Back to Journals » Patient Related Outcome Measures » Volume 12
Health-Related Quality of Life Among Heart Failure Patients Attending an Outpatient Clinic in the University of Gondar Comprehensive Specialized Hospital Northwest, Ethiopia, 2020: Using Structural Equation Modeling Approach
Authors Ewnetu Tarekegn G , Derseh Gezie L , Yemanu Birhan T, Ewnetu F
Received 29 May 2021
Accepted for publication 19 August 2021
Published 28 August 2021 Volume 2021:12 Pages 279—290
DOI https://doi.org/10.2147/PROM.S322421
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Robert Howland
Gebrekidan Ewnetu Tarekegn,1 Lemma Derseh Gezie,1 Tilahun Yemanu Birhan,1 Frew Ewnetu2
1Department of Epidemiology and Biostatistics, Institute of Public Health, College of Medicine and Health Sciences, University of Gondar, Gondar, Ethiopia; 2Department of Internal Medicine, School of Medicine, College of Medicine and Health Sciences, University of Gondar, Gondar, Ethiopia
Correspondence: Gebrekidan Ewnetu Tarekegn
Department of Epidemiology and Biostatistics, Institute of Public Health, College of Medicine and Health Sciences, University of Gondar, P.O.BOX: 196, Gondar, Ethiopia
Tel +251930781289
Email [email protected]
Background: Chronic heart failure is one of the most important public health concerns in the industrialized and developing world having increasing prevalence. Measuring quality of life using rigorous statistical methods may be helpful to provide input for decision-makers and the development of guidelines. This study aimed to assess health-related quality of life and associated factors among heart failure patients attending the University of Gondar Specialized Hospital.
Methods: A cross-sectional study was employed to select 469 heart failure patients who have follow-up at the University of Gondar Specialized Hospital consecutively from March 01 to 30, 2020. Data were entered to Epi Info 7 and exported to STATA version 15 for further statistical analysis. The quality-of-life domains were measured with World Health Organization Quality of Life BREF. Structural equation modeling was employed to estimate the relationships among exogenous, mediating, and endogenous variables simultaneously.
Results: Chronic heart failure patients had a significantly lower mean score in physical health domain (31.70 mean score), environmental health domain (38.35 mean score), and in overall quality of life domain (41.61 mean score) moderate in social relation domain (46.22 mean score), and in psychological health domain (50.21 mean score) of health-related quality of life (p-value < 0.0001). Age had a direct positive effect on health-related quality of life. Residency also had a direct negative effect on both physical and environmental health-related quality of life domain. Duration of heart failure had a direct negative effect on psychological health.
Conclusion: The finding of this study indicated that poor health-related quality of life in the physical health domain, moderately poor in overall health-related quality of life, and moderate health-related quality of life in the psychological health domain among Chronic heart failure patients. Age, residence, marital status, income, and duration of HF were significantly associated factors for quality of life among HF patients.
Keywords: health-related quality of life, heart failure, structural equation model, Ethiopia
Background
Heart failure is a global public health problem that affects more than 26 million people worldwide and 550,000 new cases are diagnosed each year.1,2 Heart failure is a serious condition, and usually, there is no cure. But many people with heart failure lead a full, enjoyable life when the condition is managed with heart failure medications and healthy lifestyle changes.3
The World Health Organization defines the quality of life as individual’s perception of their position in life in the context of the culture and value systems in which they live and concerning their goals, expectations, standards, and concerns. It is a broad-ranging concept affected in a complex way by the person’s physical health, psychological state, social relationships, and their relationship to salient features of the environment.4
World Health Statistics in 2012 showed that CHF has created an economic burden of 108 billion dollars in the health system.5 Different physical and mental complications such as fatigue, depression, anxiety, edema, shortness of breath due to the chronic and prolonged disease course, and therapeutic processes have a serious and negative impact on the quality of life (QOL).5,6 Lower HRQOLs correlate with increased hospitalization occupancy and mortality rates, and higher costs imposed on health systems, families, and patients.7–9
Health-related quality of life is influenced by numerous physical, emotional, and social factors and is uniquely perceived by each individual. The structured assessment of HRQOL is considered important in promoting patient-centric care. It puts the patient’s perspective at the forefront and can identify areas of specific need. This helps to facilitate shared decision-making and ensure that the preferences of the patient are used to guide management.4
Health-related quality of life is a broad and multidimensional concept that subjectively evaluates the physical, psychological, and social health status of individuals and is influenced by their understanding, experiences, and expectations,10 but most previous studies on health-related quality of life were considered as observed variable but HRQOL is a multidimensional concept that is better evaluated by several latent constructs.
