Back to Journals » Clinical Interventions in Aging » Volume 12
How do demographic transitions and public health policies affect patients with Parkinson’s disease in Brazil?
Authors Bovolenta TM , Felicio AC
Received 23 September 2016
Accepted for publication 19 November 2016
Published 25 January 2017 Volume 2017:12 Pages 197—205
DOI https://doi.org/10.2147/CIA.S123029
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Richard Walker
Tânia M Bovolenta, Andre C Felicio
R. Neurology Program, Hospital Israelita Albert Einstein, São Paulo, Brazil
Abstract: Brazil is currently experiencing a significant demographic transition characterized by a decrease in fertility rates and an exponential increase in the number of elderly citizens, which presents a special challenge for the health care professionals. More than other portions of the population, the elderly are most commonly affected by chronic diseases such as Parkinson’s disease. Policymakers contend that Brazil is reasonably well-prepared regarding elderly health care, with policies that aim to ensure the quality of life and the well-being of this portion of the population. However, what happens in practice falls short of what the Brazilian Constitution sets forth. Specifically, there is a clear contradiction between what the law recognizes as being a citizen’s rights and the implementation of guidelines. Because health financing in Brazil remains relatively low, the civil society tries to fill in the gaps as much as possible in the treatment of elderly patients suffering from chronic diseases such as Parkinson’s disease. In this review, we outline the current legislation in Brazil regarding the elderly and in particular, patients with Parkinson’s disease, in the context of a rapidly aging population.
Keywords: Parkinson’s disease, demographic transition, public health, health assistance financing
Introduction
The demographic transition in Brazil
Although it is little >500 years old and, therefore, young compared to the so-called “Old World”, Brazil can no longer be considered a “young” country, given its rapidly aging population.
Brazil is undergoing a significantly rapid demographic transition, and the average life expectancy is so high that a significant segment of the current population is expected to reach old age. In 1940, the elderly population (≥60 years) represented only 4.1% of Brazil’s population, and life expectancy at that time was 42.4 years. It is estimated that 13.8% and 33.7% of the population will reach the highest life expectancy by 2020 and 2060, respectively.1–3
This demographic transition can be traced to different factors, such as a reduction in fertility rates and an increased life expectancy. The increase in life expectancy is, in turn, due to social and economic development, as well as the improvement in basic sanitation, food, and education driven by the advancements in technology and medicine.4 Other probable contributors are epidemiological changes, such as a significant decrease in the number of infectious diseases5 and the growth of the labor market that occurred between 2002 and 2012. The period up to 2013 was characterized by significant socioeconomic growth among the least favored classes in Brazil.
In a 2013 population projection that incorporated data regarding mortality, fertility, and migration on national and regional levels, the Instituto Brasileiro de Geografia e Estatística (Brazilian Institute for Geography and Statistics) reported significantly reduced mortality rates nationwide, a life expectancy of 74.8 years for both sexes at birth, and an infant mortality rate of 15 deaths per 1,000 live births (compared to the life expectancy under 50 and 135 deaths per 1,000 live births in 1950).6
Brazil has seen an accelerated decline in its fertility levels since the 1970s. In the 1950s and 1960s, the average number of children per woman was ~6.2 (typical of an agrarian society with low urbanization and industrialization); in 2013, this number was 1.7, and it is estimated that the rate will drop as low as 1.5 by 2030.2,6 During the second half of the 20th century, Brazil experienced intense internal migration that brought large numbers of people from the most economically stagnant areas to the country’s more economically dynamic regions. However, this migratory pattern changed dramatically beginning in the 1980s, and states where people traditionally migrated to received fewer people, while other areas with migratory efflux began receiving a significant number of migrants.6 Together, these factors are clear contributors to the aforementioned rapid demographic transition.
It should be noted that the demographic transition occurs unevenly across Brazil’s vast territory. Due to its continental dimensions, Brazil’s different regions present different patterns of socioeconomic development and, thus, different aging patterns also. For example, the northern and northeastern regions present significantly higher fertility rates than do the southern, southeastern, and mid-western regions.
The population projection presented by the United Nations for Brazil has the shape of a pyramid in 1950 and a rectangle in 2100 when a decrease in birth and an increase in the number of adults and the elderly are predicted, beginning in 2015.7
A key issue associated with an aging population is the degree of dependence it creates within a community. The proportion of potentially economically inactive individuals (aged ≥60 years) directly affects the calibration of public policies, including money allotted to pensions as well as education and health care.8 As shown in the demographic transition projected to occur in Brazil from 2010 to 2050 (Figure 1), the growing aging population will require the urgent development of public policies addressing quality of life and health issues, which will undoubtedly create considerable burdens on the society.
