Back to Journals » Patient Related Outcome Measures » Volume 9
Health-related quality of life in ANCA-associated vasculitis and item generation for a disease-specific patient-reported outcome measure
Authors Robson JC , Dawson J , Cronholm PF, Milman N, Kellom KS , Ashdown S, Easley E, Farrar JT , Gebhart D, Lanier G, McAlear CA, Peck J, Luqmani RA, Shea JA, Tomasson G, Merkel PA
Received 27 June 2017
Accepted for publication 13 October 2017
Published 4 January 2018 Volume 2018:9 Pages 17—34
DOI https://doi.org/10.2147/PROM.S144992
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr Robert Howland
Joanna C Robson,1,2 Jill Dawson,3 Peter F Cronholm,4 Nataliya Milman,5 Katherine S Kellom,6 Susan Ashdown,7 Ebony Easley,8 John T Farrar,9 Don Gebhart,10,11 Georgia Lanier,10,11 Carol A McAlear,12 Jacqueline Peck,7 Raashid A Luqmani,7 Judy A Shea,13 Gunnar Tomasson,14 Peter A Merkel10,11
1Department of Rheumatology, Faculty of Health and Applied Sciences, University of the West of England, Bristol, UK; 2School of Clinical Sciences, University of Bristol, Bristol, UK; 3Department of Population Health (HSRU), University of Oxford, Oxford, UK; 4Department of Family Medicine and Community Health, University of Pennsylvania, Philadelphia, PA, USA; 5Division of Rheumatology, Department of Medicine, University of Ottawa, Ottawa Hospital Research Institute, Ottawa, ON, Canada; 6PolicyLab, Children’s Hospital of Philadelphia, Philadelphia, PA, USA; 7Nuffield Department of Orthopaedics, Rheumatology and Musculoskeletal Sciences, University of Oxford, Oxford, UK; 8Department of Family Medicine and Community Health, Mixed Methods Research Laboratory, University of Pennsylvania, Philadelphia, PA, USA; 9Biostatistics and Epidemiology, Hospital of the University of Pennsylvania, Philadelphia, PA, USA; 10Division of Rheumatology, Department of Medicine, University of Pennsylvania, Philadelphia, PA, USA; 11Department of Biostatistics and Clinical Epidemiology, University of Pennsylvania, Philadelphia, PA, USA; 12Vasculitis Research, University of Pennsylvania, Philadelphia, PA, USA; 13School of Medicine, University of Pennsylvania, Philadelphia, PA, USA; 14Department of Public Health Sciences, University of Iceland, Reykjavik, Iceland
Objective: The antineutrophil cytoplasmic antibody (ANCA)-associated vasculitides (AAVs) are multisystem diseases of the small blood vessels. Patients experience irreversible damage and psychological effects from AAV and its treatment. An international collaboration was created to investigate the impact of AAV on health-related quality of life (HRQoL), and develop a disease-specific patient-reported outcome measure to assess outcomes of importance to patients.
Methods: Patients with AAV from the UK, USA, and Canada were interviewed to identify salient aspects of HRQoL affected by AAV. The study was overseen by a steering committee including four patient research partners. Purposive sampling of interviewees ensured representation of a range of disease manifestations and demographics. Inductive analysis was used to identify themes of importance to patients; these were further confirmed by a free-listing exercise in the US. Individual themes were recast into candidate items, which were scrutinized by patients, piloted through cognitive interviews and received a linguistic and translatability evaluation.
Results: Fifty interviews, conducted to saturation, with patients from the UK, USA, and Canada, identified 55 individual themes of interest within seven broad domains: general health perceptions, impact on function, psychological perceptions, social perceptions, social contact, social role, and symptoms. Individual themes were constructed into >100 candidate questionnaire items, which were then reduced and refined to 35 candidate items.
Conclusion: This is the largest international qualitative analysis of HRQoL in AAV to date, and the results have underpinned the development of 35 candidate items for a disease-specific, patient-reported outcome questionnaire.