Analysis of HRQOL can identify groups with poor HRQOL, and this could guide interventions that will improve their situation and avert more serious consequences, allocate limited resources based on unmet needs, guide strategic plan, and monitor the intervention given. Moreover, limited studies were conducted on health-related quality of life among heart failure patients in Africa specifically in Ethiopia.
In response to these identified gaps, we conducted a study with appropriate statistical analysis (multivariate statistical analysis). The main objectives of the study were 1) to determine health-related quality of life and associated factors among heart failure patients, and 2) to examine the association among socio-demographic and economic, clinical related variables, and among the domain of HRQOL variables. To account for the interdependency of various factors and health-related variables, structural equation modeling was employed.
Methods and Material
Study Setting and Period
An institution-based cross-sectional study was employed at the University of Gondar comprehensive specialized hospital (UoGCSH) to take a snapshot of the population of adult heart failure patients from March 01 to 30, 2020. The Gondar city is 727 km northwest of the capital city of the country, Addis Ababa. UoGCSH is located in the center of Gondar city. Currently, the hospital has a catchment population of about 7 million serving as a referral hospital for nearby hospitals. The hospital runs several medical outpatient services including a heart failure follow-up clinic.
Population
Patients diagnosed with CHF who have to follow-up for at least 6 months and age greater than 18 years who had visited UoGCSH during the study period were selected as study participants. Chronic heart failure patients are diagnosed using Framingham criteria, for which patients should have at least one major criteria like paroxysmal nocturnal dyspnea (PND) or at least two minor criteria like hepatomegaly.11 Patients were excluded from the study if they experienced a concurrent diagnosis of other life-threatening diseases (eg, cancer).
Sample Size Determination
Following the practical recommendation on sample size for structural equation modeling a 5:1 ratio of a sample size to the number of free parameters. The total number of elements in the initial covariance matrix is  , where K equals the number of observed variables in the matrix.12 In this case, the total number of parameters is (26×27)/2 = 351. The parameters that have to be estimated in the model contain 26 observed variable variances, 21 loadings, 5 latent variable variances, 27 regression coefficients, and 6 latent variable covariances, which results in 85 free parameters. Therefore, the minimum sample size required for this study was equaled to 5×85 = (425). Then adding a 10% non-response rate, the sample size became 468.
, where K equals the number of observed variables in the matrix.12 In this case, the total number of parameters is (26×27)/2 = 351. The parameters that have to be estimated in the model contain 26 observed variable variances, 21 loadings, 5 latent variable variances, 27 regression coefficients, and 6 latent variable covariances, which results in 85 free parameters. Therefore, the minimum sample size required for this study was equaled to 5×85 = (425). Then adding a 10% non-response rate, the sample size became 468.
Sampling Technique and Procedures
Most patients in the follow-up clinic have one follow-up per month, and the required sample was taken by enumerating all patients during the study period (from March 01 to 30, 2020) consecutively until the required sample size was secured.
Variables and Measurement
Data were collected with face-to-face interviews using structured questionnaires. The questionnaire consists of socio-demographic characteristics, clinical related questions, and the WHO-QOL tool. Data related to underlying causes of HF and medication regimen were obtained by reviewing the chart, and variables like age, sex, duration of disease, marital status, educational status, occupation, monthly income, enrolment in community-based health insurance, and lastly all 26 items variables were obtained by interviewer-administered face-to-face interview.
