefficiency and to increase continuity of care, and this claim is supported by increased medication continuity in persons enrolled in managed care plans. Previous studies from Switzerland also showed positive effects of managed care in the context of the Swiss health care system on quality of care and outcomes.15 Our results support previous findings and add a new element of evidence.
Change is considerable in all medication subgroups. This is remarkable especially for those therapies with lifelong need for treatment, such as antidiabetics, or drugs for treatment of bone diseases. Given the long-term nature of these treatments, it is very unlikely that the health status of a large proportion of hospitalized patients suggests clinical need for a change in the medical management of their chronic condition. It seems to be more realistic that nonclinical factors contribute to a considerable proportion of changes. Such nonclinical factors may be poor communication between hospitals and general practitioners,1,16 different availability and pricing of medications in the hospital setting, for example, discounting of certain drugs that would be more expensive when prescribed in the ambulatory setting,17 different prescribing habits, attitudes, preferences and affinity toward evidence-based prescribing,18 or different management and different awareness of risks related to multimorbidity and polypharmacy.19,20
Several limitations have to be considered when interpreting the results of this study. First, the study is based on persons who were hospitalized in a large private hospital group. Therefore, the frequency of medication changes may be different from other hospitalized patient groups. However, we controlled for the availability of supplementary hospital insurance which grants access to extra services not covered by the basic obligatory health insurance package. Second, health insurance claims data from a single health insurer were used. This may reduce generalizability of our results to the total population of Switzerland even if Helsana is the largest health insurance in Switzerland. Third, we may have missed a small proportion of medications as our database does not include over-the-counter medications. Moreover, invoices from persons whose annual health care expenses did not exceed the annual deductible may have been missed. However, internal analyses done by Swiss health insurance companies showed that this proportion is ~1.5% of invoices, so that a potential selection bias is probably very small.
This study focused on groups of medications and the frequency of medication changes within these groups. Further studies are needed to verify the present findings in subgroups of patients as opposed to subgroups of medications. For example, it should be explored whether change associated with socioeconomic or system factors is present across different patient populations such as patients hospitalized in medical versus surgical wards or patients with certain groups of diagnoses, and what factors are associated with a high versus low probability of change. In addition, medication continuity should be explored including data from the hospital setting so that medication changes during the hospitalization can be tracked. This may be helpful to quantify the proportion of unwarranted versus appropriate medication change. Future studies are needed to explore the effects of change on health service utilization, readmission rates, and the risk of overuse, underuse, or misuse of certain medications.
Disclosure
The authors report no conflicts of interest in this work.
References
Viktil KK, Blix HS, Eek AK, Davies MN, Moger TA, Reikvam A. How are drug regimen changes during hospitalisation handled after discharge: a cohort study. BMJ Open. 2012;2(6):e001461. | ||
Gamble JM, Hall JJ, Marrie TJ, Sadowski CA, Majumdar SR, Eurich DT. Medication transitions and polypharmacy in older adults following acute care. Ther Clin Risk Manag. 2014;10:189–196. | ||
Himmel W, Kochen MM, Sorns U, Hummers-Pradier E. Drug changes at the interface between primary and secondary care. Int J Clin Pharmacol Ther. 2004;42(2):103–109. | ||
Grimmsmann T, Schwabe U, Himmel W. The influence of hospitalisation on drug prescription in primary care – a large-scale follow-up study. Eur J Clin Pharmacol. 2007;63(8):783–790. | ||
Mansur N, Weiss A, Beloosesky Y. Relationship of in-hospital medication modifications of elderly patients to postdischarge medications, adherence, and mortality. Ann Pharmacother. 2008;42(6):783–789. | ||
Mansur N, Weiss A, Hoffman A, Gruenewald T, Beloosesky Y. Continuity and adherence to long-term drug treatment by geriatric patients after hospital discharge: a prospective cohort study. Drugs Aging. 2008;25(10):861–870. | ||
Coleman EA. Falling through the cracks: challenges and opportunities for improving transitional care for persons with continuous complex care needs. J Am Geriatr Soc. 2003;51(4):549–555. | ||
Reich O, Wolffers F, Signorell A, Blozik E. Health care utilization and expenditures in persons receiving social assistance in 2012: evidence from Switzerland. Glob J Health Sci. 2014;7(4):1–11. | ||
Reich O, Rapold R, Flatscher-Thöni M. An empirical investigation of the efficiency effects of integrated care models in Switzerland. Int J Integr Care. 2012;12:e10. | ||
World Health Organization [webpage on the Internet]. ATC/DDD Index 2014 [online]. Available from: http://www.whocc.no/atc_ddd_index/. Accessed March 24, 2016. | ||
Blozik E, Rapold R, Reich O. Prescription of potentially inappropriate medication in older persons in Switzerland: does the dispensing channel make a difference? Risk Manag Healthc Policy. 2015;8:73–80. | ||
Petra Kaufmann-Kolle P, Riens B, Grün B, Kazmaier T. Qisa, Band D, Das Qualitätsindikatorensystem für die ambulante Versorgung, Pharmakotherapie, Qualitätsindikatoren für die Verordnung von Arzneimitteln. [Qisa. Quality indicators for ambulatory care. Pharmacotherapy. Quality indicators for the prescription of medications]. Göttingen: Aqua Institute; 2009. German. | ||
Beck K, Kunze U, Oggier W. Selbstdispensation: Kosten treibender oder Kosten dämpfender Faktor? [Physician dispensing: cost driving or cost limiting factor]. Manag Care. 2004;8:33–36. German. | ||
Reich O, Weins C, Schusterschitz C, Thöni M. Exploring the disparities of regional health care expenditures in Switzerland: some empirical evidence. Eur J Health Econ. 2012;13(2):193–202. | ||
Reich O, Rosemann T, Rapold R, Blozik E, Senn O. Potentially inappropriate medication use in older patients in Swiss managed care plans: prevalence, determinants and association with hospitalization. PLoS One. 2014;9(8):e105425. | ||
Johnson A, Sandford J, Tyndall J. Written and verbal information versus verbal information only for patients being discharged from acute hospital settings to home. Cochrane Database Syst Rev. 2003;4:CD003716. | ||
Cochrane RA, Mandal AR, Ledger-Scott M, Walker R. Changes in drug treatment after discharge from hospital in geriatric patients. BMJ. 1992;305(6855):694–696. | ||
Gamble JM, Hall JJ, Marrie TJ, Sadowski CA, Majumdar SR, Eurich DT. Medication transitions and polypharmacy in older adults following acute care. Ther Clin Risk Manag. 2014;10:189–196. | ||
Garcia-Caballos M, Ramos-Diaz F, Jimenez-Moleon JJ, Bueno-Cavanillas A. Drug-related problems in older people after hospital discharge and interventions to reduce them. Age Ageing. 2010;39(4):430–438. | ||
Corsonello A, Pedone C, Corica F, Incalzi RA. Polypharmacy in elderly patients at discharge from the acute care hospital. Ther Clin Risk Manag. 2007;3(1):197–203. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.