Back to Journals » Nutrition and Dietary Supplements » Volume 9
Health care costs matter: a review of nutrition economics – is there a role for nutritional support to reduce the cost of medical health care?
Authors Naberhuis JK , Hunt VN, Bell JD, Partridge JS, Goates S, Nuijten MJC
Received 17 November 2016
Accepted for publication 13 March 2017
Published 1 August 2017 Volume 2017:9 Pages 55—62
DOI https://doi.org/10.2147/NDS.S126232
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Chandrika J Piyathilake
Video abstract presented by Vivienne N Hunt.
Views: 1131
Jane K Naberhuis,1 Vivienne N Hunt,2 Jvawnna D Bell,3 Jamie S Partridge,3 Scott Goates,3 Mark JC Nuijten4
1Division of Nutritional Sciences, University of Illinois at Urbana-Champaign, Urbana, IL, USA; 2Abbott Nutrition, Research and Development, Singapore; 3Abbott Nutrition, Research and Development, Columbus, OH, USA; 4A2M (Ars Accessus Medica), Amsterdam, The Netherlands
Background and aims: As policy-makers assess the value of money spent on health care, research in the field of health economics is expanding rapidly. This review covers a period of 10 years and seeks to characterize the publication of papers at the intersection of health economics and nutrition.
Methods: Relevant publications on nutrition care were identified in the medical literature databases using predetermined search criteria. These included nutritional interventions linked to health economic terms with inclusion criteria requiring original research that included clinical outcomes and cost analyses, subjects’ ages ≥18 years, and publications in English between January 2004 and October 2014.
Results: Of the 5,646 publications identified in first-round searches, 274 met the specified inclusion criteria. The number of publications linking nutrition to economic outcomes has increased markedly over the 10-year period, with a growing number of studies in both developed and developing countries. Most studies were undertaken in Europe (39%) and the USA and Canada (28%). The most common study setting was hospital (62%) followed by community/noninstitutional care (30%). Of all the studies, 12% involved the use of oral nutritional supplements, and 13% involved parenteral nutrition. The economic outcomes consistently measured were medical care costs (53% of the studies), hospital length of stay (48%), hospital readmission rates (9%), and mortality (25%).
Conclusion: The number of publications focused on the economics of nutrition interventions has increased dramatically in recent years. Studies have demonstrated that malnutrition can increase the costs of care and length of hospital stay while corresponding studies show that nutrition interventions can help lower the cost of health care by decreasing the incidence of complications and speeding recovery. As populations age, policies that lead to wider adoption of screening, assessment, and treatment of malnutrition will be important to improve health economic outcomes.
Keywords: economics of nutrition interventions, reducing health care costs through nutrition
Introduction
Health economics is a discipline used to determine the health effects of an intervention and evaluate the cost and benefits of that intervention in order to allocate scarce resources. As nutrition products and interventions compete for space in health care budgets, the cost of nutrition care is being evaluated through health economics and outcomes research (HEOR) through a number of tools. Cost-effectiveness, modeling, predictive risk models, and budget impact analysis are just few examples of such tools that can answer the questions about a treatment’s value.1 Nutrition economics can provide a link between clinical nutrition and health outcomes to allow the evaluation of cost versus the benefit for both individual patients and society.2 The results of nutrition economics studies increasingly show that nutrition care is a cost-effective way to prevent and treat medical problems among people with acute and chronic health conditions.3,4 Specifically, the results of many studies provide evidence to support the role that nutrition can play in improving clinical outcomes while reducing the medical costs associated with malnutrition.3
Recognizing that malnutrition may be due to socioeconomic conditions as well as disease, a definition of malnutrition was agreed in 2015 by a consensus of members of the European Society for Clinical Nutrition and Metabolism (ESPEN). ESPEN recommended that subjects at risk of malnutrition are identified by validated screening tools, and that they should be assessed and treated accordingly. For individuals, identified through screening as being at risk of malnutrition, the diagnosis of malnutrition should be based on either a low body mass index (BMI) (<18.5 kg/m2) or on the combined finding of weight loss together with either a reduced BMI (age-specific) or a low fat-free mass index using gender-specific cutoffs.5
