Back to Journals » Infection and Drug Resistance » Volume 15
Health-Related Quality of Life and Associated Factors Among Covid-19 Survivors. Experience from Ethiopian Treatment Centers
Authors Kaso AW , Tesema HG, Hareru HE , Kaso T, Ashuro Z , Talemahu AA, Jore ST, Kassa R, Agero G, Hailu A
Received 17 August 2022
Accepted for publication 13 October 2022
Published 25 October 2022 Volume 2022:15 Pages 6143—6153
DOI https://doi.org/10.2147/IDR.S386566
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Suresh Antony
Abdene Weya Kaso,1 Hailmariam Getachew Tesema,2 Habtamu Endashaw Hareru,1 Taha Kaso,3 Zemachu Ashuro,1 Adugna Asefa Talemahu,4 Soressa Tafere Jore,4 Reta Kassa,1 Gebi Agero,5 Alemayehu Hailu6,7
1School of Public Health, College of Medicine and Health Science, Dilla University, Dilla, Ethiopia; 2Department of Anaesthesiology, College of Medicine and Health Science, Dilla University, Dilla, Ethiopia; 3Department of Surgery, College of Health Science, Arsi University, Asella, Ethiopia; 4School of Medicine, College of Medicine and Health Science, Dilla University, Dilla, Ethiopia; 5Department of Public Health, College of Health Science, Arsi University, Asella, Ethiopia; 6Bergen Centre for Ethics and Priority Setting, Department of Global Public Health and Primary Care, University of Bergen, Bergen, Norway; 7Harvard T.H. Chan School of Public Health, Harvard University, Boston, MA, USA
Correspondence: Abdene Weya Kaso, Email [email protected]
Background: The pandemic of the novel coronavirus (Covid-19), which is extremely stressful and has an adverse effect on people’s health-related quality of life (HRQoL), poses a serious threat to global public health. As a result, this study evaluated the health-related quality of life and associated factors among Covid-19 patients who were discharged from Ethiopian treatment centers.
Methods: We conducted a multi-center, cross-sectional study among 493 Covid-19 survivors who had been discharged from treatment centers between 1st January 2020, and 20th October 2021. We collected respondents’ data using validated Amharic version EuroQol 5-dimensional-5 levels (EQ-5D-5L) questionnaire along with medical records of the patients. Differences in HRQOL scores between patient subgroups were tested by Mann–Whitney U or Kruskal–Wallis test, and the multivariable betaMix regression was used to investigate factors associated with HRQOL scores.
Results: The EQ-5D and VAS median score for Covid-19 survivors was 0.940 (IQR: 0.783– 0.966) and 87 (IQR: 70– 91) respectively. Overall, married individuals, old-aged, individuals who had low educational status, high monthly income, comorbidities, admitted to the Intensive care Unit, received intranasal oxygen care, and prolonged hospitalization had lower utility scores and EQ-VAS scores compared to their counterparts. In multivariate betaMix regression, respondents’ health status at admission, old age, chronic obstructive pulmonary disease, asthma, and hospital length of stay were significantly associated with the lower EQ-5D-Index value and EQ-VAS score.
Conclusion: We found that Covid-19 infection had a persisting impact on the physical and psychosocial health of Covid-19 survivors. Age, having asthma and chronic obstructive pulmonary disease, having a worsening health state upon admission, and a prolonged hospital length of stay were significantly associated with the lower EQ-5D and EQ-VAS score. Therefore, the cost-effective psychological treatment such as cognitive behaviour therapy should be encouraged after hospitalization to improve the post-Covid-19 depression and fatigue.