Keywords: ANCA-associated vasculitis, quality of life, patient-reported outcomes, granulomatosis with polyangiitis, microscopic polyangiitis, eosinophilic granulomatosis with polyangiitis
Introduction
Granulomatosis with polyangiitis (GPA), microscopic polyangiitis (MPA), and eosinophilic granulomatosis with polyangiitis (EGPA) are organ- and life-threatening multisystem diseases of small arteries, known as the antineutrophil cytoplasmic antibody (ANCA)-associated vasculitides (AAVs).1 Patients present with inflammation in multiple body areas, including the lungs, ear, nose, kidneys, joints, and nerves,2 with fevers, weight loss, and fatigue.3 Treatment is with glucocorticoids and other immunosuppressants.4 A third of patients will have irreversible damage at diagnosis,5 and 40% will suffer relapse.6 One-year mortality in AAV has been >15%,7 a poorer survival rate than breast or prostate cancer;8 however, mortality in AAV has improved, likely due to the adoption of newer treatment regimens.9,10 Surveys have demonstrated impairments in health-related quality of life (HRQoL) in AAV, in particular fatigue.3,11–18 A clinician-derived survey to assess patient perspectives in granulomatosis with polyangiitis was developed in 1998;19 however, there have been no in-depth qualitative studies to capture patient perspectives on the full range of HRQoL in the AAVs as a whole.
Due to the relative rarity of AAV, with three overlapping disease phenotypes, patients with AAV are frequently considered together,4 with patients with GPA and MPA included within the same randomized controlled trials (RCTs).20–22 Primary outcomes are based on the physician-based Birmingham Vasculitis Activity Score,23,24 which records the presence or absence of disease activity.20–22,25 Patients with AAV, however, often have different perceptions of what is important to their physicians, for example, they rank fatigue as more important than dialysis or oxygen dependence.11 To guage the efficacy of treatments within RCTs, validated measurement of both physician- and patient-focused outcomes is key.11,26
The Outcome Measurement in Rheumatology (OMERACT) Vasculitis Working Group has consistently highlighted the need for a disease-specific patient-reported outcome (PRO) measure for patients with AAV,25,27 due to concern that the generic Medical Outcomes Short Form-36 (SF-36) may not capture all themes of importance. Since OMERACT 2012,27,28 an international collaboration (the UK, the USA, and Canada) has been developing an AAV disease-specific PRO measure, in line with the US Food and Drug Administration (FDA) guidelines for the development of PROs.29 The development of a new PRO instrument involves three distinct stages with patient involvement at each step: 1) item generation and piloting, 2) item reduction and scale generation, and 3) testing reliability and validity.
This paper describes the themes of importance in HRQoL in relation to AAV, identified through in-depth qualitative analysis in three countries in order to produce candidate questionnaire items for a new disease-specific PRO for AAV.
Methods
The study steering committee included members from the UK, USA, and Canada: four patient partners; medical sociologists with extensive experience in PROM development, testing, and application; qualitative researchers; and clinical researchers with an interest in vasculitis. An initial conceptual framework was developed, through literature review and steering committee input, to explore domains of interest, and this framework evolved during the study.
A core qualitative working group (CQWG), comprising researchers from the three countries, performed the qualitative analysis, developed a collaborative code book of themes, and produced and refined candidate items. The steering committee gave critical feedback throughout on developing themes and items and the project received critical scrutiny at three successive Vasculitis Workshop sessions at Outcome Measures in Rheumatology (OMERACT) conferences.27,28
Patient study sample
Patients diagnosed with AAV were recruited from three rheumatology centers in the UK, USA, and Canada. Inclusion criteria were age ≥18, ability to give informed consent, and a clinically verified diagnosis of GPA, MPA, or EGPA. Patients were purposively sampled to assure adequate representation of all three diseases, chronicity of disease, different age ranges, sex, and organ involvement. Study approvals were given by the NHS Research Committee South West-Central Bristol, the University of Pennsylvania Office of Regulatory Affairs, and the Ottawa Hospital’s Research Ethics Board. All patients provided written informed consent.
