Back to Journals » Clinical Interventions in Aging » Volume 13
Hidden blood loss and its risk factors after hip hemiarthroplasty for displaced femoral neck fractures: a cross-sectional study
Authors Guo WJ , Wang JQ , Zhang WJ, Wang WK, Xu D, Luo P
Received 15 May 2018
Accepted for publication 7 August 2018
Published 10 September 2018 Volume 2018:13 Pages 1639—1645
DOI https://doi.org/10.2147/CIA.S174196
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Zhi-Ying Wu
Wei-jun Guo,1,* Ji-qi Wang,1,* Wei-jiang Zhang,1 Wei-kang Wang,2 Ding Xu,2 Peng Luo1
1Department of Orthopaedic Surgery, Second Affiliated Hospital and Yuying Children’s Hospital of Wenzhou Medical University, Wenzhou, People’s Republic of China; 2Department of Orthopedics Trauma Surgery, RWTH Aachen University, Aachen, Germany
*These authors contributed equally to this work
Purpose: Several authors have reported the degree of total blood loss (TBL) following hemiarthroplasty for displaced femoral neck fracture; however, the research specifically investigating on hidden blood loss (HBL) after hip hemiarthroplasty is still lacking. The purpose of this study is to evaluate the HBL in patients who underwent hip hemiarthroplasty for displaced femoral neck fractures and to analyze its risk factors.
Patients and methods: From January 2015 to December 2016, 212 patients (57 males and 155 females) with displaced femoral neck fracture undergoing hip hemiarthroplasty were included in this study. The demographic and relevant clinical information of the patients were collected. According to the Gross’s formula, each patient’s height, weight, and preoperative and postoperative hematocrit were recorded and used for calculating the total perioperative blood loss and HBL. Risk factors were further analyzed by multivariate linear regression.
Results: The HBL was 525±217 mL, with 61.0%±13.6% in the total perioperative blood loss (859±289 mL), and the perioperative hemoglobin (Hb) loss was 23.8±7.4 g/L. Multivariate linear regression analysis revealed that HBL was positively associated with higher American Society of Anesthesiologists (ASA) classification (regression coefficient=62.169, 95% CI=15.616–108.722; P=0.009), perioperative gastrointestinal bleeding/ulcer (regression coefficient=155.589, 95% CI=38.095–273.083; P=0.010), and transfusion (regression coefficient=192.118, 95% CI=135.578–248.659; P<0.001). Compared with females, males had a risk of increased HBL (regression coefficient=87.414, 95% CI=28.547–146.280; P=0.004), and general anesthesia had an increased HBL compared with spinal anesthesia (regression coefficient=68.920, 95% CI=11.707–126.134; P=0.018).
Conclusion: HBL should not be ignored in patients who underwent hip hemiarthroplasty for displaced femoral neck fractures in the perioperative period, because it is a significant portion of TBL. Female patients, patients with higher ASA classification and perioperative gastrointestinal bleeding/ulcer, patients who were administered general anesthesia, or patients who underwent transfusion had a greater amount of HBL after hip hemiarthroplasty was performed. Having a correct understanding of HBL may help surgeons improve clinical assessment capabilities and ensure patients’ safety.
Keywords: hidden blood loss, risk factors, femoral neck fractures, hemiarthroplasty
Introduction
Femur neck fracture related to osteoporosis in older patients is steadily increasing. It has become a devastating injury for patients and a substantial burden for the health care system as well.1–3 Approximately 250,000 individuals diagnosed with femoral neck fractures need to be treated in the United States, with reported annual costs exceeding $4.4 billion every year.4 Hemiarthroplasty is the most common treatment for displaced femoral neck fractures in older adults, because it can promote early postoperative ambulation, lower reoperation rates, and better functional outcomes in the first year after operation compared with internal fixation.5–7 However, hip hemiarthroplasty can still lead to a large amount of blood loss. Actually, the total blood loss (TBL) after surgery for hip fracture is much greater than that observed during the operation.8,9 After the concept of hidden blood loss (HBL) was put forward in 2000,10 more and more studies have provided evidence for HBL in a range of orthopedic surgical procedures, such as hip fracture surgery,8,9,11 total knee10,12–14 or hip arthroplasty,15 and spine surgery.16–20 Several authors4,21–25 have reported the degree of TBL following hemiarthroplasty for femoral neck fracture, but only a few studies8 specifically investigated the HBL for hip hemiarthroplasty surgery. Moreover, as far as we know, there is still no published study that has analyzed risk factors for HBL after the hip hemiarthroplasty procedure. The aim of this study was to quantify HBL during hemiarthroplasty surgery in patients with displaced femoral neck fractures and to identify predictors of HBL in these patients.