Keywords: quality of life, Covid-19, Ethiopia
Introduction
Human coronaviruses are enclosed viruses with single-stranded RNA genomes that were first discovered in the 1960s. They can cause mild to severe/crtical upper respiratory tract diseases in susceptible people.1 Covid-19 is a global pandemic caused by the novel coronavirus and it was first reported in China.2 It causes a wide range of clinical manifestations, ranging from mild to severe disease, with a sore throat; dry cough, muscle pain, and high-grade fever were commonly reported signs and symptoms.3,4 Among the Covid-19 patients, 40% had abnormal findings on the chest X-ray, 92% had a fever,53% had a cough, 20% had dysosmia,10% had dysgeusia, and 39.9% had fatigue.5,6 The World Health Organization (WHO) announced the Covid-19 outbreak as a public health emergency of worldwide concern after the virus produced a significant burden of morbidity and mortality in China and other nations.7 After the WHO declared the disease as a public health threat, 281,808,270 confirmed cases and 5,411,759 deaths were reported to WHO until December 29, 2021. Out of this, Ethiopia reported 405,745 confirmed cases of Covid-19 with 6911 deaths to WHO.8 With the pandemic evolving more swiftly to more than 180 countries across all regions, concerns arose that these numbers would even get worse and reach out of control.9 Thus, countries imposed measures such as closing their borders, repatriating, banning mass gatherings and religious celebrations, suspending air travel, obligatory quarantine of suspected individuals, social distancing and hand hygiene as well as lockdown of schools and Universities.10–12 However, the government policies and social exclusion had a considerable impact on the psychological discomfort and physical activities of people, which varies with risk factors, disease severity, and epidemiology.13–16 For instance, social distancing, and lockdowns to control the rapid spread of the Covid-19 pandemic have decreased physical activity levels, increased sedentary behaviour, irregular sleeping pattern, and loss of cardiorespiratory fitness.17–20 Moreover, previous studies found that individuals who survived Covid-19 infection had also a deteriorated HRQoL, particularly in terms of their physical and psychological well-being, which resulted from prolonged hospitalization.21–23 In hospitalized individuals, the mobility, self-care, and usual activity dimensions all showed improvement, but the pain and depression/anxiety domain impairment persisted for another six months.24 For instance, a systematic review of Covid-19 revealed that the proportion of depressive symptoms after 12 weeks following severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection ranges from 11% to 28%.25,26 Several factors such as age, gender, employment status, comorbidities, health status, and socioeconomic factors have been reported to influence HRQoL in Covid-19 infected individuals.27–29
Health-related Quality of life is a multi-dimensional concept that assesses the effects of disease and chronic illnesses on the physical, mental, and social dimensions of health. It is an important tool for medical personnel to understand the patient’s perceptions of their health, the quality of the services they received, and their perception of their illness.30–33 Various tools such as Short form-36(SF-36), COV19-QoL, WHOQOL-BREF, and EQ-5D were used to assess how diseases affected the HRQoL.34–36 The EQ-5D tool was created by the EuroQol group as a straightforward and preference-based tool to characterize and quantify HRQoL based on the patient’s opinion of their health. For many years, EQ-5D-3 levels (EQ-5D-3L) were used to evaluate patients’ HRQoL. However, the EQ-5D-5L was recently designed to evaluate HRQoL due to reduced ceiling effects and good sensitivity.37,38 The five dimensions of health are described in both EQ-5D versions, however, the levels for each dimension vary. Each dimension is measured using three levels in the EQ-5D-3L and five levels in the EQ-5D-5L.39,40 Evaluation of HRQoL across various domains helps to identify the range of factors that affect patients’ well-being.41 It is also important to understand the mostly impaired HRQoL domains after the Covid-19 hospitalization. Besides, evaluation of the HRQoL of patients who survived Covid-19 infection is crucial for developing a variety of health strategies to improve the post-Covid-19 HRQoL. To the best of our knowledge, no research has yet been conducted that generated utility scores for Covid-19 survivors in Ethiopia using EQ-5D-5L. The Ethiopian population tariff has not been used to investigate the Covid-19 effects on HRQoL. As a result, this study evaluated HRQoL and associated factors among Covid-19 survivors who were discharged from Ethiopian treatment facilities.
Method and Material
Study Setting, Design, and Population
We conducted a multicenter, cross-sectional study among 493 Covid-19 survivors who had been discharged from three treatment centers in Ethiopia. We conducted this study at Dilla University hospital, Asella Referral and Teaching hospital (ARTH), and Bokoji primary hospital treatment center. The latter (i.e ARTH and Bokoji primary hospital) were found in Oromia Region whereas the former exists in South Nation, Nationalities Peoples Region. These treatment centers provide Covid-19 services under the treatment and admission protocol of the Federal Ministry of Health of Ethiopia. All patients discharged from these treatment centers between 1st January 2020 and 20th October 2021 were eligible and patients under 18 years old, who had no contact address and were deceased on arrival or during follow-up were excluded.
Sample Size and Sampling Technique
To determine the sample size for a study, we used a single population proportion method and the following assumptions: a 95% confidence level of Z a/2 = 1.96, 5% margin of error, design effect of 1.5, the proportion of problem reported in anxiety/depression dimension of EQ-5D index (p=69%)42 and non-response rate of 10%. Then, we obtained the final sample size calculation of 542. We used multi-stage sampling to recruit the study participants. We purposively selected two zones based on the availability of data and the convenience of the geographical location of the treatment centers. Then, we selected the available treatment centers in these zones using simple random sampling and allocated a sample proportionally to each treatment center based on the number of patients discharged during the study period. Then, based on the medical records of Covid-19 patients, 493 patients were interviewed using systematic random sampling.
Study Variable and Operational Definition
Health-related Quality of Life, the study’s dependent variable, is defined as an individual’s feelings of their well-beingness in terms of satisfaction with significant areas of life. In addition, the independent variables in this study were sociodemographic factors like age, sex, marital status, education level, place of residence, income, and employment status, as well as clinical traits like health status at admission, comorbidities, intravenous oxygen use, and length of hospital stay. We defined patients’ health status at admission according to the updated WHO and the Ethiopian Covid-19 national diagnosis and treatment protocol.43,44 Asymptomatic infections were defined as an absence of clinical signs and symptoms with a positive test for SARS-CoV-2 using a virologic test, whereas mild Covid-19 cases were defined as mild signs and symptoms of Covid-19 without shortness of breath, dyspnea, or abnormal chest imaging. Moderate cases were defined as the presence of clinical signs of pneumonia (fever, cough, dyspnoea, and fast breathing) but without symptoms of severe pneumonia, including SpO2 ≥94% in a room at sea level. Severe disease was defined as the presence of at least one of the following conditions: respiratory distress, a respiratory rate ≥ 30 beats/min, or lung infiltrates >50%.; oxygen saturation in resting-state ≤ 94%; or an arterial partial pressure of oxygen to fraction of inspired oxygen (PaO2/FiO2) ≤ 300 mmHg. Critically ill was defined as individuals who have respiratory failure, septic shock, and/or multiple organ dysfunction.