In-depth interviews
Exploratory semi-structured patient interviews were conducted to identify the range of salient aspects of HRQoL affected by AAV and its treatment. An interview guide of prompts and cues was developed by the steering committee. Interviews were performed by a qualitative researcher in the US (KK) and two clinical research fellows trained in qualitative interview techniques in the UK (JCR) and Canada (NM).
Analysis
Interviews were recorded and transcribed, anonymized, and systematically analyzed using a modified framework method.30–32 Coding was carried out using both an inductive (codes emerged during analysis) and deductive (codes anticipated) approach,33 with NVivo computer software used to index transcripts.34 Interviews continued until no new substantive themes arose indicating data saturation.35 The CQWG defined the themes of interest, produced a common thematic framework, and ensured uniformity of coding across sites. A proportion of transcripts from each site was double coded, to ensure common approaches.
Candidate item development
Members of the CQWG recast themes as candidate items, using patients’ descriptions throughout. Items were amended, and sometimes deleted by the CQWG, to reduce ambiguity and duplication. Piloting and further item amendment was conducted following feedback from steering committee patient partners.
US participants were invited to participate in a free-listing activity, a semi-structured interview technique in which participants are given a question or statement and asked to identify words they associate with that phrase.36 This method uncovers how groups of people with shared experiences create, associate, and categorize topics.36,37
The following questions were asked: “Which words would you use to describe your symptoms when your vasculitis: 1) first started; 2) is under control; and 3) is starting to flare?” Patient partners on the study team performed pile-sorting of the responses independently, with disagreement resolved through consensus. Following free-listing and pile-sorting, the Smith’s Salience Index (SSI)38,39 was used to identify the most salient terms. SSI scores were calculated using ARTHROPAC software. The identified salient terms were contrasted across interview themes to provide additional lens of validation for candidate item development.
Patient refinement
Three rounds of patient cognitive interviews were completed, in order to check understanding and interpretation of the candidate items.40,41 This was an iterative process, with items refined or rejected by the CQWG between each round.
In parallel, a readability and translatability assessment was completed in collaboration with a specialist UK company (Pharmaquest – translation and linguistic validation company for PROs).42 A breakout session was also held at the Vasculitis Workshop at OMERACT 2014, which sought feedback about 1) inclusion of contextual factors within the PRO and 2) attribution within the stem (or lead in sentence), to vasculitis and/or its treatment. All proposed item changes were tested by further cognitive interviews and steering committee review.
Results
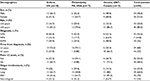
Fifty participants, 24 men and 26 women, were interviewed in the UK, USA, and Canada. Participants’ characteristics are shown in Table 1. Interview transcripts were analyzed, identifying 55 individual themes of interest, grouped into seven domains (definitions of individual themes within the codebook in Table S1). The domains identified were general health perceptions, impact on function, psychological perceptions, social perceptions, social contact, social roles, and symptoms (Box 1 shows domain structure and individual themes). The saturation table of emergent themes is shown in Table S2.
  | Box 1 Domains and individual themes from patients with ANCA-associated vasculitis |
General health perceptions
Eighty-six percent of patients used descriptions of how their general sense of self and wellness had been affected by developing AAV. Concerns about the future and difficulties making long-term plans were prominent, as was a sense of vulnerability in one’s own body.
“If I compare to 3 years ago… I was the guy who was working 7 days a week, 16 hour days, never tired. Now… Ufff. It’s not the same guy anymore.” [47-year-old male with EGPA]
“I didn’t want to set foot outside the door. Simply because I thought … I can’t trust my body anymore”. [53-year-old female with EGPA]
Impact on function
Ninety percent of participants described difficulties with reduced levels of physical function, over 80% had a reduction in mobility, and 20% described difficulties in washing and dressing. These impairments led to frustration and impacted finances and work (82%), the ability to perform household tasks (72%), taking part in hobbies and interests (46%), and restricted travel (76%).
