Back to Journals » Risk Management and Healthcare Policy » Volume 14
Health Service Utilization Among Out-of-Pocket Payers and Fee-Wavier Users in Saesie Tsaeda-Emba District, Tigray Region, Northern Ethiopia: A Comparative Cross-Sectional Study
Authors Gessesse A, Yitayal M , Kebede M , Amare G
Received 19 October 2020
Accepted for publication 11 February 2021
Published 18 February 2021 Volume 2021:14 Pages 695—703
DOI https://doi.org/10.2147/RMHP.S287504
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Marco Carotenuto
Ataklti Gessesse,1 Mezgebu Yitayal,2 Mihiretu Kebede,3,4 Getasew Amare2
1Tigray Public Health Institute, Mekelle, Ethiopia; 2Department of Health Systems and Policy, Institute of Public Health, College of Medicine and Health Sciences, University of Gondar, Gondar, Ethiopia; 3Department of Health Informatics, Institute of Public Health, College of Medicine and Health Sciences, University of Gondar, Gondar, Ethiopia; 4Leibniz Institute for Prevention Research and Epidemiology, Bremen, Germany
Correspondence: Getasew Amare P.O. Box – 196, Gondar, Ethiopia
Tel +251910151944
Email [email protected]
Background: Health service utilization among out-of-pocket payers and fee-wavier users and factors associated with it in Saesie Tsaeda-Emba District, Tigray Region, Northern Ethiopia.
Methods: A comparative community-based cross-sectional study was conducted in Northern Ethiopia. Households with at least one person who experienced illness during the last six months were included in the study. Data were collected using a structured and interviewer-administered questionnaire. Bivariable and multivariable logistic regression analyses were used to identify factors associated with the HSU.
Results: In this study, 652 individuals (489 OOP payers and 163 fee waiver users) participated with overall response rate of 98%. The overall HSU among the participants was 44.3% (41.9 for OOP users and 51.5% for fee waiver users). The study revealed that educational status (AOR = 0.35; 95% CI: 0.21, 0.59), family size (AOR = 0.60; 95% CI: 0.37, 0.97) and income level (AOR = 2.09; 95% CI: 1.12, 3.90, and AOR = 4.12; 95% CI: 2.41, 7.53) were factors significantly associated with the HSU among OOP payers. The study also revealed that educational status (AOR = 0.65; 95% CI: 0.21, 0.59), family size (AOR = 0.4; 95% CI: 0.37, 0.97), income level (AOR = 1.12; 95% CI: 1.21, 4.87), and payment mechanism (AOR = 2.21; 95% CI = 1.34, 4.67 were significantly associated with the HSU among all study participants.
Conclusion: This study shows that the level of the HSU is low. Educational status, family size, economic status, and payment mechanism were significantly associated with the HSU. Therefore, improving the community’s educational level, promoting family planning, devising income-generating strategies, and strengthening the fee waiver mechanism may enhance the HSU.
Keywords: out-of-pocket payment, fee-waiver, health service utilization, Northern Ethiopia
Background
About a third of the world population lacks access to essential medicines. Above half of them live in the poorest parts of Asia and Africa, and millions of them are dying of easily preventable and curable diseases every year.1 Nearly 1.3 billion people face challenges in financing their health services.2,3 More than 75% of sub-Saharan African (SSA) countries exercise inadequate tax revenue funding for their healthcare. The healthcare services of these countries depend on direct out-of-pocket (OOP) payment expenditure exceeding 25%, which failed to meet the Abuja agreement among the African Head of States (AHS) to allocate 15% of their total spending for the health sector by 2001.4 This is complicated by the geographic and financial inaccessibility of medicines and medical equipment. Also, inadequate medical equipment provision ultimately made people refrain from utilizing health services even when of their sickness and deadly diseases.5
Due to the weak health systems, poverty, and lack of health insurance schemes, the problem of healthcare financing is much higher for people living in low- and middle-income countries (LMIC).2,3 In LMIC countries, the primary source of funding for the HSU is through the OOP payment system. This leads to poor HSU even among people who are seriously ill. The unaffordable OOP payment, which results from the rising costs of health care, has jeopardized health outcomes and escalated poverty.1,6–8
