Back to Journals » International Journal of General Medicine » Volume 13
Group B Streptococcal Meningitis in a Healthy Young Woman: A Case Report
Authors Payus AO, Clarence C , Azman Ali R
Received 19 August 2020
Accepted for publication 11 September 2020
Published 14 October 2020 Volume 2020:13 Pages 861—864
DOI https://doi.org/10.2147/IJGM.S277394
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Video abstract presented by Alvin Oliver Payus.
Views: 545
Alvin Oliver Payus,1 Clarita Clarence,2 Raymond Azman Ali2
1Faculty of Medicine and Health Science, Universiti Malaysia Sabah (UMS), Sabah, Malaysia; 2Department of Internal Medicine, Universiti Kebangsaan Malaysia Medical Centre (UKMMC), Kuala Lumpur, Malaysia
Correspondence: Alvin Oliver Payus
Faculty of Medicine and Health Science, Universiti Malaysia Sabah, Jalan UMS, 88400 Kota Kinabalu, Sabah, Malaysia
Tel +6018-8703503
Fax +6088-320 000
Email [email protected]
Abstract: Group B streptococcus (GBS) is a rare cause of meningitis in adults that commonly affects patients with multiple underlying comorbidities. Although it is uncommon, it typically progresses very rapidly and has a high mortality rate as compared to other causes of bacterial meningitis. Here, we report a patient with GBS meningitis who had no underlying medical illness and presented with multiple episodes of seizure within hours of developing fever. Cerebrospinal fluid analysis results were consistent with bacterial meningitis, and blood cultures grew GBS. She was treated with intravenous ceftriaxone for 2 weeks and made a great recovery without any sequalae. In conclusion, although GBS meningitis is uncommon in adults, it is a serious medical disease and associated with a high mortality rate. To the best of our knowledge, this patient represents one of the few reported cases of GBS meningitis in a previously healthy young adult.
Keywords: group B streptococcus, meningitis, young adult, seizure, ceftriaxone
Introduction
Group B streptococcus (GBS), or Streptococcus agalactiae, is a major cause of meningitis in neonates and children younger than 3 years old, as a result of vertical transmission through the contaminated birth canal during labor. It is an uncommon cause of bacterial meningitis in adults, with a high mortality rate, and usually affects the elderly or patients with chronic illnesses such as diabetes, liver cirrhosis, renal failure, and many others.1 Here, we report a case of a GBS meningitis in a previously healthy young lady, and this uncommon cause of bacterial meningitis in adults is the center of discussion in this case report.
Case Report
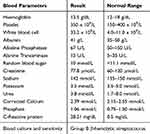
A 38-year-old lady who was teetotall and had no known medical illness presented with a 1 day history of fever. She denied having any runny nose, cough, sore throat, shortness of breath, altered bowel habit, or vomiting. She was single, worked as a cashier in a supermarket, and lived with her mother in an apartment. On the day of admission, she developed severe headache over the frontal area which was throbbing in nature, non-radiating, associated with dizziness and vomiting for two times, had no exacerbating or relieving factor, and the severity score was eight over ten. She was brought to the hospital by her mother. While on the way to the hospital, she developed a generalized tonic-clonic seizure which aborted spontaneously after 5 minutes. Upon arrival to the emergency department, she was febrile with the temperature of 39°C, and her vital signs were stable with blood pressure of 130/70 mmHg, pulse rate of 100 beats per minute, and respiratory rate of 20 breath per minute. She appeared drowsy with a Glasgow coma scale of 11/15 (E3, V3, M5). There was neck stiffness and jolt accentuation present. Examination of the nervous system revealed no abnormal finding. Her abdomen was soft, not tender, with no palpable mass or organomegaly. Her cardiorespiratory system was also normal. Routine blood investigation was taken and shows marked leucocytosis with elevated C-reactive protein (CRP). Otherwise, her liver and renal function were normal (as shown in Table 1). While in the emergency department, she developed another two episodes of generalized tonic-clonic seizure which lasted about 5 minutes each. She was given a loading dose of intravenous (IV) phenytoin 1.2 gm, and 100 mg three times daily thereafter. Computed Tomography scan of the brain was done and showed no intracranial bleeding and no visible abnormality (as shown in Figure 1). Lumbar puncture for cerebrospinal fluid (CSF) analysis was done (as shown in Table 2). The opening pressure was 30 cm H20 which was high, the CSF protein was high, at 3965 mg/dL, CSF glucose was 1.88 mmol/L, which was less than 60% of the random blood sugar, and CSF white blood cell was markedly elevated at 2100/μL with 70% neutrophil. The polymerase chain reaction for viral pathogen panel and Indian ink were otherwise negative. Bacterial meningitis was suspected and she was started on IV ceftriaxone 2 gm twice daily and IV acyclovir 500 mg three times daily. The latter was then stopped after her blood culture, which was taken on the day of admission, came back positive for Group B β-hemolytic Streptococcus and it was sensitive to penicillin and ceftriaxone. Her condition clinically improved after a few days, while her white cell count went down to 5.1x109/L, CRP went down to 3.82 mg/dL, and her fasting blood glucose level was 5.8 mmo/L. She was discharged after completing her IV ceftriaxone for 2 weeks with oral phenytoin 100 mg three times daily, which is planned to be continued for at least 6 months.
