Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 11 » Issue 1
Home-based neuromuscular electrical stimulation improves exercise tolerance and health-related quality of life in patients with COPD
Authors Coquart J , Grosbois J, Olivier C, Bart F, Castres I, Wallaert B
Received 26 January 2016
Accepted for publication 29 February 2016
Published 3 June 2016 Volume 2016:11(1) Pages 1189—1197
DOI https://doi.org/10.2147/COPD.S105049
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Richard Russell
Jérémy B Coquart,1 Jean-Marie Grosbois,2,3 Cecile Olivier,4 Frederic Bart,2 Ingrid Castres,1 Benoit Wallaert4
1Faculté des Sciences du Sport, Université de Rouen, CETAPS, EA 3832, Mont Saint Aignan, 2Service de Pneumologie, Centre Hospitalier de Béthune, Beuvry, 3Formaction Santé, Perenchies, 4Service de Pneumologie et Immunoallergologie, Centre Hospitalier Universitaire de Lille, Hôpital Calmette, Université de Lille 2, France
Background: This retrospective, observational study of a routine clinical practice reports the feasibility and efficiency of home-based pulmonary rehabilitation (PR), including transcutaneous neuromuscular electrical stimulation (NMES) or usual endurance physical exercise (UEPE), on exercise tolerance, anxiety/depression, and health-related quality of life (HRQoL) in patients with COPD.
Methods: Seventy-one patients with COPD participated in home-based PR with NMES (Group NMES [GNMES]), while 117 patients participated in home-based PR with the UEPEs (Group UEPE [GUEPE]). NMES was applied for 30 minutes twice a day, every day. The endurance exercises in GUEPE began with a minimum 10-minute session at least 5 days a week, with the goal being 30–45 minutes per session. Three upper and lower limb muscle strengthening exercises lasting 10–15 minutes were also proposed to both the groups for daily practice. Moreover, PR in both the groups included a weekly 90-minute session based on an educational needs assessment. The sessions comprised endurance physical exercise for GUEPE, NMES for GNMES, resumption of physical daily living activities, therapeutic patient education, and psychosocial support to facilitate health behavior changes. Before and after PR, functional mobility and physical exercise capacity, anxiety, depression, and HRQoL were evaluated at home.
Results: The study revealed that NMES significantly improved functional mobility (−18.8% in GNMES and −20.6% in GUEPE), exercise capacity (+20.8% in GNMES and +21.8% in GUEPE), depression (−15.8% in GNMES and −30.1% in GUEPE), and overall HRQoL (−7.0% in GNMES and −18.5% in GUEPE) in the patients with COPD, regardless of the group (GNMES or GUEPE) or severity of airflow obstruction. Moreover, no significant difference was observed between the groups with respect to these data (P>0.05).
Conclusion: Home-based PR including self-monitored NMES seems feasible and effective for severely disabled COPD patients with severe exercise intolerance.
Keywords: pulmonary rehabilitation, global management program, severity of airflow obstruction, chronic obstructive pulmonary disease, NMES
Introduction
Patients with COPD are characterized by dyspnea and physical exercise intolerance, which impair their ability to participate in physical activities and contribute to poor health-related quality of life (HRQoL).1,2 The effectiveness of pulmonary rehabilitation (PR) for these patients has been amply demonstrated,3 regardless of where it is performed (hospital, outpatient clinic, or home). A recent meta-analysis including 733 patients with COPD confirmed that home-based PR is a valuable intervention strategy to relieve dyspnea and improve exercise tolerance and HRQoL.4 Yet, to optimize self-care for these patients, a global management program is recommended that combines physical exercise, therapeutic patient education, and self-management.3,5 Although the usual endurance physical exercises (UEPEs) are often part of these global management programs,3 emerging therapies like transcutaneous neuromuscular electrical stimulation (NMES) can also be used.3,6
NMES involves the application of a low-level electrical current to targeted muscles through surface cutaneous electrodes, which depolarizes the motor neurons and induces involuntary muscle contractions.7 The main advantages of this therapy are that it does not provoke dyspnea (which can reinforce sedentary lifestyles),8 it is useful for severely disabled patients with COPD,9 and it can be used at home.10 NMES may therefore have the potential to break the vicious circle of negative emotions, unpleasant respiratory sensations, and poor exercise performance. Neder et al showed that home-based NMES for patients with “severe” or “very severe” COPD improved muscle strength and endurance, exercise tolerance, and perceived dyspnea during daily living activities.10 Home-based NMES is thus considered a nonpharmacological treatment for lower limb dysfunction and exercise intolerance in patients with “severe” or “very severe” COPD.
