Back to Journals » International Journal of General Medicine » Volume 12
Health risk behaviors, musculoskeletal disorders and associated cultural adaptation, depression: a survey among Myanmar migrant workers in Chiangmai, Northern Thailand
Authors Aung TNN , Shirayama Y, Moolphate S , Aung MN , Lorga T, Yuasa M
Received 4 March 2019
Accepted for publication 10 July 2019
Published 14 August 2019 Volume 2019:12 Pages 283—292
DOI https://doi.org/10.2147/IJGM.S207022
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Thin Nyein Nyein Aung,1 Yoshihisa Shirayama,2 Saiyud Moolphate,3 Myo Nyein Aung,4 Thaworn Lorga,5 Motoyuki Yuasa2
1Department of Public Health, Graduate School of Medicine, Juntendo University, Tokyo, Japan; 2Faculty of International Liberal Arts, Juntendo University, Tokyo, Japan; 3Department of Public Health, Faculty of Science and Technology, Chiang Mai Rajabhat University, Chiangmai, Thailand; 4Advanced Research Institute for Health Science, and Faculty of International Liberal Arts, Juntendo University, Tokyo, Japan; 5Department of Research and Community Engagement, Research Coordinating Unit, Boromrajonani College of Nursing, Nakhon Lampang, Thailand
Background and purpose: When migrants go to a new country to work, they experience transition of epidemiological risk factors, a new system of access to healthcare and changing life styles. Their comprehension of health risk factors will depend on acculturation pattern. Moreover, musculoskeletal disorders (MSDs) are significantly prevalent in such a population due to the manual work in their jobs. Myanmar immigrant’s acculturation level has not yet been studied in relation to prevalent diseases. This study aimed to investigate health risk behaviors, the prevalence of musculoskeletal disorders, and associated factors.
Methods: A cross-sectional study surveyed 414 Myanmar migrant workers in Chiangmai, Thailand. Face-to-face interviews administered structured questionnaires which comprised the transculturally validated East Asian Acculturation Measure scale, Standardized Nordic musculoskeletal questionnaires, Patient Health Questionnaires 2 and 9 for depression and questionnaires to screen health behaviors and jobs. Data analysis applied binary logistic regression.
Results: About 26.3% were current smokers and 40.8% current drinkers. Of the 75.8% of participants did not exercise, 40.1% were overweight and obese, 44.7% had prehypertension, 27.1% hypertension, and 13% had depression. The prevalence of MSDs at any site over the previous 12 months was 53.4% and it was significantly associated (P-value≤0.05) with female (adjusted odd ratio (aOR)=1.75; 95% confidence interval (CI)=1.04–2.94), depression (aOR=2.19;CI=1.10–4.39), marginalization pattern of acculturation (aOR=1.87;CI=1.09–3.21) and MSDs at any site last week (aOR=8.41;CI=4.09–17.30).
Conclusion: Health behaviors in this young, working migrant population are risky, and MSDs are common problems for migrant workers in northern Thailand. Findings of the current study highlighted health behaviors and cultural adaption as attributes to chronic, disabling, and common health problems of migrant workers. Public health interventions and recommendations considering this evidence may improve migrants’ health status, leading to better quality-of-life and productivity.
Keywords: acculturation, depression, health risk behaviors, musculoskeletal disorders, Myanmar migrant workers, Thailand
Introduction
Thailand is the main destination for international migration in the greater Mekong sub-region and, as of May 2016, about 2 million documented migrants are working in Thailand and, among them, about 80% are from Myanmar.1,2 Mostly, they are employed in low skilled jobs and manual labors. As a result, musculoskeletal disorders (MSDs) are common amongst migrant workers due to the nature of their jobs. Moreover, the perception of pain is multifactorial and the MSDs may be related to the extent of how the migrants can adapt to the new working environment and their physical and mental health. According to the criteria of Kuorinka et al,3 the MSDs may be defined as an ache, pain, discomfort, or numbness in the defined area over a set period of time. It can range from minor discomfort to severe pain and loss of function. It can lead to the migrant workers not only suffering from symptoms but also absence from jobs, treatment costs, and loss of income. The Thailand Ministry of Public Health4 noted that MSDs were the top leading cause of outpatient visits for healthcare providers in 2015. According to the World Health Organization, Thailand,5 migrant workers constitute more than six percent of the national GDP. Since migrant workers are a vulnerable population to various kinds of health and social security threats, research focusing on the migrant population is consistently necessary.
