Back to Journals » International Journal of General Medicine » Volume 15
High-Sensitivity Troponin I is an Indicator of Poor Prognosis in Patients with Severe COVID-19 Related Pneumonia
Authors Liu Y, Lu P, Peng L, Chen J, Hu C
Received 31 March 2022
Accepted for publication 22 June 2022
Published 6 September 2022 Volume 2022:15 Pages 7113—7121
DOI https://doi.org/10.2147/IJGM.S368019
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Yongjun Liu,1,2,* Peng Lu,2,3,* Lei Peng,2,3 Jie Chen,4 Chunlin Hu2,3
1Department of Critical Care Medicine, The First Affiliated Hospital of Sun Yat-sen University, Guangzhou, 510080, People’s Republic of China; 2Department of Critical Care Medicine, Union Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, 430022, People’s Republic of China; 3Department of Emergency Medicine, The First Affiliated Hospital of Sun Yat-sen University, Guangzhou, 510080, People’s Republic of China; 4Department of Critical Care Medicine, Dongguan People’s Hospital, Dongguan, 523059, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Chunlin Hu, Department of Emergency Medicine, The First Affiliated Hospital of Sun Yat-sen University, Guangzhou, 510080, People’s Republic of China, Email [email protected] Jie Chen, Department of Critical Care Medicine, Dongguan People’s Hospital, Dongguan, 523059, People’s Republic of China, Email [email protected]
Objective: Critical covid-19 patients have complications with acute myocardial injury is still unclear. We observed a series of critically ill patients, paying particular attention to the impact of myocardial injury at admission on short-term outcome.
Methods: We prospectively collected and analyzed data from a series of severe covid-19 patients confirmed by real-time RT-PCR. Data were obtained from electronic medical records including clinical charts, nursing records, laboratory findings, and chest x-rays were from Feb 8, 2020, to April 7, 2020. The Acute Physiology and Chronic Health Evaluation (APACHE II) score, CURB-65 Pneumonia Severity Score, Sequential Organ Failure Assessment (SOFA) Score and pneumonia severity index (PSI) score were made within 24 hours of admission. Cardiac injury was diagnosed as hs-cTnI were above > 28 pg/mL. The short-term outcome was defined as mortality in hospital.
Results: A total of 100 patients met the diagnostic criteria of severe patients with COVID-19 during 2020.02.08– 2020.04.07. The CURB 65, APACH2, SOFA, and PSI score were significantly higher in Critical group than in Severe group. Univariate regression analysis showed that oxygen flow, PO2/FiO2, SOFA and hs-cTnI were closely related to short-term outcome. The corresponding ROC of hs-cTnI, oxygen flow and SOFA for patient death prediction were 0.949, 0.906 and 0.652. hs-cTnI at 47.8 ng/liter predicted death, sensitivity 92.8%, specificity 92.9%; Oxygen flow at 5.5 liter/minute predicted death sensitivity 100%, specificity 77.9%; SOFA score at 5 predicted death sensitivity 100%, specificity 73.8%.
Conclusion: Our cohort study demonstrated that inhaled oxygen flow, SOFA score, and myocardial injury at admission in critically ill COVID-19 patients were important indicators for predicting short-term death of patients, the hs-cTnI can be as a risk stratification, which may provide a simple method for the physicians to identify high-risk patients and give reasonable treatment in time.
Keywords: COVID-19, high-sensitivity cardiac troponin I, short-term outcome
Introduction
Coronavirus disease 2019 (Covid-19) is a global epidemic disease, most patients can be cured,1,2 but severe patients, especially elderly patients still have a higher mortality rate.1,3 Covid-19 is a systemic disease that damages various systems throughout the body. There are many basic diseases in elderly patients. After the merger of the new crown, the two superimposed the two, resulting in aggravation of the disease and increased mortality. Coronavirus 2 (SARS-CoV-2) infects host cells through ACE2 receptors, leading to coronavirus disease (COVID-19)-related pneumonia, while also causing acute myocardial injury and chronic damage to the cardiovascular system.4 Myocardial injury associated with the SARS- CoV-2 occurred in 5 of the first 41 patients diagnosed with COVID-19 in Wuhan, which mainly manifested as an increase in high-sensitivity cardiac troponin I (hs- cTnI) levels (>28 pg/mL).5 In another report of 138 patients with COVID-19 in Wuhan, 36 patients with severe symptoms were treated in the ICU.2 The levels of biomarkers of myocardial injury were significantly higher in patients treated in the ICU than in those not treated in the ICU (median creatine kinase (CK)- MB level 18 U/l versus 14 U/l, P < 0.001; hs- cTnI level 11.0 pg/mL versus 5.1 pg/mL, P = 0.004), suggesting that patients with severe symptoms often have complications involving acute myocardial injury.5 Cardiac injury occurred in 19.7% of patients during hospitalization,6 and it was one independent risk factor for in-hospital mortality, Troponin elevation in COVID-19 patients was an important stratification biomarker.7 However, it is still unclear how myocardial injury at admission affects in-hospital mortality. This study observed the outcome of a group of critically ill patients, paying particular attention to the impact of myocardial injury on patient prognosis at admission. Focus on the changes of clinical indicators, identify high-risk patients in time, and give active treatment to effectively control the condition and win opportunities for patients to recover. Analyze the clinical data of these patients and screen early warning indicators.