“Weakness, inability to walk, to use my arms, to bathe, to do anything – I just laid in bed”. [82-year-old male with MPA]
“TV was a no-no. I got a telephone with a light on it, because it [the deafness] was that bad… I felt very isolated and very stupid”. [57-year-old male with GPA]
Psychological
Concerns about the future were highlighted in 86% of interviews with over 70% reporting experiencing fear, anxiety, or stress, and 50% describing depression or low mood. Anger or irritation was reported by almost 50%. Difficulties in making plans and the potential for premature death were described by patients of all ages.
“For the first year after I was diagnosed, I did nothing, apart from cope with me, my illness and trying to live as normal a life as possible”. [67-year-old female with GPA]
“I was only [age], my first year of college – everything is falling apart and I think I’m dying”. [36-year-old female with GPA]
Social perceptions
Participants were aware of the visibility of the condition, and its treatment side-effects, particularly in relation to glucocorticoids; these issues were discussed in 64% of interviews. A lack of empathy from others was reported by around 60% of interviewees, as was being the source of worry to others.
“To have a big puffy moon face [due to glucocorticoids] is really hard for me. Well, you’re not attractive anymore – it’s weird”. [33-year-old female with GPA]
“I think some people were more supportive than others, and it wasn’t always the people I expected to be”. [67-year-old female with GPA]
Social contact
Eighty percent of interviewees described an impact on their social life, because of fatigue, difficulties with joining in physical activities or communicating, or concerns about letting people down by having to break plans.
“If we had a dinner date on the weekend I had to rest coming up to that day just to be able to have enough energy. I got to a point where I just didn’t bother”. [51-year-old female with EGPA]
“Meetings were the worst. Because I found that I was lip-reading. In an open room with a number of people, it was a nightmare”. [57-year-old male with GPA]
Social role
Eighty-two percent of participants discussed their occupation or finances, specifically stemming from difficulties with concentration and fatigue. Roles beyond work were also discussed, within the family (70%), and changes to role and status when having to rely on others for help (64%).
“When I was getting sick in the beginning I gave up my position as the executive director of the organization and I moved into a position with less responsibility”. [52-year-old female with GPA]
“It was hard on my son as well, so he started goofing off in school. I felt like I wasn’t a good mom, I wasn’t a good wife, and I was isolated”. [51-year old female with EGPA]
Symptoms
All of the patients described symptoms due to disease and treatment in depth. Nineteen different sets of symptoms were identified, most frequently fatigue (88%), cardiorespiratory symptoms (76%), issues related to body weight (74%), and upper respiratory tract symptoms (70%). A full list of symptoms is given in Box 1, with quotes in Box 2.
  | Box 2 Patient descriptions of symptoms of ANCA-associated vasculitis and its treatment |
Free-listing and pile-sorting items of importance to patients with AAV
All 17 US patients interviewed were invited to free-list terms they associated with the onset, remission, and flaring of their AAV (Figure 1). The most salient themes at onset were pain and discomfort (SSI=0.37), nasal and sinus problems (SSI=0.32), and fatigue and energy levels (SSI=0.27). Emotional effects were within the top three during flare (SSI=0.28) and remission (SSI=0.27). Themes identified were compared with the individual themes of interest and domains from the in-depth patient interviews and no new themes were identified (Box 1 for overview and Table S1 for detailed descriptions).
