Back to Journals » Journal of Inflammation Research » Volume 16
Heparin-Binding Protein: A Prognostic Biomarker Associated with Severe or Complicated Community-Acquired Pneumonia in Children
Authors Li S, Xu Y , Wu Y, Huang H, Sun C, Xu S, Li H , Zhang X, Zhao S, Huang L
Received 20 October 2022
Accepted for publication 24 December 2022
Published 26 January 2023 Volume 2023:16 Pages 321—331
DOI https://doi.org/10.2147/JIR.S393600
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Monika Sharma
Shuang Li,1,2,* Yanwen Xu,2,* Yuhang Wu,2,* Heyu Huang,2 Chen Sun,2 Shanshan Xu,2 Huajun Li,2 Xi Zhang,3 Shiyong Zhao,4 Lisu Huang1,2
1Department of Infectious Diseases, The Children’s Hospital, Zhejiang University School of Medicine, National Clinical Research Center for Child Health, Hangzhou, Zhejiang, People’s Republic of China; 2Department of Infectious Diseases, Xinhua Hospital, Shanghai Jiao Tong University School of Medicine, Shanghai, People’s Republic of China; 3Clinical Research Unit, Xinhua Hospital, Shanghai Jiao Tong University School of Medicine, Shanghai, People’s Republic of China; 4Department of Infectious Diseases, Hangzhou Children’s Hospital, Hangzhou, Zhejiang, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Lisu Huang, Department of Infectious Diseases, The Children’s Hospital, Zhejiang University School of Medicine, National Clinical Research Center for Child Health, 3333 Binsheng Road, Hangzhou, Zhejiang Province, 310052, People’s Republic of China, Email [email protected] Shiyong Zhao, Department of Infectious Diseases, Hangzhou Children’s Hospital, 195 Wenhui Road, Hangzhou, Zhejiang Provinve, 310005, People’s Republic of China, Email [email protected]
Purpose: Heparin-binding protein (HBP) is a novel biomarker for inflammatory diseases. This study aimed to investigate the role of serum HBP in community-acquired pneumonia (CAP) in children and the association of HBP with the severity and prognosis.
Patients and Methods: A total of 125 children with CAP admitted to the hospital were enrolled in this retrospective study. We analyzed the differences in clinical characteristics and examination findings between patients with different levels of HBP. The severe or complicated CAP was defined as having severe radiographic findings and/or systemic manifestations. Receiver operator characteristic (ROC) curves detected the performance of biomarkers in identifying patients with severe or complicated pneumonia. The multivariate logistic regression models assessed the association between HBP levels and the severity and prognosis. Finally, we constructed a predictive model based on HBP.
Results: The rate of severe or complicated CAP for patients with upper-quartile HBP concentration (≥ 60 ng/mL) was 54.8%, significantly higher than that of patients with lower HBP concentration (26.6%). The level of HBP is substantially correlated with neutrophil counts, C-reactive protein, erythrocyte sedimentation rate, and serum amyloid A protein (r = 0.31, 0.26, 0.36, and 0.26, respectively). HBP achieved the highest level of discrimination for severe or complicated CAP among the biomarkers. Higher HBP concentration (≥ 60 ng/mL) was associated with a three-fold higher risk of severe or complicated CAP (adjusted odds ratio = 3.11, p < 0.05). A predictive model including four characteristics (HBP, lactate dehydrogenase, age and non-viral infection) for predicting severe or complicated CAP (with area under the ROC curve = 0.75) was built to create a nomogram.
Conclusion: Substantially elevated serum HBP is significantly associated with severe or complicated CAP and poor prognosis in children. This finding warrants further investigation of the function of HBP in the pathogenesis of CAP.
Keywords: pneumonia, biomarker, heparin-binding protein, children
Introduction
Community-acquired pneumonia (CAP) is a leading cause of hospitalization among children. The incidence of CAP in children below 5 years old is 65.8 per 1000 person-years in China.1 CAP is a heterogeneous disease that ranges from a mild, self-limited illness to a severe infection that causes respiratory failure, septic shock and even death.2 According to the data from several population-based studies in different regions, the incidence rate of severe CAP in hospitalized children ranges from 3.9% to 23.0%.3,4 Biomarkers for systemic inflammatory response will provide an objective basis for evaluating the severity of pneumonia. Several studies have investigated the predictive value of conventional inflammation biomarkers, including leukocyte counts, C-reactive protein (CRP), and procalcitonin in children with severe CAP. However, the associations between the severity and the levels of known biomarkers remain inconclusive.5,6 Currently, no biomarker has been identified as the best assessment of the severity of CAP. There is still a need to develop rapid and efficient biomarkers to overcome the limitations of traditional biomarkers for helping treatment strategy.