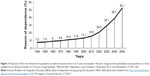  | Figure 1 Projection of the ratio between the population considered inactive (minors of 15 years and people >60 years of age) and the potentially active population, or those available for productive activities (15–59 years of age) between 1940 and 2050. Dependence ratio of elderly = (Population 60 or more/Population 15–59) ×100. |
In addition to tracing the evolution of a society’s economic dependence, this indicator also indicates the process of aging and rejuvenation. High values indicate that the productive portion of the population must support a high number of dependents (children, adolescents, and the elderly).8
Demographic transitions worldwide
In mid-2015, the world’s population reached the 7.3 billion mark, showing an increase of 1 billion people in the previous 12 years. Asia represents 60% of the world’s population, and China and India, with over 1 billion people each, are still the two most populous countries in the world, representing 19% and 18% of the global total, respectively. Some estimate that this growth will continue relatively uninterrupted, reaching 8.5 billion in 2030, then 11.2 billion in 2100, and eventually stabilizing or declining.9
As is the case for different regions across Brazil, differing degrees of development worldwide result in differences in aging across countries. In developed regions such as North America and Northern and Western Europe, the demographic transition occurred long after those regions acquired high standards of living and experienced reduced social and economic inequalities. This means that developed countries become rich and then become old. The opposite seems to be true for Latin American nations, which grow old before becoming rich. Fragile economies seem to undergo a highly compressed aging process within the contexts of increasing poverty and social and economic inequalities.10
In sum, there appear to be three types of demographic transition:
- Early transitions, such as those observed in Western European nations, where the transition began centuries ago and in a slow and gradual manner. Sweden and England, for example, took ~six decades to reduce their fertility levels by ~50%. France’s elderly population took over a century to increase from 7% to 14%.
- Late initiation, such as in Latin America and Caribbean countries, where this process started ~50 years ago, but at a more accelerated pace. Brazil reached the reduced fertility rates observed in Sweden and England in ~25 years and took only two decades to experience an increase in the elderly population similar to that of France.
- Countries that have not started their transition, such as the African nations, where the population is still young. Nine percent of the world’s population lives in countries with a high fertility rate, which include 19 African and 2 Asian countries.9–12
Parkinson’s disease
In the context of demographic transition
According to one study, in 2015, the number of individuals over 50 years old with Parkinson’s disease (PD) was between 4.1 and 4.6 million across 15 analyzed countries, including Brazil. Furthermore, the authors predicted that this number would more than double around 2030, reaching between 8.7 and 9.3 million.13 In-line with this, another study suggested that patients with PD will reach 7.1 million in the next 40 years in Europe, USA, and Canada.14
In Brazil, disclosure of PD is not compulsory; so, there are no official data on the actual number of patients with the disease. There is also a lack of adequate research studies in search of these numbers. One unofficial estimate suggests there are 220,000 cases nationwide, but a study in the state of Minas Gerais15 found a prevalence of 3.3% among the elderly aged ≥65 years. If we take this value as a reference and the available population data2 at the time of that study, we can infer that the number of PD cases nationwide may reach 630,000. This number, however, does not consider patients aged ≤64 years.
The significance of this information
There is currently no primary prevention available for PD, as its causes are not fully known, and there are, as yet, no biological markers or identifiable isolated risk factors to speak of the symptoms that may first appear about 7–10 years following the loss of 50%–70% of dopaminergic neurons within the substantia nigra in the mid-brain.16 Also, while there are patients with very light symptoms who have had PD for 20 years, others with only a few years of disease present advanced states of impairment on the Hoehn and Yahr scale (a modified scale that evaluates the stages of disability on a scale of 0–5, with 0 indicating no symptoms). Once PD has been diagnosed, secondary prevention uses medications that seek to alleviate motor and nonmotor symptoms as much as possible.
