Back to Journals » Clinical Interventions in Aging » Volume 13
Health status, health behaviors, and the ability to perform everyday activities in Poles aged ≥65 years staying in their home environment
Authors Wróblewska I , Zborowska I , Dąbek A, Susło R , Wróblewska Z, Drobnik J
Received 24 September 2017
Accepted for publication 7 December 2017
Published 1 March 2018 Volume 2018:13 Pages 355—363
DOI https://doi.org/10.2147/CIA.S152456
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Richard Walker
Izabela Wróblewska,1,2 Iwona Zborowska,1 Anna Dąbek,1 Robert Susło,1 Zuzanna Wróblewska,2 Jarosław Drobnik1
1Institute of Gerontology, Faculty of Health Sciences, Wrocław Medical University, Wrocław, Poland; 2Faculty of Natural Sciences and Technology, Karkonosze College, Jelenia Góra, Poland
Background: The incidence of chronic diseases increases with age; about 73% of people who are aged ≥60 years suffer from at least 1 chronic disease, and among those older than 70 years, chronic diseases afflict more than >84% of the population. According to epidemiological data, at least 4 chronic disease types coexist in senior citizens, causing their disability. These are mainly cardiovascular diseases; motor system diseases; ophthalmological, auditory, neurological, and mental diseases; and mental impairment. They worsen or limit self-dependence in everyday activities. The process begins with complex activities and advances with age. At first, functional performance deficits are discreet; then, they may gradually lead to complete dependence on other people or institutions.
Objective: This study aimed to assess the relationship between diseases and health behaviors, as well as the everyday functioning of people aged ≥65 years staying in their home environment.
Methods: The research involved 504 elderly people. The inclusion criteria were age (≥65 years) and staying in one’s own home environment. The direct interview technique was applied, as well as use of proprietary interview questionnaire and standardized tools used in geriatrics: Barthel scale, measuring performance in everyday activities, and the Instrumental Activities of Daily Living scale, assessing complex everyday activities.
Results: The most frequent disease among the responders was arterial hypertension (77.58%), followed by degenerative joint disease (62.10%), and circulatory failure (43.23%). Lower functional performance was associated with circulatory failure, cerebral stroke, atherosclerosis, Alzheimer’s disease, diabetes, Parkinson’s disease, degenerative joint disease, and bronchial asthma. Performance worsening significantly influenced the frequency of hospitalizations, with a mean score of 4.31 per person. Medical rehabilitation was practiced by 18.65% of the responders.
Conclusion: Circulatory failure, cerebral stroke, atherosclerosis, bronchial asthma, diabetes, degenerative joint disease, Parkinson’s disease, and Alzheimer’s disease negatively affect functional performance in elderly people. Hospitalization rates increase with lowering independence in everyday functioning. Future research is needed with regard to the relationship between the practiced rehabilitation and independence in everyday functioning of the elderly.
Keywords: the elderly, functional performance, health behaviors
Introduction
The incidence of chronic diseases increases with age; about 73% of people who are aged ≥60 years suffer from at least 1 chronic disease, and among those older than 70 years, chronic diseases afflict >84% of the population.1,2
Research shows that in people aged ≥60 years, at least 4 chronic disease types coexist; also, simultaneous occurrence of somatic and mental diseases is often observed.3 In 85% of cases, chronic diseases become the main reason for disability in people who are ≥60 years old.4–6 Among those diseases, the most frequent are cardiovascular diseases; motor system diseases; ophthalmological, auditory, neurological, and mental diseases; and mental impairment.7,8 They add to the worsening or loss of elderly people’s self-dependence in performing everyday activities,9,10 which can be divided into simple (basic) and complex activities. The former include moving, eating, bathing, dressing, undressing, using the toilet, and controlling sphincters. Among the latter are included the tasks of using the telephone, doing shopping, preparing meals, preparing and taking medicines, performing light and heavy housework, and managing money.11–13
Previous research14–17 proves that the loss of self-dependence in everyday functioning begins with complex activities and advances with age. At first, functional performance deficits are discreet; however, when increasing, they may gradually lead to complete dependence on other people or institutions.14–17 The aim of the present study was to assess the relationship between the occurring diseases and chosen health behaviors on the one hand, and the everyday functioning of people aged ≥65 years staying in their home environment on the other.