Methods
This study complied with the Declaration of Helsinki. All patients were confirmed 2019-nCoV infection by real-time RT-PCR and were admitted to a designated hospital (West Campus of Union Hospital, Huazhong University of Science and Technology) in Wuhan. We prospectively collected and analyzed data. Data were obtained from electronic medical records including clinical charts, nursing records, laboratory findings, and chest x-rays were from Feb 8, 2020, to April 7, 2020.
Researchers directly communicated with patients or their families to ascertain epidemiological and symptom data. According to the patient’s admission situation, the patients were divided into Severe group and critical group. The Severe group diagnostic standard meets one of the following conditions, RR≥30 次/min or SPO2<90% or P/F<300mmHg. The diagnostic criteria for critical group are to meet one of the following conditions, respiratory failure requires respiratory support or circulatory failure or other organ damage according to the COVID-19 pneumonia diagnosis and treatment plan, trial version 7 (Published by China National Health Commission). The Acute Physiology and Chronic Health Evaluation (APACHE II)8 score, CURB-65 Pneumonia Severity Score, Sequential Organ Failure Assessment (SOFA) Score and pneumonia severity index (PSI) score were made within 24 hours of admission. Cardiac injury was diagnosed if serum levels of cardiac biomarkers, hs-cTnI were above >28 pg/mL, or new abnormalities were shown in electrocardiography and echocardiography.5 All patients were screened for clinical chest pain symptoms and electrocardiogram changes to rule out acute myocardial infarction. Acute kidney injury was identified and classified on the basis of the highest serum creatinine level or urine output criteria according to the kidney disease improving global outcomes classification.9 The length of hospital stays, survival to discharge and death and were compared between two groups. The short-term outcomes were defined as mortality in hospital.
This study was approved by the National Health Commission of China and Ethics Commission of Union Hospital in Wuhan (2020-0177). Written informed consent was waived by the Ethics Commission of the designated hospital for emerging infectious diseases.
Statistical Analysis
Continuous variables were expressed as median (IQR, Median, 25th-75th) and compared with the Mann–Whitney U-test; Categorical variables were summarized as counts and percentages and compared by χ2 test or Fisher’s exact test between Severe and Critical groups. Univariate regression was used to analyze the correlation between each variable and the patient’s discharge survival. Logistic stepwise regression was used to screen the above independent variables to establish a logistic regression model. The sensitivity, specificity, and area under ROC were used to evaluate the performance of the selected variables. A two-sided α of less than 0.05 was considered statistically significant. Statistical analyses were done using the SPSS software, version 13.0, unless otherwise indicated.
Results
General Information
A total of 128 patients were collected during this observation period, of which 100 patients met the diagnostic criteria of severe patients with COVID-19 during 2020.02.08–2020.04.07 according to COVID-19 pneumonia diagnosis and treatment plan, trial version 7 (Published by China National Health Commission), severe patients required oxygen inhalation to maintain SPO2> 93%. The average age of 100 patients was 65 years (IQR, 26–97). There were 51 males (51%) and 49 females (49%). The combined underlying diseases were 31 (31%) diabetes, 46 (46%) hypertension, 10 (10%) coronary heart disease, 14 (14%) stroke, and 10 (10%) chronic obstructive pulmonary disease. The main clinical manifestations were fever in 76 (76%), dry cough in 48 (48%), shortness of breath in 46 (46%), diarrhea in 4 (4%) and fatigue (9%).
Epidemiological History
All patients live in Wuhan, 69 of them have a clear history of contact with infected persons, 15 (15%) have family-associated infection, 4 have been diagnosed with new coronary disease due to other diseases, and 12 have no Clear contact history. All patients were diagnosed with a positive throat swab nucleic acid test.