To the best of the authors’ knowledge, only Napolis et al assessed home-based NMES in patients with moderate COPD.11 The authors reported no significant improvement in quadriceps strength, symptom-limited peak oxygen uptake, endurance, or 6-minute walking distance after this home-based treatment in patients with “moderate” to “very severe” airflow obstruction. The authors concluded that, contrary to previously reported data from more severe patients, home-based NMES was not efficient for improving lower limb dysfunction and exercise intolerance in the group as a whole,11 thus suggesting a possible effect of COPD severity. As previously indicated by Vivodtzev et al,7 success with NMES may vary with disease severity, with less beneficial effects in patients with “moderate” COPD compared with patients more severely affected by the disease. However, the effect of home-based NMES on HRQoL has not, yet, been examined in patients with “moderate” airflow obstruction, but only in “severe” or “very severe” COPD.10
This retrospective observational study of a routine clinical practice was conducted in the north of France to compare the effects of home-based PR including NMES and PR with UEPE on exercise tolerance, anxiety/depression, and HRQoL in patients with COPD. We hypothesized that home-based NMES would be feasible and effective in improving exercise tolerance, anxiety/depression, and HRQoL in patients with COPD, but that the degree of improvements would depend on the disease severity.7
Materials and methods
Patients
Between 2012 and 2014, a home-based PR with NMES was proposed to 71 patients with COPD experiencing dyspnea during daily living activities (Group NMES: GNMES). NMES was proposed when patient performance of a 6-minute stepper test (6MST) was less than or equal to 250 strokes. Patients with higher performances were offered home-based PR with the UEPEs (Group UEPE: GUEPE). One hundred and seventeen patients were eligible for this routine clinical practice. Whatever the group, the patients chose home-based PR because of preference and/or because no PR center was nearby. COPD was confirmed in each patient by persistent post-bronchodilator airflow limitation (forced expiratory volume in 1 second/forced vital capacity: FEV1/FVC <0.70), according to Rabe et al.12 Exclusion criteria were dementia or poorly controlled psychiatric illness, neurological sequelae, or bone and joint diseases preventing physical activity. Patients receiving long-term oxygen therapy and/or noninvasive ventilation and/or continuous positive airways pressure and/or with multiple stable comorbidities were included in the study.
Moreover, six patients in GNMES were dropped from the program for the following reasons: death (n=2), exacerbation (n=2), aggravation of ischemic heart disease (n=1), and deterioration of the general status (n=1). For GUEPE, the dropouts included nine patients. The reasons were: death (n=1), exacerbation (n=4), lack of motivation (n=2), and hospitalization (n=2).
The study protocol was approved by the Observational Research Protocol Evaluation Committee of the French Language Society of Pulmonology, France. As the study data was collected as part of a PR prior to this retrospective study commencing the Observational Research Protocol Evaluation Committee advised written informed consent did not need to be obtained from the patients.