Methods
The study involved 535 people aged ≥65 years staying under the care of a family physician in an outpatient clinic, living in a city of >500,000 inhabitants. The inclusion criteria were as follows: age ≥65 years, staying in home environment, lack of significant cognitive function disorders (at least 19 points in the Mini-Mental State Examination), and providing informed consent to take part in the study. During the initial qualification, 31 senior citizens were excluded; as a result, 504 elderly people took part in the research. The method of a diagnostic survey was applied, with the direct interview technique. The authors implemented proprietary interview questionnaires (Figure S1), allowing the collection of sociodemographic data and information related to the health status of the responders. Moreover, standardized tools commonly used in geriatrics were used, namely, the Barthel scale, measuring performance in activities of daily living, and the Instrumental Activities of Daily Living (IADL) scale, assessing complex everyday activities.
All questionnaire participants provided written informed consent.
The relationships between chosen variables were examined with the use of Kendall’s tau test, Kolmogorov–Smirnov test, chi-squared test (χ2), Kruskal–Wallis test, and post hoc Dunn’s test. The statistical calculations were performed with Statistica 6.0PL software. The statistical test results were rounded off in accordance with mathematical rules to 4 decimal points.
The study was approved by the Bioethical Committee of the Wrocław Medical University (Wrocław, Poland).
Results
The analysis of the incidence of particular disease entities in the studied population showed that the number of diseases occurring in the responders ranged from 0 to 7. Only 1.98% of the studied elderly people did not suffer from any known disease. The subjects most often suffered from at 2 disease entities (24.60%), then 3 (21.03%), 4 (19.64%), 1 (18.05%), 5 (9.92%), 6 (4.56%), and – the least frequent – 7 (0.22%).
The disease with the highest incidence in the studied group was arterial hypertension (77.58%). The responders less often suffered from degenerative joint disease (62.10%) or circulatory failure (43.23%).
Comparison of the incidence of the chosen disease entities in the studied group revealed 3 statistically significant differences: women suffered more often from arterial hypertension (P<0.001) and degenerative joint disease (P<0.001) and less frequently from atherosclerosis (P<0.001) (Table 1).
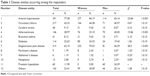  | Table 1 Disease entities occurring among the responders |
Analysis with the Kolmogorov–Smirnov test revealed that responders suffering from circulatory failure, cerebral stroke, atherosclerosis, or degenerative joint disease were older than the other subjects. Moreover, those who were not diagnosed with arterial hypertension turned out to be older than patients affected by the disease. No statistically significant differences were observed in the remaining cases (Table 2).
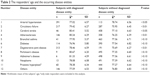  | Table 2 The responders’ age and the occurring disease entities |
At least 1 hospitalization in their previous medical history was declared by 82.54% (n=416) of the responders; out of these, 8.73% (n=44) did not indicate the number of their hospital stays. The average number of hospital stays per subject equaled 4.31 (SD =3.71; median =3; N=460).
No statistically significant difference was noted between men and women with reference to the frequency of hospitalization (P>0.10). In turn, the analysis with Kendall’s tau test showed a statistically significant (τ=0.0933; P<0.01) correlation between aging and rise in the number of hospital stays.
Within the year preceding the study, medical rehabilitation was practiced by only 18.65% (n=94) of the studied subjects. Among them, 91.49% (n=86) pointed at 1 rehabilitation center they used, and 8.51% (n=8) indicated 2 centers.
The responders were most often provided with rehabilitation procedures on an outpatient basis (46.81%) or in hospital (44.69%); only 5.32% took advantage of rehabilitation procedures performed at home. Some senior citizens (11.70%) declared that they simultaneously practiced rehabilitation also in other sites, such as a sanatarium or a prevention and rehabilitation center.
Men (13.71%) used rehabilitation procedures less frequently than women (21.28%) (P<0.05). There were no differences between the sexes with regard to the place where the procedures were applied (P>0.10).
The study subjects who took advantage of medical rehabilitation within the year before the research were younger (mean: 74.95 years old) than the remaining responders (mean: 77.97 years old), the difference being statistically significant (P<0.001). A comparison of the age of those who used rehabilitation services in various centers revealed that those provided with rehabilitation in hospital (P<0.01) or at home (P<0.05) were older than the other rehabilitated elderly.
