Back to Journals » Neuropsychiatric Disease and Treatment » Volume 11
Health care resource use and direct medical costs for patients with schizophrenia in Tianjin, People’s Republic of China
Authors Wu J, He X, Liu L, Ye W, Montgomery W, Xue H, McCombs J
Received 22 October 2014
Accepted for publication 1 December 2014
Published 7 April 2015 Volume 2015:11 Pages 983—990
DOI https://doi.org/10.2147/NDT.S76231
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Wai Kwong Tang
Jing Wu,1 Xiaoning He,1 Li Liu,2 Wenyu Ye,2 William Montgomery,3 Haibo Xue,2 Jeffery S McCombs4
1School of Pharmaceutical Science and Technology, Tianjin University, Tianjin, People’s Republic of China; 2Lilly Suzhou Pharmaceutical Company, Ltd, Shanghai, People’s Republic of China; 3Eli Lilly and Company, Sydney, Australia; 4Departments of Clinical Pharmacy and Pharmaceutical Economics and Policy, School of Pharmacy, University of Southern California, Los Angeles, CA, USA
Objective: Information concerning the treatment costs of schizophrenia is scarce in People’s Republic of China. The aims of this study were to quantify health care resource utilization and to estimate the direct medical costs for patients with schizophrenia in Tianjin, People’s Republic of China.
Methods: Data were obtained from the Tianjin Urban Employee Basic Medical Insurance (UEBMI) database. Adult patients with ≥1 diagnosis of schizophrenia and 12-month continuous enrollment after the first schizophrenia diagnosis between 2008 and 2009 were included. Both schizophrenia-related, psychiatric-related, and all-cause related resource utilization and direct medical costs were estimated.
Results: A total of 2,125 patients were included with a mean age of 52.3 years, and 50.7% of the patients were female. The annual mean all-cause costs were $2,863 per patient with psychiatric-related and schizophrenia-related costs accounting for 84.1% and 62.0% respectively. The schizophrenia-related costs for hospitalized patients were eleven times greater than that of patients who were not hospitalized. For schizophrenia-related health services, 60.8% of patients experienced at least one hospitalization with a mean (median) length of stay of 112.1 (71) days and a mean cost of $1,904 per admission; 59.0% of patients experienced at least one outpatient visit with a mean (median) number of visits of 6.2 (4) and a mean cost of $42 per visit during the 12-month follow-up period. Non-medication treatment costs were the most important element (45.7%) of schizophrenia-related costs, followed by laboratory and diagnostic costs (19.9%), medication costs (15.4%), and bed fees (13.3%).
Conclusion: The costs related to the treatment of patients with schizophrenia were considerable in Tianjin, People’s Republic of China, driven mainly by schizophrenia-related hospitalizations. Efforts focusing on community-based treatment programs and appropriate choice of drug treatment have the potential to reduce the use of inpatient services and may lead to better clinical and economic outcomes in the management of patients with schizophrenia in People’s Republic of China.
Keywords: schizophrenia, health care resource use, direct medical costs, People’s Republic of China
Introduction
Schizophrenia is a chronic and debilitating mental illness that affects millions of people in the modern society. The illness typically begins in late adolescence or early adulthood and often involves a complex set of disturbances of thinking, perception, affect, language, and sense of self and social behavior.1 According to the World Health Organization (WHO), schizophrenia affects approximately 29 million people worldwide, of whom 20 million live in developing or in the least developed countries.2 The lifetime prevalence of schizophrenia in People’s Republic of China is about 0.78% for those aged 18 or older, while it ranges from 1%–1.5% in western countries.3–5 Moreover, there are huge differences between People’s Republic of China and the West in terms of the characteristics, experience, and treatment of the disorder.3,6 A higher prevalence in women than in men, and a much higher prevalence of schizophrenia in urban areas than in rural areas have been found in People’s Republic of China.6,7
Up to 80% of patients diagnosed with schizophrenia experience persistent chronic illness with relapses during the early and later stages of the disease.1,8,9 As a result, many patients will require long-term treatment with antipsychotic medications and other support services, often for life. This disease is therefore associated with considerable economic burden. In developed countries, direct health care costs of schizophrenia, including the costs of hospitalizations, medications, outpatient care, diagnostic procedures, and long-term care services, have been shown to account for 1.5%–3% of the total national health care expenditure.10–13 People with schizophrenia also have high rates of physical comorbidities, including diabetes, hyperlipidemia, cardiovascular disease, and obesity, the treatment of which adds to the economic burden.14 Further, schizophrenia is a stigmatizing illness that leads to high levels of social rejection and high rates of unemployment. The indirect costs of schizophrenia have been estimated to range from being equivalent to direct costs to up to five times higher than the direct costs.15,16
Despite the increasing economic impact of schizophrenia, comprehensive cost-of-treatment studies have, until now, only been carried out sporadically in developing countries.17–20 The few studies that have been undertaken in developing countries suggest a pattern of costs quite dissimilar to that in the developed economies. A few studies addressing the issue of the treatment costs of schizophrenia in People’s Republic of China have also been reported. However, these studies were limited to small sample sizes (at one or two hospitals) or only inpatients.21,22 A comprehensive estimate of the costs associated with this disease is required to ensure efficient and systematic delivery of appropriate mental health services in People’s Republic of China and to inform the allocation of funds for these services. Such cost estimates are especially critical in formulating reimbursement policies in regard to new medical services and health care technologies, including new medications.