One of the novel biomarkers of inflammation, heparin-binding protein (HBP), is a member of the serine protease family. It is stored in secretory and azurophilic granules of neutrophils and is rapidly released upon stimulation during inflammatory responses.7 HBP has been considered a potential biomarker for progression to sepsis because of its capacity to induce vascular leakage and regulate a wide variety of cellular responses to inflammation.8 Its favorable prognostic value for predicting sepsis has been established in the adult populations.9 Besides, HBP’s diagnostic and discriminative role in the etiology of CAP has been reported. HBP had a higher predictive value for differentiating bacterial and viral infections than leukocyte and neutrophil counts in adult patients with CAP.10 For the pediatric population, to the best of our knowledge, the only report on the association of between serum HBP and the severity of CAP was a retrospective study enrolling critically ill children. This study found that patients with elevated HBP levels were more likely to develop respiratory failure and severe sepsis.11 In this study, as all patients were enrolled from intensive care unit, these findings could not be generalizable to the vast majority of patients with CAP. Meanwhile, radiological imaging is necessary for the diagnosis of pulmonary complications of CAP due to the nonspecific symptoms in children. In the evaluation of severe or complicated pneumonia, computed tomography (CT) can detect the area and extent of lung lesions, such as ground-glass opacities, consolidations, and pleural effusions.12,13 Thus, in contrast to some subjective assessments, CT provides information on the enlargement of lung infiltration and can be used as an imaging surrogate for the severity of CAP. At present, the understanding of the severe imaging features of HBP and lung CT in children with CAP remains insufficient. In our study, every patient had low-dose CT images due to the suspected pulmonary complications or the demands of understanding the etiology of pneumonia. We aimed to assess the role of HBP in pediatric CAP and to analyze the association of HBP with disease severity associated with pulmonary complications and systemic manifestations.
Methods
Participants
This study was a retrospective study of newly diagnosed CAP patients aged < 18 years enrolled on initial admission between May 2021 and September 2021. The definition of CAP was referred to the British Thoracic Society 2011 guidelines for the management of CAP in children.14 Enrolled individuals with CAP were those satisfying the following inclusion criteria: (1) with clinical signs and symptoms of respiratory tract infection; (2) with non-enhanced low dose CT scan consistent with pneumonia within 48 hours of admission based on the clinical demands. In terms of radiation safety, the radiation doses received by all patients were 0.4–1.6 mSv, well below the cumulative dose with potential cancer risk (30–90 mSv).15 Children were excluded if they were: (1) recently hospitalized within 7 days; (2) with neutropenia due to chemotherapy; (3) with immunodeficiency.
Data Collection and Laboratory Tests
We retrospectively collected the baseline information, clinical presentation, laboratory tests and radiographic findings by reviewing the electronic medical record. Laboratory tests included HBP, leukocyte counts and classification, platelet counts, CRP, procalcitonin, erythrocyte sedimentation rate (ESR), ferritin, lactic dehydrogenase (LDH), serum amyloid A (SAA) protein, lactate and cytokines. HBP was measured using Fluorescent Immunoanalyzer AFS-1000 and its reagents (Shanxi Kang Jianen Biotechnology Co., Ltd, Shanxi, China) according to the manufacturer’s instructions. Microbiologic assessments included blood for bacterial culture, serology for respiratory viruses, and naso/oropharyngeal swabs for the polymerase chain reaction of common respiratory pathogens. Mycoplasma pneumoniae antibody titer ≥ 1:160 on admission or a four-fold increase of the titer was required to establish a diagnosis of Mycoplasma pneumoniae infection.16 All patients with negative results of microbial etiology were diagnosed with probable viral or bacterial infection by two experienced physicians according to the clinical manifestation and other laboratory findings.17 Etiologic data was summarized using categorical variables for bacterial, viral, and Mycoplasma pneumoniae infection.