More than a half of the studied group (n=269; 53.37%) did not use any orthopedic supplies. A total of 178 subjects (35.32%) utilized 1 type of equipment. Others used 2 (n=43; 8.43%), 3 (n=10; 1.98%), 4 (n=2; 0.40%), or 5 (n=2; 0.40%) types of orthopedic supplies.
Kendall’s tau test proved that the number of orthopedic equipment types used by the responders grew with aging (τ=0.3548; P<0.001). Among the most frequently used supplies, there were walking sticks (n=122; 24.21%) and crutches (n=81; 16.07%), then walking frames (n=44; 8.73%), decubitus-preventing mattresses (n=28; 5.56%), orthopedic beds (n=18; 3.57%), wheelchairs (n=17; 3.37%), and lower limb prostheses (n=2; 0.40%).
Comparison of the number of orthopedic equipment types utilized by the study subjects revealed that women used orthopedic supplies significantly more often than men (P<0.001).
The results obtained by the responders in the Barthel scale assessment ranged from 0 (n=7) to 100 points (n=163) (Figure 1). The arithmetic mean equaled 78.11 points (SD =27.78; median =95).
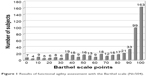  | Figure 1 Results of functional agility assessment with the Barthel scale (N=504). |
The analysis with Kendall’s tau test showed an inversely proportional correlation between the number of disease entities occurring in the responders and the Barthel scale results (τ=−0.3300; P<0.001). The more the number of diseases they suffered from, the lower their performance was in performing basic activities. Lower performance related to basic everyday activities was associated with the presence of circulatory failure, cerebral stroke, atherosclerosis, or Alzheimer’s disease (Table 3).
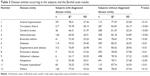  | Table 3 Disease entities occurring in the subjects and the Barthel scale results |
The analysis with Kendall’s tau test revealed that the number of hospitalizations increased with lower Barthel scale results, reflecting worse performance in the basic everyday activities (τ=−0.2302; P<0.001; N=460).
No statistically significant difference (P>0.10) was established in the comparison of mean Barthel scale results for the subjects who had implemented medical rehabilitation during the previous year (79.31 points) vs the remaining responders (77.83 points). However, it was observed that patients rehabilitated in hospital or at home were less efficient in performing basic everyday activities (P<0.01) as compared with senior citizens rehabilitated in an outpatient clinic.
The analysis with the Kolmogorov–Smirnov test revealed that people using orthopedic equipment, irrespective of its type, were significantly less self-dependent with regard to basic everyday activities (P<0.001).
The results obtained by the responders in the assessment of complex activities with the IADL (Lawton) scale ranged from 8 to 24 points. The mean number of points equaled 17.04 (SD =5.8; median =18). The vast majority of the study group (n=458; 90.87%) were subjects requiring help in performing complex activities. Only 9.13% (n=46) of the responders presented full performance in this respect (24 points) (Figure 2).
  | Figure 2 Results of functional agility assessment with the Lawton scale (N=504). |
An inversely proportional correlation was established between the number of disease entities occurring in the responders and the Lawton scale results (τ=−0.3347; P<0.001). The more the number of diseases the responders suffered from, the lower their performance was in performing complex activities.
Apart from arterial hypertension, in all cases of responders with specific diseases, the study subjects achieved significantly lower Lawton scale results, reflecting higher disability with regard to complex activities, as compared with responders without the diseases. The described differences turned out to be statistically significant only for neoplasms, diseases of the prostate, and those classified as “other” (Table 4).
  | Table 4 Disease entities occurring in the subjects and the Lawton scale results |
The analysis with Kendall’s tau test revealed an inversely proportional relationship between the number of hospitalizations and performance of complex activities (τ=−0.2576; P<0.001; N=460).
No statistically significant difference (P>0.10) was established in the comparison of Lawton scale results (17.52; n=94) for the subjects who had implemented medical rehabilitation during the previous year vs the remaining responders (16.92; n=410). Kendall’s tau test showed a correlation between lower scores in performing complex activities and increasing number of orthopedic equipment types used by the study subjects (τ=−0.5250; P<0.001). It was observed that those who used any type of the analyzed orthopedic supplies presented lower self-dependence in performing complex activities as compared with the responders who did not use the equipment (P<0.001).