Data Collection Procedure and Quality Management
We completed the EQ-5D-5L questionnaire, along with socio-demographic characteristics for patients discharged from treatment centers using telephone interviews. Clinical data such as comorbidities, status at admission, site of care, length of hospitalization, and type of supportive care received were extracted from the medical records of patients using a data abstraction form. We provided two days of training and two health experts collected data from individuals discharged from each treatment center. The principal investigator supervised and cross-checked data for completeness on daily basis.
Health-Related Quality of Life
We collected the HRQoL information of the study participants using the validated Amharic version of the EQ-5D-5L questionnaire. The EQ-5D contains five domains: Mobility, Self-Care, Usual Activities, Pain/Discomfort, and Anxiety/Depression. For each domains, there were five levels to describe the severity, namely, have no problems, have slight problems, have moderate problem, have severe problems, and have extreme problems, which could describe 3125 possible health combinations. The predicted values for the EQ-5D-5L ranged from −0.718(worst possible health) to 1(best possible health).45 EQ-5D also contains the descriptive system known as EQ Visual analogue scale [EQ-VAS]), which asks the respondents to rate their health status from the best health state(score of 100) to the worst health state (score of 0). We converted the HRQoL measured by EQ-5D to a single utility score using value set for the Ethiopian population.45
Data Analysis
Data were imported into STATA version 16 from MS Excel 2010 for analysis. We computed descriptive statistics as appropriate depending on the nature of the data. Interquartile range (IQR) and median were used to summarize continuous variables, while frequencies and percentages were computed for categorical variables. The Shapiro–Wilk test, multicollinearity, and heteroscedasticity assumption were statistically assessed on the HRQoL utility scores (index values) and EQ-VAS scores. We found data is not normally distributed using the Shapiro–Wilk test and the Kruskal–Wallis test or Mann–Whitney U-test was used to ascertain the variations in EQ-5D index score and EQ-VAS score by patient characteristics. The health utility data is typically skewed, multimodal, truncated, and frequently has a significant number of observations at the top, making the employment of fundamental models like ordinary least squares and Tobit theoretically problematic for the analysis of such data. However, betaMix regression models offer a flexible way of modeling skewed, multimodal, and truncated distribution of EQ-5D data.46 Therefore, we used the multivariable betaMix regression analysis model to identify the determinants of the HRQoL score and VAS score, and a p-value of < 0.05 was considered statistically significant.
Ethical Approval and Consent to Participate
We conducted this study in accordance with the Declaration of Helsinki. We secured the Ethical approval from the Institutional Review Board of Dilla University College of Health Sciences and Medicine. Verbal informed consent to participate was approved by the ethical committee since the period was in the 2nd Covid-19 wave and impossible for written consent. We also obtained permission from the administration of the treatment center to access the patient medical records. Participants have informed of the purpose of the study and the right to decline to participate in the interview. Moreover, no personal identifier was used, and all data gathered was kept private and only used for the study.
Result
Socio-Demographic Characteristics of Respondents and EQ-5D Index and EQ-5D-VAS Scores
A total of 493 individuals were interviewed making the response rate around 91%. Of the 493 respondents included in the studies, more than two-fifths (42.6%) were in the age group between 31–45 years, and the majority (64.9%) were male. Furthermore, about two-thirds (64.5%) of the participants were from urban, 70.8% were married, and 45.8% had primary education. Nearly half (47.9%) of the participants had a monthly income between 1000 and 2000 ETB (Ethiopian birr). We found the median EQ-5D index value for all respondents was 0.940 (IQR: 0.783, 0.966), and the median EQ-VAS was 87 (IQR: 70, 91). The median HRQoL score was lower in individuals aged > 59 years old (p = 0.001); those who were married(p = 0.001) and had informal education (p = 0.001). In addition, the median HRQoL score was lower in individuals who were farmers (p= 0.001), and who had high monthly income (p = 0.001). The EQ-VAS score also obtained similar results as that of the EQ-5D index score (Table 1).