Global management program
The intervention program is detailed in Figure 1. Briefly, as described elsewhere,5 this individual home-based PR consisted of 90-minute sessions once a week based on an educational needs assessment. It comprised endurance physical exercise for GUEPE, NMES for GNMES and resumption of the physical activities of daily living, therapeutic patient education, and psychosocial support to facilitate health behavior changes for both the groups. Each weekly session was conducted under the direct supervision of a team member, although patients were expected to continue performing endurance physical exercise or NMES on their own on the other days of the week, according to a personalized action plan. This home-based PR lasted for 6 weeks for GNMES13 and 8 weeks for GUEPE.5,14
In GNMES, the patients self-administered NMES to the bilateral quadriceps with surface electrodes. For practical reasons, NMES was administered only on a muscle. Quadriceps was selected because deficits in strength of this muscle are frequently observed in the patients with COPD.6 A portable, user-friendly, dual-channel NMES stimulator was used (Cefar Rehab X2; DJO Incorporated, Guildford, UK). Based on the practical recommendations of Gloeckl et al,15 the NMES training program comprised: 1) a symmetrical biphasic square pulsed current at 50 Hz, 2) a duty cycle of 5 seconds on and 8 seconds off, and 3) pulses of 300 microseconds. The patients increased the intensity up to the maximum tolerated level. NMES was simultaneously applied to both thighs for 30 minutes twice every day. The patients were asked to lie down with the knees positioned at a fixed angle (~45°) and not to contract the muscles during NMES.
In GUEPE, individual endurance exercise on a cycle ergometer was performed at the target heart rate, initially in 10-minute sequences, at least 5 days per week, with the goal of reaching 30–45 minutes per sequence, in one or several sessions.5
For both groups, three upper and lower limb muscle strengthening exercises were systematically proposed (with instruction sheets), lasting 10–15 minutes per day, using weights and dumbbells and/or elastic bands. Each exercise comprised a series of ten repeated movements. A 1-minute recovery period was observed between exercises. Warm-up and stretching exercises were also recommended, together with balance exercises whenever necessary. The patients were encouraged to increase the duration of their daily living activities.
The patients were evaluated at home just before and after the intervention period. The patients performed the timed up-and-go test,16 which requires no specific equipment and is easy to execute at home, to quantify functional mobility, and the 6MST to evaluate physical exercise capacity. To circumvent the environmental constraints of the 6-minute walking test, which is difficult to carry out in the patient’s home, the 6MST was performed as previously described.17–19 This field exercise test is feasible for patients with pulmonary disease,14,17,19 and it detects improved functional capacity after PR in patients with COPD.5,19 The stepper (Go Sport, Grenoble, France), with a step height fixed at 20 cm, was placed near a wall to support patients if they became unbalanced or exhausted. During the 6MST, the patients could freely regulate their stepping rate to reach the highest number of strokes. At the end of the test, the number of strokes was recorded. According to Grosbois et al, a minimal clinically important difference (MCID) of 40 steps during 6MST has been proposed.5
Each evaluation also included the administration of three questionnaires (Hospital Anxiety and Depression [HAD] questionnaire,20 Maugeri Foundation Respiratory Failure [MRF-28] questionnaire,21,22 and the Visual Simplified Respiratory Questionnaire [VSRQ]).23 The HAD questionnaire determined the patient’s psychological state in terms of anxiety and depression.20 This questionnaire has a total of 14 items (seven items for each psychological state), with responses being scored on a scale of 0–3 (the higher the score, the higher is the frequency). For both scores (ie, anxiety and depression), a change of 1.5 units or greater in magnitude was considered to be the threshold for an MCID.24 The MRF-28 questionnaire is composed of 28 items covering three theoretical components (“daily activity”, “cognitive function”, and “invalidity”) and a total score. Each item is answered as either “true” or “false” and scored as 1 or 0, respectively.22 The components and total score are then summed and expressed as a percentage of the maximum possible score. The final scores range from 0 to 100, higher scores reflecting a higher degree of impairment.22 The MCID of MRF-28 is actually unknown.5,14 The VSRQ is a valid and reliable questionnaire to assess HRQoL, and it was especially developed for patients with COPD.23 It comprises eight visual analog scales ranging from 0 to 10, with a total score ranging from 0 to 80. A higher score indicates better HRQoL. The MCID of VSRQ is equal to 3.4 units.23
The questionnaires and exercise tests were chosen in light of recent studies in which home-based PR was evaluated in patients with pulmonary disease.5,14
Statistical analysis
Data are reported as mean and standard deviation. For all data, normal Gaussian distributions were verified by the Shapiro–Wilk test and homogeneity of variance by the Levene test. When the data did not pass the test for normality and/or homogeneity of variance, they were log-transformed.