Candidate item development
Fifty-five individual themes were identified from the qualitative work (Box 1), and these were recast into an initial list of 105 candidate items by members of the CQWG. Patient descriptions informed the design of the candidate questionnaire items and response options, resulting in different sections. Patients described the overall severity of their symptoms, rather than the frequency; pain was usually described in relation to specific body areas, such as joints or muscles; and ability to function was described in terms of the amount of difficulty with completing a specific task. The candidate items were scrutinized for duplication and ambiguity of items, reducing the item pool to 42 items. Patients made it clear that it was difficult to tease apart symptoms caused by AAV versus its treatment, so both were included within the stem of the question. Items related to contextual factors (eg, support and self-efficacy – Box 1 and Table S1) were not included within the PRO itself, after discussion at an OMERACT 2014 breakout session with patient participants.28
Three rounds of cognitive interviews were conducted in the UK and USA, using the 42-item version of the questionnaire, with amendments after each round. Word changes were suggested by patients, for example, clarification of the word essential in relation to activities, and change to the period of recall from 7 days to 4 weeks. All participants reported that the questionnaire captured content relevant to them. Seven items were rejected because of ambiguity, repetition, or being contextual factors. Following the translatability assessment (Box S1), minor changes were made to a few items, and these revisions were piloted in the last round of interviews. The conceptual framework evolved in response to insights from the qualitative research, feedback from the steering committee, and breakout sessions at OMERACT, and the final version is shown in Figure 2. The resulting 35-item candidate pool is shown in Box 3.
  | Box 3 Candidate item pool for the questionnaire |
Discussion
This is the most comprehensive evaluation of the patient perspective in AAV to date. Patients have been an integral part of this work as key members of the steering committee and qualitative interview participants, reflecting all three diseases, differing disease manifestations, a wide demographic range, and three different countries. The item generation for a novel, disease-specific PRO measure is underpinned by this qualitative research, which should ensure that the final candidate items have good face validity within each country. Themes identified in previous quantitative studies are confirmed, for example, fatigue,13 anxiety, and depression,16 and the impact on everyday function and employment.17,43 Newer themes include difficulties in making plans, from short-term social engagements to life planning, previously reported in patients with systemic lupus erythematosus, rheumatoid arthritis, and GPA.19,44,45
The strengths of this study include a high level of patient involvement, and ongoing critical review through OMERACT Workshops, which have helped to ensure that each stage was consistent with best practice. Patients were purposively sampled to include a range of disease features and demographics, including a high proportion of patients with recent active disease. This was to ensure a focus on themes (and then items), which would exhibit greatest change in the context of a RCT. A third of patients had longer-standing disease, and saturation of themes was also reached within this patient group. The high rate of relapsing disease may also be a reflection of the fact that patients with GPA, who have a higher rate of relapse,46 were slightly over-represented compared with patients with MPA; this may be a potential bias of the sample. That only English-speaking participants were included is a limitation of this study. However, a translatability assessment was performed for the questionnaire items, to ensure that any future translation into a range of languages should be straightforward.47 In addition, care was taken to develop items that were not overly culture-specific, for example, describing “difficulties with traveling far from home,” rather than “going on holidays.” Interviews were performed by clinical fellows in the UK and Canada, and this may have changed the way that patients described problems in relation to their disease or treatment. Training was, therefore, provided by experienced social scientists, who also evaluated all interview transcripts.
The OMERACT Vasculitis Working Group has highlighted the lack of a disease-specific PRO for AAV.27 As per FDA guidance, the development of a PRO instrument should start with qualitative analysis involving patients with the disease, in order to identify themes of importance. However, generic PRO instruments, such as the SF-36,48 can be used to measure and compare HRQoL between patients with different chronic conditions, and population norms. A combined approach of using disease-specific and generic PRO measures may, therefore, be the optimum way of comprehensively measuring HRQoL in AAV.49
The 35-item candidate questionnaire will need to be shortened to reduce responder burden and optimize feasibility within RCTs. The next stage of development will involve a large-scale survey to facilitate further item reduction, and determine the underlying scale structure and measurement properties (reliability, validity, and responsiveness) of the final AAV-PRO instrument.
Acknowledgments
Sponsored by the University of Oxford, the Vasculitis Clinical Research Consortium and the University of Ottawa. With support from the Medical Research Fund, Oxford, the Oxfordshire Health Services Research Committee (Ref 1098), the US National Institute of Arthritis and Musculoskeletal and Skin Diseases (U54 AR057319 and U01 AR51874), the National Center for Research Resources (U54 RR019497), and the Office of Rare Diseases Research. Oxford University Innovation funded the translatability exercise. Additional support received by a Patient-Centred Outcomes Research Institute Pilot Project Grant.