 |
Table 1 Difference in EQ-5D and EQ-VAS Score by Sociodemographic Characteristics of Respondents Discharged from Covid-19 Treatment Centers in Ethiopia, 2020–2021 |
Clinical Characteristics of Respondents and EQ-5D Index and EQ-5D-VAS Scores
Nearly a third (30.6%) of the 493 Covid-19 patients interviewed had chronic conditions, and nearly a fourth (25.2%) had diabetes. When they were admitted to treatment facilities, nearly three-fourths (74%) of the participants were clinically classified as moderate, severe, or critical. With a median length of stay (LOS) of 15 days, more than half (52.1%) of participants stayed at the treatment facility for at least 15 days (IQR: 13–19). Intranasal oxygen supplementation was given to about three-fourths of the respondents (74%) and mechanical ventilation supportive treatment was used by 20% of participants who were admitted to the intensive care unit (ICU). We found that patients with chronic illnesses such as hypertension, chronic Cardiac disease, Chronic obstructive Pulmonary Disease (COPD), Asthma, Diabetic Mellitus, Chronic Kidney Disease (CKD), malignance, and HIV/AIDS had significantly lower median EQ-5D scores compared to their counterpart. In addition, individuals with severe/critical and moderate health status at admission, admitted to both ward and ICU or ICU only, received intranasal oxygen supplementation, and stayed 15 days and above in the hospital had lower median EQ-5D score (p<0.001). Similarly, VAS scores also obtained similar findings as that of the EQ-5D index score (Table 2).
 |
Table 2 Clinical Characteristics of Covid-19 Patients Discharged from Treatment Centers in Ethiopia, 2020–2021 |
Distribution of the EQ-5D-5L Dimensions
The distributions of HRQoL problems that participants reported for each EQ-5D index dimension were shown in Figure 1. The proportion of individuals who reported problems with mobility, self-care, routine activities, pain/discomfort, and anxiety/depression aspects was 40.4%, 40.6%, 49.1%, and 54.6%, respectively.
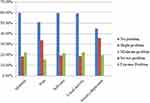 |
Figure 1 Distribution of the EQ-5D-5L dimensions among Covid-19 patients discharged from 2020–2021 in Ethiopia. |
Multivariable BetaMix Regression Model for EQ- 5D Index and EQ- 5D VAS Scores
We used multivariable betaMix regression analysis to assess the relationship between socio-demographic and clinical characteristics to predict the determinants of EQ- 5D Index and EQ- 5D VAS scores. We found that older age, being in worsening condition during admission, having COPD, asthma, and prolonged hospitalization had significant negative effects on both the EQ-5D-5L index and EQ-5D-VAS score (p < 0.05).In addition, individuals who had malignancy had lower EQ-5D-VAS scores compared to those who were without malignancy(p < 0.029) (Table 3).
 |
Table 3 Multivariate BetaMix Regression Analysis for Factors Associated with EQ-5D-Index of Covid-19 Survivors Discharged from Treatment Centers in Ethiopia, 2020–2021 |
Discussion
The Covid-19 pandemic is a threat to global public health, causing significant stress and affecting the HRQoL of the survived patients.41,47 This study used the EQ-5D-5L tool to measure the HRQoL of Covid-19 survivors and the effect of sociodemographic and clinical variables on HRQoL. In our study, the median EQ-5D-5L score for Covid-19 survivors was 0.940. This finding is supported by the finding from Vietname, 0.95,17 China, 0.949,48 and greater than the study conducted in Vietnam,0.66,49 Hong Kong, 0.897,50 Norway, 0.82,51 Iran, 0.6125,52 and Palestine, 0.65.53 The observed discrepancy was might be due to the difference in tariff value used, method of measurement, study period, study population, and comorbidities. In our study, pain/discomfort (49.1%) and anxiety/depression (54.6%) were the two commonly impaired dimensions of EQ-5D. Our findings are consistent with previous studies, which found a higher burden of psychological distress and fatigue among Covid-19 survivors.48,52,54,55 This might be due to the fact that Covid-19 survivors have anxiety/depression which is linked to worry about future careers, feelings of job insecurity, loneliness and isolation, concerns about family members, social stigma and discrimination, and workplace discrimination.56–59 The high prevalence of anxiety/depression and fatigue among Covid-19 survivors highlighted the need for using the cost-effective psychological interventions such as cognitive behaviour therapy [CBT] that have the potential of combating anxiety/depression to improve the post- Covid-19 trauma.60–62
We found that the older age Covid-19 survivors had lower scores of HRQoL compared with the younger individuals. This is supported by previous studies that found a decreased EQ-5D score with increasing age of Covid-19 patients.48,52,53,63 This might be due to psychological stress as a result of news about Covid-19, increased comorbidity, and deterioration of the physical condition of older people.64,65 The associations between lower HRQoL and prolonged hospitalization, as well as health status at admission in our study, were also consistent with the previous studies.23,63,66,67 This could be due to respondents who have worsened health status during admission had a long duration of treatment and developing psychological stress due to prolonged social exclusion and confinement in the treatment center.22–24,66–69 The association between prolonged stay on treatment and the lower HRQoL among individuals who survived Covid-19 infection, highlights the need for implementing post-Covid-19 psychological therapy that has the potential of combating anxiety/depression that persists for six months.60–62
The current study revealed a significantly lower HRQoL in individuals with comorbidities such as COPD, Asthma, Diabetic Mellitus, HIV/AIDS, malignance, CKD, and hypertension compared to their counterparts. In addition, the associations between lower HRQoL and comorbidities such as COPD, malignancy, and asthma(p<0.05), were also consistent with previous studies on Covid-19.23,41,53,55,63,70,71 This could be due to respondents who had underlying diseases might be worried about reinfection after being discharged and avoiding both urgent or emergency and routine medical care that improves their health status.72 This study has several strengths and added value to the current scientific research. We believe that this is the first study that used the EQ-5D-5L in an Ethiopian setting to determine the utility value for Covid-19 survivors. It can therefore be used for the economic evaluation analyses of Covid-19 strategies. Additionally, the study was carried out in a multi-center context and can be generalized to a similar setting in Ethiopia. However, our study is not free from limitations. As we collected the HRQoL data from participants’ self-reported preferences, the respondents might overestimate or underestimated their real health status. In addition, since there is a significant rate of anxiety and depression reported in non-Covid-19 patients, we cannot indicate whether the reductions in HRQOL in our study are differentially worse than those without Covid-19.