Other definitions of malnutrition include the presence of any of the three risk factors: underweight (ie, BMI <18.5 kg/m2 in adults or <5th percentile of a standardized distribution among children), anemia (ie, hemoglobin <110 g/L for females or 120 g/L for males), or protein-energy malnutrition (ie, serum albumin <35 g/L).6 Many studies have shown that the prevalence of malnutrition in North American, European, Asian, Australian, and Latin American hospitals can range from 20% to ≥50%.4,7 However, malnutrition is not limited to patients in hospitals; a UK study found that 93% of the estimated 3 million people malnourished or at risk of malnutrition live in the community.8 Such malnourished community-dwelling individuals are 2–3 times more likely than their well-nourished counterparts to require additional clinic visits or to be admitted to the hospital.9 Once admitted to the hospital, the malnourished individuals are more likely to experience complications (delayed wound healing, pressure ulcers, and infections), have longer hospital stays, and are at a greater risk of dying.10,11
Medical nutrition, the clinical application of knowledge about the role played by nutrients in health and disease, is increasingly being used in interventions that have been shown to improve patients’ quality of life and other health outcomes while also reducing overall health care costs.4,7,12 Such cost reductions result from lowering the readmission rates,13,14 decreasing the length of hospital stay,15 reducing the frequency of complications (postsurgical infections and pressure ulcers),12,16,17 and ultimately reducing the overall episode cost.18,19
Many of the reviews of medical nutrition and health economics focus on studies of a particular clinical condition, a specific intervention or outcome, and/or a distinct geographic location.3,4 With this review, the authors sought to take a broader look at medical nutrition linked to health economic outcomes in papers published over a decade. With this perspective, they sought to characterize and compare the nutrition economics studies that have been conducted over the review period. They looked at studies across the world to determine the level of interest in medical nutrition and to understand more about its potential to impact on health economic outcomes. Furthermore, they sought to identify the research gaps, raise awareness of the potential to improve health outcomes by implementing cost-effective treatments based on nutrition, and encourage more research to be undertaken in this field.
Methods
Relevant articles were identified according to the predetermined search criteria. Databases searched included Adis Pharmacoeconomics & Outcomes News, BIOSIS Previews, CAB Abstracts, Embase, Embase Alert, EmCare, Food Science and Technology Abstracts, Incidence & Prevalence Database, Medline, and Pascal. Search terms included the following: nutrition, nourish, deficiency, economic, health, burden, impact, cost, effectiveness, utility, benefit, incremental cost-effectiveness ratio, propensity score, length of stay, readmission, quality of life, and quality or disability adjusted life years.
Using the defined search strategy, the analysis was limited to studies addressing both economic costs (inputs) and health consequences (outputs). Inclusion required an original research study with clinical outcomes linked to nutritional interventions or protocols that included cost analyses seeking to measure health and economic outcomes. Only studies in English, with subjects >18 years of age, in the period of January 2004–October 2014 were included (Figure 1).
  | Figure 1 Flowchart of studies included in search. Abbreviations: ICER, incremental cost-effectiveness ratio; RCT, randomized controlled trial. |
There were no restrictions on study design, duration, location or setting, sample size, or the type of nutritional intervention. Both the control and comparator groups were included, including those who received usual/standard nutrition care as well as those who received no additional nutrition for the treatment of malnutrition. Studies published in a language other than English were excluded, as were trial protocols, reviews, editorials, and books.
Results
A total of 5,646 publications were identified in the first-round developed searches with 274 (4.8%) meeting the inclusion criteria. The total number of publications on health economics linked to nutrition has significantly increased over the decade, with an increasing number of studies in both developed countries and developing countries (Figure 2).
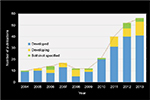  | Figure 2 Number of studies by region (developed, developing, and both/not specified), per year from 2004 to 2013. |
As expected, more studies were conducted in developed countries than in developing countries.
Populations studied
The majority of the studies were conducted in Europe (n=108 or 39% of total) and the USA/Canada (n=76; 28%). The numbers of studies from other regions were as follows: Asia (n=24; 9%), Australia/New Zealand (n=22; 8%), Africa/Middle East (n=18; 7%), and Latin America (n=10; 4%). Sixteen studies (5%) either did not specify the geographic location or included findings from multiple countries.
