Back to Journals » OncoTargets and Therapy » Volume 12
Hepatoid Adenocarcinoma Of The Lung Metastasizing To The Gingiva
Authors Wang C, Xu G, Wu G, Chen Z, Sun Z, Zheng P, Huang Y , Wang F, Yang X
Received 12 July 2019
Accepted for publication 25 September 2019
Published 23 October 2019 Volume 2019:12 Pages 8765—8768
DOI https://doi.org/10.2147/OTT.S222974
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Carlos E Vigil
Chunhua Wang,1 Guohui Xu,2 Ge Wu,2 Zhiming Chen,3 Zhiyong Sun,4 Ping Zheng,5 Yecai Huang,6 Fuqiang Wang,7 Xuegang Yang2
1Department of Radiology, Sichuan Cancer Hospital and Institute, Sichuan Cancer Center, School of Medicine, University of Electronic Science and Technology of China, Radiation Oncology Key Laboratory of Sichuan Province, Chengdu, Sichuan 610041, People’s Republic of China; 2Department of Interventional Radiology, Sichuan Cancer Hospital and Institute, Sichuan Cancer Center, School of Medicine, University of Electronic Science and Technology of China, Radiation Oncology Key Laboratory of Sichuan Province, Chengdu, Sichuan 610041, People’s Republic of China; 3PET/CT Center, The General Hospital of Western Theater Command, Chengdu, Sichuan 610083, People’s Republic of China; 4Nuclear Department, The General Hospital of Western Theater Command, Chengdu, Sichuan 610083, People’s Republic of China; 5Department of Pathology, Sichuan Cancer Hospital and Institute, Sichuan Cancer Center, School of Medicine, University of Electronic Science and Technology of China, Radiation Oncology Key Laboratory of Sichuan Province, Chengdu, Sichuan 610041, People’s Republic of China; 6Department of Radiation Oncology, Sichuan Cancer Hospital and Institute, Sichuan Cancer Center, School of Medicine, University of Electronic Science and Technology of China, Radiation Oncology Key Laboratory of Sichuan Province, Chengdu, Sichuan 610041, People’s Republic of China; 7Department of Interventional Radiology, Linshui County People’s Hospital, Guang’an, Sichuan 638500, People’s Republic of China
Correspondence: Xuegang Yang
Department of Interventional Radiology, Sichuan Cancer Hospital and Institute, Sichuan Cancer Center, School of Medicine, University of Electronic Science and Technology of China, Radiation Oncology Key Laboratory of Sichuan Province, No.55, Lane 4, RenMin Road (South), Chengdu, Sichuan 610041, People’s Republic of China
Tel +86 136 834 76844
Email [email protected]
Background: Hepatoid adenocarcinoma (HAC) of the lung, a very rare tumor, has been reported metastasizing to lymph nodes and distant tissue, with poor prognosis. We report a case of lung HAC metastasizing to the gingiva, which is a rare metastasis site.
Case Report: A 70-year-old, 50-pack-year, male smoker was diagnosed with a lung mass on a health examination. A chest CT showed a lung mass in the superior lobe of the right lung and enlarged lymph nodes in the right hilum and mediastinum. Liver and other digestive tumors were excluded. The lung mass was confirmed to be HAC by biopsy with positivity of HepPar-1. Despite erlotinib therapy, the tumor metastasized to the gingiva. Then, docetaxel and nedaplatin therapy, radiotherapy, and bevacizumab therapy were administered successively. The patient died of tumor progression 9 months after presentation.
Conclusion: Gingival metastasis of lung HAC is rare. The patient had a poor outcome. Further studies need to be conducted on lung HAC.
Keywords: hepatoid adenocarcinoma, lung, gingiva, metastasis
Introduction
Hepatoid adenocarcinoma (HAC) is a rare extrahepatic tumor characterized by its resemblance to hepatocellular carcinoma and its expression of HepPar-1. The stomach is the most common site of origin for HAC. HAC in the lung accounts for 5% of cases of HAC.1 Lung HAC tends to occur predominantly in men.2 Nodal and distant metastases are common in lung HAC and are associated with poor prognosis.2 Previous studies have described lung HAC metastasis to the brain, liver, adrenal gland, lymph nodes, bones, and tonsil.2,3 To the best of our knowledge, metastasis of lung HAC to the gingiva has not been reported in the English literature. In the present study, we report a case of primary lung HAC metastasizing to the gingiva, and the prognosis after chemotherapy and radiotherapy.
Case Report
A 70-year-old male smoker (50 pack-years) was diagnosed with a lung mass during a health examination. A chest CT showed a 6.0 × 4.6 cm2 mass in the right superior lobe of the lung with mild heterogeneous enhancement invading the nearby pleura and enlarged lymph nodes in the right hilum and mediastinum (Figure 1A–D). Genetic analyses revealed TP53 mutation. The patient was treated with erlotinib 150 mg/day. After 3 months of treatment, an FDG-PET/CT scan revealed enlargement of the lung mass (8.1 × 5.8 cm2), no significant change in the lymph nodes in the right hilum and mediastinum, and enlarged submandibular lymph nodes with abnormal uptake (maximum standard uptake value of 13.2) (Figure 1E–G). Abnormal uptake also occurred in the antrum of the stomach, which was confirmed to be gastritis by gastroscopy. A CT-guided lung needle biopsy was performed. Histopathologic examination of the mass in the right superior lobe of the lung revealed pulmonary adenocarcinoma with hepatoid features (Figure 1H). On immunohistochemistry, the tumor biopsy was positive for HepPar-1 (Figure 1I), CK, and EA, focally positive for CDX-2, and negative for α-fetoprotein (AFP) (Figure 1J), TTF-1, NapsinA, P63, P40, CD56, and Syn. The patient did not present any hepatic or other digestive tumors. Taking these results together, the patient was diagnosed with lung HAC. The serum pretreatment AFP level was not obtained, and the post-treatment AFP level was normal.
