Back to Journals » Clinical Interventions in Aging » Volume 17
Higher Concentration of Adrenocorticotropic Hormone Predicts Post-Stroke Depression
Authors Wang Y, Wang H, Sun W, Miao J, Liang W, Qiu X, Lan Y , Pan C , Li G, Zhao X, Zhu Z, Zhu S
Received 29 December 2021
Accepted for publication 30 March 2022
Published 5 April 2022 Volume 2022:17 Pages 417—427
DOI https://doi.org/10.2147/CIA.S356361
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Maddalena Illario
Yanyan Wang,1 He Wang,2 Wenzhe Sun,1 Jinfeng Miao,1 Wenwen Liang,1 Xiuli Qiu,1 Yan Lan,1 Chensheng Pan,1 Guo Li,1 Xin Zhao,1 Zhou Zhu,1 Suiqiang Zhu1
1Department of Neurology, Tongji Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, Hubei, 430030, People’s Republic of China; 2Department of Medical Affairs, Tongji Medical College, Tongji Hospital, Huazhong University of Science and Technology, Wuhan, Hubei, 430030, People’s Republic of China
Correspondence: Zhou Zhu; Suiqiang Zhu, Tel +86 18171081029 ; +86 13035101141, Fax +86 27-83663337, Email [email protected]; [email protected]
Background: Post-stroke depression (PSD) is the most common neuropsychiatric complication after stroke, seriously affecting the quality of survivors’ life. As one of the important causes of PSD, neuroendocrine mechanism has been widely studied in recent years. The main objective of this study was to investigate the relationship between adrenocorticotropic hormone (ACTH) on admission and PSD at 3 months.
Methods: This is a hospital-based prospective cohort study, which was conducted at three independent hospitals (Tongji Hospital, Wuhan First Hospital and Wuhan Central Hospital) between August 2018 and June 2019. A total of 768 ischemic stroke patients were finally eligible for analysis and categorized into equal tertiles according to the distribution of ACTH and the number of patients. The χ2-test, Mann–Whitney U-test and Kruskal–Wallis test were used to check for statistical significance. And restricted cubic spline (RCS) regression model was used to explore the non-linear relationship between continuous ACTH levels and PSD at 3 months.
Results: The optimal cut-off points of ACTH were as follows: (T1) 0.32– 20.55 pg/mL, (T2) 20.56– 39.79 pg/mL, (T3) 39.80– 143.40 pg/mL. A total of 305 patients (39.7%) were diagnosed as PSD at 3 months follow-up. Significant differences were found between the PSD and non-PSD groups in ACTH concentration (P = 0.001). After adjustment for all conventional confounders, the odds ratios of PSD were 1.735 (95% CI = 1.176– 2.560, P = 0.005) for the highest tertile of ACTH and 1.496 (95% CI = 1.019– 2.194, P = 0.040) for the middle tertile of ACTH, as compared with the lowest tertile. In multiple-adjusted RCS regression, continuous ACTH showed saturation effect relation with PSD risk after 31.02 pg/mL (P for nonlinear = 0.0143).
Conclusion: Higher ACTH level on admission is a significant and independent biomarker to predict the development of PSD at 3 months follow-up. Besides, saturation effect was revealed even if the underlying mechanism is unclear. For stroke patients, doctors should pay attention to the baseline ACTH for screening high-risk PSD in clinical practice.
Keywords: neuroendocrinology, HPA axis, adrenocorticotropic hormone, post-stroke depression, restricted cubic spline, saturation effect
Introduction
PSD is the most common mental illness after stroke, which significantly increases the disability rate, recurrence rate and mortality rate of stroke; seriously harms the quality of life of stroke survivors; and brings great pain and distress to patients and their families.1–3 According to a new review, PSD incidence was highest especially within 3 months after the acute event and the cumulative incidence of PSD was up to 52% within 5 years of stroke.4 There are many hypotheses about the pathogenesis of PSD, but the biological mechanisms remain unclear. Neuroendocrine disorders,5,6 especially hypothalamic-pituitary-adrenal (HPA) axis dysfunction,7 which is considered as a potential pathogenesis of PSD, has been aroused the concern of researchers and become a hot topic in recent years.