For anthropometric and spirometric data, a general linear model with a two-way design (Groups: GNMES vs GUEPE, and severity of airflow limitation: moderate vs severe vs very severe) was used to compare the groups and examine the effect of the severity of airflow limitation. If significant differences were obtained, a Bonferroni post hoc test was conducted.
Given the initial difference in 6MST performance between the groups, effects after the intervention period were separately tested in each group (GNMES or GUEPE) from the general linear model (severity of airflow limitation) for repeated measures (before and after the intervention period). The sphericity was checked by the Mauchley test, and when it was not met, the significance of F-ratios was adjusted according to the Greenhouse–Geisser procedure or the Huyn–Feldt procedure. When significant differences were obtained, a Bonferroni post hoc test was conducted.
To compare the GNMES and GUEPE PRs, the data after the intervention period were expressed in percentage of baseline values, and then analyzed from the general linear model with a two-way design (groups and severity). Significant differences were identified from the Bonferroni post hoc test.
Statistical significance was set at P<0.05 and all analyses were performed with the Statistical Package for the Social Sciences (release 18.0; SPSS Inc., Chicago, IL, USA).
Results
At baseline, FEV1 was 41.1%±18.4% and 40.7%±17.4% of predicted FEV1 in GNMES and GUEPE, respectively. The severity of airflow limitation in GNMES and GUEPE was regarded as “moderate” in 31.0% and 28.2% patients, “severe” in 31.0% and 40.2% patients, and “very severe” in 38.0% and 31.6% patients, respectively (Table 1). Three or more comorbidities were found for 82% and 76% patients in GNMES and GUEPE, respectively. The main comorbidities were cardiovascular disease (hypertensive and ischemic heart disease, arrhythmia, and peripheral artery disease), metabolic disease (obesity, type 2 diabetes, and hypothyroidism), rheumatic disease (osteoporosis and osteoarthritis), and anxiety and depression. Patients were younger in GUEPE (P=0.034, Table 1). Moreover, the patients with severe COPD were older compared with patients with moderate airflow limitation (P=0.027), regardless of the group (GNMES or GUEPE). Body mass index (BMI) was significantly lower in patients with very severe COPD, regardless of the group (P<0.001).
The maximum tolerated intensity level from NMES group was 19.5±6.5 mA during the first week, and 30.1±10.9 mA during the last week.
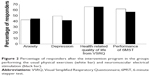
Timed up-and-go and 6MST performances were improved after the intervention period in both the groups (P≤0.01, Tables 2 and 3). Moreover, the number of strokes for the patients with moderate airflow limitation in GUEPE was significantly higher than that observed in patients with severe or very severe COPD (P<0.001, Table 3). For 6MST, the number of responders was 62% and 57% in GNMES and GUEPE, respectively (Figure 2). A significant reduction in the depression score was noted in both the groups (P<0.05, Tables 2 and 3), and the anxiety score was decreased in GUEPE after the intervention period (P=0.001). The number of responders was similar between the groups for anxiety (GNMES =45% vs GUEPE =43%). However, this percentage was higher in GUEPE compared to GNMES for depression (50% vs 45%, Figure 2). Although overall HRQoL was significantly improved in GNMES and GUEPE (P<0.05, Tables 2 and 3), only the scores from two subscales of the MRF-28 (quality of life in daily activity and invalidity) in GUEPE were reduced (P<0.05), with a lower invalidity score for patients with moderate COPD (P<0.05). For the VSRQ, the HRQoL improved in both the groups (P<0.05), with similar number of responders in GNMES and GUEPE (66% for both groups, Figure 2).
Table 4 compares the changes in HRQoL and performances between the groups (GNMES and GUEPE) according to the severity of airflow limitation. The reduction in the invalidity score of MRF-28 was significantly greater in GUEPE than in GNMES (P=0.020). No other significant difference was noted for HRQoL or performances between the groups (Table 4).
Discussion
The current study shows that NMES during home-based PR is feasible and effective, and can significantly improve timed up-and-go and 6MST performances, depression, and overall HRQoL in COPD patients with severe exercise intolerance, regardless of the severity of airflow obstruction.