Discussion
The coexistence of various diseases and complaints contributes to the lowering of senior citizens’ performance in carrying out everyday activities.18–20 It is alleged that >50% of the elderly suffer from at least 3 chronic diseases;21 among them, the most frequent are cardiovascular diseases, motor or nervous system diseases, injuries, and accidents.22
The PolSenior research, carried out in a group of 4979 people aged at least 65 years, proved that the vast majority of the elderly suffer from >1 disease, and the risk of comorbidity and loss of self-dependence increased between the ages of 70 and 84 years.23,24
Analysis of the current study data revealed that chronic diseases were present in the vast majority of the elderly aged ≥65 years. No chronic disease was diagnosed only in 1.98% of responders; the remainder of the group suffered from 1 to 7 diseases, among which the dominating ones were arterial hypertension, degenerative joint disease, circulatory failure, atherosclerosis, diabetes, benign prostatic hyperplasia, and cerebral stroke. These results support those of the research by Borowiak and Kostka25 and Dionyssiotis.26
Analysis of the research results showed that people suffering from such diseases as circulatory failure, cerebral stroke, atherosclerosis, Alzheimer’s disease, diabetes, Parkinson’s disease, degenerative joint disease, and bronchial asthma presented significantly worse performance in everyday activities,27 which, in combination with the responders’ age, can constitute a substantial determinant of hospitalization.1,25,27,28 In the studied population, the majority declared at least 1 hospital stay. It was observed that the hospitalization rate increased with lowering independence in everyday functioning.
Tollén et al29 indicate that in the elderly, rehabilitation is closely connected with prevention, and target not only senior citizens suffering from specific diseases but also those experiencing lower functional performance. The authors suggest that in this group of patients, rehabilitation should be performed by interdisciplinary teams consisting of various specialty physicians, physiotherapists, nurses, psychologists, occupational therapy specialists, speech therapists, and social workers; moreover, simultaneously with medical rehabilitation, social rehabilitation should also be implemented.29 Properly performed geriatric rehabilitation is considered an essential factor in positive aging, as well as in preventing loneliness and social isolation. In turn, its insufficiency or complete omission in elderly people contributes to the development of functional disability and multimorbidity.7
Rolnick et al30 postulate that determining a proper rehabilitation plan and site for senior citizens demands a multidisciplinary assessment of their functional status. According to various authors, rehabilitation aimed at achieving an improvement in the functional status belongs to the most frequently unmet needs of elderly people.30,31
The presented research revealed that in the preceding year, only 1/5 of the responders benefited from rehabilitation and these subjects were younger than the remainder of the studied group. Similar results were obtained by other authors, who additionally observed that the frequency of implementing rehabilitation decreased with aging.32–34
The analysis of the current study material indicated that the rehabilitation center most often visited by the responders was an outpatient clinic or a hospital; rehabilitation services were very rarely provided at home.
The performed research suggests that women are more willing to apply rehabilitation procedures than men. This may result from the fact that among people aged >60 years, disability more often occurs in women35 and, irrespective of its reason, is associated with physical activity constraints, which leads to multiorgan disorders and dependence on other people.
The most frequent causes for functional limitations in women are motor system diseases resulting from degenerative changes in the musculoskeletal system and in the connective tissue, related to degenerative joint disease and occurring in the course of inflammatory diseases of the motor system. The progressing degeneration of the articular cartilage and changes in the subcartilaginous tissue with the formation of exostosis afflict more than half of the population aged ≥65 years and the majority of senior citizens >75 years.36 The problem most often concerns obese women due to decreased effect of sex hormones and limited motor activity.37
Another reason for the constraints discussed could be loss of muscle mass. Sarcopenia, through lowered muscle mass, as well as decreased strength and functional performance of skeletal muscles, contributes to disability in elderly people.38 Its incidence increases with age and depends on sex (women are more often affected). The disease is among the most significant factors leading to decreased aerobic capacity.39
The frequent issues encountered in a rehabilitation clinic also include spine and back pain. One of the varied reasons is osteoporosis, increasing the risk of fractures in postmenopausal women. The lifetime loss of bone mass is bigger in women than in men; it raises the risk of falls – these occur in every third person aged ≥65 years and half of the population >80 years, 3 times more frequently in women.40,41
Dementia is encountered in about 1% of 60-year-old and 40% of 90-year-old people. Its main reason is Alzheimer’s disease, present in 60% of the elderly population, more often in women.23,31
Circulatory system diseases should also be mentioned in this context. They are the most common cause for death in women, especially those ≥75 years of age. Obesity is a significant factor – this health problem most frequently concerns the oldest women. It is among the main reasons for morbidity and mortality, shortens mean life expectancy, predisposes to the development of other diseases, and worsens the course and efficiency of treatment, as well as the prognosis. Literature indicates a high correlation between body mass index increase and the occurrence of degeneration of ankle, knee, and hip joint/intervertebral disk.42
One should conclude that women, because of the incidence of disease entities that impede their everyday functioning, are probably more determined than men to undertake specialized rehabilitation to support therapy.