Outcome Measurements
The primary outcome was severe or complicated CAP assessed during hospitalization. Patients were considered to have severe or complicated pneumonia if they had one or both of the following presence: (1) severe pulmonary manifestations based on radiographic findings, including pulmonary consolidation, lobar atelectasis, and pleural effusion in this study; (2) systemic manifestations that contributed to severe outcomes.18–20 For the patients enrolled in this study, systemic manifestations of severe or complicated cases were hypoxemia, liver injury (defined as the elevation of serum glutamic pyruvic transaminase ≥ 1.5 times the upper limit of the normal laboratory reference value and/or the elevation of bilirubin levels), disorders of electrolyte and acid-base balance (including unexplained metabolic acidosis and moderate to severe hyponatremia), Kawasaki disease (considered to be secondary to definite CAP during hospitalization21,22) and myocarditis. The secondary outcome was the length of hospital stay.
Statistical Analysis
Patients were grouped according to the levels of HBP. The clinical data of patients with the highest quartile (≥60 ng/mL) of HBP was compared to that of patients with the other three quartiles (<60 ng/mL) of HBP. The measurement data was presented as medians and interquartile ranges (IQR) and were compared using the Kruskal–Wallis H-test (for variables with non-normal distribution) or Student’s t-test (for variables with normal distribution). The categorical variables were compared using the chi-squared test or Fisher’s exact probability test. The associations between inflammatory biomarkers were examined by Spearman correlation analysis. Receiver operator characteristic (ROC) curves detected the performance of biomarkers in identifying patients with severe or complicated pneumonia. Multivariable logistic regression analysis was used to assess the association between the concentration of HBP and the clinical outcomes. The results were expressed as the odds ratio (OR) and 95% confidence interval (CI). Age, sex and pathogen were identified as potential confounders. Considering the influence of antibiotic use before admission, a sensitivity analysis excluding those with bacterial infections was performed to exclude the potential bias. Finally, we constructed a multivariate predictive model by machine learning algorithms. Extreme gradient boosting (XGBoost) was introduced for modeling using the “XGBoost” package in R. A nomogram was developed to visualize the multivariate predictive model. The effectiveness and robustness of the model were evaluated using a piecewise linear regression model and calibration curve. The optimal threshold point of nomogram score was determined by the ROC curve to distinguish between high-risk and low-risk groups. Kaplan-Meier survival curve was used to assess the hospital discharge probability at different points of time and to compare patients with different levels of prognostic factors. Statistical analyses were performed using the R software version 4.2.1 (http://www.R-project.org) and the EmpowerStats (www.empowerstats.com; X&Y Solutions, Inc., Boston, MA, USA).
Results
Patient Characteristics
In accordance with the selection criteria, 125 patients with CAP were enrolled in this study. The median HBP level for the patients enrolled was 26.3 ng/mL (IQR 16.5–57.1 ng/mL). According to the 75th percentile distribution, we identified the cutoff value of HBP at 60 ng/mL.
Demographic and clinical characteristics of patients with different levels of HBP are outlined in Table 1. The median age in the lower HBP (<60 ng/mL) group was 2 years (IQR 1–3 years), younger than that in the higher HBP (≥60 ng/mL) group (3 years, IQR 2–4 years). There were no statistically significant differences in gender, chronic conditions, and clinical presentations. Patients with higher HBP had a significantly higher frequency of Mycoplasma pneumoniae infection compared to the lower group (48.4% vs 28.7%), but no difference was found in the distribution of bacterial or viral infection between the two groups. Severe pulmonary radiographic findings included consolidation, atelectasis, and pleural effusion. The proportion of patients with severe radiographic findings in the higher group was 2.6-fold higher than that of patients in the lower group (41.9% vs 16.0%, p<0.05). Specifically, the higher HBP group included more patients with pulmonary consolidation. There were more patients with hypoxemia or extra-pulmonary manifestations in the higher HBP group, but the difference did not reach statistical significance. The proportion of patients with severe or complicated CAP in the higher HBP group was approximately twice higher than that of patients in the lower group (54.8% vs 26.6%, p<0.05). The median length of hospitalization in the higher HBP group was 2 days longer than that in the lower group (7 days vs 5 days, p<0.05) (Table 1).
