Back to Journals » Journal of Multidisciplinary Healthcare » Volume 12
Health care professionals’ experiences and enactment of person-centered care at a multidisciplinary outpatient specialty clinic
Authors Evén G , Spaak J , von Arbin M, Franzén-Dahlin Å, Stenfors T
Received 4 September 2018
Accepted for publication 21 December 2018
Published 14 February 2019 Volume 2019:12 Pages 137—148
DOI https://doi.org/10.2147/JMDH.S186388
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Gudrun Evén,1 Jonas Spaak,1 Magnus von Arbin,1 Åsa Franzén-Dahlin,1 Terese Stenfors2
1Department of Clinical Sciences, Karolinska Institutet, Stockholm, Sweden; 2Department of Learning, Informatics, Management and Ethics, Karolinska Institutet, Stockholm, Sweden
Introduction: Person-centered care (PCC) appears particularly suitable for patients with complex diseases and in multidisciplinary care. However, previous research tends to focus on each profession and condition separately.
Purpose: We studied how health care professionals (HCPs) understand PCC, and whether their clinical practice is aligned with their theoretical understanding, when starting clinical practice at a novel multidisciplinary clinic.
Methods: In total, 16 semi-structured interviews with HCPs and 31 non-participatory observations of outpatient meetings and other activities at the clinic such as team meetings were conducted at a multidisciplinary, integrated outpatient clinic in Sweden. All patients had simultaneous diabetes mellitus, chronic kidney disease and established cardiovascular disease. The clinic employed a PCC approach. Data were analyzed using an inductive thematic approach.
Results: Two key findings emerged. First, PCC requires a holistic view of the patient at all times during care, with everything focused on the patient. This requires that the HCPs know the patient well enough as an individual to be able to tailor the care together with them. Second, working with a PCC philosophy leads to transformed roles for HCPs in patient meetings, with more active involvement by the patient and often also their next of kin. The observations, in comparison with the interviews, showed that not all HCPs applied their views on PCC in patient meetings. Observations showed that some patient meetings were less person-centered than others, potentially due to stress or lack of time.
Conclusion: PCC require HCPs to have a holistic view of the patients and a deeper understanding of their situation, as individuals. Working with PCC also leads to a more coaching, supportive role of the HCPs.
Keywords: person-centered care, multidisciplinary, qualitative research, interviews, observations, thematic analysis, health care professionals, cardiology, nephrology, endocrinology
Introduction
The person-centered care (PCC) approach was introduced in somatic care in the late 1990s, and has remained a research topic since then.1 PCC is based on the patient’s experience, not only of their medical condition but also of their situation in life, resources, and obstacles. PCC is performed in a partnership between the patient, relatives, and health care professionals (HCPs).2 PCC has been shown to considerably improve patients’ perceived quality of life (QoL).2–8 One of the rationales behind PCC is the often-noted discrepancy between the goals of the HCP and the patient regarding the care provided; hence, it is important to include both perspectives.4,9 An example of such a discrepancy was shown in a study by Pittman and McIntyre (2013) on patients with chronic kidney disease and end-stage renal disease. Besides struggling with difficult treatment choices and other medical matters, the patients expressed that they would have liked the staff to also focus on their symptoms and not only the results.10 Previous studies show that PCC is often linked to holistic and compassionate care.11,12
A standard definition of PCC is currently lacking, with terms like “patient-centered care”, “person-centered care”, “shared decision-making”, “relationship-centered care”, and “personalization” seen in the literature, often referring to similar ideas.13–15 Other important aspects emphasized are the patient’s social support and lifestyle wishes, and the notion that everyone working around the patient should work together toward a solution that will suit the individual patient.9,16 The WHO describes PCC as an approach and a way of working so that HCPs are able to visualize the “person as a whole with many levels of needs and goals, with these needs coming from their own personal social determinants of health”.5
Many studies have shown that patients would like to participate in their care to a greater extent than they currently do17–23 and other studies indicate that patients have varying desires for involvement and information about their illness, as well as the options for available treatments.17,19–21,24–26
A number of studies have highlighted that there are differences in the extent to which PCC is suitable for all patient groups depending on age, education, ethnicity, or diagnosis, but there seems to be no consensus.19,25,27–30 A few studies have indicated that younger patients were more keen to ask more questions and get more information,27 and a higher level of education most likely had an impact on participation.25,27
In a report by the Institute of Medicine, Committee on Quality Health Care in America,26 most HCPs stated that their way of working was PCC; however, the patients reported frustration regarding their chance to participate in their own care. Several studies show that HCPs need to shift focus to be more oriented to the patient’s own values, thoughts, and experiences of their illness, to be more person-centered2,31–33 rather than based on prevailing norms.34 Previous research points out that HCPs’ own understanding of PCC is of relevance when providing safe care of good quality.35 Studies show that working with a PCC approach challenges the HCPs as they need to adopt another way of working, taking on the role of facilitator.36,37 HCPs being motivated and interested in PCC is important for practicing it.32 In some studies, PCC has been positively associated with a good working environment and the HCPs’ experience, knowledge, and interest in the approach.35,38,39 Some HCPs reported the importance of allowing enough time for developing effective teamwork and creating a good environment when implementing PCC.40 It was also found that support from the management was of great importance for the HCPs40,41 as well as the need for proper educational training.41
Based on previous research, there is a need to understand HCPs’ knowledge about and experiences of PCC, and whether their clinical practice is aligned with their theoretical knowledge. This aim of this study was to meet this need.