Although it is still not known which kinds of exercise play the most significant role in improving a patient’s health status, kinesiotherapy constitutes the crucial rehabilitation method in the elderly. It affects the maintenance and development of the range of joint motion, movement coordination, muscle strength, endurance in assuming vertical position, and performance in terms of relearning to walk and improving the general body function as well as preventing hypokinesia. Therefore, regular physical activity is recommended for senior citizens if practiced on the basis of aerobic, power, and stretching exercises.
Physical activity is the most efficient way to prevent and manage health problems in elderly people, to lower the risk of cardiovascular diseases, diabetes, obesity, hypertension, and neoplastic diseases. It also contributes to decreasing mortality.43
Conclusion
Circulatory failure, cerebral stroke, atherosclerosis, bronchial asthma, diabetes, degenerative joint disease, Parkinson’s disease, and Alzheimer’s disease add to the loss of self-dependence in everyday functioning of people aged ≥65 years.
The majority of this elderly population is hospitalized at least once, and the hospitalization rate increases along with worsening functional performance.
Additional research is essential with regard to the relationship between the practiced rehabilitation and independence in everyday functioning of the elderly.
Disclosure
The authors report no conflicts of interest in this work.
References
Palczewska A. System opieki długoterminowej a zapotrzebowanie na ten rodzaj świadczeń. [Long-term care system and demand for such services]. Probl Pielęg. 2010;18(2):198–206. Polish. | ||
Hooyman NR, Kiyak HA. Social Gerontology: A Multidisciplinary Perspective. 8th edition. Boston: Pearson; 2008. | ||
Michałkiewicz H, Wróbel J. Całościowa ocena geriatryczna – narzędzie ważne również dla fizjoterapeutów. [The overall geriatric assessment – tool also important for physiotherapists]. Zamoj Stud Mater Fizjoterapia. 2012;1(35):91–96. Polish. | ||
Metzelthin SF, van Rossum E, de Witte LP, Hendriks MR, Kempen G. The reduction of disability in community-dwelling frail older people: design of a two-arm cluster randomized controlled trial. BMC Public Health. 2010;10:511. | ||
Fillit HM, Rockwood K, Woodhouse K. Brocklehurst’s Textbook of Geriatric Medicine and Gerontology. Philadelphia: Elservier; 2010. | ||
Rizzuto D, Melis RJF, Angleman S, Qiu C, Marengoni A. Effect of chronic diseases and multimorbidity on survival and functioning in elderly adults. J Am Geriatr Soc. 2017;65(5):1056–1060. | ||
Mazurek J, Rymaszewska J, Lurbiecki J. Specyfika i czynniki warunkujące skuteczność fizjoterapii osób starszych w świetle najnowszych doniesień. [Specificity and factors determining the effectiveness of physiotherapy of the elderly – the latest news]. Now Lek. 2012;81(1):70–74. Polish. | ||
Manini T. Development of physical disability in older adults. Curr Aging Sci. 2011;4(3):184–191. | ||
Borowicz A. Testy służące do oceny sprawności funkcjonalnej osób starszych. [Tests for functional assessment in the elderly]. In: Wieczorowska-Tobis K, Kostka T, Borowicz A, editors. Fizjoterapia w geriatrii. [Physiotherapy in Geriatrics]. Warszawa: Wydawnictwo Lekarskie PZWL; 2011:45–60. Polish. | ||
Skalska A. Ograniczenie sprawności funkcjonalnej osób w podeszłym wieku. [Limitation of functional capacity in elderly persons]. Zdr Publ Zarządz. 2011;11(1):50–59. Polish. | ||