Figure 3 shows the distribution of nutrition HEOR studies by region highlighting that there is a serious dearth of studies in Asia. Of the total reviewed, only 9% of studies were from a region now accounting for 56% of the global population.20 Many countries in Asia are dealing with rapidly aging populations and some are in a “nutrition transition” as people shift from rural to urban settings. As a result of the rapid demographic and environmental change, many are experiencing rising health care costs as a consequence of increased rates of noncommunicable diseases such as diabetes, cardiovascular disease, and COPD. The lack of studies from Asia highlights that more research is needed to provide evidence about cost-effective health interventions in which nutrition plays a role in improving health outcomes. Such research needs to reflect the context of these health care systems.
  | Figure 3 Percentage of HEOR studies from 2004 to 2014 by region. Abbreviation: HEOR, health economics and outcomes research. |
Of the studies included in this literature review, 63% were conducted in hospitals, and 30% were carried out in community settings. Residential care homes (5%) or outpatient centers (2%) were less commonly reported as study sites.
Malnutrition condition
Many of the studies focus on disease-related malnutrition, which is defined as malnutrition that arises as a side effect of other diseases. It includes an inability to ingest or absorb nutrients, as well as the increased energy needs related to the disease or restricted diet as a result of the treatment.6 Table 1 shows that malnutrition accounted for 15% (42/274) of the health conditions described in the studies reviewed. The study classification by condition mirrors the health circumstances frequently associated with nutritional problems.
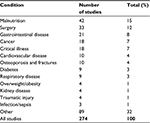  | Table 1 Breakdown of studies by described health condition |
The study grouping also includes patients with undernutrition. The ESPEN consensus authors found that the terms “malnutrition and under-nutrition” are almost equally used in the scientific literature and in clinical practice, with a slight preponderance for malnutrition.5 A potential problem with the term “malnutrition” is that it covers all deviating nutritional states due to acute or chronic health conditions as associated with surgery, gastrointestinal disease, cancer, and critical illness. Overnutrition, as evidenced by overweight or obesity, was reported in only a small proportion of the included studies (n=4; 1%), even though it is recognized that these conditions do represent a form of malnutrition in both developing and developed countries.21 Similarly, studies involving those aged >65 are underrepresented in the nutrition economics studies; few studies (n=5; 2%) were based solely on older people despite the fact that 14% of the population is ≥65 years old in developed countries (France, Sweden, UK, USA, and Japan).22 Malnutrition prevalence rates can be found to be associated with increasing longevity and aging in developed countries, which represents another research gap that should be addressed.
Nutrition interventions
Studies were classified according to the type of intervention used and it was found that 40% of interventions featured in the studies provided nutritional supplementation products and/or changed dietary practice. These included oral nutritional supplementation (ONS; 12.0%), parenteral nutrition (10.9%), special diets (9.1%), and enteral nutrition (6.9%). Other interventions included the introduction of nutrition care protocols/guidelines, micronutrient supplementation or fortification, functional ingredients to modulate the immune and inflammatory responses, and in some situations policy change to health care systems.
Outcome measures
Figure 4 shows the number of studies focused on both health and financial outcomes.
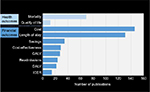  | Figure 4 Studies from 2004 to 2014 by health economic measure type. Abbreviations: QALY, quality-adjusted life year; DALY, disability-adjusted life year; ICER, incremental cost-effectiveness ratio. |
Mortality rates and quality of life (the standard of health, comfort, and happiness experienced by an individual or group23) were most frequently used as health outcome measures, while episode cost, length of hospital stay, and cost savings due to interventions were the most commonly reported economic outcomes. Other economic measurements included hospital readmission, disability-adjusted life year (DALY; it is thought of as one lost year of “healthy” life. The sum of DALYs across a population is a measurement of the gap between current health status and an ideal health situation where the entire population lives to an advanced age, free of disease and disability24), quality-adjusted life year (QALY; it is a generic measure of disease burden, including both the quality and the quantity of life lived. It is used in the economic evaluation of medical interventions to assess the value for money. One QALY equates to 1 year in perfect health24), and incremental cost-effectiveness ratio (it is a statistic used in cost-effectiveness analysis to summarize the cost-effectiveness of a health care intervention. It is defined as the difference in cost between two possible interventions, divided by the difference in their effect25).