Currently, Myanmar migrants working in Chiang Mai province, Thailand are ethnically Myanmar and Shan who shared more or less similar culture and religious practices. Though Myanmar language is an official and school language in their country of origin, their language skills are diverse depending on education background at Myanmar government schools. Their culture, social contexts and Thai Language proficiencies are also variable. Moreover, their adaptation to the Thai context in Chiang Mai is different. When migrants move to a new country to work, they experience a transition of epidemiological risk factors, a new system of access to healthcare, and changing life style such as food and drinks. However, their comprehension of health risk factors, access to healthcare and health promotion and preventive practices in a new country will depend on the acculturation process. Acculturation is a process in which an individual adopts, acquires, and adjusts to a new cultural environment.6 In public health literature, the concept of acculturation has included both unidimensional and bi dimensional models. Park7 first postulated a unidimensional model by considering the process as it occurs to entire cultures through invasion and migration. According to this theory, greater acculturation is both the result and cause of the loss of one’s original culture, and it can be best described by assimilation where an individual becomes part of the new group. One of the most widely used, Berry’s bi-dimensional model, proposed that acquiring or adhering to a new dominant culture is independent of maintaining the culture of origin. Acculturation is a long-term, lengthy, fluid process that can result in lasting change to both minority culture and dominant society. It is defined as alterations that result from continuous, direct contact between members in different cultural groups. Berry proposed four possible strategies/outcomes of acculturation: assimilation, separation, integration, and marginalization. The acculturation strategies of Myanmar migrant workers will depend on the extent in which they can adjust and develop themselves in the new environment in Thailand.8–10 When individuals do not wish to maintain the heritage culture and wish to seek daily interaction with the host culture, assimilation is defined. In contrast, when the immigrant holds the original heritage and wishes to avoid the host culture at the same time, it is termed separation. When there is an interest in maintaining both the original and host cultures, integration is the option. Marginalization is when there is little interest in maintaining the original culture (often for reasons of enforced cultural loss) and little interest in relation with the host culture (often for discrimination).11 Qualitative studies in Chiangmai found that Myanmar migrants in Chiangmai were mainly Shan ethnic, and that they had assimilation, separation, and integration patterns of acculturation.12,13 We want to measure their pattern of acculturation relating to health.
Existing literature pointed out the prevalence of musculoskeletal disorders related to their job nature and working hours, but it’s association with the pattern of acculturation and other health risk factors was not yet studied in this migrant population.14,15 In addition, acculturation can have positive or negative impacts on health,16 and, when Myanmar migrant workers move to Thailand, a country richer than their native country, their lifestyle changes and health risk behaviors also become interesting and important issue in public health.
Materials and methods
Research design
A cross- sectional survey with face-to-face interviews administering structured questionnaires was done. Adult migrant workers (18–60 years old) from Myanmar who provided written informed consent voluntarily participated in this study.
Population and study population
The sample size of the study population was calculated by using Taro Yamane formulae, and the formulae used was stated as n=[N/1+N(e)2], where, n=sample size; N=total population; and e=tolerable error (0.05 or 95%).17 The population of 81,299 Myanmar migrants working in Chiang Mai province was considered the total population and a sample size of about 398 was calculated. A total of 414 participants were included in the final analysis.
Research instruments
The questionnaires in the Thai and Myanmar version consisted of seven parts; (1) Demographic characteristics, (2) Health behaviors, (3) Job factors, (4) Standardized Nordic questionnaires, (5) East Asian Acculturation Measure (EAAM), (6) Patient Health Questionnaires 2 (PHQ2), Patient Health Questionnaires 9 (PHQ9), and (7) Health assessments.