In most SSA countries, user fees for health services had created fiscal difficulties in the 1980s and early 1990s. It was one of the several barriers limiting access to healthcare services.3,9,10 A study on user fees and health insurance from 89 countries indicated that financial disasters and poverty accompanied up to 40% of the OOP expenditure. The OOP risks poor households to go below the poverty line by causing economic impoverishment.11–15
Due to the high OOP expenditure, 100 million people are forced to face poverty every year at the HSU expense. Countries like Malawi and Zambia tried to address such challenges by waiving OOP for the poor suffering from common causes of morbidity and mortality.16 A fee waiver is a mechanism that helps the poor people cope with unaffordable OOP expenditure for HSU. It increases equity in access and financing of health services.17 However, in many LMIC, the fee waiver system suffers from implementation challenges such as unclear policy, insufficient funding, and challenges related to identifying the poor eligible for a fee waiver.18
Poor health care financing system is one of the significant challenges for HSU in Ethiopia. The per capita national health expenditure was only 20.77 US dollars compared to the other Sub-Saharan average, 93.65 US dollars in 2011. This made poor people face financial barriers for health service.19 Ethiopia has implemented free of charge health services for the poorest people. However, the system is susceptible to about 35.8% partiality and 44.5% inappropriate treatment, stigma, and discrimination against the fee waiver users by health professionals.20,21 About 36% and 14.7% are susceptible to possible under-coverage and leakage, respectively. Attaining the goals of health service equity in Ethiopia has not progressed well.22 Even though Ethiopia provides free health services to those unable to pay, the system opens a door for corruption and misuse of the service by urban dwellers and economically advantageous individuals who are not eligible. It lowers revenues unnecessarily. Besides, inhabitants of the rural areas who might not even be aware of such a system’s existence are not benefiting, which adversely affects equity.20
The unaffordable OOP expenditure for the HSU in Ethiopia is forcing people to poverty. It is unclear whether the HSU level in Ethiopia differs between the OOP and the fee-waiver users. Therefore, this study aimed to compare the HSU level and identify factors associated with the HSU among OOP payers and fee waiver users and all study participants.
Methods
Study Design and Setting
A community-based cross-sectional study design was conducted in Saesie Tsaeda-Emba district from March to April 2016. The study area, Saesie Tsaeda-Emba district, is located in the Eastern zone of Tigray regional state, 83 km away from the regional state capital, Mekelle, in Northern Ethiopia. Administratively the district is divided into 28 Kebeles (lowest administrative units in the country), and its estimated population size is 155,957. The district has eight public health facilities and 30 public health posts. The district has 302 low- and mid-level health professionals.
Study Population and Sampling Procedures
The study population was household heads aged 18 years and above who lived in selected households of Saesie-Tsaeda Emba district for at least six months. Sampling frame to select participants were prepared by screening the households in the district who have a history of illness in the household in the previous six months.
The sample size was determined using a double population proportion formula. A previous study reported 38.7% of the prevalence of HSU.23 As we could not find any study, we assume the HSU’s prevalence among fee-waiver users is 50%. Assuming a 95% confidence interval (CI), a 5% degree of precision, and a 10% non-response rate, the sample size was calculated using 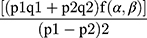 ;24 where n = required sample size, α = type I error (level of significance), β= Type two error (1- β = power of the study), p2=50% for the fee waiver, and F (α, β) = 7.9 from function table for a two-sided test. Therefore, the initial sample size was: n= [(0.387 *0.613+ 0.5*0.5) (7.9)]/(0.387-0.5)2* = 301.4429 = 302. By considering the design effect of 2 and 10% non-response rate, the final sample size was 665.
;24 where n = required sample size, α = type I error (level of significance), β= Type two error (1- β = power of the study), p2=50% for the fee waiver, and F (α, β) = 7.9 from function table for a two-sided test. Therefore, the initial sample size was: n= [(0.387 *0.613+ 0.5*0.5) (7.9)]/(0.387-0.5)2* = 301.4429 = 302. By considering the design effect of 2 and 10% non-response rate, the final sample size was 665.