The aims of this study were to quantify health care resource utilization and to estimate direct medical costs using information from people covered by the Urban Employee Basic Medical Insurance (UEBMI) scheme in Tianjin, People’s Republic of China. Firstly, we attempted to quantify the health care service utilization patterns and costs attributable to patients with schizophrenia from all causes and break down schizophrenia-related and psychiatric-related services. Secondly, we attempted to estimate the direct overall medical costs and costs associated with hospitalized (non-stable) and non-hospitalized (stable) patients. The contributions of the various cost components to schizophrenia-related costs were also determined.
Materials and methods
Database properties and study population
The data for this study were obtained from the UEBMI claims of Tianjin city for the years 2008 through 2010. The UEBMI system, which was established in 1998, is one of the three basic medical insurance systems in People’s Republic of China. Mandatory participation is planned for all employees in both public and private companies, including government officials and self-employed persons. By 2010, the enrollees in Tianjin consisted of almost 5.1 million members, representing 51.7% of the registered residences in Tianjin city.23 The analytical sample in this study was a random sample of 30% of all enrollees of the UEBMI scheme in Tianjin city.
Patients aged 18 years or above were included if they had at least one schizophrenia-relevant diagnosis (International Classification of Diseases [ICD]-10 code F20 supplemented by Chinese description) between January 1, 2008 and December 31, 2009. Index diagnosis was defined as the first observed diagnosis of schizophrenia during 2008 through 2009, and the study period was defined as 12 months following index diagnosis. Patients were excluded if they were not continuously insured for the 12-month study period. The fee-for-service payment system contains all the data relating to itemized medical services or products, such as diagnoses, procedures, hospitalizations, consultations, medications, medical consumables, and the costs of each service or product. Inpatient and outpatient care claims were retrieved from the database and included in the analysis for all schizophrenia patients.
Identification of schizophrenia-specific resource use and costs
Health care resource utilization and direct medical costs were assessed from the payers’ perspective, ie, the total amount paid by the insurer and the patient combined. The health care resource utilization and the medical costs attributable to schizophrenia-related, psychiatric-related, and all-cause health service usage were calculated respectively. All the medical services under the primary diagnosis ICD-10 F20 were defined as schizophrenia-related, and all the medical services under the primary diagnosis ICD-10 F00–F99 were defined as psychiatric-related.
Study patients were divided into hospitalized and non-hospitalized subgroups according to whether the patient had a schizophrenia-related hospitalization during the 12-month follow-up period. The basis for the formation of subgroups was the assumption that patients who did not require a hospital admission associated with a diagnosis of schizophrenia were more likely to have not relapsed and were defined as being stable.24,25 Similarly, patients were defined as unstable (or to have relapsed) if they were hospitalized because of schizophrenia during the follow-up period. It was our intention to attempt to estimate the cost differences between stable (non-relapsed) and non-stable (relapsed) patients.