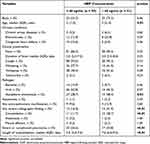 |
Table 1 Demographic and Clinical Characteristics of Children with CAP According to HBP Levels |
Laboratory Findings
Patients with higher HBP had significantly higher leukocyte counts, neutrophil counts, neutrophil percentages, and lower lymphocyte percentages (Table 2). Regarding the inflammation biomarkers, higher CRP, ESR, SAA, and interleukin-1β were observed in patients with higher HBP compared with the lower group. In contrast, no differences were present in lymphocyte count, platelet count, procalcitonin, ferritin, LDH, lactate, interleukin-2, interleukin-6, interleukin-8, interleukin-10, and tumor necrosis factor-α (Table 2). Spearman correlations were estimated between inflammatory biomarkers (Figure 1). Inflammatory biomarkers, including neutrophil counts, CRP, ESR, and SAA, were significantly correlated with the level of HBP (estimated correlations of 0.31, 0.26, 0.36, and 0.26, respectively; p<0.05 for each comparison).
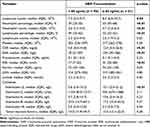 |
Table 2 Laboratory Tests of Children with CAP Stratified with HBP Levels |
Potential Factors Associated with the Severity of Pneumonia
Of the 125 children in this study, 42 (33.6%) had severe or complicated pneumonia. Severe radiology findings were confirmed in 28 patients. Of these, 22 patients were identified to have pulmonary consolidation, 4 had pleural effusion, and 4 had atelectasis. The main systemic manifestations among patients enrolled were disorders of electrolyte and acid-base balance (8 cases), Kawasaki diseases (3 cases), liver injury (3 cases), hypoxemia (2 cases), and myocarditis (1 cases). Notably, the 3 patients with manifestations of Kawasaki disease during their hospitalization were diagnosed with CAP on admission and had evidence of microbiological etiology.
No significant differences between the severe or complicated pneumonia and mild pneumonia group with regard to clinical characteristics, including age, gender, and clinical presentation (Table S1). In terms of etiology, viral infections were less common in children with severe or complicated pneumonia than in children with mild pneumonia (45.2% vs 66.3%, p<0.05). The proportion of Mycoplasma pneumoniae infection in children with severe or complicated pneumonia was 1.8-fold higher than that in children with mild pneumonia (47.6% vs 26.5%, p<0.05). The median level of HBP in patients with severe or complicated pneumonia was nearly twice higher than that in patients with mild pneumonia (43.0 ng/mL vs 24.3 ng/mL, p<0.05). However, no significant difference was observed in other potential inflammatory markers (Table S1).
The diagnostic performance of candidate inflammatory biomarkers in identifying children with severe or complicated CAP was evaluated using the area under ROC curves (Table S2). Among the candidate biomarkers, HBP achieved the highest level of discrimination for severe or complicated CAP (area under the ROC curve=0.62). Sensitivity analysis revealed consistent findings after excluding patients with bacterial infections (area under the ROC curve of HBP = 0.67) (Table S2).
HBP as a Biomarker Associated with the Severity of CAP
We analyzed the association between HBP levels and disease severity by logistic regression models. Patients with elevated HBP were more likely to develop pulmonary complications according to their radiographic findings. After adjusting for age, sex and probable pathogen, the higher HBP group had a 3-fold increased risk of developing any severe radiographic finding compared with the lower group (adjusted OR: 3.08, p<0.05, Table 3). When HBP was included in the multivariate regression model as a continuous variable, the risk of developing severe radiographic findings was increased by 10% with every 10 ng/mL increase in HBP (p<0.05, Table 3). We did not observe the association between higher HBP and the occurrence of any systemic manifestations, including hypoxemia and extra-pulmonary manifestations, in the crude and the adjusted models. However, the risk of these manifestations was increased by 13% with every 10 ng/mL increase in HBP (p<0.05, Table 3). Patients with higher HBP levels had an almost 3-fold greater risk of severe or complicated pneumonia than the lower group (adjusted OR: 3.11, p<0.05, Table 3). The risk of severe or complicated CAP was increased by 12% with every 10 ng/mL increase in HBP (p<0.05, Table 3). The higher HBP group had a 3.8-fold increased risk of staying in hospital for more than 10 days compared with the lower group (adjusted OR: 3.81, p<0.05, Table 3). Moreover, in the sensitivity analysis excluding patients with bacterial infections (17 patients), the association between the elevated HBP and the risk of severe or complicated pneumonia remained statistically significant in the multivariate model (adjusted OR: 3.86, p<0.05, Table S3).
