Back to Journals » Journal of Pain Research » Volume 16
Healthcare Costs, Time to Fitness for Work, and Related Factors in Chronic Complex Regional Pain Syndrome: A Comparative and Longitudinal Study of 5-Year Follow-Up
Authors Duong HP , Léger B , Scholz-Odermatt SM, Burrus C , Vuistiner P , Konzelmann M , Luthi F
Received 8 December 2022
Accepted for publication 8 February 2023
Published 7 March 2023 Volume 2023:16 Pages 683—693
DOI https://doi.org/10.2147/JPR.S400659
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Jonathan Greenberg
Hong Phuoc Duong,1,* Bertrand Léger,1 Stefan Markus Scholz-Odermatt,2 Cyrille Burrus,1,3 Philippe Vuistiner,1 Michel Konzelmann,1,3 François Luthi1,3,4,*
1Department of Medical Research, Clinique romande de réadaptation, Sion, 1951, Switzerland; 2Department of Statistics, Sammelstelle für die Statistik der Unfallversicherung (SSUV), c/o Swiss Accident Insurance Fund (Suva), Lucerne, 6002 Switzerland; 3Department of Musculoskeletal Rehabilitation, Clinique Romande de Réadaptation, Sion, 1951, Switzerland; 4Department of Rheumatology and Rehabilitation, Hôpital Orthopédique, University and University Hospital of Lausanne, Lausanne, 1011, Switzerland
*These authors contributed equally to this work
Correspondence: Bertrand Léger, Tel +41 27 603 2075, Email [email protected]
Purpose: To assess and compare the healthcare costs, time to fitness for work (TFW) between chronic complex regional pain syndrome (CRPS) and non-CRPS; and identify factors associated with these outcomes in a comparative longitudinal study.
Patients and Methods: 148 patients with chronic CRPS of the hand and 273 patients with chronic hand impairments but without CRPS (non-CRPS) were admitted at a Swiss rehabilitation clinic between 2007 and 2016. Healthcare costs and TFW were retrieved from insurance data over 5 years after the accident. Socio-demographic factors, biopsychosocial complexity measured by means of the INTERMED questionnaire, pain intensity and DASH disability scores were collected during rehabilitation. Generalized estimation equations and Cox proportional-hazards models were used to identify factors associated with outcomes.
Results: Healthcare costs were increased by 20% for the CRPS versus non-CRPS group (coefficient = 1.20, 95% CI = 1.08– 1.35, p< 0.001). The median TFW was longer for CRPS than non-CRPS patients (816 vs 672 days, p = 0.02). After adjusting for covariates, TFW did not differ between the two groups (hazard ratio = 0.94, 95% CI = 0.73– 1.21, p=0.61). For CRPS patients, higher healthcare costs were associated with severe or moderate initial injury, high INTERMED or DASH disability scores. Longer TFW were associated with severe initial injury, low educational level, no work contract, and high INTERMED or DASH disability scores.
Conclusion: Overall, the healthcare costs were higher for CRPS than non-CRPS patients, but the TFW was comparable. We demonstrated also the significant associations of disability and biopsychosocial factors with the healthcare costs and TFW in CRPS patients.
Keywords: complex regional pain syndrome, healthcare costs, biopsychosocial complexity, work incapacity, fitness for work, CRPS
Introduction
Complex regional pain syndrome (CRPS) is a rare but challenging condition that occurs in 0.15% of orthopedic trauma.1 CRPS of the hand is the most frequent, and its incidence is estimated at 3.7% to 14% after wrist fracture.2 Patients with CRPS have longer disability,3 lower quality of life,4 and higher economic and social burden than reference patients.1 According to a recent study using the Swiss National Accident Insurance database, the healthcare costs and number of days lost at work were 13 and 20 times higher, respectively, in patients with CPRS over the 5 years after the accident1 than in patients without CRPS.
