Back to Journals » Advances in Medical Education and Practice » Volume 9
Hands-on teaching, shadowing, and supported learning through acute clinics to help improve the confidence of and meet training needs for junior doctors working in ear, nose, and throat surgery
Authors Aryasomayajula S, Raithatha A, Haywood M , Jobanputra R, Roplekar R, Acharya V
Received 31 December 2017
Accepted for publication 3 August 2018
Published 14 November 2018 Volume 2018:9 Pages 827—835
DOI https://doi.org/10.2147/AMEP.S161187
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Md Anwarul Azim Majumder
Saraswati Aryasomayajula,1 Amit Raithatha,1 Matthew Haywood,2 Ravi Jobanputra,2 Rujuta Roplekar,1 Vikas Acharya1
1Department of ENT Surgery, Luton and Dunstable University Hospital, Luton, UK; 2Department of ENT Surgery, Lister Hospital, Stevenage, UK
Background: Ear, nose, and throat (ENT) surgery is a niche and unique specialty that has been recognized as being poorly taught throughout medical school and postgraduate training. Junior doctors who rotate into this specialty often find it hard and struggle to manage patients.
Aims: The aim of this study was to devise a junior doctor-focused induction program with specific emphasis on shadowing and partnered working to improve confidence and competence.
Methods: Feedback from previous trainees was used to identify valuable training opportunities within the 4-month rotation. Trainers identified clinical areas where supported learning could be delivered. Trainees were allocated to rotate between theater, ward, on-call shifts, and acute clinics. The degree of time spent in each area was analyzed in order to balance service provision vs learning needs. Furthermore, novel strategies were introduced in each session to maximize learning experiences. Junior doctors were aware of the opportunities that would be available to them at the start of the rotation. In order to assess whether the aims were met, a questionnaire survey was used to assess exposure to core ENT practical skills and junior doctors’ confidence levels in carrying them out unsupervised.
Results: Junior doctors spent 40% of their time assessing new acute admissions. Twenty percent of time was spent in ENT clinic, but novel practical methods of induction were introduced such as 1 week of directly supervised shadowing, followed by a transition period with regular debrief. A three-stage model was used to offer training in practical procedures in the clinical setting. Over half of the trainees felt confident in undertaking 50% of the core ENT procedures unsupervised.
Conclusion: Our study reveals that giving junior doctors a relevant, focused and appropriate induction helps orientate them, give them the opportunity to ask questions, and also find their grounding in order to begin working. Having dedicated time to shadow and be with a colleague to assess and treat patients initially, with ongoing telephone and in person support, ensured that their confidence and competence improved very quickly. It also improved workplace satisfaction and motivated doctors to undertake self-directed learning and improve and enhance their skills beyond the minimum.
Keywords: medical education, improving confidence, junior doctor training, foundation training, transitions
Introduction
Ear, nose, and throat (ENT) surgery, or otorhinolaryngology, is a vast specialty with overlap and relevance across a number of different surgical arenas. The vast clinical presentations, pathophysiology, and patient demographics allow ENT cases to be encountered in general practice, emergency medicine, general medicine, and pediatrics. This means that although ENT is classified as a surgical specialty, the knowledge and skills it encompasses are relevant to all medical and surgical trainees.1 A large proportion of ENT patients are managed on wards, and doctors responsible for patients’ day-to-day care are junior doctors of varying grades (predominantly foundation year and core training level). It can be difficult for junior doctors, especially if they are less experienced to carry out this role without adequate guidance and supervision. Seventy-eight percentage of medical schools includes an ENT rotation lasting an average of 1–2 weeks as a part of their training. Although theoretical knowledge about ENT emergencies is integrated into the curriculum, the practical skills integrated into the specialty are neither assessed nor made compulsory.2 Transition to a new specialty can be a difficult time, with the lack of familiarity and support. As a consequence of this, junior doctors can feel under-confident, demotivated, and stressed while carrying out their role. Induction programs alone are insufficient because they are usually didactic and more theoretical with less emphasis on practical aspects.3 Evans et al4 reported that an extended induction program objectively improves clinical skills but work by Berridge et al5 goes one step further to demonstrate the need for shadowing predecessors and the need for existing trainees to impart helpful tips based on recent experiences.