Patients treated in the Brazilian public health system (Sistema Único de Saúde [SUS])
As is true of most elderly patients with chronic diseases, PD patients require several regular medical visits, which, in turn, lead to relatively greater medication intake, complementary examinations, and hospitalizations. Brazilian law requires that PD patients be treated in specialized neurologic and/or geriatric services (tertiary health systems) and that they undergo periodic verifications to make sure they are correctly using their prescribed medications. In 2010, the number of specialized medical consultations (not only with neurologists) exceeded 85,000, along with an increase of 23.56% in the number of procedures performed and 12.52% in the availability of skilled professionals relative to 2007.17
Brazil has 5,570 municipalities and in September 2016, there were 1,919 high-complexity (tertiary) ambulatory centers in the country, with specialty in areas such as neurology and geriatrics. Of these, 547 were in Southeastern Brazil and 15 were teaching in hospitals run by supervised residents (seven of these also in Southeastern Brazil). During the same period, there were only 98 PD admissions recorded nationwide (55 of which were in the southeast), which clearly shows that PD is significantly underreported.18–20
As mentioned above, the number of studies on the use of health resources for PD in Brazil is extremely limited. However, another study conducted in Minas Gerais, one of Brazil’s largest states,21 provides some valuable insight. It should be noted, however, that the study is somewhat biased, as it was conducted in a reference center for neurologic disorders. Nonetheless, according to that study, the most common cause for utilizing health care resources was a scheduled ambulatory visit at a neurology clinic. The mean number of visits per patient per year was 3.8, and those with the greatest number of visits were patients with a stage 2 Hoehn and Yahr score (mean score of 4.7). The authors of that study also observed that the pattern of helath care resource utilization in Brazilian PD patients was mainly influenced by functional status, the presence of comorbid conditions, and socioeconomical factors.
PD patients require the care of a multidisciplinary team, as physiotherapy, speech therapy, and nutrition are critical for patients who quite often die from respiratory problems such as dysphagia. Only 45.8% of the patients in the Minas Gerais study21 participated in rehabilitation programs (the authors did not describe which services were used). While rehabilitation programs are available through the public health system, patients are not always guaranteed access. Oftentimes, there is a lack of available spots, programs are offered in locations that are distant from the patient’s home, or professionals fail to recommend these services to the patient. Low or no-cost therapy is provided by some municipalities that run programs for the elderly, as well as by the nongovernmental associations and universities dedicated to PD.
Although PD mostly affects the elderly, it sometimes affects working age individuals, who also suffer physical, cognitive, and social dependence. In Brazil, patients with PD are often taken care of by a family member, which causes familial strains in addition to financial ones. In the article cited above,21 16% of family members left work to temporarily take care of the patient.
Health insurance
Relative to patients who use the public health system, individuals with private health insurance generally have greater access to different types of services. However, in most Brazilian cities, these patients compete for those services with SUS patients who have access to some private services, which means that in some cases, the patient with private insurance may be treated within the public system and, therefore, enjoys double coverage, as guaranteed by a 1988 law in the Brazilian Constitution.22
In December 2012, the Agência Nacional de Saúde Suplementar (National Agency for Supplementary Health), a federal agency that guarantees the legal and administrative regulation of the private health insurance market, estimated that Brazilian health plans offered 24.7% of coverage, with 62% of the total being spent in the southeast.3
Private health plans in Brazil usually cover younger individuals, who mostly have lower costs than elderly patients, particularly those with diseases such as PD. Plans differ in terms of a client’s choice of health care providers; some offer rehabilitation therapies, but these are usually limited in terms of number of sessions, which limits therapeutic results.
Public health policies for the elderly in Brazil
The state is responsible for creating public policies that guarantee its people’s quality of life. To this end, it uses public resources to provide health policies, among other things, which are protected by special laws.23,24 In practice, however, the SUS’s services fall short of what is outlined in the Brazilian Constitution. Specifically, there is a clear contradiction between what the law recognizes as being a citizen’s rights and the implementation of guidelines.
One of the legal and regulatory frameworks of public health policies is the Política Nacional do Idoso (National Policy for the Elderly), Law No 8,842/1994,25 which aims to ensure social rights, thus promoting the elderly patients’ autonomy, integration, and participation in society. This law considers “elderly” as being 60 years of age or older. In 2003, the Estatuto do Idoso26 (Elderly Law) was approved, which, along with the Política Nacional do Idoso, is dedicated to assist this sector of the population, including those who present some degree of dependence. Also, the Política Nacional de Saúde da Pessoa Idosa (National Health Policy for the Elderly), established by Decree 2528/GM on October 19, 2006,27 aims to integrate the elderly into health care in order to ensure healthy aging, that is, preserving their functional capacity, autonomy, and quality of life, in harmony with the principles of the SUS. The SUS, in turn, directs individual and collective measures at all levels of health care.