As noted in Figure 1, the reviewed studies use a wide range of economic analyses and tools. These include measurement methods, simulation models, Markov models, cost utility models, discrete-event simulations, budget impact models, and predictive models. It is evident that a range of tools are being used by health economists and researchers to effectively measure outcomes of interest in order to determine whether a nutrition intervention offers value when making decisions about health care resources and their allocation.
The cost-effectiveness of nutrition interventions using ONS has been established in both the hospital and community settings. A systematic review of ONS in the hospital noted that, of the 12 studies with quantitative data included in the review, the mean cost saving was 12.2% for those patients using ONS.26 A similar review in the community setting found that “ONS (…) produces an overall cost advantage or near neutral balance, often in association with clinically relevant outcomes, suggesting cost effectiveness.”27 A recent randomized controlled trial with >600 malnourished patients found that consumption of a high-protein ONS (two servings/day) during hospitalization and for 90 days post discharge had a cost-effectiveness of US$33,818/QALY when modeled over the study period with <US$1,000/QALY when modeled over the life span of the patient.27
Conclusion
Nutrition economics is a relatively new area of knowledge, but the number of published studies in this field has increased more than fivefold over the last decade with less than ten papers per year in 2004 increasing to 50 in 2013. While more health economic studies have been conducted in the developed and developing regions, it is clear that there is an upward trend for such studies across the world. It is notable, however, that there is a significant shortfall of such studies in Asia, a region that accounts for >50% of the global population but where only 9% of studies were located. When the papers were classified by malnutrition topic, it was found that most studies focused on diseases or conditions that are recognized to carry an increased risk for malnutrition or undernutrition (ie, surgery, gastrointestinal disease, cancer, and critical illness). It is well known that as people age, some need additional nutritional support to maintain their health. Further research targeted toward older-aged vulnerable participants is a research gap that needs to be addressed. Such research needs to provide evidence that improved health outcomes and recovery rates together with lower costs of care can be achieved through an appropriate nutrition intervention, be it ONS or changed practice.
Numerous nutrition economics studies have examined the health and financial costs of poor nutritional status with corresponding studies providing evidence of health and financial benefits as a result of specific nutritional interventions.26,35–37 Survival (or mortality) is the one of the most frequently measured variables related to nutrition.10,28,29 One large new study showed that, to save a life, the number-needed-to-treat (the average number of patients who need to be treated to prevent one additional bad outcome) with ONS was just 20.3.30
In terms of cost-related outcomes, many studies examined the relationship between malnutrition and increased length of hospital stay and frequency, hospital readmission, and hospital episode costs.3,31,32 There is a growing body of evidence demonstrating that nutrition interventions can help lower the costs of health care by decreasing the incidence of complications and speeding recovery. The cost savings related to improvement in patients’ nutritional status outpace the relatively small costs of the nutrition interventions.3,18,33 With better health outcomes at lower costs, such nutrition interventions could be considered cost-effective at both the patient and population level.
As noted in this discussion, there is a growing body of research demonstrating that a nutrition intervention can be used as a cost-effective way mechanism. One study demonstrates cost savings of 12.2% when oral nutritional supplements are administered, with the same study estimating the cost per QALY over a lifetime being as low US$1,000.26
Since cost containment is becoming increasingly important in health care today, paying more attention to nutrition to improve health is imperative. In terms of health and financial impacts, there are a variety of HEOR tools to ask and answer the question “does the benefit exceed the cost?” As the body of research continues to grow, evidence-based decisions about “value” in nutrition care for specific patient populations can be made taking into account the different health care settings. If undernutrition and conditions of malnutrition risk are detected early through targeted screening and assessment and treated appropriately using established and stepwise treatment algorithms, it is posited that better clinical outcomes and lower costs are likely.7,34 It is believed that it is now time to advance hospital and governmental policies to incentivize nutrition screening, assessment, and treatment in both hospital and community settings. Clinical researchers around the world are invited to conduct more nutrition economics studies to take account of the differences in health care settings and find ways to improve health and economic outcomes that meet region-specific health care needs.