Chest High-Resolution CT Examination
8 people (8%) with small patch shadows or infiltration shadows; 13 (13%) with multiple small patch shadows and lung interstitial changes; 81 people with multiple ground glass shadows and infiltration shadows on both lungs (81%); 24 patients with lung consolidation (24%); 6 patients with pleural effusion (6%).
Treatment
Antiviral treatment, Abidor 0.2 Tid, until the nucleic acid test is negative; patients with anorexia and poor nutritional status are given nutritional support treatment, mainly enteral nutrition; treatment for basic diseases, such as controlling hypertension and controlling blood sugar, Anti-myocardial ischemia treatment, etc.
Respiratory Support Treatment Strategy
According to the patient’s admission SPO2, blood gas analysis results, giving suck oxygen or non-invasive ventilation or tracheal intubation with lung protective ventilation strategy, the detail decision process is shown in Figure 1.
Clinical Outcomes
There were 76 patients in Severe group, 24 patients in Critical group, the male/female ratios of the two groups is 39/12 and 35/14, χ2 = 0.330, p = 0.566. The incidence of Critical group with diabetes was 13/26, which was significantly higher than that of Severe group, 18/74, χ2 = 5.930, p = 0.015. There was no difference between the two groups with hypertension, chronic obstructive pulmonary disease (COPD), Stroke, Coronary heart disease (CHD) and tumors diseases as shown in Table 1. There was a higher incidence of shortness breath in Critical group than in Severe group (Table 1).
 |
Table 1 Severe Group and Critical Group Complicated with Basic Diseases |
The age of patients was 65 years (IQR, 55–71) in Severe group, 63 years (IQR, 56–69.5) in Critical group, p=0.865. The diagnosis time by PCR were 6 days (IQR, 4–9) in Severe group and 6 days (IQR, 5–7), p=0.813.
The temperature, blood pressure and Pulse rate were no differences between two groups. The respiratory rates were 22 times (IQR, 20–27) in Severe group lower than 31 times (IQR, 24–38) in Critical group, p<0.001. The Pulse oxygen saturation (SPO2, %) and PO2/FiO2 were significantly lower in Critical group than in Severe group (Table 2). The patients in Critical group need higher Oxygen flow to maintain the SPO2 over 93%.
 |
Table 2 The Vital Signs and Main Laboratory Test Results of the Two Groups of Patients on Admission |
The incidence of Lymphopenia was 16/74 (21.6%) in Severe group and 18/26 (69.2%) in Critical group, p<0.001. The incidence of cardiac injury was also very higher in Critical group 14/26 (52.9%) than 7/76 (9.9%) in Severe group, p<0.001. The main laboratory test results of the two groups of patients on admission are shown in Table 2. There were a lot of biochemical markers significantly different between two groups, such as BUN, LDH, CPR, Total protein, albumin, pre-albumin, HCT, Lymphocyte, PLT, hs-cTnI, Myoglobin, BNP, D-Dimer and IL-6, Table 2.
At the time of admission, the patients’ scores of CURB 65, APACH2, SOFA, and PSI, all showed that the Critical group was significantly higher than the Severe group, Table 2.
All patients in the Severe group were cured and discharged, 26 patients in the Critical group used non-invasive mask ventilation, and 12 of them underwent tracheal intubation and mechanical ventilation. 14 people in the Critical group died, and the remaining patients were discharged. The length of hospital stay was 38 days (IQR, 23–46) in Severe group, 18.5 days (IQR, 3.75–54) in Critical group, p=0.078. Differences between clinical and laboratory tests in the Critical group, the survivor and non-survivor are shown in Table 3.
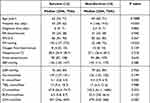 |
Table 3 Differences Between Clinical and Laboratory Tests Between Survivor and Non-Survivor in the Critical Group at Admission |
Screening of Prognostic Indicators
Univariate regression analysis showed that oxygen flow when patients were admitted to hospital, PO2/FiO2, SOFA and hs-cTnI were closely related to short-term outcome, Table 4. PO2/FiO2 predicted the survival of patients discharge, Sensitivity 90.7% and Specificity 100% at Cutoff value of 153 mmHg. Logistic Stepwise regression showed that oxygen flow at admission, hs-cTnI and SOFA scores at admission can predict the patient’s death from discharge. The corresponding ROC of hs-cTnI, oxygen flow and SOFA for patient death prediction is 0.949, 0.906 and 0.652. hs-cTnI at 47.8 ng/liter predicted death, sensitivity 92.8%, specificity 92.9%; Oxygen flow at 5.5 liter/minute predicted death sensitivity 100%, specificity 77.9%; SOFA score at 5 predicted death sensitivity 100%, specificity 73.8%.