Methods
Study design
This study combines interviews and observations held at a multidisciplinary, integrated care outpatient clinic. The HCPs worked with the overall aim of delivering PCC. To gather more information about how and to what extent the HCPs were working with a person-centered approach as they claimed they were, non-participatory observations were conducted. All HCPs who were observed were also interviewed. An inductive thematic approach was used to analyze the data.42
The study was approved by the Regional Ethics Committee in Stockholm, Karolinska Institutet, Dnr: 2014/384-31/1. The study adhered to the Declaration of Helsinki of ethical principles for medical research on humans. The participation in the study was voluntary and the informants were able to withdraw their participation at any time. The first author had not previously worked closely with the informants.
Settings
Danderyd University Hospital provides acute and specialized medical treatment to over half a million patients. In November 2013, the hospital started a person-centered, multidisciplinary outpatient clinic for persons with combined cardiovascular disease, impaired kidney function, and diabetes. The HCPs at the integrated clinic (the clinic) consist of physicians and registered nurses (RNs) who specialized in cardiology, nephrology, and endocrinology. This study was conducted at the clinic from February to October 2016. Clinicians at the clinic work there part-time, and part-time at other hospital departments. The clinic was the first department of the hospital to work explicitly with a person-centered approach, and at that point in time the hospital did not have a specified definition of PCC. Hence, the clinic used a definition of PCC as described by WHO.5 At the opening of the clinic, most of the staff attended a 1-day training course on PCC and integrated care. All HCPs in this study, except one, work there out of their own interest. The latter HCP was there due to sick leave.
Data collection
Non-participatory observations
The study was conducted using a non-participatory observation technique.43 The intention was to capture the dynamics of the interactions in the different types of meetings from a PCC perspective. The observer, being a nurse, had the advantage of having the knowledge to understand everything said during the observations and perhaps found it easy to blend into the hospital environment and also in the group of other HCPs at the clinic. The observer used an open exploratory approach without a predetermined format. This was considered the best approach to increase the understanding of how the staff worked and also to capture authentic examples from the staff’s clinical work.
During the observations, extensive notes were taken. Shortly after each observation, the notes were written down in full, with additional comments such as “patient sighs”, “the doctor nodded”, or “the interpreter interrupted the conversation”.
First, the HCPs gave their consent to participate verbally, after being informed about the study in advance by the head nurse and the researcher and asked by the receptionist the same day the observation was performed. Then, each patient, upon arrival at the clinic was given an information sheet regarding the purpose of the study and the methods, at which point the patient could consent or decline to participate verbally. The observations were made on different days of the week and at varying times during the day. The clinic did not know in advance when the researcher was scheduled to be there, and the researcher did not know what kinds of patient visits were scheduled.
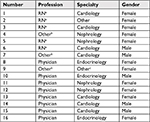
A total of 37 patients were screened for inclusion. Two patients did not want to participate; the nurse in charge declined three patients, claiming they were not fit enough to participate; and one patient was known to the researcher. Thus, 31 patients were ultimately included. The researcher conducted all observations, the length of which varied between 24 and 66 minutes (mean 42.5 minute); see Table 1.
  | Table 1 Baseline characteristics of patients in the patient meetings Note: Values describe mean (range). |
At 13 of 31 observations both nurses and physicians were present, attending so-called “team meetings”. At ten meetings, there was also a nursing student or nurse assistant in attendance, but they did not speak or interact with the team. At 19 meetings a family member was present, and at 3 meetings an interpreter was present (see Table 2). Of note is that the number of female patients was significantly lower. However, this correctly reflects the patient population at the clinic, the reason being that males develop cardiovascular disease an average of 10 years earlier than females. In the 31 observations, there were 6 different professions presented. All but one, were employed at the hospital. The interpreters were from an external agency procured by the county council. After 31 observations (22 hours), it was decided that all the data needed to inform our research question was collected.
In addition to the consultations, the researcher attended other activities at the clinic amounting to about 40 hours; ie, staff meetings, coffee and lunch breaks, site meetings, telephone calls with patients, examination of vital parameters, and administration of prescribed drugs.
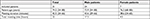
Semi-structured interviews
All the HCPs working at the clinic at that time were interviewed. Sixteen interviews were conducted, with eight physicians and eight nurses or nurse assistants. There were eleven female and five male informants. The physicians were specialists either in cardiology, nephrology or endocrinology, and the nurses were specialists in cardiology and nephrology (see Table 3). As there was a vacant position for a diabetes care nurse at the time the study was conducted, there was no nurse at the clinic with specialist training in diabetes. The interviews varied from 13 to 33 minute (mean 21.1, SD ±6.3). All interviews were conducted by the researcher and audio-recorded. Shortly after the interviews, they were transcribed verbatim. After each of the first five interviews, the transcripts were read by three researchers and the interview guide was slightly modified. The interview guide focused on exploring the HCPs’ understanding of PCC and their experiences of working with it.
Analysis
The analysis of the interview transcripts and the observation notes was done with an inductive thematic approach.42 The first author transcribed all interviews as well as the observations notes. One of the authors compared the transcribed data with the recordings to make sure there were nothing omitted. Two of the authors read the transcripts several times, and then an initial coding was done for the entire set of data and discussed among the researchers. The coding was discussed, agreed upon, and revised several times throughout the process. Codes formed so-called “working titles”, ie, themes based on similarities and relationships. The themes were discussed, reiterated and merged, and finally named. The approach used can be described as an inductive semantic method of coding that is close to the original texts. To categorize and analyze the data, NVivo 11 Plus for Windows (https://www.qsrinternational.com/nvivo/home) was used.
