Back to Journals » Journal of Healthcare Leadership » Volume 13
Health-care Waste Management and Risk Factors Among Health Professionals in Public Health Facilities of South Omo Zone, South West Ethiopia, 2018
Authors Gizalew E Snr, Girma M Snr, Haftu D Snr , Churko C , Girma Z Snr
Received 27 January 2021
Accepted for publication 30 March 2021
Published 3 May 2021 Volume 2021:13 Pages 119—128
DOI https://doi.org/10.2147/JHL.S300729
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Pavani Rangachari
Esayas Gizalew Snr, Meseret Girma Snr, Desta Haftu Snr, Chuchu Churko, Zeleke Girma Snr
Department of Public Health, Arba Minch University, Arba Minch, SNNPR, Ethiopia
Correspondence: Meseret Girma Snr
Arba Minch University, Nech Sar Campus, PO Box: 21, Arba Minch, Ethiopia
Tel +251911836862
Email [email protected]
Introduction: Health-care waste is a great concern because, in addition to containing conventional toxic pollutants like mercury, chlorinated plastics, and solvents; it also includes a number of toxic materials not found in typical waste. There were no scientific data in Ethiopia that reveal practice toward management of health-care waste. Therefore, the aim of this study was to assess the management of health professionals toward health-care waste in South Omo zone public health facilities, South West Ethiopia, 2018.
Methods: A facility-based cross-sectional study was used with in the period of February 1– 30, 2018. A total of 362 health-care workers were sampled using the lottery method. Coding and entry of data was done using Epi Info™ version: 7.2 and analyzed with SPSS version 20 computer software. Descriptive statistics were computed. Bivariate analyses and multivariable logistic regression were used to identify predictor variables for practice of health-care providers.
Results: The overall finding of safe practice on health-care waste management among health-care workers was only 29.3%. Receiving training regarding medical waste management, work hours per day among respondents, availability and usage of color coded containers and yellow plastic bags for infectious waste had significant association with safe practice on health-care waste management.
Conclusions and Recommendation: The overall finding of safe practice on health-care waste management was only 29.3% among health-care workers. This study showed that most of health-care workers did not meet standard practice. Providing training on medical waste management is essential to encourage safe practices among health-care workers and more attention should be directed at the health-care attendants in order to close the yawning gap in their practice level of medical waste management.
Keywords: medical waste management, risk factors, Ethiopia, health professionals
Introduction
Waste generated from health facilities linked with medical procedures is said to be health-care waste. More than 85% of waste generated from health-care activities are nonhazardous. The remaining 15% of health-care waste is hazardous material that may be contagious, toxic, or radioactive.1 Solid or liquid waste which comes from health-related facilities is referred to as medical waste. This waste involves two segments, that is hazardous and not hazardous waste.2
The management of health-care waste (HCW) includes planning, implementation, and monitoring of activities aimed to prevent contact, warrant the care of customers and professionals involved, prevent the incident of ecological influences while reducing the production of waste.3,4 Health-care waste is risky because of the following features: presence of contagious agents, a genotoxic or cytotoxic chemical structure, presence of poisonous or dangerous chemicals or biologically aggressive pharmaceuticals, existence of radioactivity, and presence of sharp materials.5
In a working area that has unsafe management of medical waste which might be due to a contact with infectious diseases by health professionals and clients that could in turn produce infection as a result of blood-borne pathogens.6 In a study done in 2000, sharps injuries were estimated to have caused about 66,000 hepatitis B (HBV), 16,000 hepatitis C (HCV) and 200–5000 HIV infections among health professionals. Among health-care workers, the portions of these infections that result from percutaneous work-related exposure to HCV, HBV, and HIV are 39%, 37%, and 4%, respectively.1
Everyone who come into close contact with dangerous HCW are possibly at risk from the exposure, together with those working within health facilities that produce risky waste, and those people who either handle the waste or are unprotected from it as a result of careless activities.5 In the earlier period, various struggles have been made toward proper and safe management of harmful health-care waste for low income countries by different organizations, predominantly the World Health Organization (WHO).7 Nonetheless, insufficient practices are regularly applied in most health facilities mainly in less developed countries.8,9