Gill TM, Baker DI, Gottschalk M, Peduzzi PN, Allore H, Byers A. A program to prevent functional decline in physically frail, elderly persons who live at home. N Engl J Med. 2002;347(14):1068–1074. | ||
de Labra C, Guimaraes-Pinheiro C, Maseda A, Lorenzo T, Millán-Calenti JC. Effects of physical exercise interventions in frail older adults: a systematic review of randomized controlled trials. BMC Geriatr. 2015;15:154. | ||
de Souto Barreto P. Exercise and health in frail elderly people: a review of randomized controlled trials. Eur Rev Aging Phys Act. 2009;6:75–87. | ||
Cvejin MM, Grujić V, Jakovljević D. Uloga primarne zdravstvene zastite u promociji zdravlja. [The role of primary health care in health promotion]. Med Pregl. 2000;53(5–6):262–265. Croatian. | ||
Nowossadeck S. Demografischer Wandel, Pflegebedürftige und der künftige Bedarf an Pflegekräften. Eine Übersicht. [Demographic change, people needing long-term care, and the future need for carers. An overview]. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 2013;56(8):1040–1047. German. | ||
Carmeli E, Imam B. Health promotion and disease prevention strategies in older adults with intellectual and developmental disabilities. Front Public Health. 2014;2:31. | ||
Dziechciaż M, Guty E, Wojtowicz A, Filip R. Social and health care needs of elderly people living in the countryside in Poland. Ann Agric Environ Med. 2012;19(4):746–750. | ||
Wieczorowska-Tobis K. Podstawowe pojęcia geriatrii i gerontologii. [Basic notions of geriatrics and gerontology]. In: Wieczorowska-Tobis K, Kostka T, Borowicz A, editors. Fizjoterapia w geriatrii. [Physiotherapy in Geriatrics]. Warszawa: Wydawnictwo Lekarskie PZWL; 2011:3–10. Polish. | ||
Strax TE, Luciano L, Dunn AM, Quevedo JP. Aging and developmental disability. Phys Med Rehabil Clin N Am. 2010;21(2):419–427. | ||
Yu F, Kolanowski AM, Strumpf NE, Eslinger PJ. Improving cognition and function through exercise intervention in Alzheimer’s disease. J Nurs Scholarsh. 2006;38(4):358–365. | ||
Piotrowicz K. Opieka ukierunkowana na starszego pacjenta z wielochorobowością – podejście zaproponowane przez Panel Ekspertów Amerykańskiego Towarzystwa Geriatrycznego. [Patient-centered care for older adults with multiple chronic conditions: a stepwise approach from the American Geriatrics Society]. Gerontol Pol. 2013;21(3):63–72. Polish. | ||
Lee PG, Cigolle C, Blaum C. The co-occurrence of chronic diseases and geriatric syndromes: the health and retirement study. J Am Geriatr Soc. 2009;57(3):511–516. | ||
Mossakowska M. Problemy zdrowotne osób w wieku podeszłym – wnioski z projektu PolSenior. [Health problems in the elderly: conclusions from the PolSenior project]. In: Samoliński B, Raciborski F, editors. Zdrowe starzenie się: BIAŁA KSIĘGA. [Healthy Aging: The White Book]. Warszawa: Wydawnictwo Naukowe SCHOLAR; 2013:49–54. Polish. | ||
Robinson TN, Eiseman B, Wallace JI, et al. Redefining geriatric preoperative assessment using frailty, disability and co-morbidity. Ann Surg. 2009;250(3):449–455. | ||
Borowiak E, Kostka T. Oczekiwania na świadczenia opiekuńcze starszych mieszkańców obszaru miejskiego i wiejskiego oraz instytucji opiekuńczo-pielęgnacyjnych. [Demand for nursing care services in the elderly inhabitants of urban and rural areas and elderly patients in care and nursing facilities]. Gerontol Pol. 2010;18(4):207–214. Polish. | ||
Dionyssiotis Y. Analyzing the problem of falls among older people. Int J Gen Med. 2012;5:805–813. | ||
Motl RW, McAuley E. Physical activity, disability, and quality of life in older adults. Phys Med Rehabil Clin N Am. 2010;21(2):299–308. | ||