Demographic characteristics of the participants included age, sex, education, marital status, Thai language skills, and duration of stay in Thailand. Regarding health behaviors, smoking and alcohol, sleeping hours, frequency of eating vegetables, exercise, knowledge about health insurance, and health seeking behaviors were included. Job factors included types of job, job wages, job hours per day, estimated income per month, duration of current job, and job postures.
Standardized Nordic questionnaires consisted of questionnaires asking about the last 7 days prevalence and past 12 months prevalence of MSDs indicated in the body map for nine regions (neck, shoulders, upper back, elbows, wrists/hands, lower back, hips/thighs, knees, ankles/feet) with yes or no responses. The questionnaires have been extensively used in research studies on MSDs in the general population and among different occupational groups and are considered to be highly reliable.18,19 The respondents’ subjective assessment of musculoskeletal disorders experienced in the last 1 week and last 12 months could be identified on a body map. Furthermore, whether such troubles prevented them from doing their normal activities such as job, housework, and hobbies, and whether they had seen a physician for that troubles were also asked.
Acculturation pattern was measured by the EAAM.20 The EAAM was identified as validated in an Asian population and the original EAAM was adapted for Myanmar workers in a Thailand setting. It consisted of four dimensions: Integration (5 items), Separation (7 items), Assimilation (8 items), and Marginalization (9 items). Items were rated on a 7-point Likert scale ranging from 1 (strongly disagree) to 7 (strongly agree), and the respective sub-scale items were summed and divided by the number of items to yield a mean scale for each pattern. The scales were then recoded as dichotomous variables, with 0=score less than 3.50 and 1=score greater than or equal to 3.50, in accordance with Barry.20
Depression was screened by patient health questionnaires PHQ 2 first, followed by assessment with PHQ 9 for participants with one positive response in PHQ 2. This was a validated and commonly used screening tool for depression.21 The total scores for PHQ 9 were summed up and categorized into five groups; none or minimal (0–4), mild (5–9), moderate (10–14), moderately severe (15–19), and severe (20–27) depression groups. The dichotomous variables, with 1=no depression and 2=mild, moderate, moderately severe, and severe depression, were recoded.
According to the WHO22 process of translation and adaptation of instruments, all the study instruments were translated to Myanmar and Thai languages and back translated into English and retranslated into Myanmar and Thai by independent language experts and reviewed and edited by researchers after pilot testing among migrant workers. The overall reliability coefficients Cronbach’s alpha of Nordic questionnaires, EAAM, PHQ 2, and PHQ 9 were 0.92 (Thai) and 0.89 (Myanmar), 0.82 (Thai) and 0.73 (Myanmar), and 0.97 (Thai) and 0.75 (Myanmar), respectively.
Health assessments included body weight, height, waist circumference, hip circumference, body fat percentage, blood pressure measurements. All measurements were carried out by well- trained investigators.
Data collection
This study was conducted in accordance with the Declaration of Helsinki, and ethical approval was obtained from The Ethical Review Committee for Research in Human Subjects: Boromarajonani College of Nursing Nakhon Lampang: Praboromarajchnok, Institute for Health Workforce Development, Ministry of Public Health, Thailand (approval number E 2560/39, dated October 31, 2017). Permission to recruit the migrant workers was obtained from the director of Provincial Employment Office, Chiangmai, Thailand (approval number 533.02.09, dated November 22, 2017). Data collection was done during the whole month of December 2017 at Chiangmai provincial employment office where there was a one stop service for registration of migrant workers to issue the certificate of identity by Myanmar Ministry of Labor, Immigration and Population, and visa and work permit by Thailand Ministry of Interior, Department of Employment. While waiting in the queue for the work permit and certificate of identity, we recruited the potential participants and the procedures to be conducted in our research were explained well. The measurement of blood pressure, body mass index, body fat percentage, and waist–hip ratio would not harm the participant and the risk in participation in this research was minimal and negligible. Their voluntary participation in our research was requested and they were recruited with their written informed consent. A face-to-face interview was conducted by trained research assistants who were able to speak in Thai, Myanmar, and Shan languages.
