Back to Journals » Journal of Multidisciplinary Healthcare » Volume 14
Health Science Students’ Perspective on Quality-of-Care-Relating Medical Professionalism
Authors Binh PDU , An PL , Nguyen NA, Nguyen DV, Huynh G , Gomi H, Yoshida M
Received 24 May 2021
Accepted for publication 28 July 2021
Published 18 August 2021 Volume 2021:14 Pages 2229—2238
DOI https://doi.org/10.2147/JMDH.S321094
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Pham Duong Uyen Binh,1,2 Pham Le An,3 Nghia An Nguyen,3 Dan Van Nguyen,4 Giao Huynh,5 Harumi Gomi,2 Motofumi Yoshida2
1Department of Educational Quality Assurance, University of Medicine and Pharmacy at Ho Chi Minh City, Ho Chi Minh City, Vietnam; 2Department of Social Medical Sciences, Graduate School of Medicine, International University of Health and Welfare, Tokyo, Japan; 3Faculty of Medicine, University of Medicine and Pharmacy at Ho Chi Minh City, Ho Chi Minh City, Vietnam; 4Faculty of Traditional Medicine, University of Medicine and Pharmacy at Ho Chi Minh City, Ho Chi Minh City, Vietnam; 5Faculty of Public Health, University of Medicine and Pharmacy at Ho Chi Minh City, Ho Chi Minh City, Vietnam
Correspondence: Pham Duong Uyen Binh
Department of Social Medical sciences, Graduate School of Medicine, International University of Health and Welfare, Tokyo, Japan
Tel +84 961156505
Email [email protected]
Purpose: Health science students need to be professional to improve quality of care (QOC) in the current Vietnamese healthcare system. Therefore, we aim to evaluate medicine and traditional medicine (TM) students’ perception of the professional attributes relating to QOC for improving inter-disciplined professionalism training that promotes QOC in Vietnam.
Methods: The cross-sectional study was carried on 2039 students of 6 years at the University of Medicine and Pharmacy at Ho Chi Minh City (HUMP) from the medical and TM faculty in March, 2021. The Vietnamese American Board of Internal Medicine (ABIM) questionnaire (2011) was used as the survey instrument. The confirmatory factor analysis (CFA) was performed to confirm the validity of the scale in TM students. Mean, Min–Max, standard deviation and sample paired t-test were performed for Likert scale. The one-way ANOVA was used for inferential statistics.
Results: The CFA demonstrated the validity of the Vietnamese questionnaire in measuring 4 QOC-relating professional attributes, previously found in medical students for TM students. In both faculties and across academic years, students perceived self-awareness and ensuring QOC as the leading important attribute, while social duty and professional habit as the least important attribute. Contrasting with preclinical phase, students’ perception did not differ significantly between the two faculties in their clinical years (p > 0.05).
Conclusion: TM students share universal QOC-relating professional traits with medical students. Moreover, exposure to clinical environment might increase inter-disciplined agreement on importance of these attributes. However, health sciences students’ underestimation of social duty and professional habit persists throughout 6 academic years. Hidden curriculum in clinical training such as specialist-centeredness might hinder the students’ improvement in perception of these traits. Therefore, these traits should strongly be emphasized in professionalism training to decrease the effects of hidden curriculum on them.
Keywords: medical professionalism, quality of care, inter-disciplined professionalism
Corrigendum for this paper has been published.