Acknowledgments
The authors thank Cecilia Hofmann, who provided medical writing services to develop the manuscript, and Dr Suela Sulo, from Abbott Nutrition R&D, Columbus, OH, who did a final review and edit. Jane K Naberhuis received funding for review of the literature as a student from the Division of Nutritional Sciences, University of Illinois, Urbana-Champaign.
Author contributions
All authors made substantial contributions to analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
Disclosure
Vivienne Hunt, Jamie Partridge, Jvawnna Bell, and Scott Goates receive salary from and hold stocks in Abbott Laboratories. Mark Nuijten received funding from Abbott Laboratories for his peer review and editorial contributions. The authors report no other conflicts of interest in this work.
References
Philipson T, Linthicum MT, Snider JT. Tutorial on health economics and outcomes research in nutrition. JPEN J Parenter Enteral Nutr. 2014;38(Suppl 2): 5S–16S. | ||
Lenoir-Wijnkoop I, Dapoigny M, Dubois D, et al. Nutrition economics – characterising the economic and health impact of nutrition. Br J Nutr. 2011;105:157–166. | ||
Freijer K, Bours MJ, Nuijten MJ, et al. The economic value of enteral medical nutrition in the management of disease-related malnutrition: a systematic review. J Am Med Dir Assoc. 2014;15(1):17–29. | ||
Norman K, Pichard C, Lochs H, Pirlich M. Prognostic impact of disease-related malnutrition. Clin Nutr. 2008;27(1):5–15. | ||
Cederholm T, Bosaeu I, Barazzoni R, et al. Diagnostic criteria for malnutrition – An ESPEN Consensus Statement. Clin Nutr. 2015;34(3):335–340. | ||
Linthicum MT, Thornton Snider J, Vaithianathan R, et al. Economic burden of disease-associated malnutrition in China. Asia Pac J Public Health. 2015;27(4):407–417. | ||
Correia MI, Hegazi RA, Higashiguchi T, et al. Evidence-based recommendations for addressing malnutrition in health care: an updated strategy from the feedM.E. Global Study Group. J Am Med Dir Assoc. 2014;15(8):544–550. | ||
Elia, M. Russell C.A. Combating Malnutrition: Recommendations for Action. Output of meeting of Advisory Group on Malnutrition 12 June 2008. 2009, The British Association for Parenteral and Enteral Nutrition (BAPEN), Redditch, Worcs, UK. | ||
Guest JF, Panca M, Baeyens JP, et al. Health economic impact of managing patients following a community-based diagnosis of malnutrition in the UK. Clin Nutr. 2011;30(4):422–429. | ||
Agarwal E, Ferguson M, Banks M, et al. Malnutrition and poor food intake are associated with prolonged hospital stay, frequent readmissions, and greater in-hospital mortality: results from the Nutrition Care Day Survey 2010. Clin Nutr. 2013;32(5):737–745. | ||
Shahin ES, Meijers JM, Schols JM, Tannen A, Halfens RJ, Dassen T. The relationship between malnutrition parameters and pressure ulcers in hospitals and nursing homes. Nutrition. 2010;26(9):886–889. | ||
Milne AC, Potter J, Avenell A. Protein and energy supplementation in elderly people at risk from malnutrition. Cochrane Database Syst Rev. 2005;2:CD003288. | ||
Gariballa S, Forster S, Walters S, Powers H. A randomized, double-blind, placebo-controlled trial of nutritional supplementation during acute illness. Am J Med. 2006;119(8):693–699. | ||
Stratton RJ, Hebuterne X, Elia M. A systematic review and meta-analysis of the impact of oral nutritional supplements on hospital readmissions. Ageing Res Rev. 2013;12(4):884–897. | ||
Somanchi M, Tao X, Mullin GE. The facilitated early enteral and dietary management effectiveness trial in hospitalized patients with malnutrition. JPEN J Parenter Enteral Nutr. 2011;35(2):209–216. | ||
Cawood AL, Elia M, Stratton RJ. Systematic review and meta-analysis of the effects of high protein oral nutritional supplements. Ageing Res Rev. 2012;11(2):278–296. | ||