 |
Table 3 Association Between HBP Levels and the Severity in Children with CAP |
Establishment of Risk Score Model Based on HBP
In addition, XGBoost algorithms were used to identify patients with severe or complicated CAP based on baseline characteristics and blood biomarkers. A final predictive model of HBP, LDH, age and non-viral infection was obtained using the XGBoost method (area under the ROC curve=0.75, Figure 2A). We built a nomogram incorporating these four risk factors above (Figure 2B) for predicting severe or complicated CAP. The probability of severe or complicated CAP by different levels of nomogram score is presented by piecewise linear regression modeling (Figure 2C). The calibration curve shows that the probability of severe or complicated CAP predicted by the nomogram was consistent with the actual probability (Figure 2D). The optimal cutoff value of the nomogram score determined by the ROC curve divided patients into two classes, designated as high-risk (≥74 points) and low-risk (<74 points) groups. The difference in the proportion of severe or complicated CAP in the high-risk group and the low-risk was significant [64.5% (20/31) vs 20.8% (15/72), p<0.01, Figure 2E].
Length of Hospitalization
The Kaplan-Meier curves show the length of hospital stay from admission until discharge. The probability of remaining in hospital by classification of patients with higher and lower HBP levels is shown in Figure 3A, indicating that the risk of prolonged hospitalization was increased for patients with higher HBP (p<0.01, Log rank test). The median length of stay for these groups was 7 days and 5 days, respectively (p<0.01). The Kaplan-Meier curves for patients in the high-risk group (nomogram score ≥74 points) and patients in the low-risk group (nomogram score <74 points) show good performance in distinguishing the risk of prolonged hospitalization (Figure 3B, p<0.01, Log rank test). The median length of stay for these groups was 7 days and 5.5 days, respectively (p<0.01).
 |
Figure 3 The Kaplan-Meier curves comparison of the rate of hospitalization (A) between different levels of HBP and (B) between different levels of risk score. |
Discussion
In this study, we retrospectively enrolled 125 CAP patients and analyzed the relationship between serum HBP levels and the severity and prognosis. HBP showed a strong association with severe or complicated CAP among all the potential biomarkers, and this association remained statistically significant after adjusting for potential confounding factors. Moreover, a higher level of HBP observed among children with CAP was associated with a longer hospital stay. A multivariate model consisting of HBP, LDH, age and non-viral infection for predicting severe or complicated CAP was constructed to identify the high-risk patients more effectively. Finally, we built a predictive nomogram model to make the HBP more clinically applicable.
As an important inflammatory mediator, HBP has been reported as a promising biomarker in predicting disease worsening or progression in infectious diseases. A study enrolling 487 adult patients with suspected infection in the emergency department found that 29% of the patients developed organ dysfunction, also defined as severe sepsis.23 Similarly, another study enrolled 157 children with severe CAP, and severe sepsis occurred in 21.7% of them.11 HBP could predict disease progression to severe sepsis with an area under the ROC curve value of 0.80 and 0.85 respectively in both studies.11,23 Although parallels can be seen with other studies, the incidence of severe sepsis was low in the present study. Only two patients developed hypoxemia with remission after oxygen inhalation. This study reported both pulmonary and systemic manifestations in children with CAP, and we mainly investigated the role of serum HBP levels in the occurrence of these severe presentations. The levels of HBP were independently associated with the radiographic severity of CAP in children, which were mainly related to the immune response after the tissue damage associated with pulmonary infection. As described in previous studies, HBP is expressed in neutrophils and stored in their secretory vesicles and azurophilic granules.7 Neutrophil-derived HBP is involved in vascular permeability and edema formation during the host defense and the inflammatory processes since the endothelial cells were the initial targets of HBP.24 These properties offer a potential explanation for the association between HBP levels and the severity of radiographic findings, especially for the formation of consolidation of lung tissue due to the probable endothelial damage during the intense inflammatory responses in the respiratory tract.25 A previous study has demonstrated the predictive value of HBP for acute exacerbations of interstitial lung disease.26 The mechanistic pathways were probably similar to pulmonary injury in CAP.