Unfortunately, today’s reality does not reflect the above laws’ goals. There is a major lack of funding support for most areas of research, which severely impairs progress in this area. Furthermore, new therapies are not introduced into the market, hindering people’s ability to improve their quality of life. Although there is much to be done, some milestones have been reached for this significant portion of the population, which we detail in the next few sections.
PD and public health policies in Brazil
Through the Secretaria da Atenção à Saúde (Secretariat of Health Care), the Ministério da Saúde (Ministry of Health) published an ordinance (SAS/MS No 228 on May 10, 2010)28 to establish guidelines for the diagnosis, treatment, and care of individuals with PD in Brazil. This ordinance highlights how much the government considers the disease to be important, as it uses it as an example to guide the field of aging through the Clinical Protocols and Therapeutic Guidelines.28
Often unknown to patients and/or their relatives, the following benefits and rights are guaranteed to PD patients as well as patients with other disabilities in Brazil (Table 1).
  | Table 1 Benefits and rights acquired by PD patients |
Medication
The objective of state action through the Clinical Protocols and Therapeutic Guidelines clearly outline the state’s criteria for the diagnosis of each disease, the treatment recommended with medications available in the correct doses, the control mechanisms, monitoring and checking of results, and rationalization of the prescription and supply of medicinal products.
The Componente Especializado da Assistência Farmacêutica (Specialized Component of Pharmaceutical Assistance) aims to facilitate access to medication within the SUS, and involves ensuring the integrality of drug treatments at the outpatient level. The Componente Especializado da Assistência Farmacêutica is regulated by the GM/MS No 1554, July 30, 2013 decree.29 In accordance with this decree, medications are divided into groups according to their characteristics, financing and acquisition, and forms of organization as follows:
- Group 1A: Medications financed and acquired by the Ministry of Health. 0.125, 0.25, and 1 mg tablets of Pramipexol are in this category.
- Group 1B: Medications financed by the Ministry of Health and acquired by the state Health Secretariats and the Federal District. For PD patients, the following drugs are in this group: Amantadine: 100 mg tablets; Bromocriptine: 2.5 and 5 mg delayed delivery tablets or capsules; Entacapone: 200 mg tablets; Selegiline: 5 and 10 mg tablets; Tolcapone: 100 mg tablets; Triexifenidil: 5 mg tablets.
- Group 2: Medicinal products financed and acquired by the state Health Secretariats and the Federal District.
- Group 3: Medications acquired by the state Health Secretariats and the Federal District, established by a special normative act that regulates pharmaceutical assistance. For PD patients, the following medications are in this category: Biperiden: 2 mg tablets and 4 mg controlled release tablets; Levodopa/Carbidopa: 200/50 mg and 250/25 mg tablets; Levodopa/Benserazide: 100/25 mg tablets or capsules and 200/50 mg tablets.
The current policies promoting access to medications are progressive, yet not enough to avoid operational and budgetary barriers. Firstly, not all secretariats and municipalities follow their federal obligations. There are failures in the process of medicine distribution that force patients to temporarily defray their treatment costs. In addition, new PD medications on the market are not yet available for free dispensing, which means patients must cover their costs whenever possible.
The “Farmácia Popular” (People’s Pharmacy) is yet another important government program implemented by Law No 10.85831 April 13, 2004 with establishments in >4,464 municipalities. It benefits 9 million Brazilians per month and provides PD medications.
Social insurance
Article 151 of Law 8213/91 (Planos de Beneficios da Previdência Social; Social Security Benefits)30 lists PD as a serious disease. Among other provisions, this law grants the insured person aid and retirement through social security (Instituto Nacional de Seguridade Social [INSS]). The insured person who is considered totally and completely incapable of working and who cannot be rehabilitated to earn a living will be retired after 12 months without working and will continue to receive disability aid. PD patients do not need to meet this time period requirement. Complementary Law 142/201331 allows the insured person with disabilities to retire early, and their disability is classified as either mild, moderate, or severe.
The amount received during retirement due to disability is increased by 25% when the insured person requires constant assistance, as determined by the INSS.
Despite these laws, patients in the SUS are often denied benefits without explanation. They are required to give up all work to receive the funds, but because these are often not enough to cover basic daily expenses, many patients seek work and risk losing their benefits.
Social support
Even if the disabled person has not contributed to social security, he is entitled to social protection if the per capita income of their family is lower than one-fourth of the current minimum wage.