The sample size was then proportionally allocated to each Kebele (the smallest administrative unit in Ethiopia). Eventually, 167 (25%) fee- waiver health service users and 498 (75%) OPP payers were included in the study. The ratio of 25% and 75% of the respondents were determined using the study area total waiver utilizers at K=24.
A two-stage sampling technique was employed to select the respondents of the study. First, from the total 28 Kebeles, ten of them were selected randomly using the lottery method. Then, from the ten Kebeles, households were systematically selected. The 1st household was selected by a random sampling method. Then at k=24, every 24th of the household was selected.
Data Collection
A structured, pre-tested, and interviewer-administered questionnaire was used to collect the data. The questionnaire was initially prepared in English and translated into Tigrigna (local language) and again translated back to English by language experts to check for any inconsistencies or distortions in the meaning of words and concepts. Face-to-face interviews were conducted to collect data about the HSU and associated factors among OPP payers and fee-waiver users. For administering the interview, six data collectors (diploma level nurses) and one supervisor (BSc level nurse) were recruited and trained.
Before starting the actual survey, the questionnaire was pre-tested on 5% of the total sample size outside the study area. Throughout the data collection, continuous supervision was conducted to ensure the quality of the data. A regular meeting was held between the data collectors and the principal investigator to address issues arising from interviews. Two more additional visits were made for respondents who were not found on the first visit. The collected data were reviewed and checked for completeness before entry into Epi Info.
Operational Definitions
Health Service Utilization
The use of available health care services in a health facility seeking medical treatment either through OOP payment or a fee waiver. This was measured by asking a “yes” or “no” question.
Fee-Waiver
A payment mechanism temporarily granted to people who cannot pay for health care services and are granted free HSU. This grant is given for those households who governors decide.
Out-of-Pocket Payment
A payments paid by the patient to the health provider at the time-of-service delivery.
Data Analysis
Data were checked, coded, and entered into Epi-info version 7 and then exported to SPSS version 20 for analysis. Data were split into fee-waiver and OOP payers using SPSS version 20 data splitter. Data were described using descriptive summary measures such as mean, median, and frequency statistics.
Bivariate logistic regression analysis was conducted to identify factors independently associated with the outcome variable at a p-value of 0.2. To control the effect of confounding, the multivariable logistic regression model was used. Factors associated with the HSU in the bivariable analysis at a p-value of < 0.2 were fitted into the overall model. Hence, three logistic regression models were constructed. Statistical significance was determined using the odds ratio with 95% CI. Variables having a p-value of less than 0.05 at the multivariable logistic regression model were considered independently associated with the outcome variable. Model goodness-of-fit was checked using the Hosmer-Lemeshow test, and Multicollinearity was checked by Durbin-Watson, tolerance, and Variance Inflation Factor.
Results
Sociodemographic Characteristics of the Respondents
A total of 652 (163 fees- waiver and 489 for OOP payers) individual participated in the study, making 98.2% response rate for OOP payers and 97.6% for fee-waiver users. The median and IQR age of the respondents was 41 (18) years. The median and IQR family size of respondents were 4.5 (3). Most (87%) participants were Christians, and 83.3% were married (Table 1).
 |
Table 1 Socio-Demographic Characteristics of Study Participants in Saesie Tsaeda-Emba District, Tigray Region, Northern Ethiopia, 2016 |
Health Service Utilization of Study Participants
The study showed that among the HSU was 41.9% (205/489) OPP payers, 51.5% (84/163) fee-waiver users, and 44.3% (289/652) among all study participants. The study also revealed that the main reasons for not using modern health services were financial inaccessibility (41.9% for OOP users and 32.8% for all study participants). Besides, acceptability of traditional medicine or home care preference (39.4% for OOP payers, 73.1% for fee-waiver users, and 46.8% for all study participants) (Table 2).
 |
Table 2 Health Service Utilization Among Study Participants in Saesie Tsaeda-Emba District, Tigray Region, Northern Ethiopia, 2016 |
Factors Associated with Health Service Utilization
The study indicated that marital status, educational status, family size, and income level were significantly associated with the HSU among OOP payers. However, no variable was found to be significantly associated with the HSU among fee-waiver users.