Conclusion
We found that Covid-19 infection had a persisting impact on the physical and psychosocial health of Covid-19 survivors. Age, having asthma and COPD, having a worsening health state upon admission, and a prolonged hospital length of stay were significantly associated with the lower EQ-5D and EQ-VAS scores. Therefore, cost-effective psychological therapy such as CBT should be encouraged after hospitalization to improve post-Covid-19 depression and fatigue.
Abbreviations
AIDS, Acquired Immune Deficiency Syndrome; ARTH: Asella Referral and Teaching Hospital, CFR, Case Fatality Rate; CI, Confidence Interval; CKD, Chronic Kidney Disease; COPD, Chronic Pulmonary Disease; EQ-5D-3L, Euro Qol −5-Dimension −3 Level; EQ-5D-5L, Euro Qol −5-Dimension −5 Level; HRQoL, Health-Related Quality of Life; HIV, Human Immune Virus; LMIC, Low and Medium-Income Countries; ICU, Intensive Care Unit; RNA, Ribonueclotide Acid; SD, Standard Deviation; VAS, Visual Analogous Scale; WHO, World Health Organization.
Data Sharing Statement
The datasets supporting the conclusions of this article were available from the corresponding author upon reasonable request.
Acknowledgments
The authors acknowledge Bokoji hospital, Asella Referral and Teaching hospital, and Dilla University Referral Hospital administration administrations and staff for their support during data collection. We express our grateful appreciation to Mr Angasa Demissie and Mr Mengesha Moges for their support during data collection.
Funding
The author(s) received no specific funding for this work.
Disclosure
The authors declare that they have no competing interests in this work.
References
1. De Groot Raoul J, Christian D, Chris L, et al. The species Severe acute respiratory syndrome-related coronavirus: classifying 2019-nCoV and naming it SARS-CoV-2. Nat Microbiol. 2020;5(4):536–544.
2. Park SE. Epidemiology, virology, and clinical features of severe acute respiratory syndrome-coronavirus-2 (SARS-CoV-2; Coronavirus Disease-19). Clin Exp Pediatr. 2020;63(4):119. doi:10.3345/cep.2020.00493
3. Madahar P, Wunsch H, Jha P, Slutsky AS, Brodie D. Trends in COVID-19-related in-hospital mortality: lessons learned from nationwide samples. Lancet Respir Med. 2021;9(4):322–324. doi:10.1016/S2213-2600(21)00080-1
4. Brehm TT, van der Meirschen M, Hennigs A, et al. Comparison of clinical characteristics and disease outcome of COVID-19 and seasonal influenza. Sci Rep. 2021;11(1):1–10. doi:10.1038/s41598-021-85081-0
5. Wang L, He W, Yu X, et al. Coronavirus disease 2019 in elderly patients: characteristics and prognostic factors based on 4-week follow-up. J Infect. 2020;80:639–645. doi:10.1016/j.jinf.2020.03.019
6. Hao F, Tam W, Hu X, et al. A quantitative and qualitative study on the neuropsychiatric sequelae of acutely ill COVID-19 inpatients in isolation facilities. Transl Psychiatry. 2020;10(1):1–14. doi:10.1038/s41398-020-01039-2
7. World Health Organization. WHO Director-General’s opening remarks at the media briefing on COVID-19. Geneva, Switzerland; 2020. Available from: https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-The-media-briefing-on-covid-19---11-march-2020.
8. World Health Organization. WHO Coronavirus (COVID-19) Dashboard. Geneva: World Health Organization; 2021.
9. ASSESSMENT RR. Outbreak of Acute Respiratory Syndrome Associated with a Novel Coronavirus, China; First Cases Imported in the EU/EEA; Second Update. Rapid Risk Assess; 2020.