The health-related quality measurement domain questionnaire was adopted from WHOQOL, which is also validated in Ethiopia and other parts of the countries in the world.13 It has four domains that denote an individual’s perception of quality of life in each particular domain. The WHOQOL-BREF is a 26-item instrument consisting of four domains: physical health domain (7 items), psychological health domain (6 items), social relation domain (3 items), and environmental health domain (8 items); it also contains the overall perception of QOL and general health (2 items).
Initially, a questionnaire was prepared in the English version, then translated into Amharic (local language) and translated back into English by another person to check the consistency.
Data Processing, Model Building, and Analysis
The filled questionnaires were checked manually for completeness. Data were coded and entered into Epi Info version 7, and then exported to STATA version 15 for further analysis. Descriptive and summary statistics were done using figures and tables. Reliability was also be assessed for each domain of WHOQOL-BREF using the Cronbach’s α coefficient and values of 0.7 or higher were considered satisfactory. The score of each domain of WHOQOL-BREF was obtained by averaging their corresponding items for each participant. Then, the scores were transformed linearly to a 0–100-scale as described by the author.4 HRQOL profile was categorized as low, moderate and high when the mean score was less than or equal to 45, 45–65, and greater than 65, respectably, for all domains and overall HRQOL based on literature.14
Structural equation modeling (SEM) was employed to examine the relationship between various exogenous and endogenous or mediating variables. The analysis was started with the hypothesized model (Figure 1), and modifications were performed iteratively by adding path links or including mediator variables, if theoretically supported, and comparing the model using root mean square error of approximation (RMSEA), comparative fit index (CFI) of each model fitted. Finally, an overidentified model with value RMSEA < 0.05 and CFI ≥ 0.95 was retained. Diagrammatically, the effect of each exogenous or mediating variable on the respective dependent variable was indicated by the path coefficient along with a single-headed arrow, and the correlation among disturbances (residual errors that reflect the unexplained variances in the latent endogenous variables due to all unmeasured causes) was indicated by double arrows. When mediation of effects was present, the direct, indirect, and total effects were determined using the nonlinear combination of estimator technique.
The final model (Figure 4) that fitted the data well and appeared theoretically meaningful was built by analyzing the hypothesized model (Figure 1) and inspecting iteratively the statistical significance of path coefficients and the relevance of relationships in the model.
Results
Socio-Demographic Characteristics
Of the total, 469 respondents with CHF were enrolled in the study, of whom 316 (67.40%) were women, 302 (64.2%) were married, 249 (53%) cannot read and write and 108 (38.4%) are housewives in occupation. The mean age of the patients was 53 (18.88 SD) years (Table 1).
 |
Table 1 Socio-Demographic Characteristics of Patients |
Clinical Characteristics
Around one-third 153 (32.5%) of the study participants had CHF secondary to IHD; less than one-fourth 103 (22.1%) of them had CHF secondary to valvular heart disease, the majority of patients 292 (62.3%) had not used health insurance; mean duration of HF was 6.4 years with a standard deviation of 4.60. Of the study participants, 251 (53.2%) were Lasix users (Table 2).
 |
Table 2 Personal and Clinical Characteristics of Study Patients |
Internal Consistency and Correlations Between the Domains of the WHOQOL-BREF
To check the internal consistency, Cronbach’s alpha was calculated for each domain of the instrument. All domains of WHOQOL-BREF had high values of Cronbach’s alpha (α > 0.7). Inter-domain correlation showed that there was a statistically significant correlation between domains, there is a highly positive correlation between physical health domain and social relation health domain (r=0.95, p<0.001) and as compared with psychological health domain and environmental health domain had a relatively weak correlation between them (r=0.71, p<0.001) (Table 3).