Admi H, Shadmi E, Baruch H, Zisberg A. From research to reality: minimizing the effects of hospitalization on older adults. Rambam Maimonides Med J. 2015;6(2):e0017. | ||
Tollén A, Fredriksson C, Kamwendo K. Elderly persons’ expectations of day-care rehabilitation. Scand J Occup Ther. 2007;14(3):173–182. | ||
Rolnick JA, Asch DA, Halpern SD. Delegalizing advance directives – facilitating advance care planning. N Engl J Med. 2017;376(22):2105–2107. | ||
Heyn P, Abreu BC, Ottenbacher KJ. The effects of exercise training on elderly persons with cognitive impairment and dementia: a meta-analysis. Arch Phys Med Rehabil. 2004;85(10):1694–1704. | ||
Tobiasz-Adamczyk B, Gałaś A, Brzyski P, Błędowski P, Grodzki T. Dostępność i poziom satysfakcji z opieki medycznej. [Accessibility of medical care and the level of satisfaction]. In: Mossakowska M, Więcek A, Błędowski P, editors. Aspekty medyczne, psychologiczne, socjologiczne i ekonomiczne starzenia się ludzi w Polsce. [Medical, Psychological, Sociological, and Economic Aspects of Aging in Poland]. Poznań: Termedia Wydawnictwa Medyczne; 2012:467–494. Polish. | ||
Inouye SK, Studenski S, Tinetti ME, Kuchel GA. Geriatric syndromes: clinical, research, and policy implications of a core geriatric concept. J Am Geriatr Soc. 2007;55(5):780–791. | ||
Shrivastava SRBL, Shrivastava PS, Ramasamy J. Health-care of elderly: determinants, needs and services. Int J Prev Med. 2013;4(10):1224–1225. | ||
Koziarska-Rościszewska M. Nadciśnienie tętnicze u osób w starszym wieku. [Arterial hypertension in older age]. In: Kostka T, Koziarska-Rościszewska M, editors. Choroby wieku podeszłego. Praktyka lekarza rodzinnego. [Diseases of Older Age. Family Physician’s Practice]. Warszawa: Wydawnictwo Lekarskie PZWL; 2009:42–51. Polish. | ||
Borowicz A. Choroba zwyrodnieniowa stawów. [Degenerative joint disease]. In: Wieczorowska-Tobis K, Kostka T, Borowicz A, editors. Fizjoterapia w geriatrii. [Physiotherapy in Geriatrics]. Warszawa: Wydawnictwo Lekarskie PZWL; 2011:138–153. Polish. | ||
Samborski W. Układ ruchu – choroba zwyrodnieniowa stawów. [Motor system. Degenerative joint disease]. In: Wieczorowska-Tobis K, Talarska D, editors. Geriatria i pielęgniarstwo geriatryczne. [Geriatrics and Geriatric Nursing]. Warszawa: Wydawnictwo Lekarskie PZWL; 2014:271–275. Polish. | ||
Cesari M, Pahor M. Target population for clinical trials on sarcopenia. J Nutr Health Aging. 2008;12:470–478. | ||
Krzymińska-Siemaszko R, Wieczorowska-Tobis K. Ocena sarkopenii u osób starszych – przyczynek do metodologii. [Assessment of sarcopenia in the elderly: a contribution to methodology]. Now Lek. 2012;81(1):16–20. Polish. | ||
LeBlanc KE. Problemy ze strony układu mięśniowo-szkieletowego u osób w starszym wieku. [Musculoskeletal system disorders in the elderly]. In: Rosenthal T, Nughton B, Williams M, editors. Geriatria. [Geriatrics]. Lublin: Czelej; 2009:341–382. Polish. | ||
Skalska A, Gałaś A. Upadki jako czynnik ryzyka pogorszenia stanu funkcjonalnego w starszym wieku. [Falls as a risk factor of worsening the functional status in older age]. Gerontol Pol. 2011;19(3–4):150–160. Polish. | ||
Ll Lloyd GW. Preventive cardiology and cardiac rehabilitation programmes in women. Maturitas. 2009;63(1):28–33. | ||
Ströhle A. Physical activity, exercise, depression and anxiety disorders. J Neural Transm. 2009;116(6):777–784. |
Supplementary material
  | Figure S1 Survey questionnaire. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