10. Matovu JK, Kabwama SN, Ssekamatte T, Ssenkusu J, Wanyenze RK. COVID-19 awareness, adoption of COVID-19 preventive measures, and effects of COVID-19 lockdown among adolescent boys and young men in Kampala, Uganda. J Community Health. 2021;46(4):842–853. doi:10.1007/s10900-021-00961-w
11. Galvin CJ, Li Y-CJ, Malwade S, Syed-Abdul SCOVID-19. preventive measures showing an unintended decline in infectious diseases in Taiwan. Int J Infect Dis. 2020;98:18–20. doi:10.1016/j.ijid.2020.06.062
12. Güner HR, Hasanoğlu İ, Aktaş F. COVID-19: prevention and control measures in community. Turk J Med Sci. 2020;50(9):571–577. doi:10.3906/sag-2004-146
13. Zhang WR, Wang K, Yin L, et al. Mental health and psychosocial problems of medical health workers during the COVID-19 epidemic in China. Psychother Psychosom. 2020;89(4):242–250. doi:10.1159/000507639
14. Chou R, Dana T, Buckley DI, Selph S, Fu R, Totten AM. Epidemiology of and risk factors for coronavirus infection in health care workers: a living rapid review. Ann Intern Med. 2020;173(2):120–136. doi:10.7326/M20-1632
15. Suryavanshi N, Kadam A, Dhumal G, et al. Mental health and quality of life among healthcare professionals during the COVID‐19 pandemic in India. Brain Behav. 2020;10(11):e01837. doi:10.1002/brb3.1837
16. Kurnik-łucka M, Pasieka P, Górecka-Mazur A, Rząsa-Duran E, Pękala J, Gil K Health-related quality of life of pharmacists in the pre-COVID-19 era; 2020.
17. Tran BX, Nguyen HT, Le HT, et al. Impact of COVID-19 on economic well-being and quality of life of the Vietnamese during the national social distancing. Front Psychol. 2020;11:565153. doi:10.3389/fpsyg.2020.565153
18. Gjaka M, Feka K, Bianco A, et al. The effect of COVID-19 lockdown measures on physical activity levels and sedentary behaviour in a relatively young population living in Kosovo. J Clin Med. 2021;10(4):763. doi:10.3390/jcm10040763
19. Di Stefano V, Ornello R, Gagliardo A, et al. Social distancing in chronic migraine during the COVID-19 outbreak: results from a multicenter observational study. Nutrients. 2021;13(4):1361. doi:10.3390/nu13041361
20. Wang G, Zhang Y, Zhao J, Zhang J, Jiang F. Mitigate the effects of home confinement on children during the COVID-19 outbreak. Lancet. 2020;395(10228):945–947. doi:10.1016/S0140-6736(20)30547-X
21. Ceban F, Nogo D, Carvalho IP, et al. Association between mood disorders and risk of COVID-19 infection, hospitalization, and death: a systematic review and meta-analysis. JAMA psychiatry. 2021;78(10):1079–1091. doi:10.1001/jamapsychiatry.2021.1818
22. Qu G, Zhen Q, Wang W, et al. Health‐related quality of life of COVID‐19 patients after discharge: a multicenter follow‐up study. J Clin Nurs. 2021;30(11–12):1742–1750.q doi:10.1111/jocn.15733
23. Chen K-Y, Li T, Gong F-H, Zhang J-S, Li X-K. Predictors of health-related quality of life and influencing factors for COVID-19 patients, a follow-up at one month. Front Psychiatry. 2020;11:668. doi:10.3389/fpsyt.2020.00668
24. Carenzo L, Protti A, Corte FD, et al. Short‑term health‑related quality of life, physical function and psychological consequences of severe COVID‑19. Ann Intensive Care. 2021;11:91. doi:10.1186/s13613-021-00881-x
25. Renaud-Charest O, Lui LM, Eskander S, et al. Onset and frequency of depression in post-COVID-19 syndrome: a systematic review. J Psychiatr Res. 2021;144:129–137. doi:10.1016/j.jpsychires.2021.09.054
26. Ceban F, Ling S, Lui LM, et al. Fatigue and cognitive impairment in Post-COVID-19 Syndrome: a systematic review and meta-analysis. Brain Behav Immun. 2022;101:93–135. doi:10.1016/j.bbi.2021.12.020
27. Khan AG, Kamruzzaman M, Rahman MN, Mahmood M, Uddin MA. Quality of life in the COVID-19 outbreak: influence of psychological distress, government strategies, social distancing, and emotional recovery. Heliyon. 2021;7(3):e06407. doi:10.1016/j.heliyon.2021.e06407
28. Hawlader MDH, Rashid MU, Khan MAS, et al. Quality of life of COVID-19 recovered patients in Bangladesh. PLoS One. 2021;16(10):e0257421. doi:10.1371/journal.pone.0257421
29. Islam MS, Rahman ME, Al Zubayer A, et al. Investigating poor sleep quality and associated factors during the covid-19 pandemic: a population-based survey in Bangladesh. Public Health Front. 2021;9. doi:10.3389/fpubh.2021.724520
30. Stenman U, Hakama M, Knekt P, et al. Measurement and modeling of health-related quality of life. Epidem Demog Public Health. 2010;195:130–135.