Introduction
Quality of Care (QOC) is the ultimate goal in numerous healthcare settings. According to the Institute of Medicine in the US, QOC refers to health services that help individuals achieve the desired health outcomes and align with professional knowledge.1 The World Health Organization (WHO) added healthcare quality indicators comprising safety, effectiveness, timeliness, efficiency, equity and people-centeredness.2
An obvious link between medical professionalism and QOC was noted as QOC starts with the interaction with the patients.3 Professionalism encompasses behaviors and attributes to build and maintain relationships– with patients and colleagues–all are to ensure a safe and satisfactory patient care.3–5 The American Board of Internal Medicine Foundation Physician Charter elaborated on professional physicians’ attributes such as self-awareness, ensuring QOC or social duty, etc.6
In Vietnam, professionalism and QOC become inseparable in the current health care. After the success of the first level of quality through prevention, vaccination and nutrition, the Vietnamese health status has improved.7,8 To address the emerging issues of regional disparities, chronic diseases and ageing population, the national government has moved to the second level of quality which aims at managing limited resources and reforming health financing.9–11 This has been a gradual shift from physician-based to system-based notions of quality in Vietnam.9 Patients at the system level demand more than safe care as they continue to seek compassion, information, and reassurance from their physicians.4 To fulfill these demands, efforts to establish QOC should be coupled with a recommitment to the core values of medical professionalism for multi-disciplined health workers.4 Given that medical and Traditional Medicine (TM) doctors are health professionals that directly treat the patients in the Vietnamese healthcare system, their commitment to professionalism becomes more essential in our context of QOC. This leads to the requirement of developing the professional attributes that promote QOC for both medical and TM students as soon as possible.
There are professional attributes that reflect behavioral tendency to maintain QOC. Typical QOC aspects comprise safety and error reduction, as well as multidisciplinary working and evidence-based practice in medicine.12–14 Studies in Taiwan, Japan, Sri Lanka and The Middle East (Arabia) identified several professional traits in medical students.15–17 A study in 2011 found six attributes in Vietnamese medical students, four of which closely relate to QOC (Figure 1).18 They are Self-Awareness, Professional Habits, Quality of Care and Social responsibility.18
 |
Figure 1 Ranking of professional attributes against the important level perceived by the students of Medicine and Traditional medicine and their relation to Quality of Care (QOC). |
Self-Awareness comprises Awareness of Limitation and Prudence reflects the tendency to assure patient safety and avoid errors in practice.19 Professional Habit refers to professional collaboration in QOC. Quality of Care reflects the commitment to life-long learning or up-to-date evidence-based medicine. Finally, Social duty implies that the healthcare workers with higher social responsibility find themselves more in contact with the surrounding “environment and human factors”.20 Social responsibility is perceived as an aspect of health service quality in local health institutes. Developing this trait might improve public image of health institutes and attract the patients to local health services.21
However, it is unknown which of these QOC-relating professional attributes will require more attention in TM students as opposed to medical students. Specifically, students’ perception on medical professionalism somewhat reveals the evidences of any underdeveloped professional attributes for medical educators whom are responsible for the future curriculum.22 Previous studies in Asia presented medical students’ perception on numerous professional attributes; however, none has emphasized those QOC-relating attributes in inter-disciplined setting.15–18,23 Moreover, in similar data of students’ perception in other Health sciences including TM faculty, there appears to be a lack of knowledge in Asia.
Therefore, this study aims to evaluate students’ perception on QOC-relating professionalism between Medical and TM students in a Southeast Asian context.
Materials and Methods
Design and Context
The cross-sectional study was conducted in the second term of their academic year, between March and April, 2020. Approximately 2500 students from 1st to 6th-year studying Medicine and TM voluntarily participated in this study. An electronic form of the questionnaire was sent to all participants via emails at the beginning of March, 2020. The participants were encouraged to fill in the questionnaire within one week. Reminders were sent twice in the middle of March and at the beginning of April, 2020. Finally, the response rate was 86.5%, resulting in 2039 completed questionnaires.
University of Medicine and Pharmacy, Ho Chi Minh City has provided the man power for the health system in Vietnam since 1975, including Medical and TM healthcare providers. Medical doctors practicing Medicine by chiefly using Western-based medicine model while TM doctors chiefly use integrated models of Oriental and Western medicine for patient care. Medicine and TM 6-year programs share the same basic science subjects in the preclinical phase and are separated for the clinical clerkship. TM students, unlike medical students, apply not only Western medicine but also Oriental medicine and in patient care in 6 years training of Ho Chi Minh University of Medicine and Pharmacy (HUMP). The longitudinal module of medical professionalism has been integrated into the curriculum from the 2nd year to 6th year, as of 2017. By the time of the study, most students had been initially exposed to a few elements of professionalism comprising Integrity, Compassion or Social Duty. Moreover, QOC training for medical undergraduates is limited to some lectures in public health and a 6-week community-based visit program in the 6th year.