Results
The analysis resulted in two main themes revolving around the holistic view of the patient and the transformation in the roles of the HCPs when starting to work at the clinic with a strict PCC approach (Figure 1).
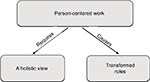  | Figure 1 Themes developed from the analysis. |
PCC requires a holistic view of the patient
In the interviews, the HCPs talked about the importance of looking at the patient as a whole person and treating them as such. This could also be seen in virtually all the observations. The intention of all the HCPs was to adopt a holistic approach, which included considering the patient’s diseases, family situation, living conditions, and so on. The staff also reported that they were trying to capture other things regarding patients, for example, by asking about their hobbies, whether they had any pets, or about their dietary habits. Many reported that they needed to collect all kinds of information about the patient to get this overall picture. Having this holistic view of the patient was important to, and a common opinion, among the HCPs.
Who is the patient sitting in front of me?
In the interviews, the HCPs all claimed to strive to find out who the patient was as a person and what kind of life they lived. However, when the interviews were compared with the observations, in a few observations it was found that the staff did not ask any other questions than those important for that specific meeting; the focus was only on medical issues. Still, most of the staff reported that the collection of different kinds of information was of great importance in order to get the whole picture of the person. Letting the patient tell their own story was often regarded as the start of the partnership. The goal was to customize the health care for that unique person who was sitting in front of the HCP, to achieve the best QoL for them. One physician mentioned the economic aspect of prescribing drugs:
Some drugs are very expensive, and some are cheaper. Then we’re sitting there believing this drug is good and we prescribe it, while the patients may be too embarrassed to say they can’t afford to buy this. Later they go to the pharmacy and find out that it’s very expensive, and they don’t pick up the prescription. We usually don’t know that. It’s important to understand the whole situation. [Physician, male. Informant 10]
During the observed meetings, almost everyone on the staff tried to capture the patient’s daily situation to form the best solutions for that particular patient. This was often done with the assistance of the patient’s next of kin:
Relative: They want to know how you’re doing and how you feel.
Nurse: Are you staying home more now?
Patient: Yes, definitely!
Nurse: How about yesterday. What did you do yesterday?
Patient: Well, what did I do […] Podiatrist […] Clean, nice feet now […] The cleaning lady came, then I keep out of the way. I’ve worked with the stock market, made my share.
Relative: Well, you didn’t do that yesterday […]
Nurse: I’m asking how your current situation is, here and now, and based on that will try to see how we can help you. That’s why I’m asking. [Observation 1]
In almost all observations the physicians reviewed the patient’s list of prescription drugs very carefully. Together with the nurse, the patient, and the next of kin, every single drug was explained and discussed in a highly elucidative way. This was later explained by one physician as being a way to capture the patient’s cognitive status and determine whether they needed assistance in administering the drugs.
Patient capability and desire
In the interviews, many of the HCPs mentioned the importance of exploring the patient’s capability. This, according to all informants, was also the clue to getting to know the patient and working together toward a better QoL. In the meetings, the researcher observed that the patient often had a goal of their own, and with assistance from the staff, adjustments were made to meet the criteria for good health care and a solution that everyone could agree on. Some reported difficulties working with cognitively challenged patients, since good communication was considered necessary for providing PCC. This was also noted in some observations:
At the end it turned into a discussion between the wife and the physician. The physician had told me beforehand that the wife was the one doing the talking, so I was prepared, but that much talking […] And it didn’t get any better with them not finding his hearing aid. The physician didn’t establish any contact with the patient despite several attempts. [Observation 10]
However, one informant held the opposite view: even patients with cognitive disabilities could and would benefit from PCC. They claimed that when you got to know the patient a bit more you were able to understand, in a way, how your patient would like to be cared for even though they were not able to express this explicitly. Sometimes it was seen as the responsibility of the staff to speak up for those who were less privileged:
For me, person-centered may be that I ask how you want to do things. Do you want me to put the right shoe on first, or the left? What’s easiest for you? Which side of the bed do you want to get up on? Even someone with serious cognitive decline can answer these questions. ‘Yes, maybe I’d rather get up on the right side.’ Maybe they’re not always 100% with me, but they’ve at least be participating in the care in another way. [Nursing student, female. Informant 9]
The staff reported feeling anxious about allowing the patient to decide the goal. It could not be a goal that went against medical knowledge; if it was, the HCPs would object. Using the patients’ chosen goal would therefore be an educational challenge. Sometimes the goal set did not amount to much, but it was nevertheless the patient’s own goal or decision. Some informants believed their own attitude would be an impediment to using the patient’s capabilities to the utmost. They reported the difficulties presented by not falling back into the traditional way of caring:
And then of course I want to know if there’s something specific the patient needs at the moment. And it can be anything from an extended certificate for sick leave, more prescriptions, to their wish to have a better understanding of why they feel like they do. And how to live in order to feel better, and such things. So, it can be very extensive. [Physician, male. Informant 15]
Transformed HCP roles
Some of the staff talked about the changed professional roles they felt came with implementing PCC as their new work approach—from acting as the leader in the decisions to becoming an advisor, expert, and partner. Some described it as sometimes even feeling that they “took on the role of negotiator in the medical decisions”. It was described as important to adopt this role in order to allow the patient to feel that they, in fact, had the last say in the matter. This was important to the staff, as they needed to feel that the decisions reached were in line with their medical or caring professional knowledge:
And then to some extent […] loosening the reins, the control mechanisms so to say, letting the patient speak first, or be the first, before you bring up everything else, is to re-evaluate our roles a bit. From being physicians giving directives, ‘do this or that’, to becoming more like experts giving advice, trying to make the patients themselves achieve understanding that they should do this, and that, and that […] ‘oh, my blood pressure’s high, I’d like it to be better, so I’ll contact my cardiologist XX, to find out how […] how to get better blood pressure’. [Physician, male. Informant 15]
Failing to achieve their target may be an obstacle since patients prioritize certain things and we need to respect that, but a patient doesn’t have the full understanding, and neither do we, so we need to meet halfway. We need to compromise sometimes when there are things we recommend that the patient definitely doesn’t want to do, but the patients also need to compromise, for instance taking the insulin they need in order to be able to live on without complications. Sometimes they need to lose weight to reduce further complications and damage, and they also need to compromise. If neither of us is prepared to back off a bit, we might stall. [Physician, male. Informant 10]
The HCPs reported that their new roles were sometimes hard to handle, depending on the patient and the other staff members at the meetings. A few talked about having different approaches depending on which patient they were seeing. Some felt that certain patients would prefer a traditional approach to care, with the physician leading the meeting and them, as patients, taking a more passive role:
I believe, despite everything, that the patient maybe expects the physician, eh, […] to have that role. I believe there are lots of traditional [roles] for both nurses and physicians as well as patients […] so I, I believe it can be good. I believe it gives a feeling of safety. [Nurse, female. Informant 5]
One nurse described in the interview that, depending on the physician, she fell into a more passive role at the team meetings compared to the individual nurse meetings. This nurse also mentioned that the patient the nurse was observed with, never actively participated in any meetings. Some of the informants mentioned that identifying the daily routine was a key component to discerning parts that could be possible goals for the patients. For example, one RN talked about the meaningless effort of discussing dietary changes with a patient when it is in fact the patient’s partner who is in charge of all the cooking in the household.
Transformed meetings
In the interviews, almost every informant mentioned that working with a PCC approach also changed the meetings with the patients. It was reported that they lasted longer compared to previously, when they only focused on the medical aspects.
The observations showed that many, but not all, meetings started with an open question about how the patient was feeling that day, and whether there was something specific they would like to talk about. The patient’s agenda drove the meeting. Of course, the staff had a plan for what they wanted to discuss, but sometimes their agenda completely changed due to the patients’ condition or wishes:
... but it requires that you have time for the visits to be able to work in this way, at least that’s the feeling. It may not take a longer time in reality, but it feels like it does. Since you cannot plan and run your own race, you have to preferably check everything with the patient. If you’ve asked them what they’d like to discuss, then you actually have to spend the consultation, a large amount of time, on that topic. [Physician, male. Informant 14]
Some of the staff said they used a conversation technique inspired by motivational interviewing. The idea was to get the patient to understand and offer suggestions for what to do in order to achieve the goals, so they could have a better QoL. In the observations, the researcher found that in more than half of the meetings the patient’s own questions were ignored, with the staff continuing the conversation as if the question had not been asked and the patient not getting an answer. These questions generally concerned medical and social issues, lifestyle, and prescribed drugs:
Patient: I’m not so good at writing with my right hand after the stroke.
Physician: It’s amazing how one can recover after a stroke. [Observation 24]
In one observed meeting, the staff used medical terminology in a way that was not properly understood by the patient and the next of kin:
Physician: When you adjust [the doses] on your own it becomes a problem. It is 75% direct acting, and 25% other. You get a problem […] let’s see […] after the conference […] Have you ever had a serious hypoglycemic attack?
Patient: Glyce ….? [Observation 21]
Physician: Then we’ve reviewed […] I hope we got everything […]. (turns to patient’s next of kin) Do you feel like we covered everything?
Next of kin: Maybe not the social aspect. I work full-time.
Physician: So, you have no domestic care? And the memory problem? We’re a bit short of time […] After the team conference we’ll likely make some adjustments to the medications. Could you provide a urine sample? We’ll send it for a culture. We’ll also discuss how to help you become more active. The nurses are good at that. We’ll also do some more bloodwork.
Next of kin: [The patient] has always been so active, and now nothing. It’s wearing him down!
Physician: Why is that, do you think?
Next of kin: His diseases.
Physician: General decline? OK. Good. Then we’re done. We’ll get back to you after the conference. Next visit in about three months (talking the whole time while exiting the room). [Observation 21]
According to the HCPs, the PCC approach mostly concentrated around the narrative and getting to know the patient and their life situation. At all meetings except two, all those in attendance sat together, listening and discussing how to improve the patient’s QoL. From the observer’s point of view, it looked like sitting around a table, discussing together, was a success since it made the meeting a bit more familiar and intimate. At the other two meetings, the physician sat behind the computer the entire time and did not once make eye contact with neither the patient nor the other attendees:
Physician: How are you doing?
Patient: Great!
Physician: Aha […] hmm (reading from the computer screen).
Patient: Yes, except for the cold I had, I usually walk down to the GP’s office and cycle once a week.
Physician: Aha […] (still on the computer)
Patient: They did an X-ray and found out that the nerves in the spine were impinged.
Physician: Hmm […] (still on the computer)
Patient: I noticed it for the first time when I was in Prague. Had a TIA [transient ischemic attack] there.
Physician: Aha […] hmm […] (still on computer).
Patient: I never went to the doctor, since we were going home the day after.
Physician: Hmm […] (still on computer).