OOP Payers who could not read and write and who had a family size of five or above were 35% (AOR = 0.65; 95% CI: 0.21, 0.59), and 40% (AOR = 0.4; 95% CI: 0.37, 0.97) less likely to use health services compared to OOP payers who could read and write, and who had a family size of below five, respectively. Besides, OOP payers who were from middle- and high-income households were 2.09 (AOR = 2.09; 95% CI: 1.12, 3.90) and 4.12 (AOR = 4.12; 95% CI: 2.41, 7.3) times more likely to use health services compared to OOP payers who were from low-income households, respectively (Table 3).
 |
Table 3 Factors Associated with Health Service Utilization Among OPP Payers and Fee-Waiver Users in Saesie Tsaeda-Emba District, Tigray Region, Northern Ethiopia, 2016 (N=652) |
The study also indicated that educational status, family size, income level, and payment mechanisms to get health service had statistically significant associations with the HSU.
Study participants who could not read and write and who had a family size of five or above were 44% (AOR = 0.56; 95% CI: 0.33, 0.75), and 32% (AOR = 0.68; 95% CI: 0.43, 0.92) less likely to use health services compared to study participants who could read and write, and who had a family size of below five, respectively. Besides, study participants who were from high-income households were 2.6 (AOR = 1.12; 95% CI: 1.21, 4.87) times more likely to use health services compared to study participants who were from low-income households, respectively. Finally, study participants who were fee-waiver users were 2.21 times (AOR = 2.21; 95% CI: 1.34, 4.47) more likely to use health services compared to study participants who were OPP payers (Table 4)
 |
Table 4 Factors Associated with Health Service Utilization Among Study Participants in Saesie Tsaeda-Emba District, Tigray Region, Northern Ethiopia, 2016 (N=652) |
Discussion
The finding of this study showed that the level of the HSU was higher for fee-waiver users compared to the OOP payers in the study area. This indicates that the OPP payers are price-sensitive to utilize health service. A related study from South Africa and Kenya reported that, following the elimination of user fees in South Africa and Kenya for curative services, the HSU was raised by 77% and 41%, respectively.10 The higher the HSU attained among the fee-waiver users could be temporarily free of charge health service privilege. A study from Kenya reported that removing user fees has increased the HSU by 41%.25
In this study, the HSU level among the OOP payers was 44.33% (CI; 40.5, 48.3). This is consistent with another study conducted in Ethiopia. Two studies in the Amhara and Oromia regions of Ethiopia reported 39%23 and 45.6%26 of the HSU, respectively. However, it is relatively higher than a study from Nigeria (31.2%).5 The level of the HSU through fee waiver was 51.5% in the current study. The recent study’s HSU is also relatively higher than the study reported from Bahir Dar, Northwest Ethiopia (30%).21 However, this finding is consistent with the research conducted in the Jimma zone, Southwest Ethiopia (45.6%).26
One would expect that the HSU among fee waiver beneficiaries to be high. However, only half (51.5%) of the fee-waiver beneficiaries utilize health service. This might be, as a study conducted in the Amhara region revealed, the system is susceptible to about 35.8% partiality and 44.5% unsafe treatment of patients in health institutions, which ultimately dissatisfies fee-waiver users and to refrain from utilizing health service. Fee-waiver beneficiaries feel that they face partiality, stigma, discrimination, and unsafe treatment.23 Similarly, a study conducted in Nigeria revealed that only 20.2% of the respondents are satisfied with prescribed drugs within the health service facilities.27
The finding of this study showed that those study participants who had a family size of below five utilized health services more than those who had a family size of five and above. This result is consistent with a study from Nigeria. In the Nigerian study, 75% of households with more than 14 family members do not utilize health service facilities.27 This might be households’ heads with large family size becoming more workloads to manage and satisfy the family members’ needs. Besides, financial constraints might also be the reason for less using health services.28
This study also showed that those participants who could at least read and write had better HSU. This is expected because education can increase individuals’ elasticity behaviour to utilize health service.29 Generally, education remains continuously strong and has a positive effect on the HSU. People who have low educational status have little attention to the HSU. The finding of this study is consistent with research conducted in India.30 The more educated the head of the household is, the more likely to utilize health service.23
Study participants whose income level was at medium and high had better HSU than those whose income level was low. This finding is consistent with studies done in Nigeria and the Amhara Region of Ethiopia.5,26 This might be the cost burden of the health services from different perspectives (direct and indirect costs), affecting their health-seeking behaviour.