Materials
Quantitative data was collected using validated Vietnamese questionnaire of medical professionalism (VMPQ) based on the framework of American Board of Internal Medicine (Appendix 1).33
Vietnamese American Board of Internal Medicine Questionnaire on Perception of Medical Professionalism
The questionnaire aimed at evaluating perception of professionalism. It asked people to express their agreeableness to the importance of various professional behaviors on a 1–5 Likert scale. It was initially developed and validated at the Taipei Medical University College of Medicine, Taiwan, by the author Tsai et al, 2007 based on the framework of professionalism by ABIM. The underlying logic is that people who score high on this scale will possess more accurate belief of what effective actions are required for satisfactory patient care.24,25
The VMPQ validated in 2014 found 23 of 32 original items that measured 6 professional attributes, 4 of which closely relate to QOC comprising Self-Awareness, Professional Habit, Social Duty with internal reliability of 0.90.
Data Analysis
Statistical analysis was performed using SPSS Statistics (SPSS Statistics Inc., Chicago, US) version 20.0. Confirmatory Factor Analysis (CFA) was performed to determine if the questionnaire is valid to measure 4 QOC-relating attributes mentioned above in TM students.
Descriptive analyses were performed to compute minimum, maximum, mean, and standard deviations for the scores in these 4 professional attributes from questionnaire responses. The sample paired t-test was used for categorical data and to compare differences between two health faculties. The one-way ANOVA Post hoc test was used for comparing differences across 6 academic years.
Ethics Approval
Our research complied with the 1964 Declaration of Helsinki. All the participants in the study signed a consent form before answering the questionnaires. They could withdraw from the study whenever they desire without any penalties for their exam scores or academic rankings. The study was approved by the Ethics Committee, University of Medicine and Pharmacy at Ho Chi Minh City, Vietnam (protocol number 197/UMP-ETHICBOARD).
Results
The mean age of students was 23.9 years. The ratio between male and female students was 59.5% and 50.5% (Table 1). The ratio between male and female in Medicine was 49.5 and 50.5, whereas the ratio in TM was 29.4% and 70.6%.
 |
Table 1 Age, Grade Point Average, Gender and Faculties of Education |
Confirmatory Factor Analysis (CFA)
The CFA results confirmed the construct validity of the questionnaire to evaluate professional attributes including 4 QOC-relating attributes in TM students.
Figure 2 presents the standardized solution for the six-factor measurement model, that observed variables which were described by rectangles, and latent variables which were enclosed in eclipses, 6-items served as indices of Social Duty, 4-items of Professional Habit, 4-items of Quality of Care, 2-items of Self-Awareness and 7 remaining items belonging to 2 other attributes. The CFA revealed a model of the strong correlation of each factor with another with standardized covariances ranging from 0.9 to 0.99. Factor loadings of the 23 items were good (ranging from 0.63 to 0.9). These results indicated an acceptable to good ability to explain factors relating to the variation of items in the model (Figure 2).
Fit statistic for the CFA model showed an unfit 6-factor model using LR test (Likelihood Ratio test) for model or baseline versus saturated comparison, corresponding to χ2(215) = 1061.3, p < 0.001, χ2(253) = 13803, p < 0.001, which indicated the expected model and the observed model were significantly different. This can be explained by the large sample size, which can affect these statistics leading to rejects in the model. However, all other fit statistics indicated a good fit of the model specified such as CFI (0.938), TLI (0.927), SRMR (0.034), CD (0.993), RMSEA (0.078, 90% CI = 0.074–0.083) (Table 2).