Hypothalamus, pituitary gland and adrenal cortex together form a complex neuroendocrine system, clinically known as the HPA axis. Corticosterone release hormone (CRH) secreted by the hypothalamus stimulates the pituitary gland to secrete ACTH, which in turn stimulates the adrenal cortex to secrete glucocorticoid (cortisol in human, corticosterone in rodents). Eventually, glucocorticoid is secreted into the blood and binds to specific receptors in multiple target tissues, exerting a powerful physiological effect.8 The activated HPA axis not only regulates homeostasis,9 stress response10 but also has a profound effect on emotional regulation.11
There are numerous studies on the relationship between HPA axis and mental illness. Previous studies have shown that patients suffering from generalized anxiety or major depression, manifested as high concentrations of CRH and exacerbated response to ACTH.12,13 It has also been suggested that elevated cortisol may be responsible for the emergence of psychotic symptoms in severe major depressive disorder.14–16 One study has shown that patients with psychotic major depression had higher cortisol levels throughout the afternoon compared to non-psychotic depressed or healthy subjects.17 Other empirical evidence suggested that the HPA axis played a key role in perinatal psychiatric disorders.18,19 Elevated cortisol levels in the second and third trimesters have been linked to prenatal depressive symptoms.18,20 A meta-analysis showed that women with major depression or anxiety disorders were blunted in responding to cortisol stress,21 and increased cortisol arousal often predicted increased vulnerability to depression.22 In addition, one study demonstrated that cortisol levels were an important mediator between childhood trauma and depressive symptoms.23 Yue et al wrote in their article: Many successful antidepressant treatments of depressive disorders using a variety of different antidepressant treatments are linked to the HPA axis.24
Thus, considering that the HPA axis played such an important role in mental illness and ACTH has proven to be an effective predictor of generalized anxiety or major depression, we hypothesized that the ACTH may also predict PSD. Further elucidation of the relationship between ACTH and PSD may ultimately lead to specific targeted treatments. The objective of our research today is to explore the association between ACTH on admission and PSD at 3 months.
Materials and Methods
Study Design and Subjects
As a multicenter prospective cohort study (Registration number: ChiCTR-ROC-17013993), our research was conducted at three independent hospitals (Tongji Hospital, Wuhan First Hospital and Wuhan Central Hospital) between August 2018 and June 2019. All patients involved in this study or their family members gave written informed consents according to the Declaration of Helsinki. The approval of the study for experiments was obtained from the Ethics Committee of Tongji Medical College, Huazhong University of Science and Technology (Approved No. of ethics committee: TJ-IRB20171108). A total of 1060 patients first-ever diagnosed stroke, including ischemic as well as hemorrhagic stroke, were consecutively enrolled and 768 patients were finally eligible for the research (Figure 1).
 |
Figure 1 The enrollment flow chart of this study. |
Inclusion and Exclusion Criteria
The inclusion criteria of this study were as follows: 1) ages 18 years and over; 2) admitted to hospital within 7 days after stroke onset, including ischemic as well as hemorrhagic stroke;and 3) stroke was confirmed by computed tomography (CT) or magnetic resonance imaging (MRI) scans.
Exclusion criteria were as follows: 1) brain dysfunction caused by other non-vascular causes (such as primary brain tumor, brain metastasis, subdural hematoma, post-seizure paralysis, brain trauma, etc.); 2) the history of dementia, depression and other mental illness; 3) aphasia, blindness, deafness and cognitive dysfunction [Mini-mental State Examination (MMSE)<17]; 4) transient ischemic attack (TIA) and subarachnoid hemorrhage; and 5) unable to complete the follow-up.
Data Collection
A standardized questionnaire was used upon admission to collect detailed information about each patient’s demographic and medical history, including age, sex, height, weight, sleep time, educational level, smoking history, drinking history, physical activity, hypertension, diabetes mellitus, hyperlipidemia and history of coronary heart disease (CHD).