Physician: If we focus on what they said at the conference (now turning towards the patient). I’ll get back to you about the kidneys and give an exact answer about how to interpret the urine samples. Regarding the heart, they haven’t done much more than adjusting the drugs. I’ll get back to you regarding this and about when to see you next time. Anything else?” [Observation 22]
Physicians reported anxiety regarding the need for enough time with the patients, and a lack of time was considered an obstacle to reaching a good level of person-centeredness. Other perceived obstacles for PCC were language or cultural barriers, a lack of competence among patients and staff, cognitive or mental impairment, and costs. A few informants stated that a big problem was unwillingness to change: regarding both the patients’ unwillingness to sacrifice anything in their lifestyle and the staff’s unwillingness to change their way of working to adopt the concept:
Well, there are colleagues […] who don’t understand that […] we’re here for the sake of the patients, not our own. [Nurse, female. Informant 2]
We’re very keen on having them take an active part and understand. […] but some are not receptive to understanding how important this is. Or maybe because they do not want to. [RN student, female. Informant 9]
Some of the more senior [staff] may say ‘I’ve always worked like this, and I won’t change’, while maybe newly graduated [staff] who have just studied person-centered care may be very keen on it. But for some it could be the other way around. [RN student, female. Informant 9]
As mentioned in the interviews, adopting the new approach and the new role was not always easy. Concerns regarding the documentation in the patient’s medical journal were a topic of discussion. A few of the informants felt that the electronic medical journals were not sufficiently updated to adopt the new approach:
The medical records aren’t quite adapted to this, we document the same way as on other […] [wards]. [Nurse, female. Informant 3]
HCPs as coaches – meeting patients where they are
Almost all HCPs in the study felt that a key component in this new approach was trying to meet the patient where they were that particular day. If they reached this goal, they were more able to know what they could do, and how, in order to make an improvement in the patients’ life. Some HCPs said it was not very easy to figure this out; it all came down to the patient’s own wishes and desires. Almost all the physicians mentioned that they spoke differently with patients depending on their social background and educational level:
For some we have to keep it very basic, while others are fully self-educated from the Internet on their diagnoses and know as much as we do. […] this places very different demands on us. [Physician, female. Informant 13]
[…] for instance, for an engineer we can be very detailed on how the muscles absorb glucose from the blood during physical activity, but if the patient has a different background we have to adjust the education we provide. [Physician, male. Informant 15]
One thing a few of the informants mentioned was the act of directing the patient to the right course “medically”. For instance, one informant talked about getting the patient to understand that some dietary changes would not show immediate results, but in the long-term would make the patient feel better. It was also mentioned that there was a struggle not to cut the patients off in an attempt to be helpful. There was a perceived need to wait for the patients to think and suggest changes themselves:
I try to work as person-centered as possible, but I often find myself putting words into the patient’s mouth and deciding for them. [Physician, male. Informant 15]
It’s often necessary to get the patient or person to understand that we want the same thing. It’s an educational challenge. To try to make the person in front of you understand that we need to, for instance, improve the blood glucose levels. Not because it’ll make you feel better today, but because if you don’t it’ll make you much worse in the future. [Physician, male. Informant 15]
In the interviews, almost every informant highlighted, that they wanted more training in the PCC approach as well as in motivational interviewing. One nurse talked about one way to get patients’ attention, by simply asking what they normally do on an ordinary day. In their reply, the nurse often picked up on the little things that could lead the way to the goals for the patients:
‘How do your daily activities work for you?’ And then you get some clues. ‘Yes, earlier I could walk the dog twice a day but now I have to ask for help.’ Then maybe you can help. ‘Yes, do you think we can make you […] take all the stairs at once, or something? Would you like to get out with the dog twice a day again? Do you think this is a reasonable target?’ [Nurse, female. Informant 3]
One informant specifically mentioned that in the patients’ narratives she could often get clues about what they were, in fact, bothered about:
If the person says that […] well I’ve gained quite a lot of weight, then this reflects their own concerns, and then we can continue discussing that particular issue. [Nurse assistant, female. Informant 4]
In the interviews, almost everyone talked about the importance of the narrative. It was found to be a new and important part of PCC:
[…] trying to understand […] to find the person’s resources. Not everybody participates that actively though […] they’re not very used to talking about themselves […] find it difficult or do not want to. Then we have to respect that, that’s person-centered from another perspective […]. (Nurse, female. Informant 3)
It was not always the medical issues that were the topic of the agenda. Sometimes the meeting took an unexpected turn, and to build rapport with the patient the HCPs needed to listen to them and set other goals for the meeting that day, otherwise the patient was not able to move on. Their thoughts were elsewhere, and they could not focus at all:
Patient: I’m mostly sad for her sake. Now I feel […] (rubs eyes). It was another woman who had ordered a new table. It was awful. I told her to stop but she said they wouldn’t break her […] but they did. […]. [Observation 19]
Engaging relatives
For all the HCPs, working with a PCC approach also included engaging the patient’s family and next of kin. Next of kin were always invited to attend meetings and teaching classes. The HCPs felt they should also be included in order to achieve improvement in the QoL of the patient and his/her family:
Next of kin: Since we’re discussing this topic […] we’ve thought about pre-packaged drugs.
Patient: Have we?
Next of kin: Yes, and you said I could decide. It feels it’s about time.
Patient: As usual, I don’t get it.
Next of kin: Just do as I tell you, and it’ll be fine.