The total direct medical costs were separated into medication costs, non-medication treatment costs, laboratory and diagnostic costs, bed fees, and the costs of other services, including blood transfusion, medical consumables, and air-conditioning, based on the classification of costs used in the UEBMI. Medication costs were further broken down into antipsychotics (typical and atypical), concomitant medications, traditional Chinese medicine (TCM), and other medications. In addition, the type of concomitant medications (antianxiety, anticholinergic, sedative-hypnotic, antidepressant, and mood stabilizer) taken was also described. Non-medication treatment costs corresponded to the costs of any other treatment except medication, which includes nursing, monitoring, psychotherapy, behavior training, and intervention. Laboratory and diagnostic costs referred to the costs of physical examinations and biochemical/pathology tests. All the costs were converted into USD with the exchange rate in 2009 (6.83 CNY equal to 1 USD).
Data were presented as percentages and mean ± standard deviation (median) where appropriate. The differences between the hospitalized and non-hospitalized groups were compared using the Wilcoxon rank-sum test, Student’s t-test, or χ2-test, as needed. A P-value of <0.05 was considered as statistically significant. Statistical analysis was performed by using STATA 12.0 (stata.com).
Results
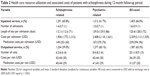
A total of 2,125 patients met the study inclusion criteria (Table 1). The mean age of patients was 52.3±12.2 years, with most of the patients at age ≥45 years (35.9% between 45 years and 54 years, 22.9% between 55 years and 64 years, and 16.5% at age ≥65 years). The percentage of female patients was 50.7%, and retired patients made up 55.7% of the sample. With respect to antipsychotic medications, 37.2% of the patients were treated with atypical-only antipsychotic medications, followed by 30.4% with typical-only, and 25.5% with both typicals and atypicals during the 12-month follow-up period. The majority (89.2%) of the patients received concomitant medications, of whom 77.3% received antianxiety agents, 46.2% received anticholinergic agents, and 31.9% received sedative-hypnotic agents. Furthermore, 76.4% of the patients were treated with TCM. Among the schizophrenia patients, 9.2% of the patients were diagnosed for depression, 7.9% for unspecified mental disorder, 6.3% for anxiety, and 1.9% for bipolar disorder. Other comorbidities that were observed included 27.5% patients with heart disease, 15.1% with hypertension, 9.3% with diabetes, and 4.1% with hyperlipidemia.
Of the total cohort, 60.8% of the patients had at least one hospitalization (hospitalized group) during the 12-month follow-up period. The patients in the hospitalized group were more likely to be male, younger, working, receiving typical antipsychotics only and concomitant medications (except for antidepressants) compared with those in the non-hospitalized group (P<0.05). In terms of mental health comorbidities, the patients diagnosed with an unspecified mental disorder in the hospitalized group were more common than in the non-hospitalized group, while the percentages of patients with depression or anxiety were comparatively lower. Besides, the patients in the hospitalized group had a lower prevalence of physical comorbidities including heart disease, hypertension, diabetes, and hyperlipidemia (P<0.001).
When considering schizophrenia-related health care service utilization and the associated costs (Table 2), the mean (median) number of admissions per patient per year was 1.4 (1), with a mean (median) length of stay of 112.1 (71) days, and a mean total cost $1,904 per admission. The mean (median) number of outpatient visits per patient per year was 6.2 (4), with a mean total cost of $42 per outpatient visit. On an average, medication costs ($40) accounted for about 95% of outpatient costs. When considering psychiatric-related health service utilization and the associated costs, there was a higher average rate of inpatient admissions (1.5) and outpatient visits (8.4), and higher costs per admission ($2,408). Finally, when looking at the utilization of all-cause health services, there was a higher average rate of outpatient visits (20.1) and lower costs per visit ($36) compared to the schizophrenia-related health service estimates.
The mean total annual schizophrenia-related costs were $1,775 per patient, compared with the psychiatric-related costs of $2,408 per patient, and the all-cause costs of $2,863 per patient (Table 3). The percentage of all-cause costs attributable to schizophrenia was 62.0%. Schizophrenia-related costs in the hospitalized group were eleven times greater than that for the non-hospitalized group ($2,772 versus $231, P<0.001). The mean annual all-cause costs for the hospitalized group were the highest, amounting to $3,953 per patient. Out-of-pocket expenses paid by the patients were significant with approximately 27.8% of the total all-cause costs among the total cohort, and the out-of-pocket percentage for schizophrenia-related total costs was 17.5%.