Blood samples were obtained from the medial cubital vein at fasting in the early morning of the second day (within 24 hours of admission). The concentrations of fasting C-peptide (FCP), adrenocorticotropic hormone (ACTH), cortisol, total WBC count (WBC) and neutrophil count (NEU) were measured in clinical laboratory of Tongji Hospital. FCP, ACTH and cortisol were measured by Abbott chemiluminescence, Roche electro-chemiluminescence immunoassay and Beckman DXI chemiluminescence, respectively. WBC and NEU were measured by fluorescence staining flow cytometry. The inflammatory factors, including interleukin (IL-1β, IL-6, IL-10, IL-18), tumor necrosis factor (TNF-α), interferon (IFN-γ) as well as brain-derived neurotrophic factor (BDNF) were measured using a solid-phase sandwich enzyme-linked immunosorbent assay kit (CUSABIO, China) according to the manufacturer’s specifications in Kind star Company, Wuhan, which was a nationwide comprehensive clinical medical testing agency. To minimize assay variance, all samples were analyzed on the same day in duplicate in a random order by a technician blind to the clinical diagnoses; the intra-assay coefficients were <5%.25
The National Institutes of Health Stroke Scale (NIHSS), Barthel index (BI), modified Rankin scale (mRS) were evaluated immediately after admission. The 17-item Hamilton Rating Scale for Depression (HAMD-17) had been proved to have good reliability and validity in Chinese population,26 which therefore was used to measure the severity of depressive symptoms at 3 and 6 months after ischemic stroke onset. This paper only presents the data analysis results of 3 months. All psychological evaluations were performed by two experienced psychiatrists who were blinded to other clinical and laboratory findings after receiving standardized training. The HAMD-17 was mainly administered in the form of face-to-face interviews in the hospital. For a small number of patients who could not come to the hospital, HAMD-17 was evaluated in the form of WeChat video and phone. Participants who met DSM-V diagnostic criteria (depression caused by another medical condition) along with HAMD-17 score >7 were diagnosed as PSD.
Statistical Analysis
Continuous variables were presented as medians [interquartile range (IQR)] because of skewed distribution while categorical variables were expressed as frequencies (percentages).
Patients were classified into two groups by HAMD-17 scores and three groups by ACTH tertiles. Group differences were assessed by χ2 tests for categorical variables and nonparametric Mann–Whitney U-test/Kruskal–Wallis test for continuous variables. The associations between ACTH levels and 3 months PSD were investigated with multivariate-adjusted binary logistic regression models, which using a backward stepwise method with input of variables if p-value <0.05 and backward elimination if p-value >0.05.27 The lowest tertile (0.32–20.55) was defined as the reference group. After adjusting for traditional confounders and main baseline variables related to PSD (which were explicitly listed in great detail in Table 1), the odds ratios (ORs) and their 95% confidence intervals (CIs) were obtained.28
 |
Table 1 Multivariate Adjusted Odds Ratios for the Association Between ACTH Levels and PSD at 3 months |
In addition, RCS regression model was conducted to provide more precise estimates and examine the shape of the associations between ACTH as a continuous measure and 3 months PSD. The reference point for ACTH was the median (11.20 pg/mL) of the reference group (the lowest tertile), and the OR was adjusted for all confounding variables (the same variables as model 3 in Table 1).29 To balance best fit and overfitting in the spline, the number of knots, between three and seven, was chosen as the lowest value for the Akaike information criterion.30
Overall, a two-sided value of p<0.05 was considered statistically significant. Data analysis were performed with Statistical Program for Social Sciences (SPSS) statistical software (version 25, Chicago, IL, USA) and R version 4.0.3. The R packages “rms” and “ggplot2” were applied.
Results
Baseline Characteristics of Patients in Non-PSD Group and PSD Group
In total, 768 patients with acute ischemic stroke were consecutively recruited in this study. Of all these potential subjects, 305 (39.7%) developed PSD at 3 months after ischemic stroke onset. Table 2 shows a comparison of baseline information between the non-PSD and PSD groups. The PSD group had a higher proportion of female (p = 0.009), lower proportion of physical activity (p = 0.002), higher NIHSS score (p < 0.001), lower BI score (p < 0.001), higher m RS score (p < 0.001). As for serum biochemicals, the PSD group showed higher level of fasting C-peptide (p=0.011), higher level of ACTH (p=0.001), higher white blood cell count (p=0.001), higher neutrophil count (p=0.001) and higher level of IL.6 (p=0.016).
 |
Table 2 Baseline Characteristics of Patients without and with PSD at 3 Months |
Characteristics of All Patients in ACTH Tertiles
Of the 768 patients, 22.4% were female and 77.6% were male. The mean age of them was 59 years (Table 3). All participants were divided into three subgroups according to tertiles of ACTH levels, which ensured the most categories with adequate number of patients per subgroups28 between the range of 0.32 and 143.40pg/mL (T1, 255 patients; T2, 257 patients; T3, 256 patients). The cut-off values for this stratification on the ACTH level into tertiles were as follows: (T1) 0.32–20.55pg/mL, (T2) 20.56–39.79pg/mL, and (T3) 39.80–143.40pg/mL. Table 3 summarized the characteristics of the patients by the tertiles of ACTH. Compared to patients with lower ACTH, those with higher ACTH were more likely to be younger (p=0.001); had lower proportions of female (p<0.001) and hypertension (p=0.027); had higher proportions of drinking (p=0.019); had higher scores of NIHSS (p=0.004), m RS (p<0.001) and HAMD at 3 months (p<0.001).
