Back to Journals » Neuropsychiatric Disease and Treatment » Volume 18
Homocysteine and Clinical Outcomes in Intracerebral Hemorrhage Patients: Results from the China Stroke Center Alliance
Authors Wang D , Cao Z, Li Z, Gu H, Zhou Q, Zhao X , Wang Y
Received 28 September 2022
Accepted for publication 25 November 2022
Published 7 December 2022 Volume 2022:18 Pages 2837—2846
DOI https://doi.org/10.2147/NDT.S391618
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Yuping Ning
Dandan Wang,1,2 Zhentang Cao,3 Zixiao Li,1,2,4 Hongqiu Gu,2 Qi Zhou,2 Xingquan Zhao,1,2,4 Yongjun Wang1,2,4
1Department of Neurology, Beijing Tiantan Hospital, Capital Medical University, Beijing, People’s Republic of China; 2China National Clinical Research Center for Neurological Diseases, Beijing, People’s Republic of China; 3Department of Neurology, The First Affiliated Hospital of Zhengzhou University, Zhengzhou, Henan, People’s Republic of China; 4Research Unit of Artificial Intelligence in Cerebrovascular Disease, Chinese Academy of Medical Sciences, Beijing, People’s Republic of China
Correspondence: Xingquan Zhao; Yongjun Wang, Department of Neurology, Beijing Tiantan Hospital, Capital Medical University, No. 119 South 4th Ring West Road, Fengtai District, Beijing, 100070, People’s Republic of China, Tel +86-010-59978891 ; +86-010-59978330, Email [email protected]; [email protected]
Objective: Elevated homocysteine (Hcy) levels play a detrimental role in ischemic stroke. Acute spontaneous intracerebral hemorrhage (ICH) accounts for nearly 25% of all stroke cases. However, the influence of Hcy levels and ICH severity on clinical outcomes is unclear.
Participants and Study Location: Data were obtained from 85,705 ICH patients enrolled in the China Stroke Center Alliance (CSCA) study, a national, hospital-based, multicenter, voluntary, quality assessment and improvement initiative performed in China. Patients were divided into high and normal Hcy groups according to their Hcy levels observed at admission.
Outcome Measures: The outcome indices included severe ICH, in-hospital mortality, and a poor functional outcome at discharge. Multivariable logistic regression was used to analyze the association of different Hcy levels with outcomes.
Results: The final analysis included 55,793 ICH patients. High homocysteine (HHcy) levels had higher adjusted odds ratios for severe ICH (OR 1.09, 95% CI 1.01– 1.10, P< 0.0001) and a poor functional outcome at discharge (OR 1.06, 95% CI 1.01– 1.10, P=0.0100) compared with normal Hcy levels. There was no significant difference between HHcy and in-hospital mortality. In the subgroup analysis, stratified by sex and history of hypertension, significant interactions were observed between HHcy and severe ICH (P for interactions was 0.0138 and 0.0120, respectively). HHcy levels exhibited greater associations for severe ICH in female patients (OR 1.07, 95% CI 1.02– 1.12) and patients without hypertension (OR 1.20, 95% CI 1.09– 1.33).
Conclusion: An elevated Hcy level exhibited significant association with severe ICH on admission and a poor functional outcome at discharge. The relationship between HHcy and ICH severity on admission was more robust in female patients and patients without hypertension. Hcy might be a valuable biomarker for ICH patients to predict severity at onset and functional outcome at discharge.
Keywords: intracerebral hemorrhage, homocysteine, stroke severity, outcome
Introduction
Homocysteine (Hcy) is a sulfhydryl-containing amino acid that occurs as an intermediate component in methionine metabolism.1 When the pathway is impaired, Hcy levels increase. According to previous studies,2–5 elevated Hcy levels exert detrimental effects and elevate the mortality rates on ischemic stroke and cardiovascular diseases. A meta-analysis reported that vitamin B supplementations that reduced Hcy prevented the combined risk of stroke, myocardial infarction, and vascular death among stroke patients.6
However, many of the previous researches have been limited to ischemic stroke, and few published studies are available concerning hemorrhagic stroke. Globally, acute spontaneous intracerebral hemorrhage (ICH) accounts for approximately 25% of all stroke cases.7 The subsequent serious complications, morbidity, and mortality associated with ICH account for approximately half of the disability-adjusted life-years lost due to stroke.7,8 Thus, ICH exacts an immense burden on families and society. Presently, there is no specific treatment available for ICH. Therefore, it is imperative to explore more effective intervention targets to reduce the fatality and disability rates associated with ICH.