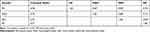 |
Table 3 Internal Consistency and Correlations Between the Domains of the WHOQOL – BREF |
HRQOL Among Patients with CHF
Among four domains of health-related quality of life, respondents scored highest and lowest mean HRQOL score in psychological health domain (50.21 with 15.61 SD) that is moderate HEQOL and physical domain (31.70 with 14.68 SD) that is low HRQOL, the remaining two domains mean score are 38.35 with 14.29 SD, and 46.22 with 14.22 SD for environmental health domain and social relation health domain, respectively. The mean score of overall HRQOL of patients with CHF was 41.61 (11.62SD) which was low QOL (Table 4).
 |
Table 4 HRQOL Among Adults with Heart Failure Patients in UoG Hospital, 2020 |
Perceived Health Satisfaction and Self-Rating of HRQOL of Patients
Study participants were asked to give their perception of their quality of life and health satisfaction. Based on their response; about one-third 165 (36%) study participants reported that their quality of life was neither good nor poor, while 142 (31%) of them had poor QOL. Regarding health satisfaction, 202 (43.10%) of them were very dissatisfied with their health and only 3.40% of them were satisfied with their health (Figures 2 and 3).
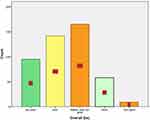 |
Figure 2 Perceived self-rated QOL of chronic heart failure patients attending at University of Gondar Hospital, 2020. |
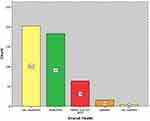 |
Figure 3 Perceived self-rated health satisfaction of chronic heart failure patients attending at University of Gondar Hospital, 2020. |
Health-Related Quality of Life and Other Associated Factors
The final model containing both the structural part (relationships among latent or observed variables) and the measurement part (relationship between a latent variable and its indicators or items) is shown in Figure 4 and Table 5. The fitted model was relatively parsimonious and well fitted with RMSEA=0.04 and CFI=0.96. Variables like sex, education, type of job, current medication, and Utilization of health insurance were excluded from the final model as their contributions were not statistically significant at an alpha level of 0.05.
 |
Table 5 The Direct, Indirect and Total Effect of Socio-Demographic and Clinical Factors on HRQOL Domains Among Patients with CHF Attending at UoG, 2020 |
In the fitted model, all the path coefficients in the diagram were statistically significant at an alpha level of 0.05. Accordingly, the model included only six exogenous variables (age, monthly income, current medication, duration of CHF, residency and educational level, four mediator variables (domains of HRQOL), and one endogenous variable (HRQOL). Six exogenous variables (age, monthly income, current medication, duration of CHF residency, and educational level were both, directly and indirectly, related to HRQOL via the mediator variables.
This estimated structural equation model indicates that environmental health factors had the most substantial causal effect on HRQOL, which was larger than the causal effects of psychological QOL, physical health, and social relationship factors. Physical health was statistically significantly associated with the age (p<0.0001), residency (p<0.0001), and underlying cause of CHF (p=0.002), psychological health domain was significantly associated with duration of CHF (P= 0.05), income (0.001), marital status (p=0.022) and age (p<0.001), social relation was statistically significantly associated with age (p<0.001) and education (p=0.006) and Regarding environmental health domain, it was associated with age (p=0.03), residency (p<0.001) occupation (p=0.040), income (p<0.0001) and health insurance (p=0.007) (Figure 4).
Testing the Structural Model of the HRQOL of Patients with CHF
Feasibility Assessment for the Hypothetical Model
The confirmatory factor analysis was performed with demographic factors, disease-related factors, behavioral factors, and HRQQOL, whereas we excluded insignificant variables (p>0.05) from the final model.
Test of the Goodness of Fit of the Hypothetical Model
The results of the analysis of the structural equation model produced using the study variables in the hypothetical model were as follows: goodness of fit for χ2 = 143.02 (P < 0.001, df = 48), GFI = 0.91, RMSEA = 0.04, NFI = 0.91, CFI = 0.95, TLI = 0.93, All of the GFI indices satisfied the recommended levels.
Effectiveness Analysis of the Hypothetical Model
The direct, indirect, and total effects of the factors associated with the HRQOL of the patients with CHF are presented in Table 5. The physical health domain had the greatest direct effect on the HRQOL with a score of 0.502. The environmental health factor had a direct effect on the HRQOL with a path coefficient of 0.485, and the psychological health factor had a direct effect on HRQOL with a path coefficient of 0.359. Social relation had a direct effect of 0.167 but statistically not significant (p-value=0.280 > 0.05) on the HRQOL. Monthly income had a direct effect on HRQOL with a path coefficient of 0.01, and a total effect of 0.02 when added to the indirect effect of environmental health factor (0.001) (Table 5).