Disclosure
Dr Robson and Professor Luqmani were supported in part by the National Institute for Health Research Musculoskeletal Biomedical Research Unit, Oxford, UK. Dr Robson was supported by a National Institute for Health Research (NIHR) clinical lectureship. Dr Milman was supported by a UCB/Canadian Rheumatology Association/Arthritis Society postgraduate rheumatology fellowship award and a research fellowship from the Department of Medicine at the Ottawa Hospital. The authors report no other conflicts of interest in this work.
References
Jennette JC, Falk RJ, Bacon PA, et al. 2012 revised international chapel hill consensus conference nomenclature of vasculitides. Arthritis Rheum. 2013;65(1):1–11. | ||
McNicholas BA, Griffin TP, Donnellan S, et al. ANCA-associated vasculitis: a comparison of cases presenting to nephrology and rheumatology services. QJM. 2016;109(12):803–809. | ||
Basu N, Jones GT, Fluck N, et al. Fatigue: a principal contributor to impaired quality of life in ANCA-associated vasculitis. Rheumatology (Oxford). 2010;49(7):1383–1390. | ||
Yates M, Watts RA, Bajema IM, et al. EULAR/ERA-EDTA recommendations for the management of ANCA-associated vasculitis. Ann Rheum Dis. 2016;75(9):1583–1594. | ||
Robson J, Doll H, Suppiah R, et al. Damage in the anca-associated vasculitides: long-term data from the European vasculitis study group (EUVAS) therapeutic trials. Ann Rheum Dis. 2015;74(1):177–184. | ||
Walsh M, Flossmann O, Berden A, et al. Risk factors for relapse of antineutrophil cytoplasmic antibody-associated vasculitis. Arthritis Rheum. 2012;64(2):542–548. | ||
Flossmann O, Berden A, de Groot K, et al; European Vasculitis Study Group. Long-term patient survival in ANCA-associated vasculitis. Ann Rheum Dis. 2011;70(3):488–494. | ||
Quaresma M, Coleman MP, Rachet B. 40-year trends in an index of survival for all cancers combined and survival adjusted for age and sex for each cancer in England and Wales, 1971–2011: a population-based study. Lancet. 2015;385(9974):1206–1218. | ||
Hilhorst M, Wilde B, van Paassen P, Winkens B, van Breda Vriesman P, Cohen Tervaert JW; Limburg Renal Registry. Improved outcome in anti-neutrophil cytoplasmic antibody (ANCA)-associated glomerulonephritis: a 30-year follow-up study. Nephrol Dial Transplant. 2013;28(2):373–379. | ||
Rhee RL, Hogan SL, Poulton CJ, et al. Trends in long-term outcomes among patients with ANCA-associated vasculitis with renal disease. Arthritis Rheumatol. 2016;68(7):1711–1720. | ||
Herlyn K, Hellmich B, Seo P, Merkel PA. Patient-reported outcome assessment in vasculitis may provide important data and a unique perspective. Arthritis Care Res (Hoboken). 2010;62(11):1639–1645. | ||
Walsh M, Mukhtyar C, Mahr A, et al. Health-related quality of life in patients with newly diagnosed antineutrophil cytoplasmic antibody-associated vasculitis. Arthritis Care Res (Hoboken). 2011;63(7):1055–1061. | ||
Basu N, McClean A, Harper L, et al. The characterisation and determinants of quality of life in ANCA associated vasculitis. Ann Rheum Dis. 2014;73(1):207–211. | ||
Carpenter DM, Thorpe CT, Lewis M, Devellis RF, Hogan SL. Health-related quality of life for patients with vasculitis and their spouses. Arthritis Rheum. 2009;61(2):259–265. | ||
Tomasson G, Boers M, Walsh M, et al. Assessment of health-related quality of life as an outcome measure in granulomatosis with polyangiitis (Wegener’s). Arthritis Care Res. 2012;64(2):273–279. | ||