Several studies have reported that high Hcy (HHcy) is an independent risk factor for hemorrhagic stroke due to the promotion of plaque rupture.9 However, it is unclear whether the Hcy level observed at admission is associated with ICH severity and clinical outcomes. Because Hcy is a modifiable risk factor that can be prevented and treated by vitamin supplementation, understanding the relationship between Hcy and ICH outcomes is clinically significant. Therefore, this study explored the relationships between Hcy levels and ICH severity and the outcomes observed in acute ICH patients.
Methods
Study Cohort and Population
The data were obtained from the Chinese Stroke Center Alliance (CSCA) registry, a national, hospital-based, multicenter, voluntary, quality assessment and improvement initiative performed in China.10 The CSCA program design, data collection, and management details have been described previously.10 Trained personnel at each participating research hospital used a web-based patient management tool (GaiDe, Inc, Beijing, China) to collect patients’ clinical data. The primary purpose of the CSCA was to facilitate quality improvement (QI). At the local level, data collection at each site was seen as a QI tool. Participating hospitals received approval from their local Institutional Review Board to collect data in the CSCA project without requiring individual patient informed consent under a common rule or a waiver of authorization and exemption. Patients were not involved in the design, recruitment, or implementation of the study, and they were not aware of the study results to avoid bias. Notably, informed consent can lead to a sampling bias, which can jeopardize the validity and generalizability of the database. An informed consent from a doctor to the patient would both influence the doctor’s following medical judgment and treatment strategy and patient’s compliance to the doctor. Moreover, patients who did not coordinate with doctors could not enrolled in this study if an informed consent is needed. Patient confidentiality was protected in the following ways: (1) the data were stripped of all identifiers before use in the research, and (2) the use of data for these purposes was closely overseen by the China National Clinical Research Center for Neurological Diseases Analytic Center.
As of July 2019, there were 85,705 patients with ICH among all the enrolled participants in CSCA. The inclusion criteria for this study included (1) patients were 18 years or older, (2) had a primary diagnosis of ICH confirmed by brain CT or MRI; (3) were within seven days of symptom onset, (4) were admitted either directly to the hospital neurology department or through the emergency department. The exclusion criteria included (1) Hcy data were unavailable and (2) the patient had a history of stroke. The final analysis included 55,793 ICH patients. The patients were divided into two groups according to their baseline Hcy levels, a normal Hcy group and a high Hcy (HHcy) group. This study defined HHcy as a Hcy level greater than 15 umol/L.4,11
Patient and Public Involvement
Previous studies concerning patient experiences in observational trials of acute stroke were consulted for this study to allow adequate inclusion of patient experiences. Physicians screened potential participants in the emergency or neurology departments at each study center. The results will be disseminated to the study participants as public documents and through the long-term health management clinic.
Data Collection
Baseline information, including sex, age, body mass index (BMI), household income, smoking and drinking status, systolic blood pressure (SBP), diastolic blood pressure (DBP), medical history, in-hospital laboratory tests, and in-hospital complications, were collected via the web-based patient data collection and management tool. The medical history included hypertension, diabetes, and hyperlipidemia. The in-hospital laboratory test included Hcy, fasting blood glucose (FBG), glycated hemoglobin (GHb), total cholesterol (TC), triglyceride (TG), and low-density lipoprotein (LDL). The blood samples were taken in ethylene-diamine-tetra-acetic-acid (EDTA) vials to quantify serum Hcy. The in-hospital complications included re-bleeding, pneumonia, poor swallowing function, pulmonary embolism, seizure, urinary tract infection, hydrocephalus, deep vein thrombosis (DVT), decubitus, and gastrointestinal bleeding. We also collected Glasgow coma scale (GCS) scores at admission and modified Rankin Scale (mRS) scores at discharge. All relevant definitions of these indexes have been reported in our previous protocol.10
Outcomes
The outcomes included severe ICH at admission, in-hospital mortality, and a poor functional outcome at discharge. The designation of severe ICH at admission referred to a GCS score of 12 or less points. In-hospital mortality was defined as all causes of mortality during hospitalization. The poor functional outcome at discharge was defined as an mRS score of 3 to 5.