Discussion
In this study, we aimed to construct a hypothetical model and verify the significance of the direct/indirect paths and the goodness of fit of the model under the theoretical assumption that demographic factors, personal-related factors, social relation, environmental factor, physical factor, disease-related factors, and behavioral factors, including depression, anxiety, fatigue, pain, sexual activity, and body image, determine the HRQOL of patients with CHF directly and indirectly.
In this study, we found that patients with CHF had lower quality of life in all domains of the WHOQOL-BREF especially in the physical health domain (mean score of 31.70) and an overall quality of life, which indicates that they know that their health is poor and affecting their HRQOL. This finding is congruent with other previous studies.15 This consistent result might be heart failure is a serious condition and leads to poor quality of life when the condition is not managed with heart failure management.
From the structural equation model, we found that environmental health factors like physical security, financial resources, and health care facility had the most substantial causal effect on HRQOL of patients with CHF with a path coefficient of 0.53 (95% CI, 0.32, 0.75), which was larger than the causal effects psychological health, and physical health, which was, in turn, larger than the causal effect of social relation domain. This finding is inconsistent with other studies.16 This inconsistency may be due to the research was conducted in a developed country and environmental health may not have a larger cause on HRQOL than the other factors. In Environmental health factors physical security, information and skill, and health facility (with the loading of 0.80) are the highly influential items on HRQOL as compared with the physical environment, financial resource, and recreation items (with loading 0.6) and transportation and home environment items (with loading 0.58). This result might be, heart failure often leads to the development of physical disabilities that, in turn, can have a detrimental effect on a patient’s quality of life.
Our finding demonstrated that, among domains of HRQOL, the physical health domain was the most affected domain for HRQOL next to the environmental health domain. This finding is In line with a couple of studies.16–18 This consistency could be defensible by CHF has more physical than mental (psychological) manifestations and social relations.
Similarly, psychological health and social relation was the least affected domain among the CHF patients. This finding is in line with other studies that were conducted southwest19 and northwest20 Ethiopia among DM patients. This consistency results in social relation and psychological health might be their social culture that gives support for diseased individuals with DM and CHF. Patients manifest more physically than mentally (psychologically).
Our results revealed that age had a significant association with all domains of HRQOL and had both a positive direct and indirect effect that resulted in a positive effect on the overall HRQOL of CHF patients. Patients aged 60 years and aboves had worse mental state, physical health, social relation, and environmental health. This finding is lined with previous studies conducted in a different research setting.21,22 Based on the knowledge that CHF incidence increases with age, researchers would anticipate that older patients who experience several limitations such as cognitive impairment, loss of personal autonomy, or anxiety and depression may have a poor quality of life.21
A study conducted in Greece21 documented that male adults have lower HRQOL in the social relation domain than female adults. However, the present study demonstrates that gender does not affect any domain of HRQOL. Direct comparisons with the findings of other studies are difficult because there are no other comprehensive HRQOL models of patients with CHF from Ethiopia or other African countries. The rural resident was associated with lower HRQOL for an environmental health domain, physical health domain, and overall HRQOL with negative path coefficients.
There is a study21 that had consistent findings with our study. This congruent finding might be patients’ lives in the rural area are more likely low in income, the physical environment may not be good, low health care accessibility to get medical treatment and most of them are uneducated so have low awareness about CHF. Being married was another socio-demographic factor that had a positive effect on environmental health and social relation among CHF patients and this is of course incongruent with other reports.21 This positive effect may be due to support from others can facilitate recovery from physical illness and enhance the ability to cope with and adapt to the consequences of chronic illnesses.
Also associated with both physical and mental (psychological) health were the years of suffering from the disease (duration of CHF) which may reflect symptoms’ severity. Patients often experience a loss of functional independence in daily activities such as feeding, dressing, housekeeping, bathing, and walking.23
It is noteworthy that evaluation is needed of all the changes that take place through the years and that may exacerbate HF patients’ quality of life such as inability to fulfill their prior role (social, professional, and family), diminished self-esteem, and distorted picture of themselves.