Studies by Goodyear6 have shown that junior doctors want to be given responsibility in the workplace in order to feel part of the team and have a positive impact in the patient’s care. They feel that administrative tasks can be deskilling and repetitive and hinder their learning process. Hence, it is vital to train junior doctors in the initial stages of their rotation. This will give a sense of empowerment, allowing them to take an interest and active role in patient management. Furthermore, such support is vital in order to build junior doctors’ confidence and, ultimately, their competence.
With the implementation of the new junior doctor contract in the UK, there is a specific guidance on working hours and shift patterns. This means that allocated “out of hours” and emergency services are provided through a system of “cross cover” often by nonspecialists. Unfortunately, in reality, this involves doctors undertaking the workload for two or more specialties, for example, general surgery and ENT during their night shifts. In order to maintain patient’s safety and run an efficient department, it is essential to train junior doctors adequately to carry out their roles and responsibilities competently. This includes exposure to all aspects of the specialty such as acute outpatient clinics and operating theaters so that a breadth of cases can be seen and various practical skills can be practiced in a supervised environment with opportunities for teaching and feedback.
Our study aims to address the issues highlighted with existing induction and training programs through introduction of a novel rota and work model (Figure S1). One of the research objectives is to assess through questionnaires if this design meets the curriculum requirements for all junior doctors by balancing training and development against service provision within the department. Through this process, we aim to empower junior doctors with the skills and knowledge to safely and confidently carry out their role as ENT junior doctors. Another research objective is to make the experience more practical and relevant for day-to-day delivery of clinical care. We aim to do this by offering structured teaching and mentoring in different clinical areas to impart clinical knowledge, skills, and training and development opportunities. The final goal of this research study is to develop a training model that can be easily implemented in different ENT departments to improve learning experiences and enhance workplace satisfaction for junior doctors.
Methods
In August 2017, a new junior doctor rota (Figure S1) and monthly departmental teaching were implemented at the Luton and Dunstable University Hospital, UK. This is a district general hospital serving approximately a population of 350,000 people. The ENT department consists of six consultants, six middle grade doctors/registrars, and six junior doctors. Being a regional head and neck center, the team is supported by specialist nurses and other health care professionals such as audiologists and speech and language therapists to allow the provision of routine, specialist, and nurse-led clinics. The trust collaborates with Bedford hospital to allow the provision of specialist services and multidisciplinary team (MDT) discussions for complex cases and provides an out of hours cross cover at middle grade and consultant level.
The two main methods of data collection in this study were participant observation and survey questionnaires. Participant observation was used to establish the main clinical areas encountered during a placement in ENT. Feedback was used from previous trainees in a locally designed “End of placement survey” addressing working hours, opportunities for training, and work load. This informed the proportion of time trainees would spend in four main areas of the department within the rota for a 4-month period. Having established this, trainers analyzed the requirements for service provision vs opportunities for training based on various activities undertaken in different clinical areas. Trainees’ time was allocated within each clinical to guide learning and maximize opportunities for structured feedback within the new rota (Figure S1). It was also ensured that there were adequate staffing levels, at the appropriate grade(s) in order to facilitate supported yet independent practice with feedback. Once the new rota and working pattern were in place, questionnaires using the Likert scale were used to assess trainee’s exposure and confidence in carrying out core ENT procedures.
The junior doctors consisted of one foundation year (FY2) doctor, one general practice (GPST1) trainee, one core surgical (CT1) trainee with an interest in pursuing ENT surgery, and three junior clinical fellows (same grade equivalent). It was appropriate to introduce this model in ENT because the specialty caters to a wide range of trainees’ interest, for example, medicine, anesthetics, and radiology among others. All new doctors rotating into the department as well as those already present from August 2017 to December 2017 were allocated to the new rota. They were aware of different training opportunities available to them at the beginning of the rotation, and permission was sought to use their comments/experiences in an anonymized manner as a part of this study.