Statistical Analysis
Baseline characteristics were compared between the two groups. Continuous variables were presented as means ± standard deviation (SD), and categorical variables as numbers (percentages). The χ2 test was performed to compare categorical variables. For normally distributed continuous variables, we used an independent t-test. For data with non-normal distributions, we used the Mann–Whitney U-test.
Multivariable logistic regression analysis was used to assess the relationship between Hcy and outcomes, including severe ICH, in-hospital mortality, and a poor functional outcome at discharge. First, the crude odds ratio (OR) was calculated. Then, we adopted two models to adjust for possible confounders. Model 1 included age and sex. Model 2 included sex, age, BMI, household income, smoking, drinking, diagnosis of diabetes mellitus, and dyslipidemia on discharge. We also performed subgroup analyses. The subgroups included age (<60 vs ≥60 years old), sex (female vs male), history of hypertension (with vs without), and history of diabetes (with vs without). Missing data were minimal and not included in the statistical analysis.
All analyses were performed using SAS software version 9.4 (SAS Institute Inc., Cary, NC, USA). A two-tailed P-value < 0.05 was considered statistically significant. A SAS macro, %gg Baseline, was used to analyze and report baseline characteristics automatically.12
Results
Characteristics of the Study Population
There were 85,705 ICH patients initially identified in the CSCA database. After excluding patients with missing Hcy data (n=7430) and a history of stroke (n=22,482), 55,793 ICH patients were included in the final analysis. A flowchart of this study is depicted in Figure 1.
 |
Figure 1 ICH and Hcy flowchart. Abbreviations: ICH, intracerebral hemorrhage; CSCA, China Stroke Center Alliance; Hcy, homocysteine. |
The mean patient age was 62.3 years, and 34,705 (62.6%) were male. The patients were divided into two groups according to their baseline Hcy levels; 22,492 (40.3%) patients were included in the HHcy group and 33,301 (59.7%) in the normal Hcy group. The baseline characteristics of the two groups are shown in Table 1. In addition to TC, other baseline variables were statistically different between the two groups. Compared to patients with normal Hcy levels, patients with HHcy were older, exhibited a higher BMI, and were more likely to be male. The HHcy group also exhibited a higher percentage of vascular risk factors, including currently smoking (24.0%), drinking (28.0%), hypertension (85.1%), and hyperlipidemia (12.8%). In addition, the HHcy group exhibited a lower percentage of diabetes (10.1%) and higher SBP, DBP, FBG, GHb, TG, and LDL (all P<0.05). The missing numbers of patients for the variables listed above were 0 (gender), 0 (age), 1589 (BMI), 0 (household income), 0 (smoking), 0 (drinking), 26 (SBP), 26 (DBP), 302 (FBG), 6164 (GHb), 44,635 (TC), 44,613 (TG), 238 (LDL), 9059 (hypertension), 49.762 (diabetes), and 48.872 (hyperlipidemia), each calculated separately.
 |
Table 1 Baseline Characteristics and Their Univariate Association with Hcy Levels |
We also examined the relationship between Hcy levels and in-hospital complications. The detailed results are shown in Table 2. Compared with the normal Hcy group, the HHcy group exhibited a higher percentage of pneumonia (P<0.0001), poor swallowing function (P=0.0001), and decubitus (P=0.0312). Other in-hospital complications, including re-bleeding, pulmonary embolism, seizure, urinary tract infection, hydrocephalus, DVT, and gastrointestinal bleeding, were not significantly different between the two groups. The missing number of patients for the variables listed above were 97 (rebleeding), 97 (pneumonia), 15,583 (swallowing function), 97 (pulmonary embolism), 97 (seizure), 97 (urinary tract infection), 97 (hydrocephalus), 97 (DVT), 97 (decubitus), and 2613 (gastrointestinal bleeding), each calculated separately.