 |
Table 2 Goodness-of-Fit Summary of Traditional Medicine Students’ Perception Based on Maximum Likelihood (ML), Robust Estimation |
Students’ Perception on Professional Attributes Relating to QOC
Table 3 presents an overview of students’ perception on the role of 4 QOC-relating professional attributes. Self-Awareness was perceived the most important in 4 professional attributes (M=4.44, SD=0.66), while Social Duty was rated as the least important for health workers (M=4.21, SD=0.62). Professional Habit and Quality of Care were relatively important professional values in healthcare delivery (M=4.34, SD=0.62; M=4.28, SD=0.56).
 |
Table 3 Mean Scores of Each Items Under 4 QOC-Relating Professional Attributes in Vietnamese Medical Professionalism Questionnaire |
Differences in Students’ Perception of Professional Attributes Relating to QOC Between the Two Faculties
Table 4 describes the mean scores of how important students rated various professional attributes according to the academic years and faculties as well as differences in mean scores between medical and TM students. Overall, most students of both faculties in each year agreed that these professional attributes are important for healthcare workers (M >4, SD <0.8).
 |
Table 4 Mean Scores of Professional Attributes Across Academic Years and Between Two Faculties |
In both faculties, the trait Self-Awareness was reported as the most important attribute, the next being Quality of Care and Professional Habit in each year. Social Duty received the lowest mean scores, which made it the least important trait in both faculties almost at all years. First year TM students demonstrated an exceptional viewpoint in which the least important attribute was Practice habit (M=0.35, SD=0.62).
Students’ perception in most attributes did not differ significantly between the two faculties in their clinical years (4th - 6th year). However, significant differences were found in the pre-clinical phase. 1st year medical students rated Professional Habit in health care higher than TM students (t(414) = 3.78; p < 0.001). 2nd year medical students significantly assigned higher scores for Self-Awareness and Social Duty over 2nd year TM students (t(356) = −3.12, p=0.002; t(356) = −3.53, p < 0.001). However, 3rd year medical students rated Self-Awareness as less desirable for healthcare workers against TM students of the same year (t(200) = 2.45, p=0.015).
Differences in Students’ Perception of Professional Attributes Across the Academic Years
There was a significant effect of academic years on perception of QOC-relating professional traits [F(5, 5) = 10.94, p < 0.000]. Post hoc comparisons using Tukey HSD test indicated as follows.
Within the medical students’ group, we only noted a significant increasing trend in mean scores of Self-awareness from 4th to 6th year (M=4.38; M=4.45; M=4.57) with the significant differences in mean scores of 6th year group versus the 4th and 5th year (p < 0.05) (Table 5). However, no trend was detected among 4 QOC-relating attributes during pre-clinical years.
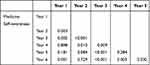 |
Table 5 Differences in Medical Students’ Perception on Self-Awareness Across Academic Years |
Within the TM group, mean scores of these professional attributes vary across academic years; therefore, no clear trend was found in both pre and clinical years.
The orders of the 4 QOC-relating attributes according to their importance to students in both groups remained unchanged from the 1st to 6th year, in which Self-Awareness presented with the highest mean scores and Professional Habit and Social Duty with lower mean scores (Table 4).
Discussion
First, this study continues to confirm that the VMPQ is valid in to measure QOC-relating professional traits in TM students. The QOC-relating traits were relatively similar with those found in Medical participants and with the ABIM definitions in the previous study of the author Nhan et al 2011. That means the VMPQ is a valid tool for measuring medical professionalism across health disciplines in Vietnam. Although medical professionalism is a somewhat contextually sensitive concept, health science students in different faculties still share universal professional traits to promote QOC.
This is the first study in Vietnam to reveal both Medical and TM students’ perceptions on QOC-relating to professional attributes. No differences were found between the faculties in the order of these 4 attributes, being from the most to the least important, which was Self-Awareness, Ensuring QOC, Professional Habit and Social Duty (Figure 1). However, between the two less important attributes, Professional Habit replaced Social Duty as the least important by junior TM students. This might be explained by the fact that unlike medical students, TM students were not exposed to senior role models in their first year due to integrated Western and Traditional medicine. Therefore, TM juniors’ perception on Professional Habit has not yet fully formed.