The degree of disability and incapacity will be evaluated through medical and social evaluations by the social service of the INSS.
Income tax
According to Law 7713/88,32 retirement pension income, including complementary private funding and alimony received by PD and other patients, is not taxed, even if the disease is contracted after retirement or after a pension is granted.
Traffic restrictions
PD patients residing in the capital of São Paulo can be exempt from traffic restrictions by simply filling out the relevant forms and presenting a medical certificate.
Interstate transportation
According to Law 8899/94 and Decree 3691/00,33 people with special needs (including PD patients) and those with low income may travel between states by bus, train, or boat without paying fares. Although the law exists, many patients are unaware of it or have difficulty obtaining the exemption due to the challenges of navigating bureaucratic processes.
Tax exemption on vehicle purchases
Patients with certain diseases including PD are given up to a 30% discount on taxes when purchasing a new passenger or mixed-use national vehicle. People may also receive a discount on a used vehicle they already own. Vehicles may be purchased directly or through a legal representative, and the discount may only be received once every 2 years.
Brazilian Law for the inclusion of people with disabilities (Law 13.146 of June 7, 2015)
This law34 was created to ensure and promote the rights and fundamental liberties of people with disabilities, as well as their social inclusion. This law is based on the Estatuto da Pessoa com Deficiência (People with Disabilities Statute), a wide-reaching project that works toward the inclusion of disabled people in various areas, such as education, transport, leisure, health, work, and justice, both through public policies and company initiatives.
Thus, by being included in this law (following a disability evaluation by a multiprofessional team), PD patients should enjoy the aforementioned benefits. However, this law has not been put into practice successfully.
Although the actions described above are part of government programs that try to meet the proposed objectives, some of which are very solid, several goals still require the support of philanthropic, religious, and nongovernmental organizations. Although supported by the patient population and their families and friends, these programs still serve only a small proportion of patients.
An online search using known search engines and the keywords “Association”, “Associations”, “Philanthropic”, “NGOS”, “Support Center”, “Institute”, “Home”, and “Parkinson’s disease” revealed 30 such associations in Brazil. Generally, one can assume that these associations do not receive any financial support from any sphere of government (although many have requested it) and that all have their own resources, as well as some sponsorship from companies or private donations. And while many are also trying to survive in the current economic conditions (in some cases with the loss of sponsorship), they consistently show that they try to offer the best care to the patients.
For example, the Associação Brasil Parkinson, located in São Paulo (which celebrated 30 years in December 2015), depends on physical therapists, speech therapists, and volunteers who serve almost 2,000 (1,200 active) registered patients through ~19,000 visits per year. The Associação Paranaense dos Portadores de Parkinsonismo (Parkinson’s association of the state of Paraná), founded in December 2000 in Curitiba and with a satellite location in São Paulo, is a nonprofit federal, state, and municipal public entity that conducted 53,800 visits in 2014 in various modalities (eg, neurology, geriatrics, nursing, massage therapy, acupuncture, physiotherapy, choral, theater) for 2,641 members. Besides these activities, the association has a pharmacy specializing in PD that freely dispenses medicinal products. Patients include association members, SUS patients, and residents of Curitiba as well as other metropolitan regions. The association relies on donations from its own patients and receives no assistance from the government. Other associations throughout Brazil arose from the initiative of doctors and other people interested in helping these patients.
Health funding in Brazil and around the world
In virtually all countries, spending on health services is shared between the public and private sectors in varying proportions. In general, in countries with high or mid-high income, health funding usually comes from public sources. In low-income countries, on the other hand, most health funding comes from the so-called “direct disbursement” (or “out-of-pocket”) funds, which represent the most inequitable and unstable form of financing.35 In Brazil, this type of expenditure varies from 30.1% to 50% of the total amount spent on health care; in Canada and in some African nations, this number is between 15% and 30%, while in the USA and some European countries, spending is <15% of the total amount.36
Brazil is perhaps the only country with a universal health system guaranteeing universal assistance that spends more with public than private funds. However, among some nations in the Organization for Economic Cooperation and Development, public funding represents ~70% of the total expenditure, which is in contrast to Brazil’s 42% of public funds spent in 2007.35
One of the main consequences of an aging population on the Gross Domestic Product (GDP) is increased health care cost. In 2013, Brazil spent 8% of its GDP (US$ 131.5 billion) on health services, 3.6% from government and 4.4% from households and nonprofit institutions. That year, 77.6% of all costs was spent on services (rising from 75.9% in 2010) and 20.6% on medications (there was a reduction from 22.3% during that same period).37
In 2013, households spent more than the government on medication (representing 1.5% vs 0.2% of household GDP; this does not include Farmácia Popular data), which highlights the flaws in medication distribution and costs (Table 2).37 Furthermore, Figure 2 shows that families spent more on out-of-pocket health expenditures than the government in 2010 and 2013.