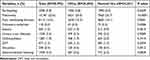 |
Table 2 Analysis of the Relationships Between Hcy Levels and in-Hospital Complications |
HHcy and Clinical Outcomes
Multivariable logistic regression was used to analyze the association of HHcy with severe ICH on admission, in-hospital mortality, and a poor functional outcome at discharge. The results are depicted in Table 3. The percentage of severe ICH was 70.2% in the HHcy group and 68.9% in the normal Hcy group. The in-hospital mortality rate was 2.1% in the HHcy group and 1.9% in the normal Hcy group. The percentage of patients with a poor functional outcome at discharge was 23.4% in the HHcy group and 22.2% in the normal Hcy group. After adjusting for stroke relevant risk factors that were significantly different between the two groups (see Table 1), the multivariate analysis revealed that HHcy had a higher adjusted odds ratio for severe ICH (OR 1.09, 95% CI 1.01–1.10, P<0.0001) and poor functional outcome at discharge (OR 1.06, 95% CI 1.01–1.10, P=0.010) compared to patients with normal Hcy levels. There was no significant difference between HHcy levels and in-hospital mortality. The missing numbers of patients for these variables were 26,870 (GCS), 32,242 (mRS), and 165 (death), each calculated separately.
 |
Table 3 Adjusted Odds Ratios (OR) for HHcy Levels and the Presence of ICH Severity on Admission (GCS≤12), in-Hospital Mortality, and a Poor Functional Outcome (mRS 3–5) at Discharge |
Subgroup Analysis
Based on the presented results and baseline characteristics, we incorporated age, sex, history of hypertension, and history of diabetes into the subgroup analysis. The results of the subgroup analysis concerning the relationship between HHcy and severe ICH are shown in Figure 2. Stratified by sex and history of hypertension, significant interactions were observed between HHcy and severe ICH (P for interaction = 0.0138 and 0.0120, respectively, Figure 2). Notably, HHcy revealed greater associations with severe ICH in female patients (OR 1.07, 95% CI 1.02–1.12) and patients without hypertension (OR 1.20, 95% CI 1.09–1.33). There were no significant interactions for the other subgroups analyzed. The subgroup analysis results for the relationships between HHcy levels and a poor functional outcome at discharge are seen in Figure 3. Finally, no significant interaction was found between HHcy and sex, age, history of hypertension, or history of diabetes (Figure 3).
 |
Figure 2 Subgroup analysis between Hcy and severe ICH. Abbreviations: DM, diabetes mellitus; OR, odd ratios; CI, confidence interval. |
 |
Figure 3 Subgroup analysis between Hcy and functional outcome at discharge. Abbreviations: DM, diabetes mellitus; OR, odd ratios; CI, confidence interval. |
Discussion
The current study indicated that an HHcy level was associated with severe ICH in patients on admission and a poor functional outcome at discharge. The subgroup analysis determined that elevated Hcy levels exhibited a greater association with severe ICH in female patients and patients without hypertension.
When Hcy was above 15umol/L, this condition was considered HHcy.13 This study indicated that in the acute ICH population, HHcy patients were older, exhibited a higher BMI, and were more frequently male. The HHcy group also included a higher percentage of patients currently smoking and drinking. These results were consistent with previous studies from the Framingham Offspring cohort,14 the third National Health and Nutrition Examination Survey (NHANES III),15 and the Hordaland Homocysteine Study (HHS).16 Hcy levels are influenced by numerous factors, including age, sex, nutrition habits, and lifestyle habits.17 Lifestyle habits include smoking, alcohol consumption, sedentary behavior, and others.18 Hcy levels increase with age, and mean concentrations of HCY in males are higher than in females. Previous studies revealed a significant positive association between plasma Hcy and smoking and drinking.14,18 Smoking may lead to deficiencies in B-vitamins or folate, and consuming alcohol affects the intestinal absorption of folic acid.19 Obesity also could result in vitamin deficiencies, especially for fat-soluble vitamins.20
We also found that the HHcy group exhibited a higher percentage of risk factors for atherosclerosis, such as hypertension and hyperlipidemia. Currently, the relationship between blood pressure and Hcy levels remains uncertain. Most studies, such as the HHS21 and NHANES III,22 indicated a positive association between the level of Hcy and blood pressure. Wu23 et al and Li24 et al also reported that HHcy was related to elevated DBP. However, other studies, such as the China Stroke Primary Prevention Trial (CSPPT),25 found no significant associations between Hcy levels and blood pressure.
Interestingly, the HHcy group had a higher percentage of pneumonia, poor swallowing function, and decubitus. The underlying mechanisms for these associations are unknown. However, one study indicated that acute ischemic stroke patients with elevated total Hcy levels had a 1.55-fold increased risk of in-hospital pneumonia.26 Hcy is currently considered to be a useful marker for inflammation. Considering the inflammation and oxidative stress theory of atherosclerosis, HHcy might accelerate the generation of high-sensitivity C-reactive protein, interleukin-8, caspase-9, matrix metalloproteinase, and other proteins that participate in the early-state formation of atherosclerosis27 and the accumulation of inflammatory factors also might result in pneumonia. Furthermore, patients with ICH have a greater need for bed rest as the medical condition of HHcy patients is more severe. These factors might be why HHcy patients exhibited more decubitus.