Students of both faculties valued the trait Self-Awareness which is congruent with previous studies in Vietnam and The Middle East (Arabia).18,26 Students’ high appreciation of Self-Awareness might also result from the medical curriculum, that has been disease and treatment focused, to form a solid clinical competence that helps protect the patients from medical errors.
The underestimation of Social Duty is consistent with the previous study a decade ago.18 This can be explained by following facts. First, training medical students has not changed its focus over the past decade, which focused on in-patient skills in central hospitals. Most modelling clinical preceptors directly teaching students are based in hospitals, whereas, there are few role models to instruct students in the community.18 Moreover, the phrase “improving access to healthcare” still implied the rural people’s access to care in most national health programs. Thus, students might view that access to health care is not their duty, but the government’s responsibility.
Similar to medical students, except the 1st year cohort, TM students perceived Social Duty as the least important. This might relate to the current job positions in the Vietnamese Healthcare System which include three kinds of doctors such as medical doctors practicing Medicine by chiefly using Western-based medicine model; traditionally medical doctors chiefly use integrated models of Oriental and Western medicine for patient care; and public health doctors consider responses with consideration to social duty as opposed to the other physicians.
Besides this, a significant increase of medical students’ Self-awareness of limitation across clinical years reflects the consistent development of this trait under the influence of hospital role models and patient safety in the formal curriculum. Therefore, Self-awareness remains most important in the unchanged orders of importance of 4 QOC-relating professional attributes across 6 years in both faculties. Unfortunately, this formal curriculum, together with the later hidden curriculum (such as specialist-centered model) in clinical setting, might have reduced the effect of the current professionalism training.22 That means inconsistently improving Professional Habit including teamwork and Social Duty that caused both group students’ perception to be continuously reported as less important.
In TM across academic years, a trend of all 4 QOC-relating attributes is undetermined. This might indicate the TM students’ confusion about professionalism due to the lack of professional role models. The role modeling in TM has not been fully conceived due to the newly developed integrated model of Western and Traditional Medicines. Therefore, it is not yet clear how much of the Western and Traditional practices play a role in patient care, and which one is the best role model. In order to confirm this, further research should be implemented.
TM and medical students in their clinical years demonstrated more agreement on the importance of professionalism than in the pre-clinical years. This indicates the impact of role modeling and interaction with patients in the clinical environment on medical professionalism.23 This might also be due to frequent doctors–patients interaction or improved students’ self-regulation in clinical settings, which might influence the professional attributes such as Self-Awareness or ensuring QOC.27,28 Based on this finding, the authentic teaching approaches of professionalism are suggested including case-based learning in the pre-clinical phase, which can be combined with role-model and real practice in the clinical phase.29
This study gives evidence to medical educators that 4 QOC-relating professional attributes should be included in future inter-disciplined professionalism training. This means that several attributes can be on the list of priorities for inter-disciplined professionalism training. Both faculties students highly appreciate Self-Awareness. However, overemphasis of this trait might lead to decreased students’ self-confidence. Minding too much about the awareness of one’s own limitations, physicians will hesitate when making clinical decisions to protect themselves from the humiliation of losing face.18 Therefore, this trait should be kept at the same training level before. Additional QOC topics should be introduced such as self-evaluation of one’s own capacity in certain contexts and medical safety.30,31
A concerning finding is that underestimation of Social Duty has been unimproved across health faculties and across academic years. Health sciences students need to understand that every medical professional has to be responsible for improving patients’ trust in and access to primary care.18 Patients’ hesitation to access to local health services leads to consequences such as overloading in central hospitals, exceeding the expenditures in many health systems and poor patient outcomes.9,32
Therefore, future professionalism training in Medicine and TM in Vietnam should emphasize social responsibility. Students can achieve this via voluntary activities which are both in community-based and hospital-based contexts.20 Guiding patients in the overloaded hospitals to shorten their waiting times and assisting people in Covid-19 pandemic within their capacity in multi-disciplined groups are feasible tasks.14 Last but not least, Professional Habit referring to collaboration should be emphasized for the junior TM students due to their extreme underestimation of this trait.