The economic impact of CRPS has been reported from previous population-based studies,1,5 but the contextual factors behind the problem have not been fully investigated. In previous studies using the International Classification of Diseases (ICD) codes as diagnostic criteria, the cohort could consist of people with self-limited as well as severe or longstanding CRPS. In addition, verifying whether a diagnosis of CRPS was appropriately documented or not in these register-based data is not possible. Diagnosing CRPS can be challenging for practitioners who are unfamiliar with it. Dutch6 and Canadian7 studies demonstrated that CRPS could be diagnosed incorrectly in 70% to 77% of suspected cases. The diagnosis uncertainty can generate an important pitfall when interpreting long-term outcomes, including costs. Moreover, because of anonymized health-related data, adequately analyzing the influence of clinical characteristics on outcomes is impossible. To overcome this limitation, a person-based approach that incorporates biopsychosocial (BPS) profiles of eligible people into models seems appropriate to assess the impact of CRPS and other BPS factors on expenditures. In CRPS, healthcare costs were found to be influenced by BPS factors including age, sex, co-morbidity, employment status, and the insurance source of claims (private or public insurance).8
The CRPS also compromises the work incapacity. According to a recent systematic review, 30% to 40% of patients with CRPS had not returned to work at the 12-month follow-up, and a further 27% to 35% would require some form of workplace adaptation.9 However, the quality of data obtained from this systematic review remains limited due to high attrition bias and variations in diagnostic criteria.9 In addition, predictors for the return to work in CRPS were often based on cross-sectional or univariate analysis due to small sample sizes.10–12 We expect that a multivariate longitudinal model predicting the work incapacity in patients with CRPS might help to better understand this condition. Among the indices for work incapacity, the time to fitness for work (TFW) is a valid measure and independent to the economic context.13 This time, determined by doctors and/or insurers, is when the person is “medically” declared fit for work in considering workplace, ethical, economic and legal criteria.14,15
We aimed to assess the healthcare costs and the TFW of people with chronic CRPS type 1 (those without documented nerve injury) of the hand, due to a musculoskeletal trauma over the 5 years after the accident by using insurance data, then compare with patients with similar hand impairments but without CRPS. We also aimed to identify factors associated with these outcomes from a BPS perspective. The social costs are out of the scope in our study because they are strongly influenced by the income of individuals.
Materials and Methods
Study Design
This is a single-center, comparative and longitudinal study of 5-year follow-up.
Study Population
Between January 2007 and June 2016, we consecutively included patients of working age (18–65 years old) admitted for rehabilitation after a wrist or hand trauma at a Swiss rehabilitation clinic. The reasons for admission were persistent pain > 3 months, functional limitations, therapeutic failure of usual outpatient care, and/or inability to return to work. Most patients were blue-collar workers and insured by Suva, the main trauma insurer in Switzerland, from which insurance data were available.
Patients were divided into two groups: CRPS and non-CRPS. Diagnosis of CRPS was based on the criteria of the “International Association for the Study of Pain” 199416 and the French diagnostic criteria17 from 2007 to 2009; since 2010 the Budapest’s criteria18 has been used and applied. Due to the use of different sets of diagnostic criteria, the medical records of all patients were retrospectively reviewed by a senior physician specializing in rheumatology, physical medicine, and rehabilitation with many years of experience in CRPS care (MK)19 to confirm the diagnosis of CRPS, particularly for patients treated between 2007 and 2009.
Exclusion criteria included: peripheral nerve lesions on the same side of the injury or multiple injury, and hand-shoulder syndrome patients. To obtain a homogenous group, patients with CRPS type II (those with a documented nerve injury) were also excluded. We also excluded patients not insured by Suva because costs and work incapacity could not be obtained.
The non-CRPS group had to fulfill all inclusion criteria, but the existence of CRPS was ruled out by the expert clinician. The non-CRPS group served as the reference group. More details can be found in a previous publication using the same samples.20
Measurements of Predictors
Sociodemographic and Clinical Variables at Admission
Age of the person (in years); sex; injury severity (severe, moderate, minor) based on Abbreviated Injury Scale score;21 education (compulsory school vs higher education); work-related accident (yes or no); work contract before injury (yes or no), pain assessed on a visual analogue scale (from 2006 to 2013) or by the Brief Pain Inventory questionnaire22 (from 2014 to 2016) and then converted to a visual analogue scale score; disability assessed by the Disabilities of the Arm, Shoulder and Hand (DASH) questionnaire;23 BPS complexity assessed by the INTERMED questionnaire24,25 and psychiatric comorbidities diagnosed by psychiatrists. Each patient underwent psychiatric evaluation conducted by a senior psychiatrist upon entry after the initial assessment conducted by the treating rehabilitation physician. The diagnosis of psychiatric comorbidities was based on the International Classification of Diseases (ICD-10) criteria.26
Intermed
The INTERMED is a validated questionnaire used to assess BPS complexity in patients.25,27 The INTERMED has been demonstrated to identify patients with complex BPS, those at risk for adverse health outcomes20,28,29 and those with high use of healthcare services.27,30 A trained nurse conducted the semi-structured interview to obtain the INTERMED score within 3 days after admission. For each of the 4 domains of the INTERMED questionnaire (biological, psychological, social, and health care), 2 items regarding the patient’s history and current status and one item regarding the patient’s prognosis are rated with a score ranging from 0 to 3. For each domain, the score ranges from 0 to 15, which leads to a total score of 0 to 60 (highest case complexity). Detailed information about the INTERMED can be found at http://www.intermedconsortium.com/.