Numerous studies have investigated the relationship between Hcy and outcomes in patients with ischemic stroke. However, only a few studies have analyzed the relationship between Hcy levels and prognosis in patients with ICH. In our study, the HHcy group exhibited a higher adjusted odds ratio for severe ICH according to the GCS. This conclusion concerning the relationship between GCS and Hcy levels was inconsistent with other studies. One study28 reported an inverse association between GCS and Hcy levels. Another study29 indicated that Hcy levels did not correlate with GCS levels on admission. Hcy may aggravate the process of atherosclerosis and elevate the risk of hemorrhagic vascular diseases by the coefficient results of the pathogenesis such as inflammatory reaction, oxidative stress theory, dyslipidemia mechanism and coagulation dysfunction.31 We found in this study that HHcy was more associated with severe ICH in female patients and patients without hypertension. We speculated that these two factors may have influenced the relationship between Hcy and GCS. Also, one study30 showed that elevated Hcy levels were related to a larger hematoma volume in patients with thalamo-ganglionic ICH but not in lobar or infratentorial ICH. The hematoma location and volume could influence the GCS score. Therefore, additional comprehensive factors need to be analyzed, including imaging indices, to explore the relationship between Hcy levels and ICH severity in greater depth.
We also found that the HHcy group had a higher adjusted odds ratio for a poor functional outcome at discharge than the normal Hcy group. No published studies have investigated the relationship between Hcy and functional outcome at discharge. Nevertheless, one study31 reported that HHcy levels were independently associated with a poorer three-month prognosis in patients with ICH. Another study32 also reported that Hcy was a predictor for mortality in patients with ICH in the north Indian population. It is possible that HHcy levels affected the endothelial cell diastolic function and apoptosis.33 We speculated that the hyalinization and apoptosis of small artery endothelial cells might cause ICH and influence its prognosis. Therefore, Hcy might be a promising biomarker for predicting short- or long-term functional outcomes in patients. However, no significant differences were observed between the HHcy and normal Hcy groups concerning in-hospital mortality. Prospective and follow-up studies are needed to validate these observations. Finally, our observation of no significant difference between HHcy and in-hospital mortality was consistent with the previous study.29
Our study investigated the relationship between Hcy levels and ICH severity and clinical outcomes. The CSCA database provided many advantages, including large sample size, for testing our hypothesis. The analysis indicated that Hcy might be a potential target for ICH treatment. However, additional basic and clinical research is needed to validate our results.
Several limitations were noted in this study. First, it was a retrospective study of the Chinese population, limiting the ability to generalize the conclusions. Some of the data quality, such as the accuracy and consistency of the Hcy level and acquired time among different labs could not be guaranteed during the study analysis. Second, the data concerning hematoma volume and location were not available, and additional study is essential to analyze the impact of these variables on ICH outcomes. Finally, the CSCA database did not provide follow-up information. Long-term functional outcomes and living status need to be evaluated in the future.
Conclusion
In summary, our study showed that elevated Hcy levels were related to severe ICH on admission and a poor functional outcome at discharge. The relationship between HHcy and ICH severity on admission was more robust in female patients and patients without hypertension. Therefore, Hcy is a promising biomarker to predict severity at onset and functional outcome at discharge for ICH patients. More attention should be given to the Hcy level of patients with ICH, not just patients with ischemic stroke.
Data Sharing Statement
All data is available at http://paper.ncrcnd.ttctrc.com/default/project-detail?id=290.
Ethics Statement
Participating hospitals received either healthcare quality assessment and research approval to collect data in the CSCA project without requiring individual patient informed consent under the common rule or a waiver of authorization and exemption from subsequent review by their Institutional Review Board (IRB of Beijing Tiantan Hospital, KY-2018-061-02).
Acknowledgments
The authors would like to express their gratitude to EditSprings (https://www.editsprings.cn) for the expert linguistic services provided.
Funding
This study is supported by Beijing Municipal Science & Technology Commission (D171100003017002, Z181100001818001), National Natural Science Foundation of China (82001239) and Beijing Hospitals Authority Innovation Studio of Young Staff Funding Support, code (202112).