Previous findings have revealed that HBP is a marker of bacterial infection in adult patients.27,28 However, a relatively small proportion of enrolled patients were diagnosed with bacterial infections in this study, and no patient was found to have positive blood culture. Therefore, we prespecified a sensitivity analysis excluding patients with bacterial infections. These results supported our findings and conclusions. In this study, children with increased HBP levels were more often infected by Mycoplasma pneumoniae. The mechanism of neutrophil infiltration into the lungs in Mycoplasma pneumoniae pneumonia involves the excessive production of various inflammatory cytokines and chemokines.29 Thus, we can infer that Mycoplasma pneumoniae infection impacts the increase of HBP. Further, we have adjusted the logistic regression models for probable pathogens to account for the direct microbial damage to the respiratory tract. We can still conclude that HBP levels are associated with severe or complicated pneumonia, and this association seems less dependent on etiology.
Furthermore, in addition to the known association between HBP and neutrophils, there were highly positive correlations between HBP and some representative acute-phase reactants, including CRP, ESR, and SAA. This finding suggests that serum HBP might aid in the clinical judgment of the degree of systemic inflammation. Although linear relationships were evaluated between HBP and these candidate biomarkers, HBP is the most important independent factor for severe or complicated pneumonia in the present study. The levels of other biomarkers had less predictive value in the outcome measures. One possible explanation would be that the HBP is a specific marker for interstitial and tissue edema formation in human tissues and organs.24 This property is different from other markers, for example, procalcitonin, the release of which follows overwhelming cytokine storms.30 The overall levels of cytokines in the patients enrolled did not increase remarkably. The procalcitonin, therefore, did not show a strong effect on disease severity in this study. However, the nomogram model built in our study has included LDH, recognized as a traditional indicator of lung damage or inflammation,31 as well as a prognostic factor in pneumonia patients.32 The elevation of HBP and LDH may have similar effects on the development of severe or complicated pneumonia.
Several limitations of the present study should be discussed. First, the exact role of HBP was unclear among CAP patients since HBP levels in lower airway samples (sputum or bronchoalveolar lavage fluid) were not detected. However, it is still reasonable to speculate that HBP in the peripheral circulation may be involved in the development of CAP according to the known mechanisms. Besides, lower airway samples are not feasible for routine disease monitoring. Second, HBP circulates in the blood with a short elimination half-life between 1 and 2 h,33 suggesting a degree of variability at each point of the disease development. Therefore, dynamic detection may compensate for this deficiency. Moreover, the threshold value of HBP determined by the upper quartile in this study should be confirmed and validated in future studies to increase validity in larger cohorts.
Conclusion
In conclusion, the level of HBP indicates the underlying disease severity of CAP in children, and the constructed nomogram based on HBP can help predict the probability of severe or complicated pneumonia in those patients. Rapidly identifying children at high risk for severe or complicated pneumonia could signal the need for closer monitoring or prolonged hospital stay for therapy.
Ethics
This study was approved by the Ethics Committee and Review Board of Xinhua Hospital affiliated to Shanghai Jiao Tong University School of Medicine (ID: XHEC-C-2013-107). All methods in this study were performed in accordance with the Declaration of Helsinki and the existing guidelines of Ethics Committee. In accordance with the informed consent exemption rules of the Ethics Committee and Review Board of Xinhua Hospital, our study complies with the informed consent exemption requirement due to the retrospective nature of the present study. Anonymity and confidentiality of patient data were guaranteed.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This investigation was supported by National Natural Science Foundation of China (No.81874265 and No.82073561), Shanghai Jiao Tong University School of Medicine (No.2020002), National Respiratory Field Key Laboratory Emergency Project (EKPG21-08), National Ministry of Science and Technology-National Key R&D Program Project (No.2021YFE0201900), and Key Discipline Construction Plan from Shanghai Municipal Health Commission (GWV-10.1-XK01).