In line with most previous studies, our results showed that NMES at home improves exercise tolerance8,10,13,25 and HRQoL in a large population with COPD,8,10 including patients with moderate airflow obstruction. Napolis et al reported no significant effect of home-based NMES on exercise tolerance in 30 patients with moderate to very severe airflow obstruction,11 which led to the hypothesis that responses might differ according to the COPD severity. Our results did not confirm this finding. However, in addition to including a larger sample, the discrepancies between our findings and those of Napolis et al might be explained by the population characteristics of our study,11 since GNMES included only patients with severe exercise intolerance (performing ≤250 strokes in 6MST). Thus, the current results suggest that NMES may be recommended even to COPD patients with severe exercise intolerance regardless of the airflow obstruction or the value of BMI.
Our results showed no significant difference between GNMES and GUEPE in the improvement of performances or HRQoL (except the invalidity score of the MRF-28) during home-based PR. Consequently, self-monitored NMES seemed to be as effective as the UEPEs for these COPD patients. Nevertheless, NMES’s main advantage is that it is feasible for severely disabled individuals,9 who are unable to endure exercise. It should be kept in mind that GNMES performed both NMES and voluntary strengthening exercises (similarly to GUEPE), two training modalities known to increase strength but through different neural mechanisms.26 In healthy human skeletal muscles, the neural adaptations induced by NMES seem to be mainly supraspinal, rather than the spinal and supraspinal adaptations from voluntary strengthening exercises.
In severely disabled patients with COPD (performance <400 m in 6-minute walking test), Vivodtzev et al showed an increase in muscle strength and endurance (on the quadriceps and calf muscles) after an NMES program (improved by +11% and +37%, respectively; P<0.03).13 They also noted a nonsignificant increase in the walking distance during an endurance shuttle test (+174 m; P=0.08). Even more interesting, the authors noted that NMES increased the mid-thigh and calf muscle cross-sectional areas (improved by +6% and +6%, respectively; P<0.05). Furthermore, the atrogin-1 protein content was downregulated after the NMES program, whereas the 70 kDa ribosomal S6 kinase content was upregulated. Collectively, these major findings suggest that NMES reduces muscle protein degradation and enhances protein synthesis, which promotes a net gain in muscle mass. As the lower limb muscles are particularly vulnerable to atrophy in COPD,6 NMES should be recommended especially to severely disabled patients as a way to gain muscle mass.
It has been well documented that home-based PR is an equivalent alternative to hospital-based PR in patients with COPD.3,4,14,27,28 Our study revealed that a personal educational intervention including either self-monitored and home-based PR with NMES (GNMES) or the UEPEs (GUEPE) was efficient to improve exercise tolerance and HRQoL. However, based on the literature, we optimized patient care by also including weekly self-management sessions5,29 and motivational interviews.5,30 It has been shown that self-management increases program engagement, improves HRQoL, reduces respiratory-related and all-cause hospital admissions, and even improves dyspnea,31–33 and that motivational interviews are more efficient when performed individually and repeatedly.34 This global management program combining NMES, therapeutic patient education, and self-management was also effective in COPD patients with lower exercise tolerance, regardless of the COPD severity.
The main limit of the current experimentation concerns the study design. This retrospective and observational study focused on a routine clinical practice in real life. Patients were thus not randomized and they were distributed into GNMES or GUEPE based on their performance in the 6MST. The patients in GNMES thus had lower exercise intolerance (performing ≤250 strokes in 6MST) than those in GUEPE. A controlled trial randomized for physical capacity regardless of the COPD severity is recommended to confirm our results. Moreover, because of the retrospective nature of the data analysis, it was not possible to evaluate the compliance of patients in both the groups. A prospective controlled randomized trial would have been better.
Conclusion
The current observational study, in the “real life”, reveals that NMES significantly improves exercise tolerance, depression, and overall HRQoL in patients with COPD, regardless of the severity of airflow obstruction. Home-based PR including self-monitored NMES seems to be feasible and effective in severely disabled individuals who are unable to perform the UEPEs.