Patients and methods
Patients
This study was approved by the ethical committee of the Second Affiliated Hospital of Wenzhou Medical University. The need for informed consent from patients was waived by the board, since it was a retrospective cross-sectional study, and all the data were collected and analyzed anonymously without any potential harm to the patients. After that, we performed a retrospective review from our electronic medical record to identify the consecutive patients who underwent hip hemiarthroplasty for displaced femoral neck fractures by the same senior surgeon (more than 15 years of clinical experience in treating femoral neck fractures) between January 2015 and December 2016 at our institution. The inclusion criteria were age>70 years, unilateral displaced femoral neck fracture, low-energy injury, no previous ipsilateral proximal femoral fracture or surgery, and completed medical data, including blood tests performed preoperatively and on the third day postoperatively. The exclusion criteria were pathological fractures, any other traumatic fracture, neoplastic diseases, and severe hematologic disorders. Finally, a total of 212 patients were included in this study.
Hip hemiarthroplasty procedures
All hip hemiarthroplasty surgeries were performed through the Moore posterolateral approach in a lateral position with a buttress between two legs. Prophylactic intravenous antibiotics (2 g cefazolin) were administered 30 minutes before the procedures. Uncemented prostheses (LCU, Link, Germany) with bipolar heads were used in all cases. Hemoglobin (Hb) and the hematocrit (Hct) levels were measured in all patients prior to the surgery and on the third postoperative day. Postoperative intravenous cefazolin (2 g, ×3 doses) was administered within the first 24 hours. The drainage tubes were removed 48 hours after the operations. Low-molecular-weight heparin was used from the time the patients were admitted until the operations were done to prevent deep venous thrombosis. All patients received 10 mg of oral rivaroxaban per day postoperatively for at least 1 month.
Transfusion management
While transfusion is widely performed when Hb is 80–90 g/L in healthy patients and 100 g/L in patients with severe cardiac disease, due to the institutional policy for restrictive transfusion, transfusions at our institution were performed only when Hb is <80 or 100 g/L for symptomatic patients (extreme weakness, chest pain, extreme paleness, or major bleeding) with destabilizing vital signs (heart rate, >100 or systolic blood pressure, <90 mmHg).
Data collection
Demographic and medical information were collected for all the patients. Age, gender, height, weight, body mass index (BMI), time to surgery, postoperative length of stay, transfusion volume, comorbidities (including hypertension, diabetes mellitus, cerebrovascular disease, cardiovascular disease, pulmonary disease, renal insufficiency [creatinine>200 mmol/L] and liver disease [chronic elevation over normal values of SGOT, SGPT, and/or γ-GT because of a known cause such as chronic hepatitis B or C], preoperative chronic anticoagulation, and perioperative gastrointestinal bleeding/ulcer), and blood tests (including Hb and Hct levels before surgery and on the third postoperative day and preoperative albumin) were recorded by surgeons. Because no patient’s BMI was >30, in our study, we only categorized patients into two groups according to the recommendation of the WHO: underweight group, BMI<18.5 and normal group, 18.5≤BMI<30. The patient’s American Society of Anesthesiologists (ASA) classification, type of anesthesia, surgical bleeding, and surgical time were assessed and recorded by anesthetists. The intraoperative blood loss was measured as the sum of the blood in suction bottles (after subtracting the lavage fluid used during the surgery) and weighed sponges during the procedure. The volume of the drainage was measured by nurses 48 hours postoperatively.
Calculation of blood loss
The estimated blood volume (EBV) was calculated according to the formula of Nadler et al26: EBV (L)=k1×height (m)3+k2×weight (kg)+k3 (for male: k1=0.3669, k2=0.03219, and k3=0.6041; for female: k1=0.3561, k2=0.03308, and k3=0.1833).