Therefore, medical waste management is a global public health issue; the effects raised from medical waste may affect the public health and the environment if neglected. Despite the governing laws, policies, and guidelines on medical waste management, it seems to be poorly managed from the collection point to the disposal point. The processes of medical waste management, which include sorting (segregation), handling/collection, storing, transporting, treatment, and thereafter disposing should be adhered to by all medical waste (MW) handlers. Medical waste produced at the hospital can greatly endanger the public health and the environment and thus cause nosocomial infections if MW is not managed well.10
The World Health Organization (WHO) reported that from the total waste produced by health-care activities, 85% is general waste and the balance is considered as hazardous, as it tends to be infectious, toxic, or radioactive.11 The infectious and hazardous nature of health-care waste makes it necessary to manage or handle such wastes with care and tact.12 Mismanaging health-care waste can have serious health implications for waste handlers (workers), health-care professionals such as, nurses, doctors, paramedical staff, laboratory technicians, pharmacists or dispensary technicians as well as patients, waste scavengers, and the general population as a whole.12
Studies have shown that a high percentage of workers who handle waste and individuals who live near dumping sites are infected with gastrointestinal parasites, and other diseases like cholera, yellow fever, and salmonellosis.13 In the world around 5.2 million people, which including 4 million children, die each year from waste management related diseases.14 European survey of needle stick injury found that nurses are exposed more commonly (91%) than doctors (6%). In a study conducted by Askarian M et al in Iran in 2003, 70% of medical, 74% of dental and 72% of nursing students reported having at least one sharps injury since the beginning of their clinical practice.15
In Ethiopia, several studies assessed the practice of health professionals toward health-care wastes. A study done in Gondar University hospital, showed that 46.3% of health-care workers had correctly practiced health-care waste segregation.16 Another study in Ethiopia reported that about 33% of respondents correctly segregated waste in their respective health facilities.17
Very few studies tried to assess HCWMP and its associated factors among health-care workers in Ethiopia. Most previous studies also recommended further research on the practice of health-care workers toward management of health-care waste and associated factors to influence policy makers. That was why the aim of this study was to assess health professionals practice regarding health-care waste management and factors associated with safe practice.
Methods and Materials
Study Setting and Period
The study was conducted in South Omo zone public health facilities. The zone has 32 public health centers with 580 health-care workers and one general hospital with 260 health-care workers. They serve a population of approximately one and half million. The zone is one of the pastoralist zones in southern region and located 755 km southwest of Addis Ababa, the capital city of Ethiopia. This study was conducted from February, 1–30, 2018.
Study Design
An institutionbased cross-sectional study was employed.
Populations
- Source population: All health-care workers working in South Omo zone public health facilities.
- Study population: randomly selected health-care workers working in South Omo zone public health facilities.
Eligibility Criteria
- All health professionals who work in the selected health facilities were included in this study and those health professionals whose service years were less than six months and absent during data collection were excluded.
Sample Size Determination
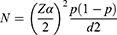
A single population proportion formula was used to determine sample size and the following assumptions were considered:
Where,
P= proportion of health-care waste practice is 31%, which is taken from previous study.18
Zα=95%CI and
d=5% margin of error.
N= the estimated sample size.
N=(1.96)2* 0.31 (1–0.31)/(0.05)2=329. We used 10% nonresponse rate, therefore final estimated sample size was 362.
Sampling Technique
In order to ensure representativeness of samples, more than 31% of all health centers were considered from the zone. Firstly, we stratified the health facilities as hospital and health centers. Jinka hospital was purposively selected since it was the only hospital in the zone. From health centers, 10 health centers (Kako, Gazer, Senegal, Keyafer, S/bili, Tolita, Wubhamer, Bitema, Metser, Bereka) were randomly selected for this study. So we included ten health centers and one general hospital in this survey. The total numbers of health professionals working in each of the selected health facilities were identified to proportionally allocate the sample size. Finally, the study participants were selected using a systematic sampling technique (Figure 1).