Conclusion
TM students share universal QOC-relating professional traits with medical students. Moreover, exposure to a clinical environment might increase the inter-disciplined agreement on importance of these traits. However, Health Sciences students’ underestimation of Social Duty and Professional Habit comprising professional collaboration persists throughout 6 academic years. Hidden curriculum in clinical training such as specialist-centeredness might hinder the students’ improvement in perception of these traits. Therefore, these traits should strongly be emphasized in professionalism training to decrease the effects of hidden curriculum on them.
Data Sharing Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Acknowledgments
The authors thank all the participants for their time and contribution to the study. The authors also acknowledge Truong Vien Nguyen, MPH for his contribution as the data analyst. We also thank Raymond A Kuschert for assisting in editing the manuscript.
Author Contributions
All authors contributed to data analysis, drafting or revising the article, gave final approval of the version to be published, agreed to the submitted journal, and agree to be accountable for all aspects of the work.
Funding
This research received no external funding.
Disclosure
The authors declare that they have no competing interests.
References
1. Chassin MR, Galvin RW. The urgent need to improve health care quality: Institute of Medicine National Roundtable on health care quality. JAMA. 1998;280(11):1000–1005. doi:10.1001/jama.280.11.1000
2. World Health Organization. Quality of Care: A Process for Making Strategic Choices in Health Systems. World Health Organization; 2006.
3. Cavers B. Quality of patient care and professionalism are intertwined. B C Med J. 2014;56(6):263.
4. Katz JN, Kessler CL, O’Connell A, Levine SA. Professionalism and evolving concepts of quality. J Gen Intern Med. 2007;22(1):137–139. doi:10.1007/s11606-006-0031-1
5. Popa D, Druguș D, Leașu F, Azoicăi D, Repanovici A, Rogozea LM. Patients’ perceptions of healthcare professionalism—a Romanian experience. BMC Health Serv Res. 2017;17(1):1–9. doi:10.1186/s12913-017-2412-z
6. Foundation A, Foundation -A-A. Medical professionalism in the new millennium: a physician charter. Obstet Gynecol. 2002;100(1):170–172.
7. Marino A, Lorenzoni L, Daniel F, Brownwood I. Health at a Glance: Asia/Pacific 2018. OECD/WHO; 2018.
8. Busse R, Panteli D, Quentin W. An introduction to healthcare quality: defining and explaining its role in health systems. Improv Healthc Qual Eur. 2019;1. doi:10.1186/s12199-017-0682-z
9. Takashima K, Wada K, Tra TT, Smith DR. A review of Vietnam’s healthcare reform through the Direction of Healthcare Activities (DOHA). Environ Health Prev Med. 2017;22(1):1–7. doi:10.1186/s12199-017-0682-z
10. Long GT. The ageing population in Vietnam: current status, prognosis, and possible policy responses. 2011.
11. Bui LN, Nguyen NT, Tran LK, Vos T, Norman R, Nguyen HT. Risk factors of burden of disease: a comparative assessment study for evidence-based health policy making in Vietnam. Lancet. 2013;381:S23. doi:10.1016/S0140-6736(13)61277-5