During weekdays, the minimum level of cover included one doctor allocated to the wards from 8 am to 5 pm, one doctor on call from 8 am to 8 pm, and one doctor on night shift from 8 pm to 8 am. The daily routine would start with a ward round at 8 am led by a consultant or senior registrar to review all inpatients, postoperative patients, and new emergency admissions. On-call responsibility included taking referrals from general practitioners and the emergency department. The tasks would involve reviewing patients for inpatient admission, booking patients for outpatient acute clinic, and offering advice or acute intervention to patients as required.
On-call and night duty responsibilities were allocated initially to clinical fellows who already had 6 months of experience within the specialty, while the other trainees were allocated to the ward-based shift. The main modalities of teaching were hands on through shadowing in clinic, assisting in theater, trainee-centered ward rounds, and supported learning while on-call. Evaluation of the mentoring and support offered was based on a combination of competencies from the foundation program and the Intercollegiate Surgical Curriculum Programme (ISCP).1–7
Results
The new junior doctor rota design (Figure S1) and organization of supervised acute clinics allowed the delivery of multimodal teaching for junior doctors from four main clinical areas over 1 month (August 2017 to September 2017). This enabled them to experience a wide patient case load and practice commonly used ENT skills such as nasal cautery, ear microsuction, and nasal packing for epistaxis in a realistic yet supervised environment with feedback. This also included the review of patients with common and acute ENT pathology in the emergency clinic.
Figure 1 outlines the proportion of time that trainees spent in four different clinical areas to balance training needs alongside service provision within the department. Due to the nature of the work undertaken, each clinical area offered the chance to develop different skills such as history taking, examination, surgical, and procedural skills. It was important for trainees to obtain a wide yet relevant skill set in order to carry out their role as an ENT junior doctor, and a correct balance of time allocation was important to achieve this.
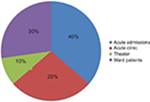  | Figure 1 Proportion of trainees’ time spent in different clinical areas with opportunities for structured learning. |
The main opportunity to gain feedback and supported learning was through the assessment of acute referrals and admissions. Forty percentage of the trainees’ time was allocated to assess new acute admissions, and 30% of their time was spent looking after existing patients on the wards. Since both these shifts ran simultaneously, at least two junior doctors were rostered every day, meaning that time management and completion of tasks were quicker, allowing them to assess new referrals together. This approach allowed a more thorough assessment of the patient, and the doctors could experience a wider range of acute and emergency ENT cases compared to working alone. Ward rounds are often perceived poorly as an environment for clinical learning as only 30% of trainees feel they learn something new or valuable.8 We adopted a trainee-centered approach, which has been shown to overcome barriers, highlight learning opportunities, and also integrate junior doctors within the team.9
Routine and specialist outpatient clinics form a significant aspect of otolaryngology as a specialty. Acute or emergency ENT clinics allow opportunity for the assessment and management of common ENT pathology, the practice of basic procedural skills, and the follow-up of patients within the scope of the junior doctor curriculum. In order to accommodate dedicating teaching time, clinic slots were extended to 30 minutes and directly supervised by a registrar grade doctor in ENT over the course of 1 week. Over a 4-month placement, junior doctors spent 20% of their time in acute clinic, initially shadowing and, then over a transition period, were able to manage and run their own clinics. This was especially useful to achieve the competencies outlined for GPST doctors.
After the introduction of European Working Time Directive in 1998, doctors theoretically cannot be scheduled to work more than 48 hours a week under British law. It was estimated that this would reduce overall training time by one-fifth.10 In order to achieve competencies, learning needs to be maximized within currently scheduled training sessions and both trainers and trainees need to be supported to achieve this.11 As a part of the foundation training curriculum, 10% of theater time was allocated to achieve skills such as suturing, injection of local anesthetic, catheterization, and airway support. The core surgical trainee on their ENT rotation was allocated 40% of theater time to meet their logbook requirements, while the workload was supported by their colleagues, who held the on-call bleep.