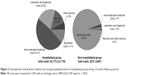
Among the annual schizophrenia-related costs for the total cohort, non-medication treatment costs were the most important component, accounting for 45.7% of total costs, followed by laboratory and diagnostic costs (19.9%), medication costs (15.4%), and bed fees (13.3%) (Figure 1). The cost components for medication were atypical antipsychotics (51.7%), typical antipsychotics (1.7%), concomitant medication (14.7%), TCM (13.6%), and other medications (18.2%). In terms of the subgroups, non-medication treatment costs (48.1%) were the largest component for the hospitalized group, and was followed by laboratory and diagnostic costs (20.9%), bed fees (14.0%), and medication costs (11.1%) (Figure 2). On the other hand, the majority of costs for the non-hospitalized group were medication costs (95.6%) (Figure 2).
Discussion
Our study provides important information about the disease-specific and all-cause associated costs for the treatment of patients with schizophrenia, from the payers’ perspective, in People’s Republic of China. The mean annual all-cause treatment costs of patients with schizophrenia were $2,863 per patient, among which psychiatric-related costs accounted for 84.1% of the total and schizophrenia-related costs accounted for 62.0%. The costs associated with the treatment of schizophrenia represent a substantial burden on the national insurance budget in the context of People’s Republic of China where the gross domestic product per capita was $3,801 in 2009.26 These costs also represent a significant burden on the individuals or their caregivers.
In the present study, the mean age of the schizophrenia patients was 52.3 years. Although this is the average age for the patients with schizophrenia rather than the onset age, the average age is still higher than that obtained in other results of claims data from Taiwan (39.7 years), Hong Kong (43.0 years), and Germany (48.0 years).17,25,27 The reason for the prevalence of older patients in our sample is that the People’s Republic of China UEBMI system includes people who are employed or retired; hence, the population that dropped out of paid employment at an early age due to the onset of schizophrenia is not captured in our data.
When comparing our results with those published for other developed and developing countries, we observe a large variation in costs. Our estimate of annual treatment costs for the schizophrenia patients in Tianjin, People’s Republic of China, is $2,863 per patient, which is much lower compared to $20,654 (2008) in the US, $8,362 (2008) in Japan, while it is a little higher than $2,600 (2005) in South Korea, and much higher than $702 (2008) in Thailand.19,20,28,29 The annual direct medical costs associated with schizophrenia are consistently substantial across different countries, and the costs in our study are disproportionately high, given the level of economic development in People’s Republic of China.
In the current study, the costs associated with non-medication treatments, primarily due to hospitalization, were the largest component (45.7%) of the schizophrenia-related costs while the costs of medication were found to be a relatively small part (15.4%). The percentage of medication costs was found to be somewhat higher than that in the findings in western countries (1.1%–12%). However, it was much lower than that seen in Taiwan (25.4%).10,17,30 The proportion of medication costs attributed to total direct medical costs varies between countries, as it is a function of individual mental health delivery systems.
In our sample, with respect to the use of antipsychotic medications, more than one-third of the patients with schizophrenia were treated with only atypical antipsychotics and less than one-third were treated with only typical agents. In many western countries, the majority of patients are treated with the newer atypical antipsychotics, as this class of medications is recommended as the first-line treatment of newly diagnosed schizophrenia.31,32 Importantly, 7% of patients in our sample received no antipsychotic medications during the follow-up period. This result would indicate that the non-treatment of schizophrenia is even more of a problem in People’s Republic of China than in the West.