Total red blood cell volume was calculated by multiplying the EBV by the patient’s Hct. Thus, the change in the red blood cell volume can be reflected through the change in Hct. In our study, TBL was calculated according to the Gross’s formula27: TBL (L)=EBV (L)×(Hctpre−Hctpost)/Hctave, where Hctpre is the initial preoperative Hct, Hctpost is Hct on the third day postoperatively, and Hctave is the average of Hctpre and Hctpost. Finally, the HBL was calculated according to the formula of Sehat et al:28 HBL=calculated TBL–visible blood loss (intraoperative blood loss+drainage volume). When transfusion was performed during the perioperative period, the formula was calculated as follows: HBL=calculated TBL+blood infusion–visible blood loss.
We assumed that blood volume would be the same on admission as on the third postoperative day, the loss of Hb during the perioperative period was measured as follows: Hb loss (g/L)=Hbpre−Hbpost, where Hbpre is the initial preoperative Hb and Hbpost is the Hb on the third day postoperatively.
Statistical analysis
Data analysis was performed using SPSS 22.0 for Mac (SPSS Inc., Chicago, IL, USA). Descriptive statistics were shown as mean±SD or number of cases and percentages, where applicable. Student’s t-test for independent samples was used to test significant differences between males and females. Univariable analysis using Pearson correlation was performed initially to identify variables potentially influencing the HBL. Any variable where the Pearson correlation had a value of P<0.1 was accepted as a candidate for multivariate linear regression analysis to identify the independent risk factors associated with HBL.29 A positive coefficient indicates a positive influence on the dependent variable (HBL), whereas a negative coefficient indicates a negative influence. All independent variables were incorporated into the model using the method of “Enter”. A value of P<0.05 was considered statistically significant.
Results
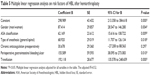
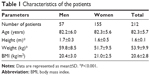
We retrospectively reviewed 212 consecutive patients who underwent hip hemiarthroplasty for displaced femoral neck fractures by the same senior surgeon from January 2015 to December 2016, including 57 males and 155 females. The average age was 82.3±5.7 years (range=70–96 years), and the average BMI was 20.6±2.8 (range=14.7–27.7). Demographic data of patients are summarized in Table 1. No differences were found in age and BMI between males and females (P>0.05). The data for Hct level loss, Hb loss, the number of patients whose Hb<100 g/L preoperatively and postoperatively, calculated TBL, visible blood loss, HBL, and percentage of HBL are shown in Table 2. The mean TBL was 859±289 mL, and the mean HBL was 525±217 mL, which accounted for 61.0%±13.6% of TBL. Nineteen (9.0%) patients had an Hb<100 g/L before surgery, whereas this number increased to 122 (57.5%) postoperatively (P<0.001, chi-squared test).
  | Table 1 Characteristics of the patients |
  | Table 2 Perioperative parameters of the patients |
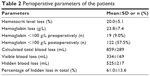
Table 3 shows the results of univariable analysis between 23 potential risk factors we mentioned earlier and HBL by using Pearson correlation analysis. Finally, six risk factors were involved in multivariate linear regression analysis to examine the association between HBL and these factors. Different levels of HBL between these six risk factors are shown in Table 4. After multivariate linear regression analysis, as Table 5 shows, higher ASA classification (P=0.009), perioperative gastrointestinal bleeding/ulcer (P=0.010), and transfusion (P<0.001) were positively correlated with HBL. Compared with women, men had an increased risk of HBL (P=0.004), and general anesthesia had an increased risk of HBL compared with spinal anesthesia (P=0.018). However, preoperative chronic anticoagulation was not an independent risk factor for HBL. Other factors such as age, BMI category, time to surgery, surgical time, postoperative length of stay, wound drainage, preoperative blood parameters, and comorbidities (except for perioperative gastrointestinal bleeding/ulcer) were not significantly correlated with HBL.