Table 1 shows the proportion of trainees who had the opportunity to receive supported clinical exposure during the course of their placement. A core set of ENT skills were used based on the degree of complexity outlined in the competencies from the foundation program and the ISCP.1–7 Questionnaires were used to ask trainees if they received practical teaching in a supported clinical environment for each procedure and, if so, trainees were asked to comment whether they felt confident enough to undertake that skill unsupervised. This was graded on a Likert scale by the junior doctors and results represented as a percentage of the total cohort.
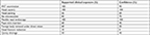  | Table 1 Proportion of trainees receiving supported clinical exposure and confidence in core ENT skills over a 4-month period Abbreviation: ENT, ear, nose, and throat. |
In order to deliver training in practical procedures, the three-stage model proposed by Fitt and Posner for proficiency in motor skills was used. The first cognitive stage was to explain the indication, relevant anatomy, and context for the procedure and allow familiarization with the equipment. A step-wise demonstration allowed the development of correct technique. Junior doctors were then able to move on to the integrative stage after practice and constructive feedback.12 All the trainees were demonstrated ENT examination, nasal cautery, and flexible nasal endoscopy. However, not everyone was able to practice other skills such as nasal fracture reduction and quinsy drainage as these pathologies were less common and management was more senior led during the induction period.
Confidence in the execution of practical skills was based on the autonomous stage in Fitt and Posner’s model.12 This was affected by the difficulty of the skill, the number of opportunities for practice, and also potential risks associated with the procedure. Nasal fracture reduction has cosmetic implications; thus, many of the new junior doctors did not feel confident enough to do this without supervision. Forty percentage of trainees felt confident in draining a quinsy because they felt that very few admitted patients had persistent true quinsy. Pope wick insertion into the ear and nasal cautery were taught and practiced extensively during the ENT placement. However, trainees’ confidence levels were affected by overall patient experience, pain, and discomfort during the procedure.
Discussion
Basic theoretical knowledge prior to supplement clinical practice
It has been shown that an introductory ENT course improves both the confidence and clinical practice of junior doctors.1,12 We therefore allocated 3 days at the beginning of the placement for trust induction to allow familiarization with computer systems, department organization, as well as other logistics. As a part of this, a theoretical lecture was delivered by a senior registrar outlining the management of common ENT emergencies, ENT examination, and the normal findings of flexible nasal endoscopy. “Learner-centered induction programs” have been shown to improve knowledge and confidence because of the transition from working in general medicine or surgery to a more specialist subject.3 Also, it was felt that having a focused and dedicated induction for this niche specialty proved to be beneficial.
Knowledge was reinforced and updated through monthly departmental teaching afternoons. Topics were delivered in a “systems based approach”, for example, the first session focused on common ear pathologies and the next session focused on thyroid and neck lumps. This was well received with good feedback, and junior doctors were rostered in turns to be on call so that everyone could attend an equal proportion of sessions. This helped to meet the training and development needs of junior doctors rather than having interrupted teaching due to service demands and clinical workload.
Senior support and feedback
When junior doctors were scheduled to be “on call”, a registrar was accessible for advice or review if the doctor was concerned. This model allowed the scope for learning through independent practice within a protected framework. Toward the end of the shift, a verbal discussion or formal review of more unwell patients would take place. This provided the opportunity for feedback on the initial diagnosis, management plans, and the opportunity to complete workplace-based assessments for junior doctors’ portfolios. Since two junior doctors assessed patients together, they were able to reflect on their colleague’s approach to the case while ensuring effective handover between shifts. Therefore, trainees spent 40% of their time assessing new admissions so that they could benefit from near-peer learning and also experience a wide range of cases. “Feedback” can be a very broad term, and often, it is not structured or completely relevant in clinical settings. Hence, trainers were informed about specific modes of delivering feedback in each of the different clinical areas. This ensured that learning objectives were specific and the feedback was tailored appropriately to match the needs of the trainee. This meant that >60% of junior doctors felt they could undertake five of the nine ENT procedures unsupervised.