31. Aaronson N, Alonso J, Burnam A, et al. Assessing health status and quality-of-life instruments: attributes and review criteria. Qual Life Res. 2002;11(3):193–205. doi:10.1023/A:1015291021312
32. Prevention CfDCa. Measuring Healthy Days Population Assessment of Health-Related Quality of Life. Atlanta, Georgia: Prevention CfDCa; 2000.
33. Alzoubi EE, Hariri R, Nj A. Oral health related quality of life impact in dentistry. J Dent Health Oral Disord Ther. 2017;6(6). doi:10.15406/jdhodt.2017.06.00221
34. Repišti S, Jovanović N, Kuzman MR, et al. How to measure the impact of the COVID-19 pandemic on quality of life: COV19-QoL –the development, reliability and validity of a new scale. Global Psychiatry. 2020;3(2):1–10.
35. Coons SJ, Rao S, Keininger DL, Hays RD. A comparative review of generic quality-of-life instruments. Pharmacoeconomics. 2000;17(1):13–35. doi:10.2165/00019053-200017010-00002
36. Ferrans CE. Differences in what quality-of-life instruments measure. J Natl Cancer Inst Monogr. 2007;2007(37):22–26. doi:10.1093/jncimonographs/lgm008
37. Herdman M, Gudex C, Lloyd A, et al. Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Qual Life Res. 2011;20(10):1727–1736. doi:10.1007/s11136-011-9903-x
38. Kreimeier S, Oppe M, Ramos-Goñi JM, et al. Valuation of EuroQol five-dimensional questionnaire, youth version (EQ-5D-Y) and EuroQol five-dimensional questionnaire, three-level version (EQ-5D-3L) health states: the impact of wording and perspective. Value Health. 2018;21(11):1291–1298. doi:10.1016/j.jval.2018.05.002
39. Buchholz I, Janssen MF, Kohlmann T, Feng Y-S. A systematic review of studies comparing the measurement properties of the three-level and five-level versions of the EQ-5D. Pharmacoeconomics. 2018;36(6):645–661. doi:10.1007/s40273-018-0642-5
40. Janssen M, Pickard AS, Golicki D, et al. Measurement properties of the EQ-5D-5L compared to the EQ-5D-3L across eight patient groups: a multi-country study. Qual Life Res. 2013;22(7):1717–1727. doi:10.1007/s11136-012-0322-4
41. Algahtani FD, Hassan SU, Alsaif B, Zrieq R. Assessment of the quality of life during COVID-19 pandemic: a cross-sectional survey from the Kingdom of Saudi Arabia. Int J Environ Res Public Health. 2021;18(3):847. doi:10.3390/ijerph18030847
42. Shah R, Ali FM, Nixon SJ, Ingram JR, Salek SM, Finlay AY. Measuring the impact of COVID-19 on the quality of life of the survivors, partners and family members: a cross-sectional international online survey. BMJ Open. 2021;11(5):e047680. doi:10.1136/bmjopen-2020-047680
43. World Health Organization. Clinical Management of COVID-19: Interim Guidance. World Health Organizatio; 2020.
44. FMOH. National Guideline for Integration of Covid-19 and Essential Healthcare Services. Addis Ababa, Ethiopia: FMOH; 2021.
45. Welie AG, Gebretekle GB, Stolk E, et al. Valuing health state: an EQ-5D-5L value set for Ethiopians. Value Health Reg Issues. 2020;22:7–14. doi:10.1016/j.vhri.2019.08.475
46. Grün B, Kosmidis I, Zeileis A Extended beta regression in R: shaken, stirred, mixed, and partitioned. Working Papers in Economics and Statistics; 2011.
47. Greco F, Altieri VM, Esperto F, Mirone V, Scarpa RM. Impact of COVID-19 pandemic on health-related quality of life in uro-oncologic patients: what should we wait for? Clin Genitourin Cancer. 2021;19(2):e63–e68. doi:10.1016/j.clgc.2020.07.008
48. Ping W, Zheng J, Niu X, et al. Evaluation of health-related quality of life using EQ-5D in China during the COVID-19 pandemic. PLoS One. 2020;15(6):e0234850. doi:10.1371/journal.pone.0234850
49. Ngo CQ, Phan PT, Vu GV, et al. Effects of different comorbidities on health-related quality of life among respiratory patients in Vietnam. J Clin Med. 2019;8:214. doi:10.3390/jcm8020214
50. Wong EL, HoID K, Wong SY, et al. Views on workplace policies and its impact on health-related quality of life during coronavirus disease (COVID-19) pandemic: cross-sectional survey of employees. Int J Health Policy Manag. 2020;1(1):1–10.
51. Garratt AM, Ghanima WG, Einvik G. Quality of life after COVID-19 without hospitalisation: good overall, but reduced in some dimensions. J Infect. 2021;8:38.