 |
Table 3 Characteristics of Patients with Ischemic Stroke According to ACTH Tertiles |
Association Between the Level of ACTH and PSD at 3 Months
In Table 1, unadjusted and multivariate-adjusted binary logistic regression models were used to estimate the association between the level of ACTH and PSD at 3 months. In unadjusted binary logistic regression model, with the lowest tertile of ACTH taken as the reference, both highest and middle tertile of ACTH were independent risk predictor of PSD with an unadjusted OR of 1.701 (95% CI=1.185–2.443, P=0.004) and 1.717 (95% CI=1.196–2.464, P= 0.003), respectively. After adjusting for confounders including age, sex, BMI, education levels, sleep time, physical activity, smoking, drinking, hypertension, diabetes mellitus, hyperlipidemia, coronary heart disease, baseline NIHSS, mRS and BI scores, the highest tertile of ACTH was remained significant independently associated with the prevalence of PSD (model 1: OR = 1.790, 95% CI = 1.230–2.605, P=0.002; model 2: OR = 1.790, 95% CI = 1.230–2.605, P=0.002; model 3: OR = 1.735, 95% CI = 1.176–2.560, P=0.005). Similar results were found in the middle tertile of ACTH (model 1: OR = 1.660, 95% CI = 1.147–2.401, P=0.007; model 2: OR = 1.660, 95% CI = 1.147–2.401, P=0.007; model 3: OR =1.496, 95% CI = 1.019–2.194, P=0.040).
Furthermore, RCS regression model was used to confirm the non-linear relationship between continuous ACTH levels and PSD at 3 months (P for nonlinear=0.0143, Figure 2). The RCS curve showed that there was saturation effect relation between ACTH and the OR value of PSD at 3 months. When the level of ACTH <31.02pg/mL, OR value showed an obvious growth trend. However, when ACTH >31.02pg/mL, as the ACTH concentration increases gradually, OR value did not change significantly.
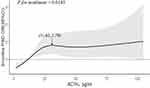 |
Figure 2 Association of ACTH levels on admission with risk of PSD at 3 months’ follow-up. Odds ratios and 95% confidence intervals derived from RCS regression. Odds ratios were estimated using logistic regression model, adjusting for the same variables as model 3 in Table 1. |
Discussions
In this multicenter prospective cohort study, we aimed to explore the association between ACTH and the development of PSD outcome. The final results suggested that higher ACTH level on admission is a significant and independent biomarker to predict the development of PSD at 3 months’ follow-up. In addition, we found that there was saturation effect relation between continuous ACTH and the risk of PSD at 3 months. To a certain extent, our findings provide useful evidence for the neuroendocrine mechanism of PSD.
A total of 39.7% of acute ischemic stroke patients were diagnosed as PSD at 3 months in this study, which is similar to the incidence reported in previous studies.31,32 Our results suggested that female and those who are physically inactive are at higher risk for PSD, which were consistent with previous studies.33,34 Our results also demonstrated that patients with PSD had significantly increased stroke severity and worse functional outcome, which was the same as other studies.35,36 A reasonable explanation of this phenomenon might be that PSD patients were more likely exposed to high-risk health behaviors such as sedentary lifestyle, smoking and nonadherence to secondary prevention measures.28 As shown in Table 2, PSD patients had higher fasting C-peptide levels. The underlying mechanism might be that high levels of fasting C-peptide reflect insulin resistance and disrupted glucose metabolism, which contributes to depression.31 Furthermore, previous studies have confirmed that neutrophil count25 as well as IL.637 were involved in the development of PSD and our study came to the same conclusion.