Koutantji M, Harrold E, Lane SE, Pearce S, Watts RA, Scott DG. Investigation of quality of life, mood, pain, disability, and disease status in primary systemic vasculitis. Arthritis Rheum. 2003;49(6):826–837. | ||
Benarous L, Terrier B, Laborde-Casterot H, et al; French Vasculitis Study Group (FVSG). Employment, work disability and quality of life in patients with ANCA-associated vasculitides. The EXPOVAS study. Clin Exp Rheumatol. 2017;103(1):40–46. | ||
Boomsma MM, Bijl M, Stegeman CA, Kallenberg CG, Hoffman GS, Tervaert JW. Patients’ perceptions of the effects of systemic lupus erythematosus on health, function, income, and interpersonal relationships: a comparison with Wegener’s granulomatosis. Arthritis Rheum. 2002;47(2):196–201. | ||
Hoffman GS, Drucker Y, Cotch MF, Locker GA, Easley K, Kwoh K. Wegener’s granulomatosis: patient-reported effects of disease on health, function, and income. Arthritis Rheum. 1998;41(12):2257–2262. | ||
Jones RB, Tervaert JW, Hauser T, et al; European Vasculitis Study Group. Rituximab versus cyclophosphamide in ANCA-associated renal vasculitis. N Engl J Med. 2010;363(3):211–220. | ||
Stone JH, Merkel PA, Spiera R, et al; RAVE-ITN Research Group. Rituximab versus cyclophosphamide for ANCA-associated vasculitis. N Engl J Med. 2010;363(3):221–232. | ||
Guillevin L, Pagnoux C, Karras A, et al; French Vasculitis Study Group. Rituximab versus azathioprine for maintenance in ANCA-associated vasculitis. N Engl J Med. 2014;371(19):1771–1780. | ||
Luqmani RA, Bacon PA, Moots RJ, et al. Birmingham vasculitis activity score (BVAS) in systemic necrotizing vasculitis. QJM. 1994;87(11):671–678. | ||
Mukhtyar C, Lee R, Brown D, et al. Modification and validation of the birmingham vasculitis activity score (version 3). Ann Rheum Dis. 2009;68(12):1827–1832. | ||
Merkel PA, Aydin SZ, Boers M, et al. The OMERACT core set of outcome measures for use in clinical trials of ANCA-associated vasculitis. J Rheumatol. 2011;38(7):1480–1486. | ||
Kirwan JR, Hewlett SE, Heiberg T, et al. Incorporating the patient perspective into outcome assessment in rheumatoid arthritis progress at OMERACT 7. J Rheumatol. 2005;32(11):2250–2256. | ||
Merkel PA, Aydin SZ, Boers M, et al. Current status of outcome measure development in vasculitis. J Rheumatol. 2014;41(3):593–598. | ||
Robson JC, Milman N, Tomasson G, et al. Exploration, development, and validation of patient-reported outcomes in antineutrophil cytoplasmic antibody-associated vasculitis using the OMERACT process. J Rheumatol. 2015; 42(11):2204–2209. | ||
Guidance for Industry: Patient-Reported Outcome Measures: Use in Medical Product Development to Support Labelling Calims. In: (FDA) USDoHaHSFaDA, editors. Maryland: FDA; 2009. | ||
McColl E. Developing questionnaires. In: Fayers P, Hays R, eds. Assessing Quality of Life in Clinical Trials. 2nd ed. Oxford, UK: Oxford Medical Publications; 2005. | ||
Ritchie J, Spencer L. Qualitative data analysis for applied policy research. In: Bryman A, Burgess RG, eds. Analysing Qualitative Data. London, UK: Routledge; 1994. | ||
Pope C, Ziebland S, Mays N. Qualitative research in health care. Analysing qualitative data. BMJ. 2000;320(7227):114–116. | ||
Fereday J, Muir-Cochrane E. Demonstrating rigor using thematic analysis: a hybrid approach of inductive and deductive coding and theme development. Int J Qual Meth. 2006;5:1–22. | ||
International Q. NVivo qualitative data analysis software. Version 10. QSR International; 2012. Available from: qsrinternational.com. Accessed October 11, 2017. | ||