Disclosure
The authors declare that there are no conflicts of interest in this work.
References
1. Sun Y, Li H, Pei Z, et al. Incidence of community-acquired pneumonia in urban China: a national population-based study. Vaccine. 2020;38(52):8362–8370. doi:10.1016/j.vaccine.2020.11.004
2. Samransamruajkit R, Wong JJ, Smathakane C, et al. Pediatric severe sepsis and shock in three Asian countries: a retrospective study of outcomes in nine PICUs. Pediatr Crit Care Med. 2021;22(8):713–721. doi:10.1097/PCC.0000000000002680
3. le Roux DM, Myer L, Nicol MP, Zar HJ. Incidence and severity of childhood pneumonia in the first year of life in a South African birth cohort: the drakenstein child health study. Lancet Glob Health. 2015;3(2):e95–e103. doi:10.1016/S2214-109X(14)70360-2
4. Sun YP, Zheng XY, Zhang HX, et al. Epidemiology of respiratory pathogens among children hospitalized for pneumonia in Xiamen: a retrospective study. Infect Dis Ther. 2021;10(3):1567–1578. doi:10.1007/s40121-021-00472-0
5. Florin TA, Ambroggio L, Brokamp C, et al. Biomarkers and disease severity in children with community-acquired pneumonia. Pediatrics. 2020;145(6):e20193728. doi:10.1542/peds.2019-3728
6. Fernandes CD, Arriaga MB, Costa MCM, et al. Host inflammatory biomarkers of disease severity in pediatric community-acquired pneumonia: a systematic review and meta-analysis. Open Forum Infect Dis. 2019;6(12):ofz520. doi:10.1093/ofid/ofz520
7. Iversen LF, Kastrup JS, Bjorn SE, et al. Structure of HBP, a multifunctional protein with a serine proteinase fold. Nat Struct Biol. 1997;4(4):265–268. doi:10.1038/nsb0497-265
8. Bentzer P, Fisher J, Kong HJ, et al. Heparin-binding protein is important for vascular leak in sepsis. Intensive Care Med Exp. 2016;4(1):33. doi:10.1186/s40635-016-0104-3
9. Wu YL, Yo CH, Hsu WT, et al. Accuracy of heparin-binding protein in diagnosing sepsis: a systematic review and meta-analysis. Crit Care Med. 2021;49(1):e80–e90. doi:10.1097/CCM.0000000000004738
10. Cai R, Li H, Tao Z. Heparin-binding protein and procalcitonin in the diagnosis of pathogens causing community-acquired pneumonia in adult patients: a retrospective study. PeerJ. 2021;9:e11056. doi:10.7717/peerj.11056
11. Huang C, Zhang C, Zhang J, Zhang L, Mo Y, Mo L. Heparin-binding protein in critically ill children with severe community-acquired pneumonia. Front Pediatr. 2021;9:759535. doi:10.3389/fped.2021.759535
12. Tan Kendrick AP, Ling H, Subramaniam R, Joseph VT. The value of early ct in complicated childhood pneumonia. Pediatr Radiol. 2002;32(1):16–21. doi:10.1007/s00247-001-0583-5
13. Hayden GE, Wrenn KW. Chest radiograph vs. computed tomography scan in the evaluation for pneumonia. J Emerg Med. 2009;36(3):266–270. doi:10.1016/j.jemermed.2007.11.042
14. Harris M, Clark J, Coote N, et al. British thoracic society guidelines for the management of community acquired pneumonia in children: update 2011. Thorax. 2011;66(Suppl 2):ii1–ii23. doi:10.1136/thoraxjnl-2011-200598
15. Brenner DJ, Hall EJ. Computed tomography--an increasing source of radiation exposure. N Engl J Med. 2007;357(22):2277–2284. doi:10.1056/NEJMra07214
16. Daxboeck F, Krause R, Wenisch C. Laboratory diagnosis of Mycoplasma pneumoniae infection. Clin Microbiol Infect. 2003;9(4):263–273. doi:10.1046/j.1469-0691.2003.00590.x
17. Ruuskanen O, Lahti E, Jennings LC, Murdoch DR. Viral pneumonia. Lancet. 2011;377(9773):1264–1275. doi:10.1016/S0140-6736(10)61459-6