 |
Table 4 Oxygen Flow When Patients Were Admitted to Hospital, PO2/FiO2, SOFA and hs-cTnI Were Closely Related to Short-Term Outcome |
Discussion
The cases included in this study met the diagnostic criteria for critically ill patients according to COVID-19 pneumonia diagnosis and treatment plan, trial version 7 (Published by China National Health Commission), and 26 of them met the diagnostic criteria for critical illness. The critically ill patients suffered from respiratory failure when they were admitted to the hospital and needed assisted ventilation. 14 people used non-invasive ventilation, and 12 people were promptly given intubation after non-invasive ventilation failure, and mechanical ventilation was performed according to the lung protective strategy. 14 patients in the Critical group died. Existing evidences show that the elderly patients with some chronic diseases have a poor prognosis, and these patients are most likely to develop into critically ill pneumonia.10 The present study, 67% of patients in this series are older than 60 years old, 46/74 (62.2%) in Severe group, 19/26 (73%) in Critical group, p=0.444. The incidence of diabetes in critical group (13/26, 50%) is significantly higher than that in Severe group (18/74, 24.3%). According to a recent report,11 diabetes should be considered as a risk factor for a rapid progression and bad prognosis of COVID-19.
Shortness of breath in clinical manifestations is an important indicator of the critical condition of the patient.12 In the present study, the incidence of shortness of breath in Severe group was significantly lower than that of in Critical group. Non-survivor 11 of 14 patients had shortness of breath, and 32 of 86 survivor had shortness of breath, p=0.004. In this study, we found that inhaled oxygen flow also indicates poor prognosis, 3 liter/min (IQR, 2–5) in Severe group, 10 liter/min (IQR, 6–10) in Critical group, p<0.001. Multivariate regression analysis shows that oxygen flow is highly correlated with patient prognosis, ROC 0.906, Oxygen flow at 5.5 liter/minute predicted death sensitivity 100%, specificity 77.9%. The ratio of arterial partial pressure of oxygen to fraction of inspired oxygen (P/F) predicted the survival of patients discharge, Sensitivity 90.7% and Specificity 100% at Cutoff value of 153 mmHg.
In this study, results were found similar to other studies,1,2,5 critical patients have a higher proportion of Lymphopenia, D-dimer, LDH and CPR increased, total protein, albumin, and pre-albumin decreased. However, univariate regression analysis showed that these variables have no significant correlation with the prognosis of patients. COVID-19 is a systemic disease that has caused lung injury as the main manifestation of systemic diseases and the incidence of multiple organ injury is relatively high in critical patients.13–15 This series of patients has a higher frequency of organ injury, kidney injury 8/72 (11%) in Severe group, 7/22 (31.8%) in Critical; liver injury 9/72 (12.5%) in Severe group, 7/22 (31.8%) in Critical group; myocardial injury 7/71 (9.9%) in Severe group, 9/17 (52.9%) in Critical, p<0.001. Stepwise regression analysis showed that myocardial injury marker hs-cTnI was closely related to the prognosis of patients, hs-cTnI at 47.8 ng/liter predicted death, ROC 0.949, sensitivity 92.8%, specificity 92.9%. In addition to the comparison of single indicators in this study, we also used the commonly used scoring system to evaluate the patients, such as APACH2, CURB 65, SOFA and PSI scores. These scoring methods can reflect the severity of the covid-19 disease, the scores in critical group were significantly higher than in severe group. Stepwise regression analysis showed that only the SOFA score could predict the death of patients on discharge, ROC was 0.652, SOFA score at 5 predicted death sensitivity 100%, specificity 73.8%. Compared with other indicators, hs-cTnI has a higher ROC, sensitivity and specificity for the prediction of short-term death of patients, hs-cTnI can be used as an important reference index for patients with poor prognosis. We also tested other myocardial biomarkers, such as Myoglobin, CK-MB and BNP, multivariate logistic regression analysis showed that these variables cannot predict the death of patients, the hs-cTnI had superiority to Myoglobin, CK-MB, BNP for prognosis of covid-19 patient due to its myocardial specificity. This also implies that we should pay more attention to myocardial damage during the treatment of covid-19 pneumonia, it may be an independent predictor for adverse outcomes.16 The impact of covid-19 on the cardiovascular system, especially myocardial injury and hemodynamics, needs further observation and research.