Health assessments were as follows; standing height without shoes and body weight without any jackets were measured by using a portable stadiometer and digital weighing scale, and body mass index (BMI) was calculated. With an Omron HBF 306 fat loss monitor, set with individual age (completed years), sex, weight (kg) and height (cm), body mass index, basal metabolic rate, body types; lean, muscular, normal, latent obesity, obesity and body fat percentage were measured. Waist circumference and hip circumference were measured to the nearest 0.1 cm by a standard measuring tape. Waist circumference was measured at the midway point between the lowest palpable rib and the anterior superior iliac crest, and hip circumference was measured around the widest part of the buttock. Blood pressure was measured by an Omron digital sphygmomanometer and the measurement was repeated a second time after taking a rest for 5 minutes if initial blood pressure was more than 140/90 mmHg.
Data analysis
Data were entered, validated, and analyzed by SPSS version 24, and some continuous variables were made into dichotomous categorical variables by using suitable standard cut-offs. Data from health assessments were categorized according to specific guidelines in each item as follows; Body Mass Index (BMI) was categorized into four groups, Underweight: BMI <18.5, Normal: BMI 18.5–22.9, Overweight: BMI 23–24.9 and Obese: BMI ≥25 according to Asia Pacific guidelines.23 Blood pressure measurements were categorized into three groups, normo-tension: systolic blood pressure (SBP) <120 mmHg and diastolic blood pressure (DBP) <80 mmHg; pre-hypertension: SBP 120–139 mmHg or DBP 80–89 mmHg; and hypertension: SBP ≥140 mmHg or DBP ≥120 mmHg in accordance with hypertension screening in Thailand.24 Central obesity was calculated by sex-specific waist–hip ratio. Waist–hip ratios ≥0.9 in males and ≥0.85 in females were regarded as central obesity by WHO cut-off points.25 Age- and sex-specific body fat percentage measurements were categorized into under-fat, standard, over-fat, and obese according to Omron fat loss monitor references.26 The under-fat group included body fat percentage 0–10% in 18–39 years old males, 0–11% in 40–59 years old males, 0–20% in 18–39 years old females, and 0–21% in 40–59 years old females. The standard body fat group included body fat percentage 11–21% in 18–39 years old males, 12–22% in 40–59 years old males, 21–34% in 18–39 years old females, and 22–35% in 40–59 years old females. The over-fat group included body fat percentage 22–26% in 18–39 years old males, 23–27% in 40–59 years old males, 35–39% in 18–39 years old females, and 36–40% in 40–59 years old females. The obese group included body fat percentage ≥27% in 18–39 years old males, ≥28% in 40–59 years old males, ≥40% in 18–39 years old females, and ≥41% in 40–59 years old females.
Socio-demographic characteristics were analyzed by the descriptive analysis and the comparison of means of four acculturation strategies with three groups of duration of stay in Thailand (group 1: <5 years, group 2: >5 years and <10 years, and group 3: >10 years) was done using the Kruskal Wallis test.
Data were stratified by MSDs sub-category and MSDs at any site over the last 7 days and last 12 months. Basic statistical associations between demographic, psychosocial, job factors, and health risk behaviors were initially evaluated by Chi square tests for MSDs at any sites over the last 12 months and last 7 days. Risk factors were then calculated by binary logistic regression. Previous 12 months MSDs at any sites was used as a dependent variable, with demographic (individual) factors and psychosocial factors as independent variables. Adjusted odds ratios (aOR) with 95% confidence interval and P-value≤0.05 were considered to be significant associated factors.