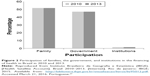  | Figure 2 Participation of families, the government, and institutions in the financing of health in Brazil in 2010 and 2013. |
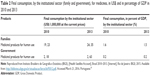  | Table 2 Final consumption, by the institutional sector (family and government), for medicines, in US$ and in percentage of GDP in 2010 and 2013 |
The health care budget in Brazil for 2016 is US$ 18,850 billion (gross total value, not counting inflation for the period), nearly US$ 4,680 billion less than that of 2015. This deficit is expected to worsen underfunding, although ~US$ 11,574 billion of that is allotted to medium- and high-complexity outpatient and inpatient services (US$ 2,808 billion less than in 2015).38
It should be noted that some health care features will become even scarcer because for some investments, loans were taken out in dollars, which generated a cost increase of ~45% during 2015.
Conclusion
The demographic transition that Brazil is experiencing demands that public policies prioritize care for the elderly, especially those with chronic diseases such as PD. The country spends relatively little on health, which hinders the implementation of a universal public health system. Furthermore, the current economic crisis “pushes” individuals who can no longer afford insurance toward the SUS, causing a higher demand than usual.
Not all current laws are properly implemented. Furthermore, civil society is actively engaged in trying to fill in the gaps left by the state or families. However, the society is most often concerned with children, youth, and the environment than it is with the elderly and the chronically ill.
We conclude that more research is needed to fully understand the total cost of PD in Brazil. This information will allow resources to be better allocated and ensure that patients have a better quality of life while simultaneously reducing the government’s economic burden.
Disclosure
The authors report no conflicts of interest in this work.
References
Instituto Brasileiro de Geografia e Estatística (IBGE). [Demographic Trends. An analysis of the population based on the results of the Demographic Censuses 1940 and 2000] [Internet]. Rio de Janeiro: IBGE; 2007. Available from: http://biblioteca.ibge.gov.br/visualizacao/livros/liv34956.pdf. Accessed February 8, 2016. Portuguese. | ||
Instituto Brasileiro de Geografia e Estatística (IBGE). [Sociodemographic and Health Indicators in Brazil]. [Internet]. Rio de Janeiro: IBGE; 2009. Available from: http://www.ibge.gov.br/english/estatistica/populacao/indic_sociosaude/2009/indicsaude.pdf. Accessed February 8, 2016. Portuguese. | ||
Instituto Brasileiro de Geografia e Estatística (IBGE). [Synthesis of social indicators. An analysis of the living conditions of the Brazilian population]. [Internet]. Rio de Janeiro: IBGE; 2013. Available from: http://biblioteca.ibge.gov.br/visualizacao/livros/liv95011.pdf. Accessed February 10, 2016. Portuguese. | ||
Zago MA. [Clinical research in Brazil]. Ciênc saúde coletiva. 2004;9:363–374. Portuguese. | ||
Parahyba MI, Simões CCdS. [Disability prevalence among the elderly in Brazil]. Ciênc saúde coletiva. 2006;11:967–974. Portuguese. | ||
Instituto Brasileiro de Geografia e Estatística (IBGE). [Projections of the Brazilian Population and Federative Units]. [Internet]. Rio de Janeiro: IBGE; 2013. Available from: http://www.ibge.gov.br/apps/populacao/projecao/. Accessed February 11, 2016. Portuguese. | ||
United Nations. Population Division. World Population Prospects 2015.[Internet]. USA; 2015. Available from: https://esa.un.org/unpd/wpp/Graphs/DemographicProfiles/. Accessed July 18, 2016. | ||
Instituto Brasileiro de Geografia e Estatística (IBGE). [Ratio of dependence by age group]. Rio de Janeiro: IBGE, 2006. [Internet]. Available from: http://seriesestatisticas.ibge.gov.br/series.aspx?vcodigo=CD95. Accessed February 17, 2016. Portuguese. | ||