Acknowledgments
The authors would like to thank the rehabilitation team who managed the patients: G Tywoniuk, S Duriez, F Urbain, V Wauquier, and M Lambinet. The authors would also like to thank Adair, France Oxygène, Homeperf, LVL Medical, Orkyn, Santélys, SOS Oxygène, Sysmed, VitalAire, and ARS Nord-Pas-de-Calais for their support of the home-based PR program.
Disclosure
JM Grosbois received financial support from Adair, France Oxygène, Homeperf, LVL, Orkyn, Santélys, SOS Oxygène, Sysmed, VitalAire and the ARS Nord Pas de Calais for home-based PR program. The other authors report no conflicts of interest in this work.
References
Amann M, Regan MS, Kobitary M, et al. Impact of pulmonary system limitations on locomotor muscle fatigue in patients with COPD. Am J Physiol Regul Integr Comp Physiol. 2010;299(1):314–324. | ||
Barreiro E, Gea J. Respiratory and limb muscle dysfunction in COPD. COPD. 2015;12(4):413–426. | ||
Spruit MA, Singh SJ, Garvey C, et al. An official American Thoracic Society/European Respiratory Society statement: key concepts and advances in pulmonary rehabilitation. Am J Respir Crit Care Med. 2013;188(8):e13–e64. | ||
Liu XL, Tan JY, Wang T, et al. Effectiveness of home-based pulmonary rehabilitation for patients with chronic obstructive pulmonary disease: a meta-analysis of randomized controlled trials. Rehabil Nurs. 2014;39(1):36–59. | ||
Grosbois J-M, Gicquello A, Langlois C, et al. Long term evaluation of home-based pulmonary rehabilitation in patients with chronic obstructive pulmonary disease. Int J Chron Obstruct Pulmon Dis. 2015;25(10):2037–2044. | ||
Maltais F, Decramer M, Casaburi R, et al. An official American Thoracic Society/European Respiratory Society statement: update on limb muscle dysfunction in chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2014;189(9):15–62. | ||
Vivodtzev I, Lacasse Y, Maltais F. Neuromuscular electrical stimulation of the lower limbs in patients with chronic obstructive pulmonary disease. J Cardiopulm Rehabil Prev. 2008;28(2):79–91. | ||
Vieira PJ, Chiappa AM, Cipriano G Jr, Umpierre D, Arena R, Chiappa GR. Neuromuscular electrical stimulation improves clinical and physiological function in COPD patients. Respir Med. 2014;108(4):609–620. | ||
Vivodtzev I, Pepin JL, Vottero G, et al. Improvement in quadriceps strength and dyspnea in daily tasks after 1 month of electrical stimulation in severely deconditioned and malnourished COPD. Chest. 2006;129(6):1540–1548. | ||
Neder JA, Sword D, Ward SA, Mackay E, Cochrane LM, Clark CJ. Home based neuromuscular electrical stimulation as a new rehabilitative strategy for severely disabled patients with chronic obstructive pulmonary disease. Thorax. 2002;57(4):333–337. | ||
Napolis LM, Dal Corso S, Neder JA, Malaguti C, Gimenes AC, Nery LE. Neuromuscular electrical stimulation improves exercise tolerance in chronic obstructive pulmonary disease patients with better preserved fat-free mass. Clinics. 2011;66(3):401–406. | ||
Rabe KF, Hurd S, Anzueto A, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am J Respir Crit Care Med. 2007;176(6):532–555. | ||
Vivodtzev I, Debigare R, Gagnon P, et al. Functional and muscular effects of neuromuscular electrical stimulation in patients with severe COPD: a randomized clinical trial. Chest. 2012;141(3):716–725. | ||
Grosbois JM, Le Rouzic O, Monge E, Bart F, Wallaert B. La réhabilitation respiratoire: évaluation de deux types de prise en charge, ambulatoire versus domicile. [Comparison of home-based and outpatient, hospital-based, pulmonary rehabilitation in patients with chronic respiratory diseases]. Rev Pneumol Clin. 2013;69(1):10–17. French. | ||