Outcomes
Healthcare costs and TFW (days) were retrieved over a 5-year follow-up starting with the registration of the accident at the insurance company (Suva). In Switzerland, accident insurance is mandatory and covers all accident-related healthcare costs and pays for sick leave for both occupational and non-occupational accidents. The healthcare costs comprise all expenditures allocated for diagnostic procedures (eg, medical consultations, laboratory, or radiological examinations) and treatment (eg, surgery, medication, hospitalisation, and rehabilitation, including physiotherapy/occupational therapy). The healthcare costs were in Swiss francs (CHF) and are presented in US dollars using the average exchange rate from 2007 to 2021 (1 CHF = 1.011 USD).31
The TFW is defined as number of days for which compensation was paid by the insurer between the accident and the fitness for work over the 5 years after the accident. The fitness for work is assessed by the treating physician and/or the insurer’s medical officer. Compensation payments include two forms in a consecutive manner (daily allowances and/or permanent disability pensions). Daily allowances are paid until the employee has returned to work (or is fit to work) or until the employee is declared permanently disabled. Once the employee is deemed permanently disabled, the compensation payments switch from daily allowances to permanent disability pensions, which are defined analogously. Compensation payments stop when the employee has return to work or is deemed fit to work. Times with partial work incapacity are counted pro rata (ie, 10 days at 50% work capacity are counted as 5 days). The number of days with compensation for part-time employees was defined in the same way.
Statistical Analysis
Baseline characteristics between CRPS and non-CRPS groups were compared by chi-squared test for sex, injury severity, work-related accident, education, work contract, psychiatric comorbidities, Student t-test for age, pain intensity, DASH and INTERMED total scores; and Wilcoxon rank sum tests for TFW. The difference in the cumulative percentage of patients being unfit for work between the 2 groups was estimated using the Log rank test and Kaplan-Meier survival function.
Generalized estimation equations (GEEs) were used to assess the independent effect of CRPS on healthcare costs for the whole cohort, and to identify the significant factors related to costs in the two groups. To account for selection bias, the models were adjusted for the following covariates collected at admission: age, sex, education, work-related accident, work contract, injury severity, pain severity, psychiatric comorbidities, DASH disability and INTERMED total scores. Given the number of covariates, the sample size is estimated between 100 and 200 patients for each group.32 The GEE, an extension of generalized linear models, allows regression analyses on dependent variables that are non-normally distributed for longitudinal data.33 For healthcare costs (non-normally distributed variable), we applied a logarithmic link, then a gaussian function in the models. For model selection, we tested the quasi-likelihood under the quasi-information criterion (QIC) with different variance structures: exchangeable, autoregressive AR(1) or AR(2).34 The AR(2) was chosen because it had the smallest QIC among different variance structures. The coefficients in the model estimate the average change of response variable for every 1-unit increase in a covariate.33
A Cox proportional-hazards regression model was used to examine the effect of CRPS on TFW for the whole cohort. A full model was performed to examine the effects of above-mentioned factors on the probability of being fit for work at 5 years after the trauma for both groups. To complete the analyse, a reduced model with backward selection procedure removing predictors with p > 0.10 was also performed. A hazard ratio (HR) < 1 showed a decreased probability of being fit for work, and CI expressed the confidence intervals. The assumption of proportional hazards was checked for each covariate by plotting the Schoenfeld residuals against the work incapacity duration and fitting a smoothed curve. This hypothesis was found acceptable for all predictors.
The overall proportion of missing data in our study was 18% for all variables included. The reasons of missing data were mostly due to the failure to send or retrieve questionnaires, and loss of data from paper registration to an electronic database. In addition, the outcomes were not different between participants with or without missing data (Table S1). Therefore, missing data appeared to be missing completely at random, thus complete-case analysis was used as it produces unbiased estimates.35
P < 0.05 was considered statistically significant. All analyses were performed with Stata 16.0 (StataCorp LP, College Station, TX, USA).
Ethics Approval
Access to healthcare and social costs is strictly restricted to scientific employees of Suva. To guarantee data confidentiality, all data were anonymized. This retrospective comparative study was approved by the ethics committee of the local medical association (CER-VD 2021–01222). Our study complies with the Declaration of Helsinki.