Kerr C, Nixon A, Wild D. Assessing and demonstrating data saturation in qualitative inquiry supporting patient-reported outcomes research. Expert Rev Pharmacoecon Outcomes Res. 2010;10(3):269–281. | ||
Borgatti SP. Elicitation techniques for cultural domain analysis. Enhanced ethnographic methods: audiovisual techniques, focused group interviews, and elicitation techniques. In: Ethnographer Toolkit. Walnut Creek, CA: Alta Mira; 1999:115–151. | ||
Schrauf RW, Sanchez J. Using freelisting to identify, assess, and characterize age differences in shared cultural domains. J Gerontol B Psychol Sci Soc Sci. 2008;63(6):S385–S393. | ||
Borgatti SP, Carboni I. On measuring individual knowledge in organizations. Organ Res Methods. 2007;10(3):449–462. | ||
Handweker WP, Borgatti SP. Reasoning with numbers. In: Bernard HR, editors. The Handbook of Methods in Cultural Anthropology. Lanham, MD: Altamira Press; 1998:549–593. | ||
Drennan J. Cognitive interviewing: verbal data in the design and pretesting of questionnaires. J Adv Nurs. 2003;42(1):57–63. | ||
Conrad F, Blair J. From impressions to data: increasing the objectivity of congitive interviews. Paper presented at: American Statistical Association 1996; Alexandria, VA, USA. | ||
PharmaQuest [homepage]. Available at: http://www.corptransinc.com/pharmaquest. Accessed January 5, 2017. | ||
Basu N, McClean A, Harper L, et al. Markers for work disability in anti-neutrophil cytoplasmic antibody-associated vasculitis. Rheumatology (Oxford). 2014;53(5):953–956. | ||
Cleanthous S, Newman SP, Shipley M, Isenberg DA, Cano SJ. What constitutes uncertainty in systemic lupus erythematosus and rheumatoid arthritis? Psychol Health. 2013;28(2):171–188. | ||
Cleanthous S, Isenberg DA, Newman SP, Cano SJ. Patient Uncertainty Questionnaire-Rheumatology (PUQ-R): development and validation of a new patient-reported outcome instrument for systemic lupus erythematosus (SLE) and rheumatoid arthritis (RA) in a mixed methods study. Health Qual Life Outcomes. 2016;14:33. | ||
Puechal X, Pagnoux C, Perrodeau E, et al. Long-term outcomes among participants in the WEGENT trial of remission-maintenance therapy for granulomatosis with polyangiitis (Wegener’s) or microscopic polyangiitis. Arthritis Rheumatol. 2016;68(3):690–701. | ||
Wild D, Grove A, Martin M, et al; ISPOR Task Force for Translation and Cultural Adaptation. Principles of good practice for the translation and cultural adaptation process for patient-reported outcomes (PRO) measures: report of the ISPOR task force for translation and cultural adaptation. Value Health. 2005;8(2):94–104. | ||
Ware JE Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. conceptual framework and item selection. Med Care. 1992;30(6):473–483. | ||
Robson JC, Milman N, Tomasson G, et al. Exploration, development, and validation of patient-reported outcomes in antineutrophil cytoplasmic antibody-associated vasculitis using the OMERACT process. J Rheumatol. 2015;42(11):2204–2209. |
Supplementary materials
  | Table S2 Saturation table: domains and subcodes of emergent themes from 50 in-depth individual patient interviews within the US, Canada (CAN), and UK. 0 = theme not present; 1 = theme present |
  | Box S1 Translatability of the questionnaire |
Reference
Conway K, Patrick DL, Gauchon T, Acquadro C. Enhancing crosscultural appropriateness for newly developed patient-reported outcome (PRO) instruments: the use of translatability assessment. In. Patient Reported Outcomes Newsl. 2010;44:9–12. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.