 |
Figure 1 Computed Tomographic imaging of the brain done on admission, showing no intracranial bleeding and no space occupying lesion. |
Discussion
Group B streptococcus (GBS), or Streptococcus agalactiae is an encapsulated, Gram positive β-hemolytic facultative bacteria that produce a narrow zone of hemolysis on a sheep blood agar. Although it normally colonizes in the gastrointestinal and genitourinary tract of an asymptomatic hosts,2 GBS is one of the leading causes of sepsis and meningitis in children younger than 3 years old, especially in the neonates.1,2 It is, however, an uncommon cause of community-acquired bacterial meningitis in adults where it accounts only in 1.3% of total meningitis cases in adult,2 and usually occurs in the elderly or in patients with severe underlying comorbidities that increased risk of infections, such as diabetes mellitus, liver cirrhosis, advance kidney disease, chronic alcoholism, or having a distant foci of infections.3,4
The clinical manifestation of GBS meningitis is similar with meningitis caused by other pathogens, which is acute onset and associated with neurological dysfunction.5 In spite of that, GBS meningitis will usually progress very rapidly and the patient will normally present within 24 hours of symptoms onset, as compared to bacterial meningitis of other causes. Apart from that, GBS meningitis is considered very dangerous as the mortality rate is about 27–34%, which is relatively higher compared to meningococcal meningitis.1 Factors associated with high mortality include advanced age, the presence of neurological complications such as coma or focal localizing signs, and systemic complications such as respiratory failure, kidney failure, shock, or consumption coagulopathy.2–4
In terms of treatment, the majority of GBS infections are fortunately still sensitive to the penicillin group of antibiotics, as well as cephalosporins and vancomycin as the alternatives.6 Therefore, a high index of suspicion among clinicians in order to initiate the appropriate treatment timely is the key to successful treatment of GBS meningitis.
Unlike the other cases reported in the literature, our patient was a young lady with no underlying medical illness and was not taking any medication that could increase the risk of infection. She developed generalized tonic-clonic seizure with 24-hours of developing fever and headache. She responded well to the antibiotic treatment, and was discharged well without any neurological impediment.
Conclusion
In conclusion, this case report serves to share an unusual cause of community acquired meningitis in a previously healthy young adult and, at the same time, to elucidate the importance of recognizing Streptococcus agalactiae as one of the potential pathogens in patients presenting with meningoencephalitis.
Consent for Publication and Ethics Approval
Written informed consent was obtained from the patient for her anonymized information to be published in this article. Our institution does not require ethical approval for reporting individual cases.
Acknowledgments
The authors would like to thank the Director General of Ministry of Health of Malaysia for his permission to publish this article. Professor Azman Ali is now affiliated with the Department of Medicine, Faculty of Medicine, Universiti Teknologi MARA, 47000 Sungai Buloh, Selangor, Malaysia.
Disclosure
None of the authors received financial support for this work and they do not have any conflicts of interest to disclose.
References
1. Khan FY. Streptococcus agalactiae meningitis in adult patient: a case report and literature review. Case Rep Infect Dis. 2016;21:2016.
2. van Kassel MN, Bijlsma MW, Brouwer MC, van der Ende A, van de Beek D. van de Beek D. Community-acquired group B streptococcal meningitis in adults: 33 cases from prospective cohort studies. J Infect. 2019;78(1):54–57. doi:10.1016/j.jinf.2018.07.009
3. Kjærgaard N, Bodilsen J, Justesen US, et al. Community-acquired meningitis caused by beta-haemolytic streptococci in adults: a nationwide population-based cohort study. Eur J Clin Microbiol Infect Dis. 2019;38(12):2305–2310. doi:10.1007/s10096-019-03678-w
4. Germano N, Sibbel MG, Summerfield D, Pitzenberger A. Group B streptococcus meningitis complicated by periodic lateralising epileptiform discharges in an elderly patient with type 2 diabetes mellitus. BMJ Case Reports CP. 2019;12(8):e228040. doi:10.1136/bcr-2018-228040
5. Thigpen MC, Whitney CG, Messonnier NE, et al. Bacterial meningitis in the United States, 1998–2007. N Eng J Med. 2011;364(21):2016–2025. doi:10.1056/NEJMoa1005384
6. van Kassel MN, van Haeringen KJ, Brouwer MC, Bijlsma MW, van de Beek D. van de Beek D. Community-acquired group B Streptococcal meningitis in adults. J Infect. 2020;80(3):255–260. doi:10.1016/j.jinf.2019.12.002
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.