In recent years, psychiatrists have become increasingly interested in the relationship between HPA axis and depression. Nevertheless, as for HPA axis disorder and depression, which is the cause and which is the effect, there is no unified conclusion at present. Some studies suggested that HPA axis disorder is the consequence or an epiphenomenon of depression. For example, a study showed that depressed patients present with increased cortisol levels and attenuated immune responses.38 Another study also described that depressed patients have increased circulating levels of proinflammatory cytokines, which can further stimulate the HPA axis and cortisol.39 A reasonable explanation is that anxiety and depression patients are often accompanied by sleep disorders,40 which can trigger vascular inflammation to a certain extent,41,42 and then lead to the increase in peroxides, free radicals and glucocorticoids in the body, and the excessive activation of cytokines, and eventually develop into endocrine disorders. Other studies, however, take the opposite view. Pariante et al8 described the relationship between HPA axis hyperactivity and depression graphically as a chicken–egg relationship, insisting that HPA axis disorder is a risk factor predisposing to the development of depression. A widely accepted potential mechanism was outlined as follows. The HPA axis is a primary stress system in the human body, which is sensitive to both acute and chronic stress.10,43 As an important mediator, glucocorticoid regulates stress responses through the negative feedback regulation of the HPA axis by binding to the glucocorticoid receptor (GR).8,44 Under pathological conditions, the impairment of the GR-mediated negative feedback system of the HPA axis results in constant HPA axis hyperactivity and chronically high glucocorticoid levels, leading to the development of depressive disorders.45–47 Besides, the hippocampus and the prefrontal cortex are involved in the negative feedback regulation of the HPA axis and in the pathogenesis of depression.47–49 Furthermore, increased inflammation as another important biological finding in major depression is often associated with hyperactivity of the HPA axis, although the underlying molecular and clinical mechanisms are still unclear.50 IL-6, a widely studied pro-inflammatory cytokine, has been found to be a factor associated with major depressive disorder and increased IL-6 activity may cause depression through activation of HPA axis or influence of the neurotransmitter metabolism.51 Carvalho et al also described increased plasma IL-6 and increased plasma cortisol levels in the same depressed individuals,52 which further confirmed the notion that increased inflammation and cortisol hypersecretion are indeed coexistent and related biological abnormalities.
Considering there are many similarities between the pathogenesis of depression and PSD, it is reasonable to deem that there is a close link between hyperactivity of HPA axis and PSD. Our data show that as ACTH levels go up, so do cortisol levels and pro-inflammatory cytokine IL-6 levels (Table 3), which was consistent with previous studies.50–52 It seems that our study supports the latter conclusion because the risk of PSD at 3 months increases with ACTH levels on admission (Table 1 and Figure 2). However, we did not measure ACTH dynamically at follow-up, so we were unable to understand the serum ACTH levels of patients after the onset of PSD. We therefore fail to know whether PSD will further affect ACTH. A reasonable hypothesis is that HPA axis disorder and PSD influence each other, cause and effect each other, leading to vicious cycle, but the specific mechanism still needs further study.
Strengths and Limitations
The main advantage of this study is that it is a prospective cohort study, which enhances the credibility of etiological inferences. In addition, the sample size of the study was large enough and we adjusted many confounders in different models to make the results more referential. Furthermore, compared with microRNAs, ACTH, as a common objective biomarker, is more readily available. Finally, though further studies are still needed to confirm the association between the ACTH level on admission and the risk of PSD at 3 months, our study results revealed the saturation effect between them.
However, this study had several limitations. First of all, patients with dysarthria, aphasia or other diseases were excluded, and these excluded patients might be suffered from depressive symptoms. This might cause a selection bias, resulting in a lower rate of PSD than actual data. Moreover, the loss rate of follow-up may reduce statistical power of the analyses. Another limitation is the sex imbalance in our study population, with female accounting for only 22.4%, which is caused by the fact that the number of male stroke patients in the Neurology department of Tongji Hospital is far more than that of female. Therefore, more studies are needed to explore the relationship between ACTH and PSD in other populations with adequate number of women and other geographic populations.
Conclusions
Higher ACTH level on admission is a significant and independent biomarker to predict the development of PSD at 3 months’ follow-up. Further investigations are needed to clarify the underlying mechanism of saturation effect relation between continuous ACTH and PSD. For Chinese elderly stroke patients, doctors should pay attention to the baseline ACTH for screening high-risk PSD in clinical practice.
Abbreviations
PSD, post-stroke depression; HPA, hypothalamic pituitary adrenal; CRH, corticotropin releasing hormone; ACTH, adrenocorticotropic hormone; GR, glucocorticoid receptor; HAMD-17, 17-item Hamilton Rating Scale for Depression; TNF-α, tumor necrosis factor-α; BDNF, brain-derived neurotrophic factor; BMI, body mass index; CHD, coronary heart disease; WBC, white blood count; NEU, neutrophil count; IL, interleukin; IFN, interferon; NIHSS, The National Institutes of Health Stroke Scale; BI, Barthel Index; mRS, modified Rankin Scale; RCS, restricted cubic spline.
Data Sharing Statement
The database used in the current study are available from the corresponding authors on reasonable request.