Study Variables
Dependent variable: practice on health-care waste management (safe and unsafe practice).
Independent variables:- sociodemographic variables: age, profession category, educational status and work experience. Behavioral factors: improper medical waste segregation and management, and use of personal protective equipment (PPE).19
Work environment: length of working hours (per day), availability of color-coded containers, rules and regulations, existence of control measure, working department, training and existence of legislation policies, and guidelines for medical waste management practice (MWMP) and its implementations of rules, guideline of health-care waste management.
Operational Definitions
Practices: in this study health-care waste management practice is dichotomized as safe and unsafe practice. The respondents were considered as having safe practice if they responded to five or more of practice questions and unsafe practice if they answered four or fewer practice questions. A score of 1 was given for correct practice and 0 for incorrect practice.20–23
Data Collection Procedures
Data were collected using a pretested and structured self-administered questionnaire which was adapted from the WHO recommendation assessment tool and different literature.24,25 The tool contained three main components like sociodemographic factors, behavioral factors, work environment factors, and practice questions related with waste management. Three data collectors (two BSc nurse, one health officer) and one supervisor whose background is BSc nurse were recruited for this survey. The trained data collectors provided the questionnaire to randomly selected health-care workers to gather the data from February 1–30, 2018. From the expected 362 health professionals who were approached for survey, 358 responded it.
Data Quality Management
Firstly, the questionnaire was prepared in English and then translated to Amharic, then back to English in order to look for consistency of the questions. Two-day training was given for data collectors before they started data collection. Regular supervision was made during data collection period. Collected data was checked for its completeness.
Data Processing and Analysis
Data were entered in to Epi-Info™ version 7.2.2.6 software and exported to SPSS version 20 for analysis. Descriptive analyses like frequency distribution were computed for sociodemographic and other important variables. Binary logistic regression analysis was employed to show the relationship between practice of health professionals towards health-care waste management and their associated factors. All variable which have p-value <0.25 was then entered into the multivariable logistic regression model. A p-value <0.05 and 95%CI were used to see the strength of association between factors and the outcome variable. Finally, the results were presented using tables, frequencies, figures, and texts.
Ethical Consideration
This study was conducted in accordance with the Declaration of Helsinki. Before data collection we obtained an ethical clearance letter from IRB (Institute Research Ethics Review Board) (reference number cmhs/PG/772/10), Arba Minch University. We also obtained permission from South Omo zone health department and each woreda health offices before conducting data collection. Finally informed verbal consent was obtained from each respondent and it was approved by IRB, Arba Minch University. The respondent’s confidentiality was maintained.
Results
Sociodemographic Characteristics of Respondents
The study comprised of a total sample size of 362 health-care workers. Of this, 358 health-care workers participated giving a response rate of (98.9%). Distribution of the respondents by sex indicated that male employees accounted for the highest proportion, 186 (52%). According to the age distribution of the respondents the majority 168 (46.9%) of the participants were in the age group of 26 to 30 years old. Regarding religion 169 (47.2) were Orthodox followed by 139 (38.8) Protestants. One hundred and seventeen (32.7%) were nurses and 74 (20.7%) were laboratory technicians. From an education perspective, 241 (67.3%) were diplomas holders followed by 114 (31.8%) degree holders. Regarding work experience 241 (67.3%) of the respondents had between one and five years experience (Table 1).
 |
Table 1 Sociodemographic Characteristics of the Respondents in South Omo Zone Public Health Institution March, 2018 |
Health-care Waste Management Among Health-care Workers Disaggregated by Profession in South Omo Zone Public Health Institution
A total of 74.3% health care workers used gloves when handling medical waste, of which 80% were doctors, 80.3% staff nurses, 70.3% laboratory technicians, 55.6% health officers, 76% midwives, 73.8% pharmacists and 74.4% other staff. Segregating into different color-coded bag activity was mostly practiced by doctors (80%), followed by staff nurses (72.6%), but least practiced by health officers (48.1%). Regarding use of the biohazard symbol, the time for waste store laboratory technicians (68.9%) followed by other health staff (63.7%). The majority of doctors (80%) were applying health-care waste management (HCWM) guidelines and policy to manage health-care waste but the least, only (29.6%), were applied by health officers (Table 2).