United Nations. World Population Prospects: the 2015 Revision, Key Findings and Advance. [Internet]. New York, USA; 2015. Available from: https://esa.un.org/unpd/wpp/publications/files/key_findings_wpp_2015.pdf. Accessed July 20, 2016. | ||
Lebrão ML. [Aging in Brazil: Aspects of Demographic and Epidemiological Transition]. Saúde Coletiva. Vol ano/vol. 4. São Paulo, Brasil: Editorial Bolina; 2007:135–140. Portuguese. | ||
Veras RP. Experiências e tendências internacionais de modelos de cuidado para com o idoso [International experiences and trends in health care models for the elderly]. Cien Saude Colet. 2012;17(1):231–238. Portuguese. | ||
Wong LLR, Carvalho JA. [The rapid aging process in Brazilian population: serious challenges for public policy]. Revista Brasileira de Estudos de População. 2006;23:5–26. Portuguese. | ||
Dorsey ER, Constantinescu R, Thompson JP, et al. Projected number of people with Parkinson disease in the most populous nations, 2005 through 2030. Neurology. 2007;68(5):384–386. | ||
Bach J-P, Ziegler U, Deuschl G, Dodel R, Doblhammer-Reiter G. Projected numbers of people with movement disorders in the years 2030 and 2050. Mov Disord. 2011;26(12):2286–2290. | ||
Barbosa MT, Caramelli P, Maia DP, et al. Parkinsonism and Parkinson’s disease in the elderly: a community-based survey in Brazil (the Bambuí study). Mov Disord. 2006;21(6):800–808. | ||
Ferraz HB. [Parkinson disease Clinical and Therapeutic Practice. Neurological Series – Diagnosis and Treatment.]. São Paulo – Brasil: Editora Atheneu; 2005. Portuguese. | ||
[Ministry of Health. National Health Plan 2012–2015 PNS]. [Internet]. Brasília (DF): Ministério da Saúde; 2011. Available from: http://conselho.saude.gov.br/biblioteca/Relatorios/plano_nacional_saude_2012_2015.pdf. Portuguese. Accessed March 1, 2016. Portuguese. | ||
[Ministry of Health. Datasus Information Technology at the SUS Service. CNES – Establishments by Level of Attention]. [Internet]. Brasil; 2016. Available from: http://tabnet.datasus.gov.br/cgi/tabcgi.exe?cnes/cnv/atencbr. Portuguese. Accessed October 4, 2016. Portuguese. | ||
[Ministry of Health. Datasus Information Technology at the SUS Service. SUS Ambulatory Production]. [Internet]. Brasil; 2016. Available from: tabnet.datasus.gov.br/cgi/tabcgi.exe?cnes/cnv/atencbr.def/. Accessed October 4, 2016. Portuguese. | ||
[Ministry of Health. Datasus Information Technology at the SUS Service. Morbidade Hospitalar do SUS – by place of hospitalization]. [Internet]. Brasil; 2016. Available from: http://tabnet.datasus.gov.br/cgi/tabcgi.exe?sih/cnv/niuf.def. Accessed October 4, 2016. Portuguese. | ||
Vargas AP, Carod-Artal FJ, Nunes SS, Melo M. Disability and use of healthcare resources in Brazilian patients with Parkinson’s disease. Disability and Rehabilitation. 2008;30(14):1055–1062. | ||
[Constitution of the Federative Republic of Brazil]. Brasília (DF): Senado; 1988. Portuguese. | ||
Roncalli AG. [The development of public health policies in Brazil and the construction of the Unified Health System]. Odontologia em Saúde Coletiva: planejando ações e promovendo saúde. Porto Alegre, Brasil: ArtMed; 2003:28–49. Portuguese. | ||
Teixeira EC. [The role of public policies in local development and the transformation of reality]. Salvador, Brasil: AATR; 2002:1–11. Portuguese. | ||
[Presidency of the Republic. Law no. No. 8,842 of January 4, 1994. It provides on the national policy of the elderly, creates the National Council for the Elderly and makes other provisions. Official Gazette of the Federative Republic of Brazil]. Brasília (DF): 1994 Jan 04. Available from: http://www.planalto.gov.br/ccivil_03/leis/L8842.htm. Accessed March 1, 2016. Portuguese. | ||
[Presidency of the Republic. Law no. 10,741 of October 1, 2003. It provides for the Statute of the Elderly and provides other measures. Official Gazette of the Federative Republic of Brazil]. Brasília (DF): 2003 Out 01. Available from: http://www.planalto.gov.br/ccivil_03/leis/2003/l10.741.htm. Accessed March 1, 2016. Portuguese. | ||