Results
Socio-demographic characteristics of the participants
The mean age of the study participants was 29.45±9.03 years, with 55.8% being male and 44.2% being female. Most of them were Shan ethnics (about 87%) and about 49% of participants did not have formal school education (shown in Table 1). According to the findings of the EAAM, separation was the most predominant acculturation strategy, followed by integration, assimilation, and marginalization (Figure 1).
 |
Table 1 Characteristics of the study population |
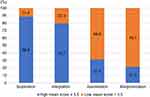 |
Figure 1 Acculturation strategies of the study participants. |
By comparing the means of four acculturation strategies, the significant differences between the means of separation, integration, assimilation strategies and three groups of duration of stay in Thailand were noted (Figure 2).
 |
Figure 2 Differences between the means of acculturation strategies and duration of stay in Thailand. |
Health assessment of the participants
The mean body fat percentage was 23.26±7.09% and about 68.1% could not have adequate sleeping hours at night; health assessments are described in Table 2.
 |
Table 2 Health assessments of the study population |
Prevalence of musculoskeletal disorders
Of the 53.4% of participants had MSDs at any site over the last 12 months and about 18.1% had MSDs at any site over the last 7 days. Low back was the most prevalent site in both situations, and the results are shown in Table 3. Binary logistic regression analysis indicated statistically significant associations (P-value≤0.05) between MSDs at any site over the last 12 months and several factors, and the results are given in Table 4.
 |
Table 3 Prevalence of musculoskeletal disorders |
 |
Table 4 Factors associated with MSDs at any site in the last 12 months |
Discussion
Our study population included a young adult working population mainly, but their health behaviors are risky. When compared to the findings of a prospective cohort study in the Thai rural community of similar socioeconomic characteristics which was conducted from 2008–2015, percentages of current smokers and prehypertension are higher in our participants than Thai adults in that study. (26.3% vs 20.82% and 44.7% vs 29.39% respectively).27 The mean duration of smoking in the study participants is about 8.00±8.52 years. But, about 40.8% of current drinkers in this study are lower than 44.13% in that cohort study and spirits is the most common type of alcohol in this population. The prevalence of hypertension and insufficient physical activity is also lower than Thai adults in the rural community (28.93% vs 27.1% and 77.28% vs 75.8%, respectively). However, the prevalence of smoking, alcohol drinking and physical inactivity is quite high compared to another study of Myanmar youth workers in Samut Sakhon (Central Thailand) in 2000 (21.5% current smokers, 25.4% alcohol drinkers, and 36.7% physical inactivity).28 Their health behaviors are riskier than that of their host and native countries.4,29,30 Although their lifestyles are risky, their knowledge about the healthcare system is poor. About 34.3% of participants do not know the migrant health insurance scheme (30 baht scheme) for registered migrants provided by the Thai government, which is higher than 10% in IOM report 2015.31
Low back MSDs is the most prevalent site like other studies in migrants in Thailand, and about 33.6% of our participants have 12 months prevalence of low back MSDs, which is higher than a study of Myanmar migrant workers in the seafood industry in Thailand.32,33
Female workers are more significantly associated with MSDs than males, and this finding is in agreement with another study of Myanmar migrant labor in Thailand, and the perception of pain and lower pain tolerance may be one of the precipitating factors for MSDs in females.34
About 13.0% of participants have depression, which is lower than the 33.3% depression rate in a study of Myanmar migrant workers in Thai and Myanmar border in 2016 but higher than the 12% prevalence of mild depression in a study conducted among Myanmar migrant students in Thailand.35,36 Depressed participants have chronic MSDs two times more than the no depression group. Perception of pain is multifactorial and a significant association of MSDs with depression is consistent with other studies.37,38
Acculturation patterns of study participants are separation (mean±SD=4.94±1.15), followed by integration (4.56±1.35), assimilation (2.96±1.18), and marginalization (2.53±1.12). Recent immigrants will be unlikely to immediately integrate into a new culture. Therefore, the time elapsed since arrival in Thailand will be an important factor to be considered, and significant differences between the means of separation, integration, assimilation, and duration of stay in Thailand were noted in this study. The marginalization group did not have any significant differences in means, but it had a significant association with MSDs at any site over the last 12 months. Immigration is one of the social determinants of health and acculturation may affect positive or negative health outcomes.37,39–41 People with a marginalization pattern of acculturation reject the receiving culture and discard the heritage culture. As Schwartz and colleagues state, it is not clear whether the immigrant paradox is due to immigrants’ acquisition of receiving-culture practices, loss of heritage culture practices, or both.42,43 Our study found that the marginalization pattern was significantly associated with chronic MSDs but in a study of South Eastern Asian female workers in Korea, separation had a significant association with work-related MSDs.44
The MSDs at any site over the last 7 days have a significant association with the MSDs at any site over the last 12 months and chronicity of the MSDs may be dependent on the acute MSDs, which is an important alarming feature for reduction of prevalence, recurrence, and chronicity of the MSDs among migrant workers.