 |
Table 2 HCWM Among Health-care Workers Disaggregated by Profession in South Omo Zone Public Health Institution, 2018 |
Behavioral and Working Environment Related Factors
Out of the total respondents 304 (84.9%) had awareness of disease transmitted by improper management of medical wastes. Among the respondents almost all (98%) of them used PPE when handling HCW. Regarding to awareness of proper accident and injury reporting system, vaccinated against hepatitis B and awareness of the general precautions respondents were 80.7%, 75.1% and 76.5%, correspondingly. Among the total respondents 216 (60.3%) worked eight hours a day. Only 57% of the color-coded containers were available in the wards of the respondents, but 70.9% of respondents had access to guidelines and policies of HCWM. Only 28.8% of the respondents had received training regarding HCWM (Table 3).
 |
Table 3 Behavioral and Work Environment Factors Related with Practice Toward HCWM (N=358) |
Prevalence of Safe Practice Among Health-care Workers Toward Health-care Waste Management
Out of the 358 HCWs, 105 HCWs were safely practicing HCWM with prevalence of 29.3% (95%CI: 24.6–34) (Figure 2).
 |
Figure 2 Shows the prevalence of health-care waste management among health professionals at South Omo zone public health facilities. |
Two hundred and sixty-six (74.3%) of the respondents used gloves when handling health-care waste. Only 200 (55.9%) of respondents safely treated infectious waste with sterilization and disinfection before disposal and 41.3% of respondents apply medical waste management guidelines and policy to manage health-care waste correctly. Two hundred and forty-one, (67.3%) used the readily existing waste bins for placing of medical waste (Table 4).
 |
Table 4 Prevalence of Health-care Waste Management Practice Among Health-care Worker at South Omo Zone Public Health Facilities 2018 |
Factors Associated with Health-care Waste Management Practice
In multivariable logistic regression analysis, receiving training regarding MWM, work hours per day among respondents, availability of color code containers and usage yellow color-coded containers to collect infectious waste were factors associated with HCWM practice. Health-care workers who had training regarding health-care waste management (AOR: 9.233, 95%CI: 4.907–17.373) were 9.23 times more likely to safely practice compared to health-care workers who did not have training. HCWs who worked eight hours (AOR: 7.39, 95%CI: 3.486–15.668) were 7.39 times more likely to safely practice health-care waste management when compared to those who were working more than eight hours. Regarding availability of color-coded containers respondents who had color-coded containers in their ward (AOR: 2.43, 95%CI: 1.343, 4.423) were 2.43 more likely to safely practice HCWM than those who did not. Respondents who had yellow color-coded containers in their working department (AOR: 4.77, 95%CI: 2.557–8.910) were 4.77 more likely to safely practice health-care waste management when compared to health-care workers who did not used yellow colour-coded containers (Table 5).
 |
Table 5 Multivariable Logistic Regression Analysis Showing Association of Variables with Practice of Health-care Waste Management, 2018 |
Discussion
In Ethiopia, health-care waste management is a critical issue and therefore there is a need for an assessment of current management practices among health professionals for decision making.
This study showed that 29.3% of the respondents were safely practicing health-care waste management. This result is lower than the study done in Bangladesh in which about 45% of health professionals practiced health-care waste management properly.9 It is also less than a study done in Ludhiana hospital in India the biomedical waste (BMW) management practice was (59.1%) which was safe practice.26 These might be due to various reasons: unavailability of color-coded containers and lack of containers labeled with the biohazard symbol for contagious health-care waste, commitment and sense responsibility among health-care workers (HCWs), inappropriate waste management and disposal systems, inadequate financial and human resources and the lower priority given to the topic may be responsible for causing such problems.