Our results show that more than half of the patients (60.8%) were hospitalized during the 12-month follow-up period and that the schizophrenia-related treatment costs for patients with a hospitalization were eleven times greater than that of the patients who were not hospitalized. For patients with a hospitalization, the mean schizophrenia-related length of stay per admission (112.1 days) is much longer than the average length of stay for all diseases (10.5 days) in People’s Republic of China.33 Moreover, the length of stay for the patients with schizophrenia was greater than that in the finding in Korea (99 days) and much greater than those in many other countries (9.1 days–39.8 days).34–38 However, it was shorter than that reported in Japan (over 700 days) and UK (130.2 days).39,40 While our study provided evidence of the substantial impact of hospitalization, the burden of hospitalization is likely to be even greater due to other intangible or indirect costs. Substantial hospitalization-induced societal costs can arise due to lost productivity, increased family burden, elevated rates of suicide, and other comorbidities.10
In comparison with other countries, the majority of schizophrenia patients are treated in inpatient facilities in People’s Republic of China as indicated in this study by the high rates of hospitalization and long duration of stay. These findings highlight that strategies to avoid hospitalization could be an effective way to reduce the costs of care. Firstly, appropriate choices of effective medications and strategies to improve medication adherence have been shown to reduce relapse rates and improve treatment outcomes.31 Secondly, alternative models of care delivery, such as the increased use of community-based mental health care service, less reliance on inpatient treatment, and greater use of psychosocial rehabilitation could be employed more widely in People’s Republic of China.41
Currently, in People’s Republic of China, there are very few free-standing community psychiatric centers and the outpatient departments in many general hospitals rarely provide services for patients with schizophrenia. The public health care system is focused on the treatment of acute exacerbations of mental illness and less emphasis is placed on community-based approaches to deliver interventions that have been shown to reduce disease severity and prevent relapses or provide rehabilitation care. However, international evidence has shown that community-based programs are an effective means to lower hospitalization rates compared to the hospital-based interventions among people with mental health conditions.42 Moreover, these services have been shown to reduce hospital use by diverting patients from hospital admissions into community-based treatment programs.43,44 In this way, the medical care of patients could be supported and more efficiently designed using innovative outpatient treatment options such as psycho-education, family interventions, specialist nursing care, socio-therapy, treatment provided by visiting patients at home, and care provided by caregivers. Community-based alternatives to inpatient care were shown to be cost-effective.45
The comparison above shows that resource use and their costs do differ by country, depending on how health care financing is structured and health care is delivered, as well as by the incentives and constraints facing individual clinical staff. Country-specific resource utilization patterns along with their associated costs would thus be of interest to stakeholders and policy makers. Based on our results, future investigations could focus on the key drivers of hospitalization in People’s Republic of China that have not been presented here.
Our results should be interpreted with caution for several reasons. Firstly, our sample may not be representative of the population with schizophrenia in Tianjin, People’s Republic of China, as the UEBMI system only covers the population in employment and retirees. Actually, the costs among insured patients might be higher than uninsured patients. Secondly, more detailed socioeconomic information (such as the income level) and clinical information (such as illness severity) are not available in health insurance claims data; so, we were unable to investigate their influence on direct medical costs. Thirdly, our cost analysis was performed using claims data and only direct medical costs were considered. While indirect costs are considered to be higher than direct costs associated with schizophrenia, indirect costs such as loss of productivity and the cost to caregivers were not examined in this study.11
Conclusion
This claims data study estimated the health care resource utilization and the direct medical costs associated with treating patients with schizophrenia in Tianjin, People’s Republic of China. The results indicate that there are significant condition-related and all-cause direct medical costs associated with the treatment of patients with schizophrenia in Tianjin, People’s Republic of China. Costs were primarily driven by high rates of hospitalization and long periods in hospital. Therefore, the efforts focusing on interventions that can improve treatment outcomes, such as programs to improve access to effective medications and medication adherence, and the implementation of community-based treatment programs, may lead to better clinical and economic outcomes in the long-term management of schizophrenia in People’s Republic of China.
Acknowledgment
This research was supported by Eli Lilly & Company.
Disclosure
Wenyu Ye and William Montgomery are minor stock holders and employees of Eli Lilly and Company. Li Liu and Haibo Xue were employees of Eli Lilly and Company at the time this study was conducted. The other authors report no conflicts of interest in this work.