52. Arab-Zozani M, Hashemi F, Safari H, Yousefi M, Ameri H. Health-related quality of life and its associated factors in COVID-19 patients. Osong Public Health Res Perspect. 2020;11(5):296–302. doi:10.24171/j.phrp.2020.11.5.05
53. Hamdan A, Ghanim MRM, Mosleh R. COVID-19 confinement and related well being measurement using the EQ-5D questionnaire: a survey among the Palestinian population. Int J Clin Pract. 2021;75(10). doi:10.1111/ijcp.14621
54. Busico M, Intile D, Sívori M, et al. Risk factors for worsened quality of life in patients on mechanical ventilation. prospec Multicent study Med Intensiva. 2016;40(7):422–430. doi:10.1016/j.medin.2016.01.002
55. Shimels T, Kassu RA, Bogale G, et al. Health related quality of life of patients with chronic non-communicable diseases during the coronavirus pandemic in Ethiopia: a multi-facility study; 2020.
56. Rajabimajd N, Alimoradi Z, Griffiths MD. Impact of COVID-19-related fear and anxiety on job attributes: a systematic review. Asian J Soc Psychol. 2021;4(2):51. doi:10.4103/shb.shb_24_21
57. Patil ST, Datar MC, Shetty JV, Naphade NM. “Psychological consequences and coping strategies of patients undergoing treatment for COVID-19 at a tertiary care hospital”: a qualitative study. Asian J Soc Psychol. 2021;4(2):62. doi:10.4103/shb.shb_5_21
58. Alimoradi Z, Ohayon MM, Griffiths MD, Lin C-Y, Pakpour AH. Fear of COVID-19 and its association with mental health-related factors: systematic review and meta-analysis. BJPsych Open. 2022;8(2):2. doi:10.1192/bjo.2022.26
59. Sangma RD, Kumar P, Nerli LM, Khanna AM, Vasavada DA, Tiwari DS. Social stigma and discrimination in Coronavirus Disease-2019 survivors and its changing trend: a longitudinal study at tertiary care center Gujarat, India. Asian J Soc Psychol. 2022;5(2):68. doi:10.4103/shb.shb_12_22
60. Ho CS, Chee CY, Ho RC. Mental health strategies to combat the psychological impact of COVID-19 beyond paranoia and panic. Ann Acad Med Singapore. 2020;49(1):1–3.
61. Zhang MW, Moodle: HR. The cost effective solution for internet cognitive behavioral therapy (I-CBT) interventions. Technol Health Care. 2017;25(1):163–165. doi:10.3233/THC-161261
62. Soh HL, Ho RC, Ho CS, Tam WW. Efficacy of digital cognitive behavioural therapy for insomnia: a meta-analysis of randomised controlled trials. Sleep Med. 2020;75:315–325. doi:10.1016/j.sleep.2020.08.020
63. Kaso A, Agero G, Hurisa Z, Kaso T, Ewune HA, Hailu A. Evaluation of health-related quality of life of covid-19 patients: a hospital-based study in South Central Ethiopia. Health Qual Life Outcomes. 2021;19(1):1. doi:10.1186/s12955-021-01900-y
64. Li Y-P, Lin C-Y, Kuo Y-J, Chen Y-P, Griffiths MD. Gender differences in the factors associated with the fear of COVID-19 among Taiwanese older people. INQUIRY. 2021;58:00469580211055587.
65. Mistry SK, Ali A, Akther F, Yadav UN, Harris MF. Exploring fear of COVID-19 and its correlates among older adults in Bangladesh. Global Health. 2021;17(1):1–9. doi:10.1186/s12992-021-00698-0
66. Qi M, Li P, Moyle W, Weeks B, Jones C. Physical activity, health-related quality of life, and stress among the Chinese adult population during the COVID-19 pandemic. Int J Environ Res Public Health. 2020;17(18):6494. doi:10.3390/ijerph17186494
67. Taboada M, Moreno E, Cariñena A, et al. Quality of life, functional status, and persistent symptoms after intensive care of COVID-19 patients. Br J Anaesth. 2021;126(3):e110–e113. doi:10.1016/j.bja.2020.12.007
68. Temperoni C, Grieco S, Pasquini Z, et al. Clinical characteristics, management and health related quality of life in young to middle age adults with COVID-19. BMC Infect Dis. 2021;21(1):1–10. doi:10.1186/s12879-021-05841-1
69. Tsuzuki S, Miyazato Y, Terada M, Morioka S, Ohmagari N, Beutels P. Impact of long-COVID on health-related quality of life in Japanese COVID-19 patients. Health Qual Life Outcomes. 2022;20(1):1–9. doi:10.1186/s12955-022-02033-6
70. Nguyen HC, Nguyen MH, Do BN, et al. People with suspected COVID-19 symptoms were more likely depressed and had lower health-related quality of life: the potential benefit of health literacy. J Clin Med. 2020;9:965. doi:10.3390/jcm9040965
71. Samlani Z, Lemfadli Y, Ait Errami A, Oubaha SKK, Krati K. The impact of the COVID-19 pandemic on quality of life and well-being in Morocco. Community Med Public Health. 2020;6(2):130–134. doi:10.17352/2455-5479.000091
72. Czeisler MÉ, Marynak K, Clarke KE, et al. Delay or avoidance of medical care because of COVID-19–related concerns—United States, June 2020. Morb Mortal Wkly Rep. 2020;69(36):1250. doi:10.15585/mmwr.mm6936a4
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