Limitations and strengths of the study
Due to ethical reasons, our study participants represented only registered migrant workers. Moreover, subjective assessments of pain may be affected by different thresholds and memories over 12 months. Workloads by job tasks were known to be a primary risk for work-related MSDs.45,46 This study did not collect these factors, as we aimed to focus on whether there was an association between any other non-job factors and MSDs. Therefore, the findings from the current study without measures of job tasks and physical load factors provide a clue to understand the multiple risk factors for MSDs rather than conclusive evidence. A strength of our study was that we used translated questionnaires by well-trained research assistants, public health university students who were able to speak three languages, Thai, Myanmar, and Shan, and the study participants were a vulnerable migrant population.
Conclusion
Health risk behaviors, increased risks of being overweight, obesity, depression, and their significant associations with the chronic MSDs in this young adult working population are quite challenging to public health interventions. Labor intensive occupations might minimize social interactions and have a negative effect on acculturation (while simultaneously negatively impacting the worker’s health). The findings of one of the social determinants of health; acculturation affecting the MSDs should be considered in addition to the ergonomic strategies to improve MSDs of Myanmar migrant workers in Thailand. The longitudinal study to follow-up how acculturation strategies change with their stay in a host country and its impact on health could be useful to prevent chronic, disabling, and common musculoskeletal problems in this registered migrant population. Gender, depression, pattern of acculturation, and the acute MSDs will be additional important determinants of the chronic MSDs in the young adult working population. Target interventions aimed at improving the psychosocial and socio-cultural aspects of the working environment of migrant workers should be included in the local migrant friendly health services. In addition, according to the Thailand migration report of 2019, there is no integrated health information system for the data base on migrant health.47 The fragmented databases managed by the Ministry of Interior, Ministry of Labor and Ministry of Public Health should be synchronized to provide the important resources for future research on the top leading cause of outpatient visits; musculoskeletal disorders among migrant workers in Thailand.
Acknowledgments
We would like to thank study participants and the director of the provincial employment office, Chiangmai, Thailand for their collaboration for data collection there. This study was financially supported by the Japanese Ministry of Education Grant 15K 08822.
Author contributions
Thin Nyein Nyein Aung and Yoshihisa Shirayama were lead authors who designed the study. All authors contributed to data analysis, drafting or revising the article, gave final approval of the version to be published, and agreed to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
1. International Organization for Migration. Thailand Migration Profile; 2015.
2. Provincial Employment Office. Number of Migrants. Chiangmai, Thailand; 2016.
3. Kuorinka I, Jonsson B, Kilbom A, et al. Standardised Nordic questionnaires for the analysis of musculoskeletal symptoms. Appl Ergon. 1987;18(3):233–237.
4. Ministry of Public Health. Stastistical Thailand 2017; 2017. Available from: http://bps.moph.go.th/new_bps/sites/default/files/stratistics60.pdf.
5. World Health Organization. WHO country cooperation strategy, Thailand: 2017–2021; 2017. Available from: http://apps.who.int/iris/bitstream/10665/255510/1/9789290225829-eng.pdf.