This study has the following limitations: the first is a single center, and the included patients are mainly severe patients over 60 years old. To fully understand the occurrence of myocardial injury in covid-19 patients, it is necessary to expand the observation population, but most of the mild patients no hospital observation is required, and it is difficult to know about the incidence of myocardial injury in total covid-19 patients. Second, the observation time of patients in this study is relatively short; Third, the sample size of this group of patients is too small, so used all-cause mortality as short-term outcome. Studies with a larger number of samples have also been published,6 the systematic observation of the impact of myocardial injury on in hospital mortality can better reflect the value of hs-cTnI as a risk stratification.
In summary, our cohort study demonstrated that inhaled oxygen flow, SOFA score, and myocardial injury at admission in critically ill COVID-19 patients were important indicators for predicting short-term death of patients, the hs-cTnI can be as a risk stratification, which may provide a simple method for the physicians to identify high-risk patients and give reasonable treatment in time.
Acknowledgments
We gratefully acknowledge all the health-care workers on the front line of West campus of Union Hospital, Huazhong University of Science and Technology and the First Affiliated Hospital of Sun Yat-sen University and all the patients involved in the study. This study was supported by funding from the Shenzhen Science and technology R&D Fund (Grant No. JCYJ20160608142215491) and Guangdong Province Basic and Applied Basic Research Fund Project (Grant No. 2020A1515010120 and 2020A1515110919). The funders had no role in the study design, data collection, analysis, decision to publish, or the preparation of the manuscript.
Disclosure
The declare no conflicts of interests.
References
1. Guan WJ, Ni ZY, Hu Y, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382(18):1708–1720. doi:10.1056/NEJMoa2002032
2. Wang D, Hu B, Hu C, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020;323(11):1061–1069. doi:10.1001/jama.2020.1585
3. Wang L, He W, Yu X, et al. Coronavirus disease 2019 in elderly patients: characteristics and prognostic factors based on 4-week follow-up. J Infect. 2020;80:639–645. doi:10.1016/j.jinf.2020.03.019
4. Zheng YY, Ma YT, Zhang JY, et al. COVID-19 and the cardiovascular system. Nat Rev Cardiol. 2020;17(5):259–260. doi:10.1038/s41569-020-0360-5
5. Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497–506. doi:10.1016/S0140-6736(20)30183-5
6. Shi S, Qin M, Shen B, et al. Association of cardiac injury with mortality in hospitalized patients with COVID-19 in Wuhan, China. JAMA Cardiol. 2020;5(7):802–810. doi:10.1001/jamacardio.2020.0950
7. Maloberti A, Biolcati M, Giannattasio C. Troponin elevation in COVID-19 patients: an important stratification biomarker with still some open questions. Int J Cardiol. 2021;341:107–109. doi:10.1016/j.ijcard.2021.07.049
8. Knaus WA, Draper EA, Wagner DP, et al. APACHE II: a severity of disease classification system. Crit Care Med. 1985;13(10):818–829. doi:10.1097/00003246-198510000-00009
9. Khwaja A. KDIGO clinical practice guidelines for acute kidney injury. Nephron Clin Pract. 2012;120(4):c179–184. doi:10.1159/000339789
10. China Nhcotpro. Chinese clinical guidance for COVID-19 pneumonia diagnosis and treatment, 7th edn; 2020. Available from: https://kjfy.meetingchina.org/msite/news/show/cn/3337.html.
11. Guo W, Li M, Dong Y, et al. Diabetes is a risk factor for the progression and prognosis of COVID-19. Diabetes Metab Res Rev. 2020;e3319. doi:10.1002/dmrr.3319
12. Du Y, Tu L, Zhu P, et al. Clinical features of 85 fatal cases of COVID-19 from Wuhan: a retrospective observational study. Am J Respir Crit Care Med. 2020;201:1372–1379. doi:10.1164/rccm.202003-0543OC
13. Chen L, Li X, Chen M, et al. The ACE2 expression in human heart indicates new potential mechanism of heart injury among patients infected with SARS-CoV-2. Cardiovasc Res. 2020;116(6):1097–1100. doi:10.1093/cvr/cvaa078
14. Su H, Yang M, Wan C, et al. Renal histopathological analysis of 26 postmortem findings of patients with COVID-19 in China. Kidney Int. 2020;98:219–227. doi:10.1016/j.kint.2020.04.003
15. Yang F, Shi S, Zhu J, et al. Analysis of 92 deceased patients with COVID-19. J Med Virol. 2020;92:2511–2515. doi:10.1002/jmv.25891
16. Ni W, Yang X, Liu J, et al. Acute myocardial injury at hospital admission is associated with all-cause mortality in COVID-19. J Am Coll Cardiol. 2020;76:124–125. doi:10.1016/j.jacc.2020.05.007
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