Disclosure
There is no financial or non-financial conflict of interest in our study.
References
1. Djuric D, Jakovljevic V, Zivkovic V, et al. Homocysteine and homocysteine-related compounds: an overview of the roles in the pathology of the cardiovascular and nervous systems. Can J Physiol Pharmacol. 2018;96(10):991–1003. doi:10.1139/cjpp-2018-0112
2. Shi Z, Guan Y, Huo YR, et al. Elevated total homocysteine levels in acute ischemic stroke are associated with long-term mortality. Stroke. 2015;46(9):2419–2425. doi:10.1161/strokeaha.115.009136
3. Studies Collaboration H. Homocysteine and risk of ischemic heart disease and stroke: a meta-analysis. JAMA. 2002;288(16):2015–2022. doi:10.1001/jama.288.16.2015
4. Sacco RL, Anand K, Lee HS, et al. Homocysteine and the risk of ischemic stroke in a triethnic cohort: the Northern MAnhattan Study. Stroke. 2004;35(10):2263–2269. doi:10.1161/01.Str.0000142374.33919.92
5. Cui R, Moriyama Y, Koike KA, et al. Serum total homocysteine concentrations and risk of mortality from stroke and coronary heart disease in Japanese: the JACC study. Atherosclerosis. 2008;198(2):412–418. doi:10.1016/j.atherosclerosis.2007.09.029
6. Kataria N, Yadav P, Kumar R, et al. Effect of vitamin B6, B9, and B12 supplementation on homocysteine level and cardiovascular outcomes in stroke patients: a meta-analysis of randomized controlled trials. Cureus. 2021;13(5):e14958. doi:10.7759/cureus.14958
7. Krishnamurthi RV, Ikeda T, Feigin VL. Global, regional and country-specific burden of ischaemic stroke, intracerebral haemorrhage and subarachnoid haemorrhage: a systematic analysis of the global burden of disease study 2017. Neuroepidemiology. 2020;54(2):171–179. doi:10.1159/000506396
8. Van Asch CJ, Luitse MJ, Rinkel GJ, et al. Incidence, case fatality, and functional outcome of intracerebral haemorrhage over time, according to age, sex, and ethnic origin: a systematic review and meta-analysis. Lancet Neurol. 2010;9(2):167–176. doi:10.1016/s1474-4422(09)70340-0
9. Li Z, Sun L, Zhang H, et al. Elevated plasma homocysteine was associated with hemorrhagic and ischemic stroke, but methylenetetrahydrofolate reductase gene C677T polymorphism was a risk factor for thrombotic stroke: a Multicenter Case-Control Study in China. Stroke. 2003;34(9):2085–2090. doi:10.1161/01.Str.0000086753.00555.0d
10. Wang Y, Li Z, Wang Y, et al. Chinese Stroke Center Alliance: a national effort to improve healthcare quality for acute stroke and transient ischaemic attack: rationale, design and preliminary findings. Stroke Vasc Neurol. 2018;3(4):256–262. doi:10.1136/svn-2018-000154
11. Ganguly P, Alam SF. Role of homocysteine in the development of cardiovascular disease. Nutr J. 2015;14:6. doi:10.1186/1475-2891-14-6
12. Gu HQ, Li DJ, Liu C, et al. %ggBaseline: a SAS macro for analyzing and reporting baseline characteristics automatically in medical research. Ann Transl Med. 2018;6(16):326. doi:10.21037/atm.2018.08.13