Ethics Approval and Consent to Participate
All patients involved in this study or their family members gave written informed consents according to the Declaration of Helsinki. The approval of the study for experiments was obtained from the Ethics Committee of Tongji Medical College, Huazhong University of Science and Technology (Approved No. of ethics committee: TJ-IRB20171108).
Acknowledgments
We would like to acknowledge all participants of this project and investigators for collecting data.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work. SZ and ZZ had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Funding
This work was financially supported by the National Key R&D Program of China (grant number 2017YFC1310000), Hubei Technological Innovation Special Fund (grant number 2019ACA132), and National Natural Science Fund of China (grant numbers 82101605, 82001218, and 82171465). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Disclosure
The authors report no conflicts of interest for this work nor concerning the materials or methods used in this study nor the findings specified in this paper.
References
1. Villa RF, Ferrari F, Moretti A. Post-stroke depression: mechanisms and pharmacological treatment. Pharmacol Ther. 2018;184:131–144. doi:10.1016/j.pharmthera.2017.11.005
2. Ayerbe L, Ayis S, Crichton S, Wolfe CD, Rudd AG. The long-term outcomes of depression up to 10 years after stroke; the South London stroke register. J Neurol Neurosurg Psychiatry. 2014;85(5):514–521. doi:10.1136/jnnp-2013-306448
3. Robinson RG, Jorge RE. Post-stroke depression: a review. Am J Psychiatry. 2016;173(3):221–231. doi:10.1176/appi.ajp.2015.15030363
4. Chun HY, Ford A, Kutlubaev MA, Almeida OP, Mead GE. Depression, anxiety, and suicide after stroke: a narrative review of the best available evidence. Stroke. 2021;53:1402–1410.
5. Zhang E, Liao P. Brain-derived neurotrophic factor and post-stroke depression. J Neurosci Res. 2020;98(3):537–548. doi:10.1002/jnr.24510
6. Taroza S, Rastenyte D, Burkauskas J, Podlipskyte A, Mickuviene N. Lower serum free triiodothyronine levels are associated with symptoms of depression after ischemic stroke. J Psychosom Res. 2019;122:29–35. doi:10.1016/j.jpsychores.2019.04.018
7. Loubinoux I, Kronenberg G, Endres M, et al. Post-stroke depression: mechanisms, translation and therapy. J Cell Mol Med. 2012;16(9):1961–1969. doi:10.1111/j.1582-4934.2012.01555.x
8. Pariante CM, Lightman SL. The HPA axis in major depression: classical theories and new developments. Trends Neurosci. 2008;31(9):464–468. doi:10.1016/j.tins.2008.06.006
9. Joseph DN, Whirledge S. Stress and the HPA axis: balancing homeostasis and fertility. Int J Mol Sci. 2017;18(10):10. doi:10.3390/ijms18102224
10. Gaffey AE, Bergeman CS, Clark LA, Wirth MM. Aging and the HPA axis: stress and resilience in older adults. Neurosci Biobehav Rev. 2016;68:928–945. doi:10.1016/j.neubiorev.2016.05.036
11. Barden N. Implication of the hypothalamic-pituitary-adrenal axis in the physiopathology of depression. J Psychiatry Neurosci. 2004;29(3):185–193.