12. Encourage IID. Quality improvement training for healthcare professionals. 2012.
13. McGeorge E, Coughlan C, Fawcett M, Klaber RE. Quality improvement education for medical students: a near-peer pilot study. BMC Med Educ. 2020;20:1–7. doi:10.1186/s12909-020-02020-9
14. Worsley C, Webb S, Vaux E. Training healthcare professionals in quality improvement. Future Hosp J. 2016;3(3):207. doi:10.7861/futurehosp.3-3-207
15. Monrouxe LV, Chandratilake M, Gosselin K, Rees CE, Ho MJ. Taiwanese and Sri Lankan students’ dimensions and discourses of professionalism. Med Edu. 2017;51(7):718–731. doi:10.1111/medu.13291
16. Nishigori H, Harrison R, Busari J, Dornan T. Bushido and medical professionalism in Japan. Acad Med. 2014;89(4):560. doi:10.1097/ACM.0000000000000176
17. Tsai T-C, Lin C-H, Harasym PH, Violato C. Students’ perception on medical professionalism: the psychometric perspective. Med Teach. 2007;29(2–3):128–134. doi:10.1080/01421590701310889
18. Nhan VT, Violato C, Le An P, Beran TN. Cross-cultural construct validity study of professionalism of Vietnamese medical students. Teach Learn Med. 2014;26(1):72–80. doi:10.1080/10401334.2013.857333
19. Borrell-Carrió F, Epstein RM. Preventing errors in clinical practice: a call for self-awareness. Ann Fam Med. 2004;2(4):310–316. doi:10.1370/afm.80
20. Jazi ZH, Peyrovi H, Zareian A. Nurse’s social responsibility: a hybrid concept analysis in Iran. Med J Islam Repub Iran. 2019;33:44.
21. Lubis AN, Lumbanraja P, Lubis RR, Hasibuan BK. A study of service quality, corporate social responsibility, hospital image, and hospital value creation in Medan. 2017.
22. Martin J, Lloyd M, Singh S. Professional attitudes: can they be taught and assessed in medical education? Clin Med (Northfield Il). 2002;2(3):217. doi:10.7861/clinmedicine.2-3-217
23. Monrouxe LV, Rees CE, Hu W. Differences in medical students’ explicit discourses of professionalism: acting, representing, becoming. Med Edu. 2011;45(6):585–602. doi:10.1111/j.1365-2923.2010.03878.x
24. Ajzen I. Attitudes, Personality, and Behavior. UK: McGraw-Hill Education; 2005.
25. Jha V, Bekker HL, Duffy SR, Roberts TE. A systematic review of studies assessing and facilitating attitudes towards professionalism in medicine. Med Edu. 2007;41(8):822–829. doi:10.1111/j.1365-2923.2007.02804.x
26. Al-Rumayyan A, Van Mook W, Magzoub M, et al. Medical professionalism frameworks across non-Western cultures: a narrative overview. Med Teach. 2017;39(sup1):S8–S14. doi:10.1080/0142159X.2016.1254740
27. Benbassat J, Baumal R. Enhancing self-awareness in medical students: an overview of teaching approaches. Acad Med. 2005;80(2):156–161. doi:10.1097/00001888-200502000-00010
28. Cho KK, Marjadi B, Langendyk V, Hu W. Medical student changes in self-regulated learning during the transition to the clinical environment. BMC Med Educ. 2017;17(1):1–8.
29. Weidenbusch M, Lenzer B, Sailer M, et al. Can clinical case discussions foster clinical reasoning skills in undergraduate medical education? A randomised controlled trial. BMJ Open. 2019;9(9):e025973. doi:10.1136/bmjopen-2018-025973
30. Evans D, Sheares BJ, Vazquez T-L. Educating health professionals to improve quality of care for asthma. Paediatr Respir Rev. 2004;5(4):304–310. doi:10.1016/j.prrv.2004.07.007
31. Wu AW, Busch IM. Patient safety: a new basic science for professional education. GMS J Med Educ. 2019;36(2):Doc21.
32. Cheng T-M. Vietnam’s health care system emphasizes prevention and pursues universal coverage. Health Aff. 2014;33(11):2057–2063. doi:10.1377/hlthaff.2014.1141
33. Nhan VT. An instrument to assess of the perceptions of the medical professionalism of Vietnamese medical students and physicians: A psychometric analysis [unpublished dissertation]. Italy: University Ambrosiana; 2011.
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