  | Table 3 Perioperative parameters of the patients and results of Pearson correlation analysis for hidden blood loss |
  | Table 4 Hidden blood loss among different clinical factors |
Discussion
Hip hemiarthroplasty may result in less visible blood loss than total hip or knee arthroplasty surgery,30 but older patients with displaced femoral neck fractures are physiologically more susceptible to postoperative anemia due to the reasons of older age, higher ASA grade, frailty, and greater concomitant diseases.22 Blood loss can result not only from the initial fracture but also from the operation, and it can remain hidden for a period of time even after surgery.31 According to previous studies, postoperative anemia after hip fracture surgery is related to an inferior functional recovery and a detrimental effect on mortality.32,33 In the study by Foss and Kehlet,8 the HBL of hip fracture in connection with surgery was an excess of up to six times more than they observed during the operation. Therefore, the HBL of this patient group should not be ignored. Many researchers have referred to the TBL after hemiarthroplasty for femoral neck fractures. Some of them4,22–24,34,35 used Hb loss between the preoperative and postoperative periods to evaluate the volume of blood loss. To a certain extent, Hb loss could reflect the perioperative TBL, but this method might not be very accurate; particularly when the transfusion was performed, because the Hb loss would be discounted or lower than it really was. Other authors reported the TBL of hemiarthroplasty for femoral neck fractures ranging from 629 to 737 mL in relatively small population.21,25 After systematic searches, few researchers are investigating HBL after hip hemiarthroplasty. Foss and Kehlet8 found that the HBL after hemiarthroplasty was 987 mL, which accounts for 75% of TBL (1,301 mL), in 167 patients with femoral neck fractures. Although with this relatively large population, their aim was to discover the HBL after different hip fracture surgeries, including screws, hemiarthroplasty, dynamic hip screw and intramedullary nailing, they did not specifically explore the factors that might influence the HBL. According to our understanding, a systematic investigation of HBL after hemiarthroplasty for displaced femoral neck fractures and its risk factors is still lacking.
We performed a detailed investigation on 212 consecutive patients with displaced femoral neck fracture after hip hemiarthroplasty, with relatively complete clinical data, and used a relatively reliable approach for estimating HBL, based on the combination formulas of Nadler et al, Gross, and Sehat, which have been widely used to calculate HBL in orthopedic surgery.12,15–19 Moreover, some authors15,36–38 utilized these formulas to calculate the HBL after total hip arthroplasty recently (HBL ranged from 429 to 1,050 mL), which could be considered as one of the reasons for us to use these formulas as well. We found that the HBL after hip hemiarthroplasty was 525±217 mL, accounting for 61.0%±13.6% of TBL (859±289 mL). Our results showed that there was a significant amount of HBL after hip hemiarthroplasty, which should not be ignored for estimating perioperative blood loss, as the number of patients whose Hb<100 g/L was increased from 9.0% preoperatively to 57.5% postoperatively in our study. Thus, patients must be closely monitored after surgery because of the potential adverse effects of anemia. Similar to previous studies,4,22–24,34,35 we found that the perioperative Hb loss was 23.8±7.4 g/L. However, either HBL or TBL in our results was less than that in the research by Foss and Kehlet (HBL=987 mL, TBL=1,301 mL). The reasons might be as follows:
- The height and weight of our patients were smaller than Westerners, resulting in the calculated TBL based on the patient’s height and weight being lower than that in their study consequently.
- Because of the strict transfusion policy in our hospital (Hb<80 g/L or 100 g/L for symptomatic patients with destabilizing vital signs), only 29.7% of our patients were transfused.
In the research by Foss and Kehlet, the patients were transfused with blood for a level of Hb<100 g/L at any point during their admission, and about 50.6% of patients received transfusions after hip fracture surgery. Transfusion has been demonstrated as a risk factor that is associated with increased HBL.15 Consistently, after multiple linear regression, we found that blood transfusion was an independent risk factor that can increase the HBL after hip hemiarthroplasty. Pattison et al39 speculated that the postoperative blood loss might, at least in part, arise from hemolysis. Moreover, evidence showed that hemolysis would occur after a large number of stored red cells were transfused.40,41 Thus, we agreed with the view of Miao et al15 that patients who received blood transfusion had a higher HBL after hemiarthroplasty, might probably due to hemolysis. In addition, the study suggested that gender, ASA classification, type of anesthesia, and perioperative gastrointestinal bleeding/ulcer were independent risk factors for HBL.