12. Sousa VC, Mantas I, Stroth N, et al. P11 deficiency increases stress reactivity along with HPA axis and autonomic hyperresponsiveness. Mol Psychiatry. 2021;26(7):3253–3265. doi:10.1038/s41380-020-00887-0
13. McEwen BS. Physiology and neurobiology of stress and adaptation: central role of the brain. Physiol Rev. 2007;87(3):873–904. doi:10.1152/physrev.00041.2006
14. Nandam LS, Brazel M, Zhou M, Jhaveri DJ. Cortisol and major depressive disorder-translating findings from humans to animal models and back. Frontiers in Psychiatry. 2020;10. doi:10.3389/fpsyt.2019.00974
15. Holsboer F, Ising M. Central CRH system in depression and anxiety - evidence from clinical studies with CRH1 receptor antagonists. Eur J Pharmacol. 2008;583(2–3):350–357. doi:10.1016/j.ejphar.2007.12.032
16. Keller J, Gomez R, Williams G, et al. HPA axis in major depression: cortisol, clinical symptomatology and genetic variation predict cognition. Mol Psychiatr. 2017;22(4):527–536. doi:10.1038/mp.2016.120
17. Belanoff JK, Kalehzan M, Sund B, Fleming Ficek SK, Schatzberg AF. Cortisol activity and cognitive changes in psychotic major depression. Am J Psychiatry. 2001;158(10):1612–1616. doi:10.1176/appi.ajp.158.10.1612
18. Seth S, Lewis AJ, Galbally M. Perinatal maternal depression and cortisol function in pregnancy and the postpartum period: a systematic literature review. BMC Pregnancy Childbirth. 2016;16(1):124. doi:10.1186/s12884-016-0915-y
19. Dickens MJ, Pawluski JL. The HPA axis during the perinatal period: implications for perinatal depression. Endocrinology. 2018;159(11):3737–3746. doi:10.1210/en.2018-00677
20. Orta OR, Gelaye B, Bain PA, Williams MA. The association between maternal cortisol and depression during pregnancy, a systematic review. Arch Womens Ment Health. 2018;21(1):43–53. doi:10.1007/s00737-017-0777-y
21. Zorn JV, Schur RR, Boks MP, Kahn RS, Joels M, Vinkers CH. Cortisol stress reactivity across psychiatric disorders: a systematic review and meta-analysis. Psychoneuroendocrinology. 2017;77:25–36. doi:10.1016/j.psyneuen.2016.11.036
22. Hardeveld F, Spijker J, Vreeburg SA, et al. Increased cortisol awakening response was associated with time to recurrence of major depressive disorder. Psychoneuroendocrinology. 2014;50:62–71. doi:10.1016/j.psyneuen.2014.07.027
23. Ju Y, Wang M, Lu X, et al. The effects of childhood trauma on the onset, severity and improvement of depression: the role of dysfunctional attitudes and cortisol levels. J Affect Disord. 2020;276:402–410. doi:10.1016/j.jad.2020.07.023
24. Yue L, Xiao-Lin H, Tao S. The effects of chronic repetitive transcranial magnetic stimulation on glutamate and gamma-aminobutyric acid in rat brain. Brain Res. 2009;1260:94–99. doi:10.1016/j.brainres.2009.01.009
25. Sun W, Miao J, Song Y, et al. Systemic low-grade inflammation and depressive symptomology at chronic phase of ischemic stroke: the chain mediating role of fibrinogen and neutrophil counts. Brain Behav Immun. 2022;100:332–341. doi:10.1016/j.bbi.2021.10.011
26. Zheng YP, Zhao JP, Phillips M, et al. Validity and reliability of the Chinese Hamilton depression rating scale. Br J Psychiatry. 1988;152:660–664. doi:10.1192/bjp.152.5.660
27. Sun WZ, Li G, Song Y, et al. A web based dynamic MANA Nomogram for predicting the malignant cerebral edema in patients with large hemispheric infarction. BMC Neurol. 2020;20(1). doi:10.1186/s12883-020-01935-6
28. Huang G, Chen H, Wang Q, et al. High platelet-to-lymphocyte ratio are associated with post-stroke depression. J Affect Disord. 2019;246:105–111. doi:10.1016/j.jad.2018.12.012
29. Wang A, Xu J, Chen G, et al. Oxidized low-density lipoprotein predicts recurrent stroke in patients with minor stroke or TIA. Neurology. 2018;91(10):e947–e55. doi:10.1212/WNL.0000000000006118
30. Johannesen CDL, Langsted A, Mortensen MB, Nordestgaard BG. Association between low density lipoprotein and all cause and cause specific mortality in Denmark: prospective cohort study. BMJ Brit Med J. 2020;371:m4266.
31. Wang YY, Sun WZ, Miao JF, et al. Higher fasting C-peptide is associated with post-stroke depression: a multicenter prospective cohort study. BMC Neurol. 2021;21(1). doi:10.1186/s12883-021-02413-3
32. Ayerbe L, Ayis S, Wolfe CDA, Rudd AG. Natural history, predictors and outcomes of depression after stroke: systematic review and meta-analysis. Brit J Psychiat. 2013;202(1):14–21. doi:10.1192/bjp.bp.111.107664
33. Pascoe MC, Parker AG. Physical activity and exercise as a universal depression prevention in young people: a narrative review. Early Interv Psychia. 2019;13(4):733–739. doi:10.1111/eip.12737
34. De Ryck A, Brouns R, Geurden M, Elseviers M, De Deyn PP, Engelborghs S. Risk factors for poststroke depression: identification of inconsistencies based on a systematic review. J Geriatr Psych Neur. 2014;27(3):147–158. doi:10.1177/0891988714527514
35. Li G, Miao JF, Sun WH, et al. Lower serum uric acid is associated with post-stroke depression at discharge. Frontiers in Psychiatry. 2020;11:52.