References
Lehman AF, Lieberman JA, Dixon LB, et al; American Psychiatric Association; Steering Committee on Practice Guidelines. Practice guideline for the treatment of patients with schizophrenia. Am J Psychiatry. 2004;161(2 suppl):1–56. | ||
World Health Organization. Schizophrenia and Public Health. Geneva: World Health Organization; 1998. | ||
Phillips MR. Characteristics, experience, and treatment of schizophrenia in China. Dialogues Clin Neurosci. 2001;3(2):109–119. | ||
Bijl RV, Ravelli A, van Zessen G. Prevalence of psychiatric disorder in the general population: results of The Netherlands Mental Health Survey and Incidence Study (NEMESIS). Soc Psychiatry Psychiatr Epidemiol. 1998;33(12):587–595. | ||
National Institute of Mental Health. Schizophrenia?; 2013. Available from: http://www.nimh.nih.gov/health/statistics/prevalence/schizophrenia.shtml. Accessed March 12, 2015. | ||
Phillips MR, Zhang J, Shi Q, et al. Prevalence, treatment, and associated disability of mental disorders in four provinces in China during 2001–2005: an epidemiological survey. Lancet. 2009;373(9680):2041–2053. | ||
Picchioni MM, Murray RM. Schizophrenia. BMJ. 2007;335(7610): 91–95. | ||
Falkai P, Wobrock T, Lieberman J, et al; WFSBP Task Force on Treatment Guidelines for Schizophrenia. World Federation of Societies of Biological Psychiatry (WFSBP) guidelines for biological treatment of schizophrenia, Part 1: acute treatment of schizophrenia. World J Biol Psychiatry. 2005;6(3):132–191. | ||
Taylor M, Chaudhry I, Cross M, et al; Relapse Prevention in Schizophrenia Consensus Group. Towards consensus in the long-term management of relapse prevention in schizophrenia. Hum Psychopharmacol. 2005; 20(3):175–181. | ||
Knapp M, Mangalore R, Simon J. The global costs of schizophrenia. Schizophr Bull. 2004;30(2):279–293. | ||
Wu EQ, Birnbaum HG, Shi L, et al. The economic burden of schizophrenia in the United States in 2002. J Clin Psychiatry. 2005;66(9): 1122–1129. | ||
Andlin-Sobocki P, Rossler W. Cost of psychotic disorders in Europe. Eur J Neurol. 2005;12(suppl 2):74–77. | ||
Chisholm D, Gureje O, Saldivia S, et al. Schizophrenia treatment in the developing world: an interregional and multinational cost-effectiveness analysis. Bull World Health Organ. 2008;86(7):542–551. | ||
Lambert TJ, Velakoulis D, Pantelis C. Medical comorbidity in schizophrenia. Med J Aust. 2003;178(suppl):S67–S70. | ||
Knapp M, Kavanagh S. Economic outcomes and costs in the treatment of schizophrenia. Clin Ther. 1997;19(1):128–138. | ||
Goeree R, Farahati F, Burke N, et al. The economic burden of schizophrenia in Canada in 2004. Curr Med Res Opin. 2005;21(12):2017–2028. | ||
Lang HC, Su TP. The Cost of Schizophrenia Treatment in Taiwan. Psychiatr Serv. 2004;55(8):928–930. | ||
Grover S, Avasthi A, Chakrabarti S, Bhansali A, Kulhara P. Cost of care of schizophrenia: a study of Indian out-patient attenders. Acta Psychiatr Scand. 2005;112(1):55–63. | ||
Chang SM, Cho SJ, Jeon HJ, et al. Economic burden of schizophrenia in South Korea. J Korean Med Sci. 2008;23(2):167–175. | ||
Phanthunane P, Whiteford H, Vos T, Bertram M. Economic burden of schizophrenia: empirical analyses from a survey in Thailand. J Ment Health Policy Econ. 2012;15(1):25–32. | ||
Yang SL, Qian MC, Lu W, et al. Cost of treating medical conditions in psychiatric inpatients in Zhejiang, China. Shanghai Arch Psychiatry. 2011;23(6):329–337. | ||
Zhai JG, Zhao JP, Chen JD, et al. The economic burden of patients with schizophrenia in two hospitals from Hunan and Shandong province (in Chinese). Chin J Psychiatry. 2007;40(1):41–44. | ||
Tianjin Daily 2012. 2013. Available from: http://www.gov.cn/gzdt/2012-05/09/content_2132977.htm. Accessed August 14, 2013. | ||
Hong J, Windmeijer F, Novick D, Haro JM, Brown J. The cost of relapse in patients with schizophrenia in the European SOHO (Schizophrenia Outpatient Health Outcomes) study. Prog Neuropsychopharmacol Biol Psychiatry. 2009;33(5):835–841. | ||