Results
Sociodemographic and Clinical Characteristics Between CRPS and Non-CRPS Groups
We included 148 patients with chronic CRPS of the hand and 273 patients without CRPS. Figure 1 presents the flow chart of the study. CRPS and non-CRPS patients did not significantly differ in initial injury severity, education, work contract, work-related accident, or the INTERMED total score (Table 1).
 |
Table 1 Socio-Demographic and Clinical Characteristics Between CRPS and Non-CRPS Patients |
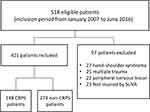 |
Figure 1 Flow chart of the study. |
The proportion of women, as well as the mean age, DASH disability scores were significantly higher for CRPS than non-CRPS patients: 30% vs 10%, p<0.001; 44.0 vs 40.6 years, p=0.002; 58.4 vs 49.7 points, p<0.001, respectively.
Outcomes Between CRPS and Non-CRPS Groups
The median healthcare costs were significantly higher for the CRPS than non-CRPS group from 1 year to 5 years after the accident (Table 2). After adjusting for covariates, CRPS was associated with an increase of 20% (≈ 8200 USD) in healthcare costs (β = 1.20, 95% CI = 1.08–1.35, p<0.001) as compared with non-CRPS (Table 3).
 |
Table 2 Median and Interquartile Ranges for Cumulative Healthcare Costs (in 1000 USD) from 1 to 5 Years After the Trauma for CRPS and Non-CRPS Groups |
 |
Table 3 Independent Effects of CRPS on Healthcare Costs and Time to Fitness for Work for the Whole Cohort |
The median TFW was longer for CRPS than non-CRPS patients (816 vs 672 days, p = 0.02). However, after adjusting for covariates, TFW did not differ between the two groups (HR = 0.94, 95% CI = 0.73–1.21, p = 0.61) (Table 3).
The Kaplan-Meier function for TFW for the two groups was presented in the Figure 2. The percentage of patients being unfit for work in the first year after the accident was 84% for CRPS and 80% for non-CRPS, but then this percentage decreased sharply and reached a final minimal percentage (<5%) at 5-year in the two groups. Interestingly, the TFW curve was comparable between the two groups (Log rank test=0.35).
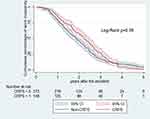 |
Figure 2 Kaplan-Meier analysis of time to fitness for work in the chronic complex regional pain syndrome (CRPS) and non-CRPS groups. |
Factors Related to Healthcare Costs
For CRPS patients, increased healthcare costs were associated with moderate (β = 1.26; 95% CI = 1.08–1.46, p = 0.004) or severe (β = 1.73; 95% CI = 1.34–2.24, p < 0.001) initial injury as compared with minor injury (Table 4); or with the INTERMED total score (β = 1.014 per score point; 95% CI = 1.001–1.028, p = 0.030) and the DASH disability score (exp β = 1.008 per score point; 95% CI = 1.005–1.012, p<0.001) (Table 4). The healthcare costs were expected to increase by 1.4% (≈ 650 USD) for every additional INTERMED score point (0–60 points) and to increase by 0.8% (≈ 370 USD) for every additional disability score point (0–100 points).
 |
Table 4 Factors Associated with Healthcare Costs in CRPS and Non-CRPS Groups According to Generalized Estimation Equation Models |
For non-CRPS patients, increased healthcare costs were associated with only severe initial trauma (exp β= 1.68; 95% CI = 1.36–2.09, p <0.001) (Table 4).
Factors Related to TFW
For CRPS patients, longer TFW was associated with severe initial injury (HR= 0.31, 95% CI = 0.14–0.67, p = 0.003), or with increased INTERMED score (HR= 0.95 for each additional point, 95% CI = 0.91–0.98, p = 0.006) or DASH disability score (HR= 0.98 for each additional point, 95% CI 0.97–0.99, p = 0.001), no work contract (HR= 0.61, 95% CI = 0.39–0.94 p = 0.03) (Table 5). In the reduced model, longer TFW was also associated with low educational level (HR=0.62, 95% CI:0.41–0.93, p=0.02) together with other significant predictors obtained from the full model (Table S2).
 |
Table 5 Factors Associated with the Time to Fitness for Work in CRPS and Non-CRPS Groups According to Cox Proportional-Hazard Models (Full Model) |
For non-CRPS patients, longer TFW was associated with male sex (HR 0.55, 95% CI = 0.33–0.93, p = 0.02), or with increased DASH disability score (HR= 0.99 for each additional point, 95% CI = 0.98–0.99, p = 0.03) in the full model (Table 5).