6. Akarowhe K. Effects and remedies to cultural shock on the adolescent students. Sociol Int J. 2018;2(4). doi:10.15406/sij
7. Park RE. Human migration and the marginal man. Am J Sociol. 1928;33(6):881–893. doi:10.1086/214592
8. Berry JW. Immigration, acculturation, and adaptation. Appl Psychol. 1997;46(1):5–34.
9. Berry JW. Acculturation: living successfully in two cultures. Int J Intercult Relat. 2005;29(6):697–712. doi:10.1016/j.ijintrel.2005.07.013
10. Fox RS, Merz EL, Solórzano MT, Roesch SC. Further examining Berry’s model: the applicability of latent profile analysis to acculturation. Meas Eval Couns Dev. 2013;46(4):270–288. doi:10.1177/0748175613497036
11. Berry JW. A psychology of immigration. J Soc Issues. 2001;57(3):615–631. doi:10.1111/josi.2001.57.issue-3
12. Jirattikorn A. Migration, Media Flows and the Shan Nation in Thailand. Austin: University of Texas; 2008.
13. Pripotjanart T Inequality and way of life of Burmese migrants in Thailand: a case study in Chiangmai.
14. Thetkathuek A, Yingratanasuk T, Jaidee W, Ekburanawat W. Cold exposure and health effects among frozen food processing workers in eastern Thailand. Saf Health Work. 2015;6(1):56–61. doi:10.1016/j.shaw.2014.10.004
15. Soe KT, Laosee O, Limsatchapanich S, Rattanapan C. Prevalence and risk factors of musculoskeletal disorders among Myanmar migrant workers in Thai seafood industries. Int J Occup Saf Ergon. 2015;21(4):539–546. doi:10.1080/10803548.2015.1096609
16. Davies AA, Basten A, Frattini C. Migration: a social determinant of the health of migrants. Eurohealth. 2009;16(1):10–12.
17. Yamane T. Statistics: An Introductory Analysis; 2nd ed. Tokyo: Harper & Row, New York, Evanston & London and John Weatherhill Inc.; 1973.
18. Crawford JO. The Nordic musculoskeletal questionnaire. Occup Med (Chic Ill). 2007;57(4):300–301. doi:10.1093/occmed/kqm036
19. De Barros E, Alexandre NMC. Cross‐cultural adaptation of the Nordic musculoskeletal questionnaire. Int Nurs Rev. 2003;50(2):101–108.
20. Barry DT. Development of a new scale for measuring acculturation: the East Asian Acculturation Measure (EAAM). J Immigr Health. 2001;3(4):193–197. doi:10.1023/A:1012227611547
21. Maurer DM. Screening for depression. Depression. 2012;100:23.
22. World Health Organization. Process of translation and adaptation of instruments; 2009. Available from: http://wwwwhoint/substance_abuse/research_tools/translation/en/. Accessed May 22, 2018
23. World Health Organization. The Asia-Pacific Perspective: Redefining Obesity and Its Treatment. Sydney: Health Communications Australia; 2000.
24. Charoendee K, Sriratanaban J, Aekplakorn W, Hanvoravongchai P. Assessment of population coverage of hypertension screening in Thailand based on the effective coverage framework. BMC Health Serv Res. 2018;18(1):208. doi:10.1186/s12913-018-2996-y
25. World Health Organization. WaistCircumference and waist ratio, waist-hip.
26. Gallagher D, Heymsfield SB, Heo M, Jebb SA, Murgatroyd PR, Sakamoto Y. Healthy percentage body fat ranges: an approach for developing guidelines based on body mass index. Am J Clin Nutr. 2000;72(3):694–701. doi:10.1093/ajcn/72.3.694
27. Kittithaworn A, Dy R, Hatthachote P, et al. Incidence and associated factors of Type 2 diabetes: a community-based cohort study in the central region of rural community in Thailand. Asia Pac J Public Health. 2019;31(1):72–83. doi:10.1177/1010539518822441
28. Howteerakul NS, Suwannapong N, Than M. Cigarette, Alcohol Use and Physical Activity among Myanmar Youth Workers, Samut Sakhon Province, Thailand. Southeast Asian Journal of Tropical Medicine and Public Health. 2005;36(3).
29. Ministry of Health. Report on National Survey of Diabetes Mellitus and Risk Factors for Non Communicable Diseases in Myanmar; 2014.
30. World Health Organization. Non communicable diseases country profile. Thailand. 2018; Available from: https://www.who.int/nmh/countries/tha_en.pdf.