36. Qiu XL, Miao JF, Lan Y, et al. Association of cerebral artery stenosis with post-stroke depression at discharge and 3 months after ischemic stroke onset. Frontiers in Psychiatry. 2020;11. doi:10.3389/fpsyt.2020.585201
37. Spalletta G, Cravello L, Imperiale F, et al. Neuropsychiatric symptoms and interleukin-6 serum levels in acute stroke. J Neuropsychiatry Clin Neurosci. 2013;25(4):255–263. doi:10.1176/appi.neuropsych.12120399
38. Zhan HQ, Huang F, Yan FL, et al. Alterations in splenic function and gene expression in mice with depressive-like behavior induced by exposure to corticosterone. Int J Mol Med. 2017;39(2):327–336. doi:10.3892/ijmm.2017.2850
39. Wang H, Ahrens C, Rief W, Gantz S, Schiltenwolf M, Richter W. Influence of depression symptoms on serum tumor necrosis factor-alpha of patients with chronic low back pain. Arthritis Res Ther. 2010;12(5):R186. doi:10.1186/ar3156
40. Aizawa H, Cui WP, Tanaka K, Okamoto H. Hyperactivation of the habenula as a link between depression and sleep disturbance. Front Hum Neurosci. 2013;7. doi:10.3389/fnhum.2013.00826
41. Blair LM, Porter K, Leblebicioglu B, Christian LM. Poor sleep quality and associated inflammation predict preterm birth: heightened risk among African Americans. Sleep. 2015;38(8):1259–1267. doi:10.5665/sleep.4904
42. Bandyopadhyay A, Sigua NL. What is sleep deprivation? Am J Respir Crit Care Med. 2019;199(6):P11–P2. doi:10.1164/rccm.1996P11
43. Beurel E, Toups M, Nemeroff CB. The bidirectional relationship of depression and inflammation: double trouble. Neuron. 2020;107(2):234–256. doi:10.1016/j.neuron.2020.06.002
44. Adzic M, Djordjevic J, Djordjevic A, et al. Acute or chronic stress induce cell compartment-specific phosphorylation of glucocorticoid receptor and alter its transcriptional activity in Wistar rat brain. J Endocrinol. 2009;202(1):87–97. doi:10.1677/JOE-08-0509
45. Sapolsky RM, Romero LM, Munck AU. How do glucocorticoids influence stress responses? Integrating permissive, suppressive, stimulatory, and preparative actions. Endocr Rev. 2000;21(1):55–89. doi:10.1210/edrv.21.1.0389
46. Pariante CM. Risk factors for development of depression and psychosis glucocorticoid receptors and pituitary implications for treatment with antidepressant and glucocorticoids. Ann N Y Acad Sci. 2009;1179:144–152.
47. Wei K, Xu YZ, Zhao ZX, et al. Icariin alters the expression of glucocorticoid receptor, FKBP5 and SGK1 in rat brains following exposure to chronic mild stress. Int J Mol Med. 2016;38(1):337–344. doi:10.3892/ijmm.2016.2591
48. Guidotti G, Calabrese F, Anacker C, Racagni G, Pariante CM, Riva MA. Glucocorticoid receptor and FKBP5 expression is altered following exposure to chronic stress: modulation by antidepressant treatment. Neuropsychopharmacology. 2013;38(4):616–627. doi:10.1038/npp.2012.225
49. Djordjevic A, Adzic M, Djordjevic J, Radojcic MB. Stress type dependence of expression and cytoplasmic-nuclear partitioning of glucocorticoid receptor, Hsp90 and Hsp70 in Wistar rat brain. Neuropsychobiology. 2009;59(4):213–221. doi:10.1159/000223733
50. Pariante CM. Why are depressed patients inflamed? A reflection on 20 years of research on depression, glucocorticoid resistance and inflammation. Eur Neuropsychopharmacol. 2017;27(6):554–559. doi:10.1016/j.euroneuro.2017.04.001
51. Ting EY, Yang AC, Tsai SJ. Role of interleukin-6 in depressive disorder. Int J Mol Sci. 2020;21(6):2194. doi:10.3390/ijms21062194
52. Carvalho LA, Juruena MF, Papadopoulos AS, et al. Clomipramine in vitro reduces glucocorticoid receptor function in healthy subjects but not in patients with major depression. Neuropsychopharmacology. 2008;33(13):3182–3189. doi:10.1038/npp.2008.44
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