In this study, demographic factors such as age, sex, religion, marital status, and occupation were not associated with the HSU for both study participants. Contrary to this finding, males are reported to utilize health service more likely than females in Kenya’s study. The relationship between age and morbidity is also said to have a U-shaped relationship that could force older and younger age groups more likely to seek health service.31 We suggest a bigger population-based comparative study to investigate the influence of demographic, socioeconomic, and disease-related characteristics of OOP or fee-waiver users on the HSU.
Limitation of the Study
This study was conducted only in one district, which might not give a full picture of its HSU region. There might also be a response bias in which study participants might not remember HSU’s issues. The other limitation of the study was that we could not measure the study participants’ actual monthly income, which might overestimate or underestimate their actual income, leading to misclassification of income level.
Conclusion
This study shows that the level of the HSU is low. Educational status, family size, economic status, and payment mechanism are significantly associated with the HSU. Therefore, improving the community’s educational level, promoting family planning, devising income-generating strategies, and strengthening the fee waiver mechanism may enhance the HSU.
Abbreviations
AOR, adjusted odds ratio; CI, confidence interval; OOP, out-of-pocket; CBHI, community-based health insurance; HSU, health service utilization; LMIC, low- and middle-income countries; SHI, social health insurance; SPSS, Statistical Package for Social Sciences; SSA, Sub-Saharan Africa.
Data Sharing Statement
The datasets supporting the conclusions of this article are available upon request to the corresponding author. Due to data protection restrictions and participant confidentiality, we do not make participants’ data publicly available.
Ethics Approval and Consent to Participate
This study was conducted in accordance with the Declaration of Helsinki. Ethical clearance was obtained from the Ethical Review Committee of Institute of Public Health, College of Medicine and Health Sciences, University of Gondar. Written informed consent was taken from each participant. Moreover, verbal informed consent was obtained from those participants who could not read and write, approved by the ethical committee. Each eligible participant was informed about the purpose of the study. Participants were also assured that their name was not written on the data’s questionnaire and confidentiality kept at all levels.
Acknowledgments
We deeply express our gratefulness to the University of Gondar to approve the ethical issue and its technical and financial support. We would like to thank the study participants, data collectors, and supervisors for their study participation.
Author Contributions
All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; agreed to submit to the current Journal; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
Disclosure
The authors declare that they have no competing interests in this work.
References
1. Telles R. Drug Subsidy Programs in the Developing World: The Impact of the “Farmácia Popular” Program on Health Outcomes in Brazil. Georgetown University; 2009.
2. Lekashingo LD. Exploring the Effects of User Fees, Quality of Care and Utilization of Health Services on Enrolment in Community Health Fund, Bagamoyo District. Tanzania: Muhimbili University of Health and Allied Sciences; 2012.
3. Roy B, Gupta S. Public-private partnership and user fees in healthcare: evidence from West Bengal. Econ Polit Wkly. 2011;46(38):74–78.
4. McIntyre D, Gilson L, Mutyambizi V. Promoting equitable health care financing in the African context: current challenges and future prospects; 2005.
5. Chukwudi ON, Uyilewhoma IM, Chukwudi OE, et al. Determinants of health services utilization among the elderly in Calabar Municipality, Cross River State, Nigeria. Eur J Preventive Med. 2015;3(5):129–136.
6. Acharya A, Vellakkal S, Kalita S, et al. Do social health insurance schemes in developing country settings improve health outcomes and reduce the impoverishing effect of healthcare payments for the poorest people. Systematic Rev. 2011.
7. Gebremeskel T. The impact of community based health insurance in health service Utilization in Tigray: A Case of kilte Awlaelo woreda (Doctoral dissertation, Mekelle University).
8. Muyanga, Joel Mwinzi. Removal of User Fees in Public Health Facilities in Kenya: the Inequality Effect on Health Care Utilisation between the Poor and the Non-Poor. [Internet]. Population Poverty and Social Development (PPSD). 2011. Available from: http://hdl.handle.net/2105/10812.