31. Pukchanok MEP, Vungsiriphisal P. Assessing potential changes in the migration patterns of Myanmar migrants and their impacts on Thailand: supplementary report; 2015. Available from: https://thailand.iom.int/supplementary-report-assessing-potential-changes-migration-patterns-myanmar-migrants-and-their.
32. Tomita S, Arphorn S, Muto T, Koetkhlai K, Naing SS, Chaikittiporn C. Prevalence and risk factors of low back pain among Thai and Myanmar migrant seafood processing factory workers in Samut Sakorn Province, Thailand. Ind Health. 2010;48(3):283–291. doi:10.2486/indhealth.48.283
33. Phajan T, Nilvarangkul K, Settheetham D, Laohasiriwong W. Work-related musculoskeletal disorders among sugarcane farmers in north-eastern Thailand. Asia Pac J Public Health. 2014;26(3):320–327. doi:10.1177/1010539514528026
34. Meepradit P. The prevalence and risk factors of musculoskeletal disorders among burmese migrant labor in Thailand. Arch Curr Res Int. 2016;1–7. doi:10.9734/ACRI/2016/23830
35. Meyer SR, Decker MR, Tol WA, Abshir N, Mar AA, Robinson WC. Workplace and security stressors and mental health among migrant workers on the Thailand–Myanmar border. Soc Psychiatry Psychiatr Epidemiol. 2016;51(5):713–723. doi:10.1007/s00127-015-1162-7
36. Khine HP, Panza A. Factors affecting anxiety and depression in myanmar migrant adolescents in Bang Bon District, Thailand. J Health Res. 2010;24(Suppl. 2):33–35.
37. Kim M, Chen J-L, Kools S, Weiss S. The impact of personality traits and acculturation on the mental health of Korean American adolescents. Psychology. 2016;7(09):1256. doi:10.4236/psych.2016.79128
38. Tribble AG, Summers P, Chen H, Quandt SA, Arcury TA. Musculoskeletal pain, depression, and stress among Latino manual laborers in North Carolina. Arch Environ Occup Health. 2016;71(6):309–316. doi:10.1080/19338244.2015.1100104
39. Castañeda H, Holmes SM, Madrigal DS, Young M-ED, Beyeler N, Quesada J. Immigration as a social determinant of health. Annu Rev Public Health. 2015;36:375–392. doi:10.1146/annurev-publhealth-032013-182419
40. Fox M, Thayer Z, Wadhwa PD. Assessment of acculturation in minority health research. Soc Sci Med. 2017;176:123–132. doi:10.1016/j.socscimed.2017.01.029
41. Choi S, Rankin S, Stewart A, Oka R. Effects of acculturation on smoking behavior in Asian Americans: a meta-analysis. J Cardiovasc Nurs. 2008;23(1):67–73. doi:10.1097/01.JCN.0000305057.96247.f2
42. Schwartz SJ, Zamboanga BL. Testing Berry’s model of acculturation: A confirmatory latent class approach. Cultur Divers Ethnic Minor Psychol. 2008;14(4):275. doi:10.1037/a0012818
43. Schwartz SJ, Unger JB, Zamboanga BL, Szapocznik J. Rethinking the concept of acculturation: implications for theory and research. Am Psychol. 2010;65(4):237. doi:10.1037/a0019330
44. Lee H, Ahn H, Park CG, Kim SJ, Moon SH. Psychosocial factors and work-related musculoskeletal disorders among Southeastern Asian female workers living in Korea. Saf Health Work. 2011;2(2):183–193. doi:10.5491/SHAW.2011.2.2.183
45. Yoopata P. Perceived work strain as indicator for occupational risks in Thai female field activities. APHEIT J. 2012;18(1):26–38.
46. Park J, Kim Y, Han B. Work sectors with high risk for work-related musculoskeletal disorders in Korean men and women. Saf Health Work. 2018;9(1):75–78. doi:10.1016/j.shaw.2017.06.005
47. United Nations Thematic Working Group on Migration in Thailand. Thailand Migration Report; 2019.
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