The relationship between gender and HBL is still controversial. Some authors reported that gender was not correlated with HBL,15,19 and others14,16 found that gender plays a role in HBL, with a greater contribution in men relative to women. In our series, men had a larger amount of HBL than women. One reasonable explanation might be that men have a greater height and weight than women; consequently, they have a greater calculated blood volume and calculated TBL. The multiple linear analysis also showed that ASA classification was an independent risk factor for HBL. The reason might be that the patient with a higher ASA classification have poor cardiopulmonary compensation, function of coagulation, and level of tolerable anemia than the patient with lower ASA.16 Our results showed that the mean HBL of ASA IV was 686±302 mL, which was significantly more than the patients with ASA III (539±212 mL) and ASA II (468±191 mL). In other words, the patients with higher ASA classifications seem to have significant HBL in hip hemiarthroplasty. We found that there was an association between different types of anesthesia and HBL; general anesthesia was associated with higher HBL compared with spinal anesthesia. As general anesthesia causes vasodilation of patients, it not only leads to an increase in intraoperative or postoperative blood loss but also leads to an increase in blood infiltration into the tissue compartments, which causes a higher amount of HBL. An incidence of 6.1% gastrointestinal hemorrhage or ulceration was found in our patients, which has a significantly positive correlation with HBL. It might be easily ignored by surgeons as well.
Our study suffers from several limitations. First, the number of patients included in our cross-sectional study was still relatively small. Thus, our finding should be verified by a large number of patients or multicentre studies in the future. Second, according to the previous research, we used the Hct on the third postoperative day to calculate the TBL, as we assumed that fluid shifts would have been completed in patients at this time. If this is not the case, however, the HBL that was obtained might be falsely low. Finally, we regularly used rivaroxaban to prevent venous thromboembolism postoperatively; however, evidence41–43 has shown that rivaroxaban for thromboprophylaxis after hip arthroplasty will increase major bleeding or clinically relevant bleeding postoperatively, which might then affect the volume of HBL.
Conclusion
The current study indicates that HBL is a significant portion of TBL in patients after hip hemiarthroplasty for displaced femoral neck fractures. Female patients, patients with higher ASA classification and perioperative gastrointestinal bleeding/ulcer, patients who were administered general anesthesia, or patients who underwent transfusion had a greater amount of HBL after hip hemiarthroplasty was performed. HBL and its risk factors should also be taken into account when considering the perioperative strategies of fluid infusion and blood transfusion. The more effectively HBL is controlled, the better the rehabilitation of patients.
Acknowledgment
Peng Luo was supported by the funding of Chinese scholarship council (CSC).
Disclosure
The authors report no conflicts of interest in this work.
References
Butler M, Forte ML, Joglekar SB, Swiontkowski MF, Kane RL. Evidence summary: systematic review of surgical treatments for geriatric hip fractures. J Bone Joint Surg Am. 2011;93(12):1104–1115. | ||
Renken F, Renken S, Paech A, Wenzl M, Unger A, Schulz AP. Early functional results after hemiarthroplasty for femoral neck fracture: a randomized comparison between a minimal invasive and a conventional approach. BMC Musculoskelet Disord. 2012;13:141. | ||