[Ministry of Health. Ordinance No. 2,528 of October 19, 2006. Approves the National Health Policy of the Elderly Person. Official Gazette of the Federative Republic of Brazil]. Brasília (DF): 2006 Out 19. Available from: http://www.mds.gov.br/webarquivos/publicacao/assistencia_social/Normativas/politica_idoso.pdf. Accessed March 3, 2016. Portuguese. | ||
[Ministry of Health. Ordinance n° 228 of May 10, 2010. Clinical protocol and therapeutic guidelines – Parkinson’s disease. Official Gazette of the Federative Republic of Brazil]. Brasília (DF): 2010 Mai 10. Available from: http://bvsms.saude.gov.br/bvs/saudelegis/sas/2010/prt0228_10_05_2010.html. Accessed March 3, 2016. Portuguese. | ||
[Ministry of Health. Ordinance No. 1554, dated July 30, 2013. Provides for the rules for financing and execution of the Specialized Component of Pharmaceutical Assistance within the Unified Health System (SUS). Official Gazette of the Federative Republic of Brazil] Brasília (DF): 2013 Jul 30. Available from: http://bvsms.saude.gov.br/bvs/saudelegis/gm/2013/prt1554_30_07_2013.html. Accessed March 1, 2016. Portuguese. | ||
[Presidency of the Republic. Law No. 8213 of July 24, 1991. Provides for the Plans of Benefits of Social Security and other measures. Official Gazette of the Federative Republic of Brazil]. Brasília (DF): 1991 Jul 24. Available from: http://www.planalto.gov.br/ccivil_03/leis/L8213cons.htm. Accessed March 4, 2016. Portuguese. | ||
[Presidency of the Republic. Supplementary Law No. 142 of May 08, 2013. Regulates § 1 of art. 201 of the Federal Constitution, regarding the retirement of the insured person of the General Social Security Regime – RGPS. Official Gazette of the Federative Republic of Brazil]. Brasília (DF): 2013 Mai 08. Available from: http://www.planalto.gov.br/ccivil_03/leis/LCP/Lcp142.htm. Accessed March 4, 2016. Portuguese. | ||
[Presidency of the Republic. Law no. 7,713 of December 22, 1988. It amends the income tax legislation and makes other provisions. Official Gazette of the Federative Republic of Brazil]. Brasília (DF): 1988 dez 22. Available from: http://www.planalto.gov.br/ccivil_03/decreto/d3691.htm. Accessed March 11, 2016. Portuguese. | ||
[Presidency of the Republic. Decree No. 3.691, dated December 19, 2000. Regulates Law No. 8,899, of June 29, 1994, which provides for the transportation of persons with disabilities in the interstate collective transportation system. Official Gazette of the Federative Republic of Brazil]. Brasília (DF): 2000 dez 19. Available from: http://www.planalto.gov.br/ccivil_03/leis/L7713.htm. Accessed March 10, 2016. Portuguese. | ||
[Presidency of the Republic. Law no. 13,146, dated July 6, 2015. Institutes the Brazilian Law on the Inclusion of Persons with Disabilities (Statute of Persons with Disabilities). Official Gazette of the Federative Republic of Brazil]. Brasília (DF): 2015 Jul 06. Portuguese. | ||
Piola FS, Servo LM, Sá EBd, Paiva ABd. [SUS Funding: Recent Path and Scenarios for the Future]. Porto Alegre – Brasil 2012:9–33. Portuguese. | ||
WHO-World Health Organization. Global Health Observatory (GHO) data: Out-of-pocket expenditure on health as a percentage of private expenditure on health (%), 2013. [Internet]. USA; 2016. Available from: http://www.who.int/gho/health_financing/out_pocket_expenditure/en/. Accessed March 20, 2016. | ||
Instituto Brasileiro de Geografia e Estatística (IBGE). [Health Satellite Account]. Brasil 2010–2013. [Internet]. Rio de Janeiro: IBGE; 2015. Available from: http://biblioteca.ibge.gov.br/visualizacao/livros/liv95012.pdf. Accessed March 21, 2016. Portuguese. | ||
[Ministry of Health. National Health Fund]. [Internet]. Brasil; 2016. [cited 2016 Nov 2]. Available from: http://www.fns.saude.gov.br/visao/consulta/grafico/comparativo/filtro.jsf. Accessed March 20, 2016. Portuguese. |
 © 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