Discussion
During 5 years after the injury leading to CRPS, the presence of chronic CRPS in patients with hand impairments was significantly associated with increased healthcare costs. However, the magnitude of difference in costs between CRPS and non-CRPS groups (1.2 times) was not as high as that reported with a population-based approach (13 times).1 The median TFW was longer in CRPS, however, after adjusting for covariates, it did not differ between the two groups. In addition, the cumulative percentage of patients being unfit for work was comparable between the two groups. For CRPS patients, predictors of healthcare costs were the level of the initial trauma, the INTERMED, and DASH disability scores. Predictors of longer TFW were severe initial injury, low educational level, no work contract before the injury, high scores of INTERMED and DASH disability.
The healthcare costs for CRPS in our study at 5 years after the accident were about 2 times higher than those reported in an earlier Swiss population-based study.1 The main reason for this discrepancy is probably that we included chronic and refractory CRPS, which might represent the most expensive form. The earlier study1 used ICD-10 codes as diagnostic criteria in register-based data, so the sample might be more heterogeneous than ours in terms of disease severity and duration. In addition, the comparison of healthcare costs in CRPS within or between countries is difficult or even impossible given the regional imbalance, the constant increase in medical expenses, and differences in medical expenses among specialties.5 Also, the presence of chronic CRPS in hand impairments was associated with 1.2 times higher healthcare costs compared to the reference group, but not as much as previously reported (13 times).1 This finding might be due to the reference and CRPS groups being relatively similar in terms of initial hand impairments and socio-demographic characteristics. A longitudinal study in the United States (US) found the diagnosis of CRPS associated with an increase in total costs (2.17-fold) and pain medicine costs (2.56-fold) as compared with baseline costs.8
The median TFW was longer in the CRPS than in the non-CRPS group. However, after adjusting for covariates, the presence of CRPS was no longer associated with an increased probability of work incapacity. The percentage of patients being unfit for work in the first year after the accident was 84% in the CRPS (Figure 2), which was higher than that described in the recent systematic review of 7 studies.9 But this percentage decreased sharply during the 5-year follow-up after the accident. There has been a wide discrepancy surrounding the rate of work incapacity in CPRS. Sandroni et al found permanent job restrictions related to CRPS in only 11% of the cases in their US study from review data of 10 years.36 However, De Mos et al found a high impact of diseases on the ability to work in their Netherlands study: 31% of participants were permanently incapable of working even at 5.8 years after the initiating injury.3 This discrepancy might be likely due to differences in outcome definition or social insurance systems. In the Netherlands, all injured workers receive financial compensation from the government for sick leave, whereas in the US, this is less common.3 It has been shown that different aspects in the compensatory systems (access to benefit, slow case management, size of wage benefit) might also affect the return to work.37
To our knowledge, this is the first study that aimed to identify the relevant factors associated with healthcare costs and work incapacity in CRPS by modeling longitudinal insurance data. The main healthcare cost drivers were severe or moderate initial injury, level of disability, and BPS complexity. The healthcare costs were expected to increase by 1.4% for every additional INTERMED score point (0–60 points) and by 0.8% for every additional disability point (0–100). In the literature, studies that reported factors related to healthcare costs in CRPS were scarce. Previous study8 demonstrated that significant predictors of pain medication costs in patients with CRPS were age, sex, co-morbidity, employment status, and the insurance source of claims (private or public insurance).
Our findings agree with previous studies demonstrating injury severity and disability38 and educational level10,12 as predictors for longer duration of work absence in CRPS. The TFW in our study was also predicted by the presence of work contract and level of BPS complexity assessed by the INTERMED questionnaire. The INTERMED questionnaire might be considered as a useful screening tool for patients with high-risk of poor outcomes,20,27,28 including healthcare costs and TFW. In the literature, other factors associated with favorable work prognosis in CRPS were: a sedentary or white-collar job,10 or early diagnosis (within 8 months).12 Interestingly, depression but not pain intensity or CRPS severity was associated with the longer work absence in CRPS.38
Although we could not establish a direct cause and effect, this research may have clinical implications. We demonstrated the significant associations of physical disability and BPS factors with healthcare costs and TFW. Future studies should determine whether intervention programs for these factors could improve the outcomes. Previous study has shown that addressing BPS complexity for patients after trauma is pertinent for providing good care and improving the outcome.39
Strengths and Limitations
This study has many strengths: the relatively large sample for a rare chronic pain condition, the long-term follow-up, and the design of a comparative study. In addition, the RTW data obtained from insurance claims has the advantage of no loss to follow-up or recall bias as observed in the RTW based on questionnaire. These two methods share some agreement and give complementary information on others.15 The duration of follow-up is long enough as it often takes up to four years until the closure of the case (www.unfallstatistik.ch). Furthermore, our comparative group is very similar, which allows a more judicious comparison between groups. This person-based approach provides additional information as compared to the population-based approach.