Burgers PT, Hoogendoorn M, van Woensel EA, et al. Total medical costs of treating femoral neck fracture patients with hemi- or total hip arthroplasty: a cost analysis of a multicenter prospective study. Osteoporos Int. 2016;27(6):1999–2008. | ||
Carlson VR, Ong AC, Orozco FR, Lutz RW, Duque AF, Post ZD. The Direct Anterior Approach Does Not Increase Return to Function Following Hemiarthroplasty for Femoral Neck Fracture. Orthopedics. 2017;40(6):e1055–e1061. | ||
Gjertsen JE, Fenstad AM, Leonardsson O, et al. Hemiarthroplasties after hip fractures in Norway and Sweden: a collaboration between the Norwegian and Swedish national registries. Hip Int. 2014;24(3):223–230. | ||
Svenøy S, Westberg M, Figved W, et al. Posterior versus lateral approach for hemiarthroplasty after femoral neck fracture: Early complications in a prospective cohort of 583 patients. Injury. 2017;48(7):1565–1569. | ||
Ng ZD, Krishna L. Cemented versus cementless hemiarthroplasty for femoral neck fractures in the elderly. J Orthop Surg. 2014;22(2):186–189. | ||
Foss NB, Kehlet H. Hidden blood loss after surgery for hip fracture. J Bone Joint Surg Br. 2006;88(8):1053–1059. | ||
Smith GH, Tsang J, Molyneux SG, White TO. The hidden blood loss after hip fracture. Injury. 2011;42(2):133–135. | ||
Sehat KR, Evans R, Newman JH. How much blood is really lost in total knee arthroplasty? Correct blood loss management should take hidden loss into account. Knee. 2000;7(3):151–155. | ||
Chechik O, Thein R, Fichman G, Haim A, Tov TB, Steinberg EL. The effect of clopidogrel and aspirin on blood loss in hip fracture surgery. Injury. 2011;42(11):1277–1282. | ||
Schwab PE, Lavand’homme P, Yombi JC, Thienpont E. Lower blood loss after unicompartmental than total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2015;23(12):3494–3500. | ||
Subramanyam KN, Khanchandani P, Tulajaprasad PV, Jaipuria J, Mundargi AV. Efficacy and safety of intra-articular versus intravenous tranexamic acid in reducing perioperative blood loss in total knee arthroplasty: a prospective randomized double-blind equivalence trial. Bone Joint J. 2018;100-B(2):152–160. | ||
Prasad N, Padmanabhan V, Mullaji A. Blood loss in total knee arthroplasty: an analysis of risk factors. Int Orthop. 2007;31(1):39–44. | ||
Miao K, Ni S, Zhou X, et al. Hidden blood loss and its influential factors after total hip arthroplasty. J Orthop Surg Res. 2015;10:36. | ||
Wen L, Jin D, Xie W, et al. Hidden Blood Loss in Anterior Cervical Fusion Surgery: An Analysis of Risk Factors. World Neurosurg. 2018;109:e625–e629. | ||
Wu YS, Zhang H, Zheng WH, Feng ZH, Chen ZX, Lin Y. Hidden blood loss and the influential factors after percutaneous kyphoplasty surgery. Eur Spine J. 2017;26(7):1878–1883. | ||
Zhang H, Chen ZX, Sun ZM, et al. Comparison of the Total and Hidden Blood Loss in Patients Undergoing Open and Minimally Invasive Transforaminal Lumbar Interbody Fusion. World Neurosurg. 2017;107:739–743. | ||
Wen L, Jin D, Xie W, et al. Hidden Blood Loss in Posterior Lumbar Fusion Surgery: An Analysis of Risk Factors. Clin Spine Surg. 2018;31(4):180–184. | ||
Xu D, Ren Z, Chen X, et al. The further exploration of hidden blood loss in posterior lumbar fusion surgery. Orthop Traumatol Surg Res. 2017;103(4):527–530. | ||
Chang JD, Kim IS, Lee SS, Yoo JH, Hwang JH. Unstable intertrochanteric versus displaced femoral neck fractures treated with cementless bipolar hemiarthroplasty in elderly patients; a comparison of 80 matched patients. Orthop Traumatol Surg Res. 2016;102(6):695–699. | ||
Lee C, Freeman R, Edmondson M, Rogers BA. The efficacy of tranexamic acid in hip hemiarthroplasty surgery: an observational cohort study. Injury. 2015;46(10):1978–1982. | ||
Pala E, Trono M, Bitonti A, Lucidi G. Hip hemiarthroplasty for femur neck fractures: minimally invasive direct anterior approach versus postero-lateral approach. Eur J Orthop Surg Traumatol. 2016;26(4):423–427. | ||