Gloeckl R, Marinov B, Pitta F. Practical recommendations for exercise training in patients with COPD. Eur Respir Rev. 2013;22(128):178–186. | ||
Podsiadlo D, Richardson S. The timed “Up & Go”: a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc. 1991;39(2):142–148. | ||
Delourme J, Stervinou-Wemeau L, Salleron J, Grosbois JM, Wallaert B. Six-minute stepper test to assess effort intolerance in interstitial lung diseases. Sarcoidosis Vasc Diffuse Lung Dis. 2012;29(2): 107–112. | ||
Borel B, Fabre C, Saison S, Bart F, Grosbois JM. An original field evaluation test for chronic obstructive pulmonary disease population: the six-minute stepper test. Clin Rehabil. 2010;24(1):82–93. | ||
Coquart JB, Lemaitre F, Castres I, Saison S, Bart F, Grosbois J. Reproducibility and sensitivity of the 6-minute stepper test in patients with COPD. COPD. 2015;12(5):533–538. | ||
Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67(6):361–370. | ||
Carone M, Bertolotti G, Anchisi F, Zotti AM, Donner CF, Jones PW. Analysis of factors that characterize health impairment in patients with chronic respiratory failure. Quality of Life in Chronic Respiratory Failure Group. Eur Respir J. 1999;13(6):1293–1300. | ||
Janssens JP, Heritier-Praz A, Carone M, et al. Validity and reliability of a French version of the MRF-28 health-related quality of life questionnaire. Respiration. 2004;71(6):567–574. | ||
Perez T, Arnould B, Grosbois JM, et al. Validity, reliability, and responsiveness of a new short Visual Simplified Respiratory Questionnaire (VSRQ) for health-related quality of life assessment in chronic obstructive pulmonary disease. Int J Chron Obstruct Pulmon Dis. 2009;4:9–18. | ||
Bhandari N, Jain T, Marolda C, ZuWallack RL. Comprehensive pulmonary rehabilitation results in clinically meaningful improvements in anxiety and depression in patients with chronic obstructive pulmonary disease. J Cardiopulm Rehabil Prev. 2013;33(2):123–127. | ||
Maddocks M, Nolan C, Man W, et al. Neuromuscular electrical stimulation to improve exercise capacity in patients with severe COPD: a randomised double-blind, placebo-controlled trial. Lancet Respir Med. 2016;4:27–36. | ||
Hortobagyi T, Maffiuletti NA. Neural adaptations to electrical stimulation strength training. Eur J Appl Physiol. 2011;111(10):2439–2449. | ||
Vieira DS, Maltais F, Bourbeau J. Home-based pulmonary rehabilitation in chronic obstructive pulmonary disease patients. Curr Opin Pulm Med. 2010;16(2):134–143. | ||
Maltais F, Bourbeau J, Shapiro S, et al. Effects of home-based pulmonary rehabilitation in patients with chronic obstructive pulmonary disease: a randomized trial. Ann Intern Med. 2008;149(12):869–878. | ||
Bourbeau J, Nault D, Dang-Tan T. Self-management and behaviour modification in COPD. Patient Educ Couns. 2004;52(3):271–277. | ||
Miller WR, Rollnick S. Motivational Interviewing: Preparing People for Change. New York: Guilford Press; 2002. | ||
Benzo R, Vickers K, Ernst D, Tucker S, McEvoy C, Lorig K. Development and feasibility of a self-management intervention for chronic obstructive pulmonary disease delivered with motivational interviewing strategies. J Cardiopulm Rehabil Prev. 2013;33(2):113–123. | ||
Bourbeau J, van der Palen J. Promoting effective self-management programmes to improve COPD. Eur Respir J. 2009;33(3):461–463. | ||
Zwerink M, Brusse-Keizer M, van der Valk PD, et al. Self management for patients with chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2014;3:CD002990. | ||
Lundahl B, Burke BL. The effectiveness and applicability of motivational interviewing: a practice-friendly review of four meta-analyses. J Clin Psychol. 2009;65(11):1232–1245. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.