9. Mubyazi G, Massaga J, Kamugisha M, et al. User charges in public health facilities in Tanzania: effect on revenues, quality of services and people’s health-seeking behaviour for malaria illnesses in Korogwe district. Health Services Management Res. 2006;19(1):23–35. doi:10.1258/095148406775322061
10. Kapinga FC. Assessing performance of exemption scheme: a case study of the Ocean Road Cancer Institute; 2012.
11. Alkenbrack SE. Health insurance in Lao PDR: examining enrolment, impacts, and the prospects for expansion; 2011.
12. Hardeman W, Van Damme W, Van Pelt M, Por I, Kimvan H, Meessen B. Access to health care for all? User fees plus a health equity fund in Sotnikum, Cambodia. Health Policy Plan. 2004;19(1):22–32. doi:10.1093/heapol/czh003
13. Honda A. User Fees Policy and Equitable Access to Health Care Services in Low-And Middle-Income Countries-With the Case of Madagascar. Tokyo: Institute for International Cooperation, Japan International Cooperation Agency; 2006.
14. Mebratie A.D. Essays on evaluating a community based health insurance scheme in rural Ethiopia [Internet]. ISS PhD Theses. International Institute of Social Studies of Erasmus University (ISS); 2015. Available from: http://hdl.handle.net/1765/78363.
15. Xu K, Saksena P, Jowett M, Indikadahena C, Kutzin J, Evans DB. Exploring the thresholds of health expenditure for protection against financial risk. World Health Rep. 2010:19.
16. Habiyonizeye Y. Implementing community-based health insurance schemes: lessons from the case of Rwanda (Master's thesis, Høgskolen i Oslo og Akershus. Fakultet for samfunnsfag).
17. Bitrán R, Giedion U. Waivers and exemptions for health services in developing countries. Final draft. World Bank. 2002;89.
18. Munishi V. Assessment of user fee system: implementation of exemption and waiver mechanisms in Tanzania: successes and challenges (Master's thesis, University of Cape Town).
19. Technology Transfer and Research Translation Directorate atEPHI. Policy dialogue: improving health care financing in Ethiopia; 2014.
20. Ashagrie G, Abebe Y. Free health care provision and its financial implications in Gondar town, northwest Ethiopia. Ethiopian J Health Develop. 2017;18:2.
21. Engida E, Mariam DH. Assessment of the free health care provision system in Bahir Dar area, northern Ethiopia. Ethiopian J Health Develop. 2002;16(2):173–182. doi:10.4314/ejhd.v16i2.9808
22. Woldie M, Jirra C, Tegegn A. An assessment of the free health care provision system in Jimma town, southwest Ethiopia. Ethiopian J Health Develop. 2005;19(3):188–194.
23. Mesganaw F, Degu G. Health service utilization in Amhara Region of Ethiopia. EthiopJHealth Dev. 2003;17(2):141–147.
24. Fleiss JL, Levin B, Paik MC. Statistical Methods for Rates and Proportions. John Wiley & Sons; 2013.
25. Amarech G. Challenges of healthcare financing: economic and welfare effects of user fees in urban Ethiopia. 2007.
26. Girma F, Jira C, Girma B. Health services utilization and associated factors in jimma zone, South west ethiopia. Ethiop J Health Sci. 2011;21:3.
27. Awoyemi T, Obayelu O, Opaluwa H. Effect of distance on utilization of health care services in rural Kogi State, Nigeria. J Human Ecol. 2011;35(1):1–9. doi:10.1080/09709274.2011.11906385
28. Kassile T, Lokina R, Mujinja P, Mmbando BP. Determinants of delay in care seeking among children under five with fever in Dodoma region, central Tanzania: a cross-sectional study. Malar J. 2014;13(1):348. doi:10.1186/1475-2875-13-348
29. Regassa T, Agero G. Factors affecting prenatal care utilization in East Wollega Zone, Oromia Regional State, Ethiopia. Sci Technol Arts Res J. 2014;3(2):148–154. doi:10.4314/star.v3i2.19
30. Govindasamy P, Ramesh B. Maternal education and the utilization of maternal and child health services in India; 1997.
31. Kimani DN. Out-of-Pocket Health Expenditures and Household Poverty: Evidence from Kenya. University of Nairobi; 2014.
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