Emara WM, Moez KK, Elkhouly AH. Topical versus intravenous tranexamic acid as a blood conservation intervention for reduction of post-operative bleeding in hemiarthroplasty. Anesth Essays Res. 2014;8(1):48–53. | ||
Kang JS, Moon KH, Kim BS, Yang SJ. Topical administration of tranexamic acid in hip arthroplasty. Int Orthop. 2017;41(2):259–263. | ||
Nadler SB, Hidalgo JH, Bloch T. Prediction of blood volume in normal human adults. Surgery. 1962;51(2):224–232. | ||
Gross JB. Estimating allowable blood loss: corrected for dilution. Anesthesiology. 1983;58(3):277–280. | ||
Sehat KR, Evans RL, Newman JH. Hidden blood loss following hip and knee arthroplasty. Correct management of blood loss should take hidden loss into account. J Bone Joint Surg Br. 2004;86(4):561–565. | ||
Jameson SS, Mason JM, Baker PN, Elson DW, Deehan DJ, Reed MR. The impact of body mass index on patient reported outcome measures (PROMs) and complications following primary hip arthroplasty. J Arthroplasty. 2014;29(10):1889–1898. | ||
van den Bekerom MP, Hilverdink EF, Sierevelt IN, et al. A comparison of hemiarthroplasty with total hip replacement for displaced intracapsular fracture of the femoral neck: a randomised controlled multicentre trial in patients aged 70 years and over. J Bone Joint Surg Br. 2010;92(10):1422–1428. | ||
Foss NB, Kristensen MT, Kehlet H. Anaemia impedes functional mobility after hip fracture surgery. Age Ageing. 2008;37(2):173–178. | ||
Lawrence VA, Silverstein JH, Cornell JE, Pederson T, Noveck H, Carson JL. Higher Hb level is associated with better early functional recovery after hip fracture repair. Transfusion. 2003;43(12):1717–1722. | ||
Carson JL, Noveck H, Berlin JA, Gould SA. Mortality and morbidity in patients with very low postoperative Hb levels who decline blood transfusion. Transfusion. 2002;42(7):812–818. | ||
Qiu M, Zhang X, Cai H, Xu Z, Lin H. The impact of hemocoagulase for improvement of coagulation and reduction of bleeding in fracture-related hip hemiarthroplasty geriatric patients: A prospective, single-blinded, randomized, controlled study. Injury. 2017;48(4):914–919. | ||
Ghanem ES, Richard RD, Wingert NCH, Gotoff JR, Graham JH, Bowen TR. Preoperative Use of Clopidogrel Does Not Affect Outcomes for Femoral Neck Fractures Treated With Hemiarthroplasty. J Arthroplasty. 2017;32(7):2171–2175. | ||
Lei Y, Huang Q, Huang Z, Xie J, Chen G, Pei F. Multiple-Dose Intravenous Tranexamic Acid Further Reduces Hidden Blood Loss After Total Hip Arthroplasty: A Randomized Controlled Trial. J Arthroplasty. 2018. | ||
Liu X, Zhang X, Chen Y, Wang Q, Jiang Y, Zeng B. Hidden blood loss after total hip arthroplasty. J Arthroplasty. 2011;26(7):1100–1105. | ||
Wang JQ, Chen LY, Jiang BJ, Zhao YM. Oxidized Regenerated Cellulose Can Reduce Hidden Blood Loss after Total Hip Arthroplasty: A Retrospective Study. J Invest Surg. 2018:1–7. | ||
Pattison E, Protheroe K, Pringle RM, Kennedy AC, Dick WC. Reduction in haemoglobin after knee joint surgery. Ann Rheum Dis. 1973;32(6):582–584. | ||
Karkouti K, Callum JL, Acker JP, Yip P, Rao V. Red Cell Transfusion-Associated Hemolysis in Cardiac Surgery: An Observational Cohort Study. Anesth Analg. 2017;124(6):1986–1991. | ||
Orlov D, Karkouti K. The pathophysiology and consequences of red blood cell storage. Anaesthesia. 2015;70(Suppl 3):29e9–29e12. | ||
Venker BT, Ganti BR, Lin H, Lee ED, Nunley RM, Gage BF. Safety and Efficacy of New Anticoagulants for the Prevention of Venous Thromboembolism After Hip and Knee Arthroplasty: AMeta-Analysis. J Arthroplasty. 2017;32(2):645–652. | ||
Ning G-Z, Kan S-L, Chen L-X, Shangguan L, Feng S-Q, Zhou Y. Rivaroxaban for thromboprophylaxis after total hip or knee arthroplasty: a meta-analysis with trial sequential analysis of randomized controlled trials. Sci Rep. 2016;6(1):23726. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.