The finding of the present study also showed that income had a positive direct effect on the physical health, psychological health, and environmental health domain of HRQOL. These findings were consistent with previous studies.24 We know that financial situation is an important determinant of health, negatively affecting health outcomes and contributing to health inequities. Patients with a low income had low quality of life because most CHF patients are medical treatment dependent and unable to afford treatment costs.
Strength and Limitation
In this study, HRQOL was assessed based on the standardized tool that is validated for both developed and developing countries (WHOQOL_BREF). The current study also used multivariate analysis (SEM) that enables simultaneous analysis of the impact of multiple independent variables on several dependent variables and the subsequent direct comparison of the respective impact of the independent variables on the dependent variables. This also enables to incorporate the correlation between the latent variable and to determine direct, indirect, and total effect when mediation effect presents simultaneously. However, this study is not without limitations, the present study has been conducted in a single center, which limits the generalizability of the finding in Ethiopia; further multicenter studies are needed to address this issue.
Conclusion
The finding of the study indicated that a moderate to poor HRQOL in the physical dimension (31.70 mean score), moderately poor overall HRQOL (41.61 mean score), and a moderate to high HRQOL in the psychological health domain. Socio-demographic factors (age, residence, and marital status), clinical factors (duration of CHF) were factors associated with HRQOL among CHF. The results indicated that the importance of QOL assessment at appropriate periods, determining the exact treatment dimensions required, and implementing comprehensive HRQOL promotion programs in all physical, mental, environmental, and social relation dimensions.
Based on this result, approaches should be developed or effectively managing physical factors, psychological, and environmental factors to improve the QOL of patients with CHF. Developing and providing intervention programs to enhance social support can lead to improved quality of life for patients, because of the long-term and chronic illness of the patient.
Abbreviations
GFI, goodness-of-fit index; CFA, confirmatory factor analysis; CFI, comparative fit index, CHF; chronic heart failure, NFI, normal fit index; HRQOL, health-related quality of life; SEM, structural equation modeling; RMSEA, root mean square error of approximation; SD, standard deviation; TLI, Tucker–Lewis index; UoGCSH, University of Gondar Comprehensive Specialized Hospital; WHO, World Health Organization; WHOQOL, World Health Organization Quality of Life.
Data Sharing Statement
The datasets supporting the conclusions of this article are available upon request to the corresponding author.
Ethics Approval and Consent to Participate
Ethical approval was obtained from the Institutional Review Board (IRB) of the institute of public health, the University of Gondar, and a permission letter was obtained from the hospital administrator’s office. This study was conducted following the Declaration of Helsinki. The purpose of the study was well explained and informed consent was secured from study participants.
Acknowledgments
We would like to thank the University of Gondar for giving ethical clearance to conduct this research. Additionally, we wish to express my sincere thanks and appreciation to data collectors and supervisors for their support during the data collection period.
Author Contributions
All authors contributed to data analysis, drafting, or revising the article, have agreed on the journal to which the article will be submitted, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Disclosure
The authors declare that they have no competing interests in this work.
References
1. Roger VL. Epidemiology of heart failure. Circu Res. 2013;113(6):646–659.
2. Juenger J, Schellberg D, Kraemer S, et al. Health related quality of life in patients with congestive heart failure: comparison with other chronic diseases and relation to functional variables. Heart. 2002;87(3):235–241.
3. Bui AL, Horwich TB, Fonarow GC. Epidemiology and risk profile of heart failure. Nat Rev Cardiol. 2011;8(1):30. doi:10.1038/nrcardio.2010.165
4. Group W. Development of the World Health Organization WHOQOL-BREF quality of life assessment. Psychol Med. 1998;28(3):551–558. doi:10.1017/S0033291798006667
5. Cook C, Cole G, Asaria P, Jabbour R, Francis DP. The annual global economic burden of heart failure. Int J Cardiol. 2014;171(3):368–376.