Physician: Pre-packaged drugs are actually not a bad idea. So, ultrasound of the bladder now right away, new bloodwork next week, and the next visit during week 26. [Observation 13]
In the observations, it was noted that when there was a family member present the patients seemed to take on a more passive role. At one meeting, where the patient was accompanied by two adult children, the patient could hardly speak at all, as the children dominated the conversation, likely with the best of intentions.
Discussion
We studied how HCPs experience and enact PCC at an integrated outpatient multidisciplinary clinic. The main results of the study revolve around the notion that working with a PCC approach often presumes a holistic view of the patient, and can also lead to changed roles. The HCPs describe that they adopt a new, more coaching role in this new approach. All the informants state that listening and talking to patients is the most important part when meeting with them. At these meetings, the HCPs, next of kin and the patient together form the goals for the treatment and care. It all comes down to helping the patient understand and take the lead in their own health; certainly, with the help of the HCPs and their next of kin. This indicates that the families need to take on a new role,26 as do the HCPs. The HCPs in this study (like those in previous research) indicated that the HCPs knew their previous roles in their normal context, but needed guidance or support when adopting a new approach whereby their role developed more into that of a facilitator.36 Some HCPs in the study mentioned that they used the team conferences for support, but also suggested that scheduled training would be of relevance.
According to our findings, the HCPs are fully convinced that PCC is the optimal approach for this patient group. They also convey a belief that almost all patients would benefit from PCC. Patients need to be capable and take an active role in the partnership. One informant mentioned that you can use this approach even with patients with cognitive impairment, but in a different way, ie, talking to their next of kin and getting to know the patient through them. In doing this, you will be able to learn about the patients’ habits and wishes. Previous research shows that PCC might be better suited for younger and more educated persons,25,27. This study stated that HCPs found the approach very suitable for capable patients with a willingness to strive for a better QoL.
Some HCPs mentioned the complexity in shifting their way of working and that there are many work-related issues to consider, such as medical records and administrative routines. Implementing a new concept at a hospital is surely a challenge.12 The traditional way of working was not always well adapted to the new approach; one example given by the HCPs was that the medical records had not been updated to suit PCC. Suggested improvements included a combined medical record template that both RNs and physicians could use.
Previous research shows that working with PCC requires a holistic view of the patient,11,12,32 therefore, getting the right HCPs could be an important component in getting everything on track. In this study, it was reported that HCPs in traditional settings are sometimes unwilling to change, claiming that they have always worked in a particular way and it has worked out nicely. The HCPs in the study mentioned that HCPs must take an interest in adopting this new way of working. Previous research indicates that an understanding of PCC was important to the HCPs.12,32,35 Almost all the HCPs in this study, at their own initiative, had applied for a position at this clinic based on their own interest. One HCP was scheduled to work at the clinic when a colleague suddenly became sick, and this HCP was not interested in PCC at all. The new approach also includes working together with the patient’s next of kin in a different way. As one RN mentioned, there is no point in spending time at the meetings talking about dietary changes when the patient does none of the cooking in the household; rather, it is better to wait until the partner who, in fact, does the cooking is there. The HCPs found that getting to know the patient and their social situation is helpful in deciding on different kinds of solutions. This means that some HCPs found that there is no point in proposing things that the patient is not able to do, from an economic, social, nursing, or medical perspective. If the patient needs something, it must be proportional to their ability. For example, if monetary barriers arise, HCPs may suggest solutions to manage them if they know the situation the patient is in. The importance of building a special partnership with the patient according to PCC has also been found in previous research.12,35
Some of the HCPs mentioned that PCC was more time-consuming, at least in the beginning. The meaning of PCC is that from a longer perspective it will save time for both patients and HCPs. In traditional care, before even meeting the patient the HCPs have read their medical journal and often already decided what the problem is, only based on this reading. The patient’s questions are in less focus, since the HCPs must finish the meeting on time as other patients are waiting and there is a tight schedule at the clinics. Working with PCC and letting the patients decide the agenda more or less forces the HCPs to listen to them in a different way.
In an ideal PCC meeting, the patient is the one who decides what subject to discuss. The patient must feel that their problem will be taken care of. Traditionally, in health care settings, HCPs do not always strive to reach an understanding with the patient. In PCC, the understanding and the teamwork provide for a good relationship and create the possibility for the patient to have good compliance in their medications, for example, and to therefore be alert to side effects and other problems: it is based on the patient understanding their condition.
As part of the aim of this study, a comparison was made of the observations and the interviews, and the discrepancies noted were few. The HCPs all understand PCC and how it will be implemented in the daily work at the clinic. However, in some senses, there were differences. In all interviews the HCPs said that they started the meeting with an open question, asking the patient what they would like to talk about or how they felt. However, studying the observations showed that this was not true as a few HCPs did not. Even if the HCPs’ intentions were good, one could note that they often did not wait for the patient’s answer or truly listen to what they said. This was clearly seen when observing a particular HCP, who used terminology the patient did not understand and only sat at the computer for the entire meeting, reading from the medical journal. Inadequate staffing, found to be a barrier to working with PCC,32 was also mentioned by some of the HCPs in this study. Some HCPs pointed out that proper training about the concept of PCC was needed. They all had to use self-study to improve their skills, and it might be noticed in the observations, as they, to some extent, had slightly different ways of working.