13. Genest J. Hyperhomocyst(e)inemia--determining factors and treatment. Can J Cardiol. 1999;15(Suppl B):35b–38b.
14. Jacques PF, Bostom AG, Wilson PW, et al. Determinants of plasma total homocysteine concentration in the Framingham Offspring cohort. Am J Clin Nutr. 2001;73(3):613–621. doi:10.1093/ajcn/73.3.613
15. Jacques PF, Rosenberg IH, Rogers G, et al. Serum total homocysteine concentrations in adolescent and adult Americans: results from the third National Health and Nutrition Examination Survey. Am J Clin Nutr. 1999;69(3):482–489. doi:10.1093/ajcn/69.3.482
16. Nygård O, Vollset SE, Refsum H, et al. Total plasma homocysteine and cardiovascular risk profile the Hordaland Homocysteine Study. Jama. 1995;274(19):1526–1533. doi:10.1001/jama.1995.03530190040032
17. Refsum H, Smith AD, Ueland PM, et al. Facts and recommendations about total homocysteine determinations: an expert opinion. Clin Chem. 2004;50(1):3–32. doi:10.1373/clinchem.2003.021634
18. Chrysohoou C, Panagiotakos DB, Pitsavos C, et al. The associations between smoking, physical activity, dietary habits and plasma homocysteine levels in cardiovascular disease-free people: the ‘ATTICA’ study. Vasc Med. 2004;9(2):117–123. doi:10.1191/1358863x04vm542oa
19. Halsted CH, Villanueva JA, Devlin AM, et al. Metabolic interactions of alcohol and folate. J Nutr. 2002;132(8 Suppl):2367s–2372s. doi:10.1093/jn/132.8.2367S
20. Thomas-Valdés S, Tostes M, Anunciação PC, et al. Association between vitamin deficiency and metabolic disorders related to obesity. Crit Rev Food Sci Nutr. 2017;57(15):3332–3343. doi:10.1080/10408398.2015.1117413
21. Refsum H, Nurk E, Smith AD, et al. The Hordaland Homocysteine Study: a community-based study of homocysteine, its determinants, and associations with disease. J Nutr. 2006;136(6Suppl):1731s–1740s. doi:10.1093/jn/136.6.1731S
22. Lim U, Cassano PA. Homocysteine and blood pressure in the third national health and nutrition examination survey, 1988–1994. Am J Epidemiol. 2002;156(12):1105–1113. doi:10.1093/aje/kwf157
23. Wu H, Wang B, Ban Q, et al. Association of total homocysteine with blood pressure in a general population of Chinese adults: a cross-sectional study in Jiangsu province, China. BMJ Open. 2018;8(6):e021103. doi:10.1136/bmjopen-2017-021103
24. Li WX, Liao P, Hu CY, et al. Interactions of methylenetetrahydrofolate reductase gene polymorphisms, folate, and homocysteine on Blood pressure in a Chinese hypertensive population. Clin Lab. 2017;63(4):817–825. doi:10.7754/Clin.Lab.2016.160918
25. Huo Y, Li J, Qin X, et al. Efficacy of folic acid therapy in primary prevention of stroke among adults with hypertension in China: the CSPPT randomized clinical trial. JAMA. 2015;313(13):1325–1335. doi:10.1001/jama.2015.2274
26. Wang F, Wang L, Du H, et al. Elevated total homocysteine predicts in-hospital pneumonia and poor functional outcomes in acute ischemic stroke. Curr Neurovasc Res. 2020;17(5):745–753. doi:10.2174/1567202617666201214111244
27. Pang X, Liu J, Zhao J, et al. Homocysteine induces the expression of C-reactive protein via NMDAr-ROS-MAPK-NF-κB signal pathway in rat vascular smooth muscle cells. Atherosclerosis. 2014;236(1):73–81. doi:10.1016/j.atherosclerosis.2014.06.021
28. Dai D, Sun Y, Liu C, et al. Association of Glasgow coma scale with total homocysteine levels in patients with hemorrhagic stroke. Ann Nutr Metab. 2019;75(1):9–15. doi:10.1159/000501191
29. Bernstein JE, Savla P, Dong F, et al. Inflammatory markers and severity of intracerebral hemorrhage. Cureus. 2018;10(10):e3529. doi:10.7759/cureus.3529
30. Zhou F, Chen B, Chen C, et al. Elevated homocysteine levels contribute to larger hematoma volume in patients with intracerebral hemorrhage. J Stroke Cerebrovasc Dis. 2015;24(4):784–788. doi:10.1016/j.jstrokecerebrovasdis.2014.11.005
31. Wang D, Wang W, Wang A, et al. Association of severity and prognosis with elevated homocysteine levels in patients with intracerebral hemorrhage. Front Neurol. 2020;11:571585. doi:10.3389/fneur.2020.571585
32. Ram S, Amit K, Vivek V, et al. Incremental accuracy of blood biomarkers for predicting clinical outcomes after intracerebral hemorrhage. J Stroke Cerebrovasc Dis. 2021;30(3):105537. doi:10.1016/j.jstrokecerebrovasdis.2020.105537
33. Esse R, Barroso M, Tavares De Almeida I, et al. The contribution of homocysteine metabolism disruption to endothelial dysfunction: state-of-the-art. Int J Mol Sci. 2019;20(4):867. doi:10.3390/ijms20040867
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