Trainee-centered approach on ward rounds
In order to overcome barriers to learning on ward rounds, a trainee-centered approach was adopted; which gave the session a formal framework with clear objectives.9 An initial virtual or paper ward round was conducted with the whole team where a brief history about each patient was reviewed and juniors were asked to contextualize the patient load as per their learning outcomes for that particular session. The “legitimate peripheral participation model”, introduced by Lave and Wegner, was adopted to improve the feeling of participation, offering a sense of teamwork and inclusion.13 Junior doctors were then allocated clear roles allowing them to contribute in a meaningful way, with a view that further experience and confidence would allow them to take on more responsibility. This was achieved by asking the junior doctor to review a patient of their choice and present the findings back to a senior member of the team for discussion, questions, and feedback. This approach offered continuity of care as juniors were allocated one full week of ward responsibilities to engage in day-to-day discussions for the patient. It also increased patient’s safety because junior doctors are often the first to assess acutely unwell patients on the ward and their decision process was aided through engaging in trainee-centered ward rounds.
Such an approach raised the issue of time resource limitations as junior doctors are also expected to document the consultant’s and/or senior doctors’ management plan. This was solved by the consultant/senior doctor simultaneously reviewing another patient and junior doctors taking it in turns to present patients while their other colleague(s) managed the administrative duties.
Role of acute clinics in the training program
Having received theoretical background knowledge, training in practical skills, and first-hand shadowing experience, junior doctors were then able to run their own acute ENT clinics. Specialist consultant clinics would be running simultaneously so that trainees could escalate any concerns or seek advice at all times, if required. With the new design of the rota (Figure S1), junior doctors would systematically rotate from on-call shifts to clinic shifts. This meant that they could often review the same patients after discharge, allowing continuity of care and understanding of the complete patient pathway to consolidate their knowledge. This was also an opportunity to gain exposure to common ENT procedures in relatively well patents, and >60% of trainees had exposure to seven of the nine core ENT procedures in order to meet their curriculum requirements.
Optimizing learning in theater
In the literature, it is reported that learning experience in the operating theater can be optimized through actual participation, realistic learning objectives and expectations, and understanding of the patient pathway.14 The new rota design (Figure S1) and multimodal learning opportunities addressed these themes in the theater environment. Evidence also suggests that regular participation by junior doctors in ward rounds which involve the whole multidisciplinary team, including allied healthcare professionals, allows for wider continuity of learning. Furthermore, trainees were asked to express expected learning outcomes prior to each session with a senior registrar or consultant and a discussion ensued about how these can be achieved alongside feedback and agreed action points after the theater session.
Conclusion
ENT is an interesting, varied, and stimulating specialty for junior doctors when learning opportunities are made explicit. However, the specialist nature of practical skills involved warrants the need for adequate shadowing and teaching in the initial stages. Being a trainee is a difficult and stressful time with many transitions during the early stages of career progression, which are often potential barriers to learning. It is important to identify these challenges and tackle them with novel initiatives that maximize learning opportunities in a limited amount of time, due to the short-span of specialty rotations. Consultant and registrars are often keen to teach, and junior doctors are keen to learn, but the pressures of clinical duties hinder the transmission of important skills. Hence, we propose a formal, structured approach in different clinical areas to improve the training and education needs of ENT junior doctors. Since many of the principles are generic, the principles could be transferred and trialed in other specialties. This model of training within the department can also be applied in various hospitals across the region to allow consistency in training. The European Standards of Postgraduate Medical Training (European Union of Medical Specialists) is a nongovernmental organization representing national associations of medical specialists at the European level. They have created a training program for specialists with postgraduate training in otorhinolaryngology with the aim of competency-based assessments.15 One of the requirements is to provide evidence of skills in a logbook format.
This model of hands-on teaching can be used to optimize the delivery of training within the European Union of Medical Specialists program. An initial analysis of the logbook components and clinical areas in which these can be achieved allows an appropriate working pattern to be created. This ensures that the trainees obtain the necessary clinical exposure while providing structured feedback opportunities, unique to the tasks undertaken in that area. Trainers also need to be informed of various modalities by which to deliver structured clinical learning experiences. The breadth of exposure and confidence in undertaking the necessary competency-based tasks can then be evaluated using a questionnaire-based survey.