Our study also has several limitations. First, our sample is mainly composed of men and blue-collar workers. The exposure group was patients with chronic CRPS type 1 of the hand which is the most common form of the condition.5 This population bias might limit the generalization of results. However, these patients are also likely the source of much of the costs and are vulnerable to return to work. Second, although the models involved a wide range of factors, potentially relevant factors influencing the return to work such as patients’ return-to-work expectations and insurance systems have not been investigated.40,41 Third, we do not have data to estimate intangible costs (costs related to pain and suffering).42 Furthermore, a more in-depth assessment of the 4 dimensions assessed by the INTERMED (biological, psychological, social, and healthcare system) would be helpful but would represent a greater burden for patients as well as clinicians and researchers in that a batch of questionnaires would be required.
Conclusion
Healthcare costs were higher for patients with hand impairments complicated by chronic CRPS than those without CRPS. However, the magnitude of difference in costs (20%) between CRPS and non-CRPS patients was not as high as that reported with a population-based approach. Overall, the TFW did not significantly differ between the 2 groups. For CRPS patients, predictors of healthcare costs were severe or moderate initial trauma, the INTERMED, and DASH disability scores. Factors associated with longer TFW were severe initial injury, low educational level, not having a work contract, high INTERMED and DASH disability scores. Our results stress the importance of addressing these factors, both for providing good care and for improving the outcome in CRPS patients. We also suggest conducting additional person-based comparative studies to better understand the BPS factors associated with the burden of CRPS on both patients and society.
Abbreviations
AR, Autoregressive; BPS, Biopsychosocial; CI, Confidence Intervals; CRPS, Complex regional pain syndrome; DASH, Disabilities of the Arm, Shoulder, and Hand; GEE, Generalized estimation equations; HR, Hazard Ratio; ICD, International Classification of Diseases; QIC, Quasi-information criterion; TFW, Time to fitness for work; VAS, Visual Analog Scale.
Data Sharing Statement
All datasets used and analyzed during the current study are available from the corresponding author upon reasonable request.
Ethics Approval and Informed Consent
This retrospective comparative study was approved by the ethics committee of the local medical association (Commission cantonale d'ethique de la recherche sur l'être humain (CER-VD 2021-01222)).
Author Contributions
HPD, BL, and FL contributed to the conceptualization of the research project. HPD had full access to all the data in the study, performed the statistical analysis, and synthesized the results. SMS analyzed the integrity of the insurance data. HPD, BL, SMS, MK, PV, CB, and FL analyzed and interpreted the results. HPD and FL wrote the first draft of the manuscript. All authors made a significant contribution to the work reported, and took part in drafting, revising, or critically reviewing the article. All authors gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest.
References
1. Scholz-Odermatt SM, Luthi F, Wertli MM, Brunner F. Direct health care cost and work incapacity related to complex regional pain syndrome in Switzerland: a retrospective analysis from 2008 to 2015. Pain Med. 2019;20(8):1559–1569. doi:10.1093/pm/pnz030
2. Rolls C, McCabe C, Llewellyn A, Jones GT. What is the incidence of complex regional pain syndrome (CRPS) Type I within four months of a wrist fracture in the adult population? A systematic review. Hand Therapy. 2020;25(2):45–55. doi:10.1177/1758998320910179
3. de Mos M, Huygen FJ, van der Hoeven-Borgman M, Dieleman JP, Ch Stricker BH, Sturkenboom MC. Outcome of the complex regional pain syndrome. Clin J Pain. 2009;25(7):590–597. doi:10.1097/AJP.0b013e3181a11623
4. van Velzen GAJ, Perez R, van Gestel MA, et al. Health-related quality of life in 975 patients with complex regional pain syndrome type 1. Pain. 2014;155(3):629–634. doi:10.1016/j.pain.2013.12.017
5. Kim H, Lee CH, Kim SH, Kim YD. Epidemiology of complex regional pain syndrome in Korea: an electronic population health data study. PLoS One. 2018;13(6):e0198147. doi:10.1371/journal.pone.0198147
6. Frolke JP, van Rumund A, de Waardt D, et al. Complex regionaal pijnsyndroom type 1? Bij 77% van de patiënten een andere diagnose gesteld [Complex regional pain syndrome type 1? In 77% of people had a different diagnosis]. Ned Tijdschr Geneeskd. 2009;153(12):550–553. Dutch.