In this study health-care workers who had training regarding health-care waste management were 9.23 times more likely to safely practice HCWM compared to health-care workers who did not have training. It is consistent with a study done in Gondar town, Ethiopia, in that there was significant association between training and safe practice of health-care waste management.17 This might be due to lack of attention and prior arrangement to give training to all HCWs regarding health-care waste management.
The respondents who worked eight hours a day were 7.3 times more likely to safely practice health-care waste management compared to the respondents who worked more than eight hours a day. This result is consistent with a study done in Gondar University hospital, Ethiopia in that there was significant association between working hours and safe practice of health-care waste management.16 It might be due to working more than the recommended hours leads to unsafe practice of health-care waste management and less emphasis on its consequences.
In this study HCWs who had color-coded containers in their working department were 2.43 times more likely to safely practice health-care waste management when compared to health-care workers who had no color-coded containers in their wards. This result is in line with a study done in Gondar University hospital and Addis Ababa. The possible reason might be availability of color-coded containers in the working department initiate them to use and clean their environment.27,28
Regarding usage of yellow color-coded containers to collect infectious waste, respondents who used yellow color-coded containers were 4.77 times more likely to manage health-care waste safely compared to HCWs who did not use yellow color-coded containers. This finding is in agreement with studies done in different parts of the world.27,29,30 It might be that some health-care workers did not give value and were careless of the risk of infectious waste. It might be also due to less emphasis and commitment given to waste management on the side of concerned officials.
This study has the following limitations: allied structures/support staff: cleaners and administrative staff were not included in this study. We did not include observation checklist for assessing practice.
Conclusion and Recommendation
The overall findings of this study showed that only 29.3% safely practiced health-care waste management, which indicated that the majority of HCWs did not meet standard practice. Moreover, there was unsafe waste management practice in the study area. This study showed that receiving training regarding MWM; work hours per day among respondents, availability of color-coded containers and usage of yellow color-coded containers to collect infectious waste were significantly associated with safe practice of health-care waste management. Health-care workers should try to exert their own effort to assure safe practice of the health-care waste. Health centers, districts, zonal health departments and other concerned bodies should try to fulfill necessary equipment such as different color-coded containers and manpower to reduce the overload of work and to adjust the work time per day.
Abbreviations
AOR, adjusted odds ratio; BMW, biomedical wastes; COR, crude odds ratio; IRB, Institute Research Review Board; HCWM, health-care waste management; HCWs, health-care workers; HCW, health-care waste; HBV, hepatitis B virus; HCV, hepatitis C virus; MW, medical wastes; MWMP, medical waste management practice; PPE, personal protective equipment; SNNPR, Southern Nations Nationalities of People's Region; SPSS, statistical package for social sciences.
Data Sharing Statement
The data used to support the findings of this study are available from the corresponding author upon request.
Acknowledgments
Our heartfelt thanks go to South Omo zone and South Ari woreda administration and South Omo Health Department for their goodwill till completion of the courses. We would like to express our heartfelt gratitude to the Department of Public Health, College of Medicine and Health Science, Arba Minch University. We would like to thank data collectors, supervisors and study participants.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This research was funded by Arba Minch University grants for student research.
Disclosure
The authors report no conflicts of intererst in this work.
References
1. Chartier Y, editor. Safe Management of Wastes from Health-Care Activities. World Health Organization; 2014.
2. Uwa CU. Level of awareness as indicators for healthcare waste management in Tertiary Health Facilities in Enugu Metropolis (Nigeria). J Environ Sci Toxicol Food Technol. 2013;5(6):33–37.
3. Services. MoHaS. Infection Prevention Control Guidelines. Windhoek: Government Printers; 2010.
4. Neupane S. Bio medical waste management in hospitals; 2010. Available from: http://wwwlegalindiacom/bio-medical-waste-management-in-hospitals/.
5. World Health Organization. Status of Health-Care Waste Management in Selected Countries of the Western Pacific Region. 2015.