Stratton RJ, Ek AC, Engfer M, et al. Enteral nutritional support in prevention and treatment of pressure ulcers: a systematic review and meta-analysis. Ageing Res Rev. 2005;4(3):422–450. | ||
Philipson TJ, Snider JT, Lakdawalla DN, Stryckman B, Goldman DP. Impact of oral nutritional supplementation on hospital outcomes. Am J Manag Care. 2013;19(2):121–128. | ||
Snider JI, Jena AB, Linthicum MT, et al. Effect of hospital use of oral nutritional supplementation on length of stay, hospital cost, and 30-day readmissions among Medicare patients with COPD. Chest. 2015;147(6):1477–1484. | ||
2015 World Population Data Sheet. Washington, DC: Population Reference Bureau. Available from: http://www.prb.org/Publications/Datasheets/2015/2015-world-population-data-sheet.aspx. Accessed March 3 2016. | ||
Obesity and Overweight Fact Sheet Number 311. Geneva: World Health Organization; 2015 [cited March 3, 2016]. Available from: http://www.who.int/mediacentre/factsheets/fs311/en. Accessed March 3 2016. | ||
National Institute on Aging National Institutes of Health, NIH Publication no. 11-7737 October 2011. Available from: http://www.who.int/ageing/publications/global_health.pdf. Accessed March 3 2016. | ||
QoL definition. Available from: http://www.medicinenet.com/script/main/art.asp?articlekey=11815. Accessed February 28, 2017. | ||
DALY definition. Available from: http://www.who.int/healthinfo/global_burden_disease/metrics_daly/en/. | ||
Whitehead SJ, Ali S. Health outcomes in economic evaluation: the QALY and utilities. Br Med Bull. 2010;96(1):5–21. | ||
Elia M, Normand C, Norman K, Laviano A. A systematic review of the cost and cost effectiveness of using standard oral nutritional supplements in the hospital setting. Clin Nutr. 2016;35(2):370–380. | ||
Zhong Y, Cohen JT, Goates S, Luo M, Nelson J, Neumann PJ. The cost-effectiveness of oral nutrition supplementation for malnourished older hospital patients. Appl Health Econ Health Policy. 2017;15(1):75–83. | ||
Allard JP, Keller H, Jeejeebhoy KN, et al. Malnutrition at hospital admission-contributors and effect on length of stay: a prospective cohort study from the Canadian Malnutrition Task Force. JPEN J Parenter Enteral Nutr. 2016;40(4):487–497. | ||
Datema FR, Ferrier MB, Baatenburg de Jong RJ. Impact of severe malnutrition on short-term mortality and overall survival in head and neck cancer. Oral Oncol. 2011;47(9):910–914. | ||
Deutz NE, Matheson EM, Matarese LE, et al. Readmission and mortality in malnourished, older, hospitalized adults treated with a specialized oral nutritional supplement: a randomized clinical trial. Clin Nutr. 2016;35(1):18–26. | ||
Lim SL, Ong KC, Chan YH, Loke WC, Ferguson M, Daniels L. Malnutrition and its impact on cost of hospitalization, length of stay, readmission and 3-year mortality. Clin Nutr. 2012;31(3):345–350. | ||
Barker LA, Gout BS, Crowe TC. Hospital malnutrition: prevalence, identification and impact on patients and the healthcare system. Int J Environ Res Public Health. 2011;8(2):514–527. | ||
Freijer K, Lenoir-Wijnkoop I, Russell CA, et al. The view of European experts regarding health economics for medical nutrition in disease-related malnutrition. Eur J Clin Nutr. 2015;69(5):539–545. | ||
Loser C. Malnutrition in hospital: the clinical and economic implications. Dtsch Arztebl Int. 2010;107(51–52):911–917. | ||
Correia MI, Waitzberg DL. The impact of malnutrition on morbidity, mortality, length of hospital stay and costs evaluated through a multivariate model analysis. Clin Nutr. 2003;22(3):235–239. | ||
Thibault R, Makhlouf AM, Kossovsky MP, et al. Healthcare-associated infections are associated with insufficient dietary intake: an observational cross-sectional study. PLoS One. 2015;10(4):e0123695. | ||
Fry DE, Pine M, Jones BL, Meimban RJ. Patient characteristics and the occurrence of never events. Arch Surg. 2010;145(2):148–151. |
 © 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