7. Mailis-Gagnon A, Lakha SF, Allen MD, Deshpande A, Harden RN. Characteristics of complex regional pain syndrome in patients referred to a tertiary pain clinic by community physicians, assessed by the Budapest clinical diagnostic criteria. Pain Med. 2014;15(11):1965–1974. doi:10.1111/pme.12584
8. Elsamadicy AA, Yang S, Sergesketter AR, et al. Prevalence and cost analysis of complex regional pain syndrome (CRPS): a role for neuromodulation. Neuromodulation. 2018;21(5):423–430. doi:10.1111/ner.12691
9. Johnson S, Cowell F, Gillespie S, Goebel A. Complex regional pain syndrome what is the outcome? - A systematic review of the course and impact of CRPS at 12 months from symptom onset and beyond. Eur J Pain. 2022;26(6):1203–1220. doi:10.1002/ejp.1953
10. Dumas S, Pichon B, Dapolito AC, et al. Work prognosis of complex regional pain syndrome type I: multicenter retrospective study on the determinants and time to return to work. J Occup Environ Med. 2011;53(12):1354–1356. doi:10.1097/JOM.0b013e318239e0ef
11. Dauty M, Renaud P, Deniaud C, Tortellier L, Dubois C. Conséquences professionnelles des algodystrophies [Professional outcome of reflex sympathetic dystrophy]. Ann Readapt Med Phys. 2001;44(2):89–94. French. doi:10.1016/S0168-6054(00)00065-9
12. Kang JE, Kim YC, Lee SC, Kim JH. Relationship between complex regional pain syndrome and working life: a Korean study. J Korean Med Sci. 2012;27(8):929–933. doi:10.3346/jkms.2012.27.8.929
13. Young AE, Wasiak R, Gross DP. Recurrence of work-related low back pain and disability: association between self-report and workers’ compensation data. Spine. 2013;38(26):2279–2286. doi:10.1097/BRS.0000000000000016
14. Serra C, Rodriguez MC, Delclos GL, Plana M, Gomez Lopez LI, Benavides FG. Criteria and methods used for the assessment of fitness for work: a systematic review. Occup Environ Med. 2007;64(5):304–312. doi:10.1136/oem.2006.029397
15. Vuistiner P, Luthi F, Erhart P, Scholz SM, Deriaz O. Subjective perceptions as prognostic factors of time to fitness for work during a 4-year period after inpatient rehabilitation for orthopaedic trauma. Swiss Med Wkly. 2015;145:w14235. doi:10.4414/smw.2015.14235
16. Merksey H, Bogduk N. Classification of Chronic Pain: Description of Chronic Pain Syndromes and Definitions of Pain Term. Seattle: IASP Press; 1994.
17. Doury PC. Algodystrophy. A spectrum of disease, historical perspectives, criteria of diagnosis, and principles of treatment. Hand Clin. 1997;13(3):327–337. doi:10.1016/S0749-0712(21)00094-9
18. Harden RN, Bruehl S, Perez RS, et al. Validation of proposed diagnostic criteria (the “Budapest Criteria”) for complex regional pain syndrome. Pain. 2010;150(2):268–274. doi:10.1016/j.pain.2010.04.030
19. Konzelmann M, Deriaz O, Luthi F. Diagnosis of partial complex regional pain syndrome type 1 of the hand: retrospective study of 16 cases and literature review. BMC Neurol. 2013;13:28. doi:10.1186/1471-2377-13-28
20. Duong HP, Konzelmann M, Vuistiner P, et al. Psychiatric Comorbidity and Complex Regional Pain Syndrome Through the Lens of the Biopsychosocial Model: a Comparative Study. J Pain Res. 2020;13:3235–3245. doi:10.2147/JPR.S278614
21. Baker SP, O’Neill B, Haddon W
22. Cleeland CS, Ryan KM. Pain assessment: global use of the Brief Pain Inventory. Ann Acad Med Singap. 1994;23(2):129–138.