6. Zambroski CH, Moser DK, Bhat G, Ziegler CJE. Impact of symptom prevalence and symptom burden on quality of life in patients with heart failure. 2005;4(3):198–206.
7. Alla F, Briançon S, Guillemin F, et al. Self‐rating of quality of life provides additional prognostic information in heart failure. Insights into the EPICAL study. Eur J Cardiovasc Nurs. 2002;4(3):337–343.
8. Angermann CE, Gelbrich G, Störk S, et al. Effect of escitalopram on all-cause mortality and hospitalization in patients with heart failure and depression: the MOOD-HF randomized clinical trial. JAMA. 2016;315(24):2683–2693.
9. Gupta A, Allen LA, Bhatt DL, et al. Association of the hospital readmissions reduction program implementation with readmission and mortality outcomes in heart failure. JAMA Cardiol. 2018;3(1):44–53.
10. Thommasen HV, Berkowitz J, Thommasen AT, Michalos AC. Understanding relationships between diabetes mellitus and health-related quality of life in a rural community. Rural Remote Health. 2005;5(3):441. Epub 2005 Aug 6. PMID: 16120021.
11. Byrd RJ, Steinhubl SR, Sun J, Ebadollahi S, Stewart WF. Automatic identification of heart failure diagnostic criteria, using text analysis of clinical notes from electronic health records. Int J Med Inf. 2014;83(12):983–992.
12. Schumacker RE, Lomax RG. A Beginner’s Guide to Structural Equation Modeling. Psychology Press; 2004.
13. Lopes AC. 25 anos representando os clínicos brasileiros. Rev Soc Bras Clín Méd. 2014;12:1.
14. Whoqol Group. Development of the World Health Organization WHOQOL-BREF quality of life assessment.Psychol Med 1998;28(3):551–558.
15. AbuRuz ME, Alaloul F, Saifan A, Masa’Deh R, Abusalem S. Quality of life for Saudi patients with heart failure: a cross-sectional correlational study. Glob J Health Sci. 2015;8(3):49. doi:10.5539/gjhs.v8n3p49
16. Lee S-Y, Song X-Y, Skevington S, Hao Y-T. Application of structural equation models to quality of life. Struct Equat Modeling. 2005;12(3):435–453. doi:10.1207/s15328007sem1203_5
17. Mijinyawa M, Yusuf S, Gambo M, Saidu H, Dalhatu A. Health related quality of life among patients with ischaemic heart disease in Kano, Nigeria. J Vasc Med Surg. 2016;4(282):2.
18. Boczor S, Daubmann A, Eisele M, Blozik E, Scherer M. Quality of life assessment in patients with heart failure: validity of the German version of the generic EQ-5D-5L™. BMC Public Health. 2019;19(1):1464. doi:10.1186/s12889-019-7623-2
19. Muze M, Hailu E, Woldemichael K, Fekecha B. Health related quality of life and its associated factors among diabetic patients attending diabetes clinic in Jimma university teaching hospital, Ethiopia, 2014. J Diabetes Metab. 2017;8(751):2. doi:10.4172/2155-6156.1000751
20. Reba K, Argaw Z, Walle B, Gutema H. Health-related quality of life of patients with diagnosed type 2 diabetes in Felege Hiwot Referral Hospital, North West Ethiopia: a cross-sectional study. BMC Res Notes. 2018;11(1):544. doi:10.1186/s13104-018-3625-x
21. Audi G, Korologou A, Koutelekos I, et al. Factors affecting health related quality of life in hospitalized patients with heart failure. Cardiol Res Pract. 2017;2017:1.
22. Gallagher AM, Lucas R, Cowie MR. Assessing health‐related quality of life in heart failure patients attending an outpatient clinic: a pragmatic approach. ESC Heart Fail. 2019;6(1):3–9. doi:10.1002/ehf2.12363
23. Dunlay SM, Manemann SM, Chamberlain AM, et al. Activities of daily living and outcomes in heart failure. Circ Heart Fail. 2015;8(2):261–267.
24. Health-related quality of life of patients with myocardial infarction, trend, and predictors, 2018: Available from: https://opus.lib.uts.edu.au.
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