18. de Benedictis FM, Kerem E, Chang AB, Colin AA, Zar HJ, Bush A. Complicated pneumonia in children. Lancet. 2020;396(10253):786–798. doi:10.1016/S0140-6736(20)31550-6
19. Dean P, Florin TA. Factors associated with pneumonia severity in children: a systematic review. J Pediatric Infect Dis Soc. 2018;7(4):323–334. doi:10.1093/jpids/piy046
20. Scott JA, Wonodi C, Moïsi JC, et al. The definition of pneumonia, the assessment of severity, and clinical standardization in the Pneumonia etiology research for child health study. Clin Infect Dis. 2012;54(suppl_2):S109–S116. doi:10.1093/cid/cir1065
21. Principi N, Rigante D, Esposito S. The role of infection in Kawasaki syndrome. J Infect. 2013;67(1):1–10. doi:10.1016/j.jinf.2013.04.004
22. Turnier JL, Anderson MS, Heizer HR, Jone PN, Glodé MP, Dominguez SR. Concurrent respiratory viruses and Kawasaki disease. Pediatrics. 2015;136(3):e609–e614. doi:10.1542/peds.2015-0950
23. Linder A, Arnold R, Boyd JH, et al. Heparin-Binding Protein Measurement Improves the Prediction of Severe Infection with Organ Dysfunction in the Emergency Department. Crit Care Med. 2015;43(11):2378–2386. doi:10.1097/CCM.0000000000001265
24. Gautam N, Olofsson AM, Herwald H, et al. Heparin-binding protein (HBP/CAP37): a missing link in neutrophil-evoked alteration of vascular permeability. Nat Med. 2001;7(10):1123–1127. doi:10.1038/nm1001-1123
25. Goldenberg NM, Kuebler WM. Endothelial cell regulation of pulmonary vascular tone, inflammation, and coagulation. Compr Physiol. 2015;5(2):531–559. doi:10.1002/cphy.c140024
26. Xue M, Zhang T, Lin R, et al. Clinical utility of heparin-binding protein as an acute-phase inflammatory marker in interstitial lung disease. J Leukoc Biol. 2022;112(4):861–873. doi:10.1002/JLB.3MA1221-489R
27. Fisher J, Linder A. Heparin-binding protein: a key player in the pathophysiology of organ dysfunction in sepsis. J Intern Med. 2017;281(6):562–574. doi:10.1111/joim.12604
28. Ma J, Lu Q, Tu S, Miao X, Zhao J. A diagnostic test: combined detection of heparin-binding protein, procalcitonin, and C-reactive protein to improve the diagnostic accuracy of bacterial respiratory tract infections. J Thorac Dis. 2022;14(3):721–728. doi:10.21037/jtd-22-260
29. Tamiya S, Yoshikawa E, Ogura M, Kuroda E, Suzuki K, Yoshioka Y. Neutrophil-mediated lung injury both via TLR2-dependent production of IL-1alpha and IL-12 p40, and TLR2-independent CARDS toxin after Mycoplasma pneumoniae infection in mice. Microbiol Spectr. 2021;9(3):e0158821. doi:10.1128/spectrum.01588-21
30. Hatherill M, Tibby SM, Turner C, Ratnavel N, Murdoch IA. Procalcitonin and cytokine levels: relationship to organ failure and mortality in pediatric septic shock. Crit Care Med. 2000;28(7):2591–2594. doi:10.1097/00003246-200007000-00068
31. Drent M, Cobben NA, Henderson RF, Wouters EF, van Dieijen-Visser M. Usefulness of lactate dehydrogenase and its isoenzymes as indicators of lung damage or inflammation. Eur Respir J. 1996;9(8):1736–1742. doi:10.1183/09031936.96.09081736
32. Lu A, Wang C, Zhang X, Wang L, Qian L. Lactate dehydrogenase as a biomarker for prediction of refractory mycoplasma pneumoniae pneumonia in children. Respir Care. 2015;60(10):1469–1475. doi:10.4187/respcare.03920
33. Fisher J, Kahn F, Wiebe E, et al. The dynamics of circulating heparin-binding protein: implications for its use as a biomarker. J Innate Immun. 2022;14(5):447–460. doi:10.1159/000521064
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