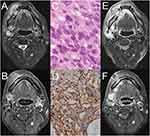
The patient had a gingival mass with pain 3 weeks after undergoing PET/CT. MRI of the neck showed a mass on the right lower gingiva with destruction of the mandible, and enlarged right submandibular lymph nodes (Figure 2A and B). Histopathologic examination of the mass on the right lower gingiva revealed an HAC metastasis (Figure 2C). Immunohistochemistry was positive for HepPar-1 (Figure 2D), CK, CK19, MOC31, and CDX-2, and negative for AFP, TTF-1, NapsinA, P63, P40, and SOX-10. After docetaxel 80 mg and nedaplatin 100 mg chemotherapy, radiotherapy of 33 Gy (2.2 Gy per time) was performed, and the patient acquired an infection caused by gingival tumor necrosis during treatment. MRI showed necrosis of the gingival mass without any significant decrease in size, while the lymph metastasis in the neck worsened (Figure 2E and F). The patient was treated with bevacizumab 300 mg after radiotherapy. The patient died of disease progression 9 months after presentation.
Discussion
Lung HAC is a rare tumor subtype and is still poorly understood. HAC was defined in 1990 as an AFP-producing adenocarcinoma with hepatoid features.4 Two criteria for the diagnosis of lung HAC were adopted: typical acinar or papillary adenocarcinoma and a component of carcinoma resembling hepatocellular carcinoma producing AFP.4 The diagnostic criteria for lung HAC were modified in 2014. Tumors containing components of typical adenocarcinoma with hepatoid features, signet-ring cells, or neuroendocrine carcinoma were included in lung HAC,5 and AFP expression was not a mandatory feature for a diagnosis of lung HAC.5 Previous cases demonstrated a male predominance in lung HAC.2 The case of lung HAC we reported was an old male smoker.
Nodal and distant metastases are common in lung HAC, as reported. We reported a case of lung HAC metastasizing to the gingiva. The oral cavity is an infrequent site of solid tumor metastasis. A previous study reviewed 673 cases of oral metastasis, of which the sites of origin included the lung in 112 cases, jawbone in 58 cases, and oral mucosa in 54.6 To the best of our knowledge, this is the first report of primary lung HAC metastasizing to the gingiva.
Because of its rarity, no standardized treatment for lung HAC has been established, although surgical resection, chemotherapy, and/or radiotherapy have been suggested as the most common treatments for lung HAC.7 In the reviewed reports, there was a long survival after surgery at an early stage. However, in general, prognosis in patients with unresectable disease is extremely poor.3 In the present case, the patient had reached a late clinical stage, with nodal and distant metastases, which resulted in a poor prognosis. After treatment with erlotinib, docetaxel and nedaplatin, radiotherapy, and bevacizumab, the patient succumbed 9 months after presentation owing to the tumor progression, which is consistent with previous studies showing that lung HAC patients with unresectable disease have a generally poor prognosis with overall survival of 6–11 months.3 Furthermore, the patient acquired an infection caused by gingival tumor necrosis during chemoradiotherapy, suggesting that chemotherapy combined with radiotherapy may be a possible treatment for lung HAC patients with metastasis to the gingiva. As a case report, the limitation of this case is the small sample, providing a limited contribution regarding therapy for and prognosis of lung HAC.
In conclusion, primary lung HAC metastasizing to the gingiva is a rare event. Further studies are required for better understanding of this tumor and tumor metastasis.
Ethics And Consent Statements
The study was approved by the Ethics Committee of Sichuan Cancer Hospital. Informed consent and approval for publication of any accompanying images for the case were obtained from the patient’s next of kin.
Acknowledgment
This study was supported in part by the Sichuan Science and Technology Plan Project, no. 18YYJC0665, and Sichuan Medical Research Project, no. Q18004.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Metzgeroth G, Strobel P, Baumbusch T, Reiter A, Hastka J. Hepatoid adenocarcinoma - review of the literature illustrated by a rare case originating in the peritoneal cavity. Onkologie. 2010;33(5):263–269. doi:10.1159/000305717
2. Grossman K, Beasley MB, Braman SS. Hepatoid adenocarcinoma of the lung: review of a rare form of lung cancer. Respir Med. 2016;119:175–179. doi:10.1016/j.rmed.2016.09.003
3. Valle L, Thomas J, Kim C, et al. Hepatoid adenocarcinoma of the lung metastasizing to the tonsil. Mol Clin Oncol. 2017;6(5):705–707. doi:10.3892/mco.2017.1215
4. Ishikura H, Kanda M, Ito M, Nosaka K, Mizuno K. Hepatoid adenocarcinoma: a distinctive histological subtype of alpha-fetoprotein-producing lung carcinoma. Virchows Arch A Pathol Anat Histopathol. 1990;417(1):73–80. doi:10.1007/bf01600112
5. Haninger DM, Kloecker GH, Bousamra Ii M, Nowacki MR, Slone SP. Hepatoid adenocarcinoma of the lung: report of five cases and review of the literature. Mod Pathol. 2014;27(4):535–542. doi:10.1038/modpathol.2013.170
6. Mallikarjun JH, Mujib BR, Naik R, Patil ST. Metastatic small cell carcinoma of the cervix to the oral cavity: a rare case report and an insight into pathogenesis of metastasis. J Oral Maxillofac Pathol. 2015;19(2):247–250. doi:10.4103/0973-029X.164541
7. Qian GQ, Yin FY, Li GX, Chu JG. Hepatoid adenocarcinoma of the lung. QJM. 2016;109(9):619–620. doi:10.1093/qjmed/hcw107
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.