In the modern National Health Service (NHS) in the UK, rota gaps are a constant topic of debate and would affect our proposed rota design (Figure S1). However, with good planning and management, these can be overcome through additional cover arranged in advance. Our findings span over a period of 4 months with positive implications. However, there is a role for further audit and evaluation over a longer period of time. This would highlight other barriers that would need to be addressed and provide data for the long-term efficacy of this model as well as its impact on the future careers of doctors having undertaken a placement in ENT. We feel that such a model is crucial to maintain the balance of training against service provision for current junior doctors as it ultimately forms as an investment in their progression to future leaders within the NHS.
Disclosure
The authors report no conflict of interest in this work.
References
The Intercollegiate Surgical Curriculum. Educating the surgeons of the future. Available from: https://www.iscp.ac.uk/static/public/syllabus/syllabus_omfs_2016.pdf. Accessed June 7, 2017. | ||
Elloy M, Sama A. Does an ENT Introductory Course Improve Junior Doctors’ Confidence in Managing ENT Emergencies? RCS The Bulletin. 2010;92(9):1–5. | ||
Acharya V, Mansour S, Amis SM, Reyahi A. Can the transition process from foundation doctor to neurosurgical specialty trainee be improved through “learner-centered induction programs”? Adv Med Educ Pract. 2015;6:591–595. | ||
Evans DE, Wood DF, Roberts CM. The effect of an extended hospital induction on perceived confidence and assessed clinical skills of newly qualified pre-registration house officers. Med Educ. 2004;38(9):998–1001. | ||
Berridge EJ, Freeth D, Sharpe J, Roberts CM. Bridging the gap: supporting the transition from medical student to practising doctor-a two-week preparation programme after graduation. Med Teach. 2007;29(2–3):119–127. | ||
Goodyear HM. First year doctors experience of work related wellbeing and implications for educational provision. Int J Med Educ. 2014;5:103–109. | ||
The Foundation Programme [homepage on the Internet]. Progression through foundation training. Available from: http://www.foundationprogramme.nhs.uk/curriculum/Progression-through-foundation-training#4. Accessed June 7, 2017. | ||
Qureshi NS, Swamy NN. Postgraduate trainees’ assessment of the educational value of ward rounds in obstetrics and gynaecology. J Obstet Gynaecol. 2008;28(7):671–675. | ||
Acharya V, Reyahi A, Amis SM, Mansour S. Do “trainee-centered ward rounds” help overcome barriers to learning and improve the learning satisfaction of junior doctors in the workplace? Adv Med Educ Pract. 2015;6:583–588. | ||
Phillip H, Fleet Z, Bowman K. The European Working Time Directive-interim report and guidance from The Royal College of Surgeons of England Working Party. London: Royal College of Surgeons; 2003. | ||
Chikwe J, de Souza AC, Pepper JR. No time to train the surgeons: More and more reforms result in less and less time for training. BMJ. 2004;328(7437):418–419. | ||
Reznick RK, Macrae H. Teaching surgical skills-changes in the wind. N Engl J Med. 2006;355(25):2664–2669. | ||
Lave J, Wegner E. Situated Learning: Legitimate Peripheral Participation. Cambridge: Cambridge University Press; 1991. | ||
Fernando N, Mcadam T, Youngson G, Mckenzie H, Cleland J, Yule S. Undergraduate medical students’ perceptions and expectations of theatre-based learning: how can we improve the student learning experience? Surgeon. 2007;5(5):271–274. | ||
Union Europeenne des medecins specialistes european union of medical specialists. Training Requirements for the Specialty of …. Available from: https://www.uems.eu/__data/assets/pdf_file/0015/1554/UEMS_2012.29_-_Template_structure_for_European_Training_Requirements.pdf. Accessed April 27, 2018. |
Supplementary material
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