Zeidler J, Slawik L, Fleischmann J, Greiner W. The costs of schizophrenia and predictors of hospitalization from the statutory health insurance perspective. Health Econ Rev. 2012;2(1):9. | ||
National Bureau of Statistics of China. 2013. Available from: http://data.stats.gov.cn/workspace/index?a=q&type=global&dbcode=hgnd&m=hgnd&dimension=zb&code=A020106®ion=000000&time=2009,2009. Accessed March 12, 2015. | ||
Law WL, Hui HY, Young WM, You JH. Atypical antipsychotic therapy of treatment of schizophrenia in Hong Kong Chinese patients – a cost analysis. Int J Clin Pharmacol Ther. 2007;45(5):264–270. | ||
Nicholl D, Akhras KS, Diels J, Schadrack J. Burden of schizophrenia in recently diagnosed patients: healthcare utilization and cost perspective. Curr Med Res Opin. 2010;26(4):943–955. | ||
Sado M, Inagaki A, Koreki A, et al. The cost of schizophrenia in Japan. Neuropsychiatr Dis Treat. 2013;9:787–798. | ||
Garattini L, Barbui C, Clemente R, Cornago D, Parazzini F; Study Group SCORE. Direct costs of schizophrenia and related disorders in Italian Community mental health services: a multicenter, prospective 1-year follow up study. Schizophr Bull. 2004;30(2):295–302. | ||
NICE clinical guidelines. Schizophrenia: Core Interventions in the Treatment and Management of Schizophrenia in Primary and Secondary Care; 2009. Available from: http://guidance.nice.org.uk/cg82/. Accessed August 1, 2013. | ||
Weinbrenner S, Assion HJ, Stargardt T, Busse R, Juckel G, Gericke CA. Drug prescription patterns in schizophrenia outpatient: analysis of data from a German health insurance fund. Pharmacopsychiatry. 2009;42(2):66–71. | ||
Ministry of health China. China’s Health Statistics Yearbook 2011; 2014. Available from: http://wsb.moh.gov.cn/htmlfiles/zwgkzt/ptjnj/year2011/index2011.html. Accessed August 21, 2013. | ||
Stensland M, Watson PR, Grazier KL. An examination of costs, charges, and payments for inpatient psychiatric treatment in community hospitals. Psychiatr Serv. 2012;63(7):666–671. | ||
Tarricone R, Gerzeli S, Montanelli R, Frattura L, Percudani M, Racagni G. Direct and indirect costs of schizophrenia in community psychiatric services in Italy. The GISIES study. Interdisciplinary Study Group on the Economic Impact of Schizophrenia. Health Policy. 2000; 51(1):1–18. | ||
Stargardt T, Edel MA, Ebert A, Busse R, Juckel G, Gericke CA. Effectiveness and cost of atypical versus typical antipsychotic treatment in a nationwide cohort of patients with schizophrenia in Germany. J Clin Psychopharmacol. 2012;32(5):602–607. | ||
Marcus SC, Olfson M. Outpatient antipsychotic treatment and inpatient costs of schizophrenia. Schizophr Bull. 2008;34(1):173–180. | ||
Strutton DR, Gutierrez B, Blanchette CM. Influence of medication treatment patterns on resource use for patients hospitalized for schizophrenia. Am J Health Syst Pharm. 2008;65(1):42–48. | ||
Warner R. Recovery from schizophrenia: an international perspective. a report from the WHO collaborative project, the international study of schizophrenia. Am J Psychiatry. 2007;164(9):1444–1445. | ||
Munro J, Osborne S, Dearden L. Hospital treatment and management in relapse of schizophrenia in the UK: associated costs. Psychiatrist Online. 2011;35:95–100. | ||
McDaid D, Thornicroft G. Balancing Institutional and Community-Based Care. Policy Brief. Belgium: WHO European Observatory on Health Systems and Policies; 2004. | ||
Guo S, Biegel DE, Johnsen JA, Dyches H. Assessing the impact of community-based mobile crisis services on preventing hospitalization. Psychiatr Serv. 2001;52(2):223–228. | ||
Geller JL, Fisher WH, McDermeit M. A national survey of mobile crisis services and their evaluation. Psychiatr Serv. 1995;46(9):893–897. | ||
Zealberg JJ, Santos AB, Fisher RK. Benefits of mobile crisis programs. Hosp Community Psychiatry. 1993;44(1):16–17. | ||
Tanioka T, Chiba S, Onishi Y, et al. Factors associated with discharge of long-term inpatients with schizophrenia in Japan: a retrospective study. Issues Ment Health Nurs. 2013;34(4):256–264. |
 © 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.