23. Hudak PL, Amadio PC, Bombardier C. Development of an upper extremity outcome measure: the DASH (disabilities of the arm, shoulder and hand) [corrected]. The Upper Extremity Collaborative Group (UECG). Am J Ind Med. 1996;29(6):602–608. doi:10.1002/(SICI)1097-0274(199606)29:6<602::AID-AJIM4>3.0.CO;2-L
24. Huyse FJ, de Jonge P, Lyons JS, Stiefel FC, Slaets JP. INTERMED: a tool for controlling for confounding variables and designing multimodal treatment. J Psychosom Res. 1999;46(4):401–402. doi:10.1016/s0022-3999(98)00099-3
25. Huyse FJ, Lyons JS, Stiefel FC, et al. ”INTERMED”: a method to assess health service needs. I. Development and reliability. Gen Hosp Psychiatry. 1999;21(1):39–48. doi:10.1016/S0163-8343(98)00057-7
26. World Health Organization. The ICD-10 classification of mental and behavioural disorders. Available from: https://apps.who.int/iris/bitstream/handle/10665/37108/9241544554.pdf.
27. Stiefel FC, de Jonge P, Huyse FJ, et al. ”INTERMED”: a method to assess health service needs. II. Results on its validity and clinical use. Gen Hosp Psychiatry. 1999;21(1):49–56. doi:10.1016/S0163-8343(98)00061-9
28. Luthi F, Stiefel F, Gobelet C, Rivier G, Deriaz O. Rehabilitation outcomes for orthopaedic trauma individuals as measured by the INTERMED. Disabil Rehabil. 2011;33(25–26):2544–2552. doi:10.3109/09638288.2011.579223
29. Ludwig G, Dobe-Tauchert P, Nonnast-Daniel B, et al. Assessing psychosocial vulnerability and care needs of pretransplant patients by means of the INTERMED. Z Psychosom Med Psychother. 2014;60(2):190–203. doi:10.13109/zptm.2014.60.2.190
30. Koch N, Stiefel F, de Jonge P, et al. Identification of case complexity and increased health care utilization in patients with rheumatoid arthritis. Arthritis Rheum. 2001;45(3):216–221. doi:10.1002/1529-0131(200106)45:3<216::AID-ART251>3.0.CO;2-F
31. US Dollar Swiss Franc exchange rate Available from: https://www.macrotrends.net/2558/us-dollar-swiss-franc-exchange-rate-historical-chart.
32. Harrell FE
33. Ballinger GA. Using generalized estimating equations for longitudinal data analysis. Organ Res Methods. 2004;7(2):127–150. doi:10.1177/1094428104263672
34. Cui J. QIC program and model selection in GEE analyses. Stata J. 2007;7(2):209–220. doi:10.1177/1536867X0700700205
35. Kang H. The prevention and handling of the missing data. Korean J Anesthesiol. 2013;64(5):402–406. doi:10.4097/kjae.2013.64.5.402
36. Sandroni P, Benrud-Larson LM, McClelland RL, Low PA. Complex regional pain syndrome type I: incidence and prevalence in Olmsted county, a population-based study. Pain. 2003;103(1–2):199–207. doi:10.1016/S0304-3959(03)00065-4
37. Bartys S, Frederiksen P, Bendix T, Burton K. System influences on work disability due to low back pain: an international evidence synthesis. Health Policy (New York). 2017;121(8):903–912. doi:10.1016/j.healthpol.2017.05.011
38. Bean DJ, Johnson MH, Heiss-Dunlop W, Kydd RR. Factors associated with disability and sick leave in early complex regional pain syndrome type-1. Clin J Pain. 2016;32(2):130–138. doi:10.1097/AJP.0000000000000234
39. de Jonge P, Hadj FB, Boffa D, et al. Prevention of major depression in complex medically ill patients: preliminary results from a randomized, controlled trial. Psychosomatics. 2009;50(3):227–233. doi:10.1176/appi.psy.50.3.227
40. Hara KW, Bjorngaard JH, Jacobsen HB, et al. Biopsychosocial predictors and trajectories of work participation after transdiagnostic occupational rehabilitation of participants with mental and somatic disorders: a cohort study. BMC Public Health. 2018;18(1):1014. doi:10.1186/s12889-018-5803-0
41. Duong HP, Garcia A, Hilfiker R, Leger B, Luthi F. Systematic review of biopsychosocial prognostic factors for return to work after acute orthopedic trauma: a 2020 update. Front Rehabil Sci. 2021;2:791351. doi:10.3389/fresc.2021.791351
42. Fautrel B, Boonen A, de Wit M, Grimm S, Joore M, Guillemin F. Cost assessment of health interventions and diseases. RMD Open. 2020;6:3. doi:10.1136/rmdopen-2020-001287
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