6. Sawalem M, Selic E, Herbell JD. Hospital waste management in Libya: a case study. Waste Manage. 2009;29(4):1370–1375. doi:10.1016/j.wasman.2008.08.028
7. Shinee E, Gombojav E, Nishimura A, Hamajima N, Ito K. Healthcare waste management in the capital city of Mongolia. Waste Manage. 2008;28(2):435–441. doi:10.1016/j.wasman.2006.12.022
8. Organization. WHO. Healthcare Waste Management. Fact Sheet. Vol. 281. October, 2004.
9. Patwary MA, O’Hare WT, Street G, Elahi KM, Hossain SS, Sarker MH. Quantitative assessment of medical waste generation in the capital city of Bangladesh. Waste Manage. 2009;29(8):2392–2397. doi:10.1016/j.wasman.2009.03.021
10. URT. Performance Audit on the Management of Healthcare Waste. Dar Es Salaam: NAO and MoHSW M; 2014.
11. Riyaz BS, Asima B, Subhas GT. Liquid waste treatment plant in tertiary care teaching hospitals attached to government hospital college. J Indian Soc Hosp Waste Manage. 2010;9:41–46.
12. Fei- Baffoe B. Household and Industrial Waste Management. Kwame Nkrumah Science University of Science and Technology K-; 2020.
13. Manyele SV, Anicetus H. Management of medical waste in Tanzania hospitals. Tanzan J Health Res. 2006;8(3).
14. Akter N. Medical waste management: a review.
15. Askarian M, Shaghaghian S, McLaws ML. Needle stick injury among nurses of Fars province; October 21, 2008. Availbale from: https://doi.org/10.1016/j.annepidem.2007.07.106.
16. Mesfin A, Worku W, Gizaw Z. Assessment of health care waste segregation practice and associated factors of health care workers in Gondar University Hospital, North West Ethiopia, 2013. Univ J Public Health. 2014;2(7):201–207.
17. Hayilmichael D, Davy A, Yirsaw D, Zegeye A. Assessing the management of health care waste in Hawssa City Ethiopia. Waste Manag Res. 2010;29(8):854–862.
18. Tadesse Alemayehu1 AWaNA. Medical waste collectors in Eastern Ethiopia are exposed to high sharp injury and blood and body fluids. J Prev Infect Control. 2014;2(2):7.
19. Rappe CM, Nyregen G. Clinical waste management and disposal markets huge impact on alternate site due to strangest regulations. J Environ Sci Technol. 2009;21(5):961–979.
20. Ama Twumwaa AM, Godi A, Carboo D, Tarkang. EE. Waste management practices of a regional hospital in Ghana. Cent Afr J Public Health. 2015;1:3.
21. Imchen T, Kumari R, Singh JV, Srivastava K, Singh A. A study of biomedical waste management among healthcare personnel at a tertiary hospital in Lucknow district. Int J Community Med Public Health. 2017;4(5):1483–1487. doi:10.18203/2394-6040.ijcmph20171460
22. Level WHOWH-cwmRatfc.
23. Global health care waste project module 4: national healthcare waste management planning.
24. Kannur K, Shyamala R
25. WHO. Survey Questionnaire for HCW Management. South East Asia: World Health Organization; 2004.
26. Karmakar N, Datta SS, Datta A, Nag K. A cross-sectional study on knowledge, attitude and practice of biomedical waste management by healthcare personnel in a tertiary care hospital of Agartala, Tripura. Natl J Res Community Med. 2016;5:189–195.
27. Adogu P, Ubajaka C, Nebuwa J. Knowledge and practice of medical waste management among health workers in a Nigerian general hospital. Asian J Sci Technol. 2014;5(12):833–838.
28. Thurn JR. HIV and occupational risk: evolving ways to protect healthcare workers. Postgrad Med. 1997;102(4):155–161. doi:10.3810/pgm.1997.10.334
29. Mayele S, Lysenga T. Factors affecting medical waste management in low level health facilities in Tanzania. Afr J Environ Sci Technol. 2010;4(5):304–318.
30. Suwaran M, Ramesh G. Study about awareness and practices about health care waste management among hospitals staff in a medical college hospital Banglore. Iran J Basic Med Sci. 2012;3(1):7–11.
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.