Methodological considerations
The strength of this study is the combination of interviews and observations. The researcher was able to observe whether the HCPs actually worked person-centered as they reported. The majority of the observations were done before interviewing the staff. This was an advantage, since informants were not able to act in some particular way they perceived to be pertinent to the study as they did not know the specifics of the topic. Another strength was that everyone who was observed was also interviewed. Being a single observer is perhaps also a limitation due to the fact it is only one person’s observations. In this study, the observation material was discussed with the co-authors throughout the observation period. The combination of methods also strengthens the validity and reliability of the study.44 In regard to the number of observations conducted, the continuous analysis indicated that enough data had been gathered to inform the research aim.
Being an RN, the observer (ie, the first author) had the advantage of having the knowledge to understand everything that was said during the observations. However, this could place a certain bias when understanding the observations. Being an HCP perhaps also made it easy to blend in to the hospital environment as well as the group of other HCPs at the clinic. As the clinic treat patients with combination of three major types of diseases, it is a very complex medical and nursing challenge. One limitation is that the study only explores the HCPs’ experiences and enactment of PCC at one clinic and hence the findings may not directly be transferable to other settings. However, the study may be helpful in other areas when introducing PCC or as a part of further PCC training.
Future research
This study highlights the experiences of PCC from the HCPs perspective and its application in clinical practice. It is also important to study the experiences of the patients and their next of kin, in order to get a better understanding of the PCC approach. There is a need for more research highlighting the views of the HCPs in other settings.
This study raises new questions regarding working with PCC, such as “What components enable a successful way of working with PCC?” “Is PCC dependent on the HCPs that provide the care?” “Does PCC result in improved patient outcomes?” “How do patient perceptions of PCC compare with HCP perceptions?”
Conclusion
According to the HCPs, working with a PCC approach means that everything and everyone is gathered around the patient. The HCPs assumed that this means you need to have a holistic view of the patient at all times during the care. You must get to know the patient well enough to be able to tailor unique care to each patient. The HCPs’ intention is to get to know the patients and their wishes, needs and capabilities, as well as their knowledge about their diseases. Working with PCC also leads to altered roles whereby the HCPs need to meet the patient in their current situation and state of mind, on that particular day. It also means other approaches to conversations and meetings, and involving the patient’s next of kin in a different and more active way in the care. Some HCPs claim that this approach was not new to them, but is rather in line with how they have always cared for their patients. The study showed some discrepancies in the observations vs the interviews, as some HCPs did not apply their views in their meetings with patients.
Acknowledgments
This work was supported by Danderyd University Hospital, Department of Emergency Medicine, Emil och Wera Cornells Stiftelse and Signe och Olof Wallenius Stiftelse.
Disclosure
Dr Spaak and Dr Stenfors received funding from the regional county (ALF) and from the Kamprad Family Foundation. Dr Spaak received funding from Vårdalsstiftelsen and Karolinska Institutet. The authors report no other conflicts of interest in this work.
References
Jayadevappa R, Chhatre S. Patient centered care—a conceptual model and review of the state of the art. Open Health Serv Policy J. 2011;4(1):15–25. | ||
Ekman I, Swedberg K, Taft C, et al. Person-centered care—ready for prime time. Eur J Cardiovasc Nurs. 2011;10(4):248–251. | ||
Stewart M, Ryan B, Bodea C. Is patient-centred care associated with lower diagnostic costs? Healthc Policy. 2011;6(4):27–31. | ||
Gill PS. Patient engagement: an investigation at a primary care clinic. Int J Gen Med. 2013;6:85. | ||
World Health Organization. WHO Global Strategy on Integrated People-centred Health Services 2016–2026. Executive summary. Geneva, Switzerland: WHO; 2015. | ||
Harding E, Wait S, Scrutton J. The State of Play in Person-centred Care: A Pragmatic Review of How Person-centred Care is Defined, Applied and Measured, Featuring Selected Key Contributors and Case Studies across the Field. London: The Health Policy Partnership; 2015. | ||
de Silva D. Helping Measure Person-centred Care: A Review of Evidence About Commonly Used Approaches and Tools Used to Help Measure Person-Centred Care. London: The Evidence Centre; 2014. | ||
Sahlen KG, Boman K, Brännström M. A cost-effectiveness study of person-centered integrated heart failure and palliative home care: based on a randomized controlled trial. Palliat Med. 2016;30(3):296–302. | ||
Sepucha KR, Levin CA, Uzogara EE, Barry MJ, O’Connor AM, Mulley AG. Developing instruments to measure the quality of decisions: early results for a set of symptom-driven decisions. Patient Educ Couns. 2008;73(3):504–510. | ||
Pittman ZCL, McIntyre CW. A systematic exploration of individual haemodialysis patient preferences for treatment outcome: symptoms or survival. J Am Soc Nephrol. 2013;24(Abstract FR-OR013):39A. | ||
Sharp S, McAllister M, Broadbent M. The vital blend of clinical competence and compassion: how patients experience person-centred care. Contemp Nurse. 2016;52(2–3):300–312. | ||
Ogden K, Barr J, Greenfield D. Determining requirements for patient-centred care: a participatory concept mapping study. BMC Health Serv Res. 2017;17(1):780. | ||
Goodrich J, Cornwell J. Seeing the person in the patient. The King’s Fund: London; 2008. | ||
Goodrich J. Exploring the wide range of terminology used to describe care that is patient-centred. Nurs Times. 2009;105(20):14–17. | ||
The Health Foundation. Person-Centred Care Made Simple—What Everybody Should Know About Person-Centred Care. The Health Foundation; London: 2017. | ||
Calisi R, Boyko S, Vendette A, Zagar A. What is person-centred care? A qualitative inquiry into oncology staff and patient and family experience of person-centred care. J Med Imaging Radiat Sci. 2016;47(4):309–314. | ||
Kirk P, Kirk I, Kristjanson LJ. What do patients receiving palliative care for cancer and their families want to be told? A Canadian and Australian qualitative study. BMJ. 2004;328(7452):1343. | ||
Ward MM, Sundaramurthy S, Lotstein D, Bush TM, Neuwelt CM, Street RL. Participatory patient–physician communication and morbidity in patients with systemic lupus erythematosus. Arthritis Rheum. 2003;49(6):810–818. | ||
Bastiaens H, van Royen P, Pavlic DR, Raposo V, Baker R. Older people’s preferences for involvement in their own care: a qualitative study in primary health care in 11 European countries. Patient Educ Couns. 2007;68(1):33–42. | ||
Fallowfield LJ. Treatment decision-making in breast cancer: the patient-doctor relationship. Breast Cancer Res Treat. 2008;112(S1):5–13. | ||
Kvåle K, Bondevik M. What is important for patient centred care? A qualitative study about the perceptions of patients with cancer. Scand J Caring Sci. 2008;22(4):582–589. | ||
Alharbi TS, Carlström E, Ekman I, Jarneborn A, Olsson LE. Experiences of person-centred care—patients’ perceptions: qualitative study. BMC Nurs. 2014;13(1):28–28. | ||
Ridd M, Shaw A, Lewis G, Salisbury C. The patient–doctor relationship: a synthesis of the qualitative literature on patients’ perspectives. Br J Gen Pract. 2009;59(561):e116–e133. | ||
Coulter A. Do patients want a choice and does it work? BMJ. 2010;341:c4989. | ||
Flynn KE, Smith MA, Vanness D. A typology of preferences for participation in healthcare decision making. Soc Sci Med. 2006;63(5):1158–1169. | ||
Institute of Medicine Committee on Quality of Health Care in America. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington (DC): National Academies Press (US); 2001. | ||
Siminoff LA, Graham GC, Gordon NH. Cancer communication patterns and the influence of patient characteristics: disparities in information-giving and affective behaviors. Patient Educ Couns. 2006;62(3):355–360. | ||
Cassileth BR, Zupkis RV, Sutton-Smith K, March V. Information and participation preferences among cancer patients. Ann Intern Med. 1980;92(6):832–836. | ||
Hibbard JH, Greene J, Tusler M. Improving the outcomes of disease management by tailoring care to the patient’s level of activation. Am J Manag Care. 2009;15(6):353–360. | ||
Volandes AE, Ferguson LA, Davis AD, et al. Assessing end-of-life preferences for advanced dementia in rural patients using an educational video: a randomized controlled trial. J Palliat Med. 2011;14(2):169–177. | ||
Aoun SM, O’Brien MR, Breen LJ, O’Connor M. “The shock of diagnosis”: qualitative accounts from people with motor neurone disease reflecting the need for more person-centred care. J Neurol Sci. 2018;387:80–84. | ||
Pelzang R, Wood B, Black S. Nurses’ understanding of patient-centred care in Bhutan. Br J Nurs. 2010;19(3):186–193. | ||
Schoot T, Proot I, Legius M, ter Meulen R, de Witte L. Client-centered home care: balancing between competing responsibilities. Clin Nurs Res. 2006;15(4):231–254. | ||
Rushton C, Edvardsson D. Reconciling conceptualizations of ethical conduct and person-centred care of older people with cognitive impairment in acute care settings. Nurs Philos. 2018;19(2):e12190. | ||
Ross H, Tod AM, Clarke A. Understanding and achieving person-centred care: the nurse perspective. J Clin Nurs. 2015;24(9–10):1223–1233. | ||
Adolfsson ET, Smide B, Gregeby E, Fernström L, Wikblad K. Implementing empowerment group education in diabetes. Patient Educ Couns. 2004;53(3):319–324. | ||
Boström E, Isaksson U, Lundman B, Lehuluante A, Hörnsten Å. Patient-centred care in type 2 diabetes—an altered professional role for diabetes specialist nurses. Scand J Caring Sci. 2014;28(4):675–682. | ||
van der Meer L, Nieboer AP, Finkenflügel H, Cramm JM. The importance of person-centred care and co-creation of care for the well-being and job satisfaction of professionals working with people with intellectual disabilities. Scand J Caring Sci. 2018;32(1):76–81. | ||
Edvardsson D, Fetherstonhaugh D, McAuliffe L, Nay R, Chenco C. Job satisfaction amongst aged care staff: exploring the influence of person-centered care provision. Int Psychogeriatr. 2011;23(08):1205–1212. | ||
McCormack B, Dewing J, Breslin L, et al. Developing person-centred practice: nursing outcomes arising from changes to the care environment in residential settings for older people. Int J Older People Nurs. 2010;5(2):93–107. | ||
Coyne I, O’Neill C, Murphy M, Costello T, O’Shea R. What does family-centred care mean to nurses and how do they think it could be enhanced in practice. J Adv Nurs. 2011;67(12):2561–2573. | ||
Braun V, Clarke V. What can “thematic analysis” offer health and wellbeing researchers? Int J Qual Stud Health Well-being. 2014;9(1):26152. | ||
Mays N, Pope C. Qualitative research: observational methods in health care settings. BMJ. 1995;311(6998):182–184. | ||
Liu F, Maitlis S. Non-participant observation. In: Mills, AJ, Durepos G, Wiebe E, editors. Encyclopedia of Case Study Research. Volume 2. Los Angeles CA; London: SAGE; 2010:609–611. |
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.