Back to Journals » Research and Reports in Urology » Volume 14
Gross Hematuria Caused by Intravesical Migration of a Forgotten Intrauterine Device: A Case Report and Literature Review
Authors Salih MA, Tefera AT, Gebrehiwot FG , Mideksa AG , Halala NS, Gebreselassie KH
Received 3 March 2022
Accepted for publication 17 August 2022
Published 27 August 2022 Volume 2022:14 Pages 291—296
DOI https://doi.org/10.2147/RRU.S364889
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Panagiotis J Vlachostergios
Mohammed Abdulaziz Salih, Alemayehu Tegegne Tefera, Fitsum Gebreegziabher Gebrehiwot, Adugna Getachew Mideksa, Nebiyou Samuel Halala, Kaleab Habtemichael Gebreselassie
Urology Unit, Department of Surgery, St. Paul’s Hospital Millennium Medical College, Addis Ababa, Ethiopia
Correspondence: Kaleab Habtemichael Gebreselassie, Urology Unit, Department of Surgery, St. Paul’s Hospital Millennium Medical College (SPHMMC), Swaziland Street, Addis Ababa, Ethiopia, Tel +251 913632425, Email [email protected]; [email protected]
Abstract: Intrauterine device (IUD) is the second most widely used method of contraception worldwide. Up to 14% women prefer IUD for its attractive advantages such as cost effectiveness, high efficiency, and low complication rate. Despite these advantages, however, some complications may occur. One of these complications is uterine perforation and migration of the device to involve adjacent viscera such as peritoneum, bowel, vessels, and rarely bladder. IUD migration into the urinary bladder is uncommon, and only 70 cases are reported in the literature. Recurrent urinary tract infection and bladder calculi are the commonest presentations, and, rarely, women can present with gross hematuria. A high index of suspicion is needed in the evaluation of women who report pregnancy after IUD insertion as it might be the first clue to suspect migration. A forgotten and long-standing IUD increases the risk of uterine perforation and migration. A routine abdominal radiography, cystoscopy, and transvaginal ultrasonography are diagnostic. A computed tomography can also be employed in selected cases to delineate anatomic relations. Urologists should consider a vesical foreign body such as migrated IUD in women with recurrent lower urinary infections. Gross hematuria in a young woman should alert the urologist, and the evaluation should address a detailed contraceptive history. Every migrated IUD should be removed via endoscopy, laparoscopy, or open surgery. Proper follow-up and education of women before and after IUD insertion is also recommended to pick up on complications in time. Here, we report the successful open surgical treatment of a woman who had a forgotten IUD for 15 years and ultimately presented with gross hematuria due to trans-vesical migration. As to our literature search, there was no similar case reported from a urology center from Ethiopia.
Keywords: gross hematuria, migrated IUD, uterine perforation, contraceptive, bladder calculi
Introduction
Intrauterine device (IUD) is the second most widely used method of contraception worldwide. Up to 14% women prefer IUD for its attractive advantages such as cost effectiveness, high efficiency, low complication rate, as well as durable and reversible effects. Despite these advantages, however, some complications of IUD have been reported. One of these complications is transmural migration of the device to involve adjacent viscera such as peritoneum, bowel, vessels, and rarely bladder. Depending on the pattern of migration and its consequences, gynecologists, urologists, and general surgeons can be involved in the management of these patients.1–3
Extrauterine migration of IUD is an uncommon but feared complication. Full thickness erosion of the uterus is reported in up to 1.6 cases per 1000 IUD insertions.4,6 It is often reported after a preceding event of iatrogenic uterine wall perforation during insertion. Occasionally, it can occur spontaneously despite a proper IUD placement. The most common sites of migration are the peritoneal cavity, rectum, colon, and bladder.7 The symptoms caused by IUD migration can be quiet variable depending on the organ involved.8,9
Uterine wall perforation with an associated trans-vesical migration is uncommon.3,7 Recurrent urinary tract infection (UTI) and bladder calculi are the commonest presentations, and, rarely, women can present with gross hematuria.7–9 Here we report successful open surgical treatment of a woman who had a forgotten IUD for 15 years and ultimately presented with gross hematuria from trans-vesical migration. As to our literature search, there was no similar case reported from a urology center from Ethiopia.10
Case Presentation
A 38-year-old female presented to our center with a recurrent gross hematuria for the past six months. She also reported an intermittent attack of lower abdominal pain and storage lower urinary tract symptoms (LUTS) over the last 15 years. She visited multiple health care centers and was repeatedly diagnosed with urinary tract infection (UTI) for which she took multiple antibiotic regimens. A new onset of intermittent gross hematuria started six months ago with a noticeable worsening in amount periodically during menstrual flow.
She also reported passage of stone fragments during micturition in the same year. She gave birth to two children vaginally and has a regular menses. She had no history of surgical procedures in her past. Her general and pelvic examination was unremarkable. Laboratory work-up results were normal except the detection of multiple red blood cells (RBCs) on urine microscopy and E. coli on urine culture. She was treated with ciprofloxacin for one week.
An abdominopelvic ultrasound study performed by a resident trainee returned to be normal. The urologist suspected a possible bladder tumor and ordered cystoscopy. A rigid cystoscopy was performed after two weeks and revealed a T-shaped whitish material attached to the posterior bladder wall with small calculi over its surface (Figure 1A and B). A trial of cystoscopic removal with a forceps was unsuccessful as it was adherent to the bladder wall. A migrated IUD was suspected from the shape of the material, and a computed tomography (CT) scan was sent for complete evaluation of the scenario. Moreover, the patient was requested for a detailed contraceptive history, and she reported insertion of IUD 15 years back at a local health center. She did not return to the health center for follow-up visit as she was not told to do so. She was sexually active for the past 15 years and got pregnant twice in the past fifteen years approximately two and four years after the IUD insertion, respectively. During both pregnancies, she did not report it to the health center.
 |
Figure 1 A cystoscopic view of a migrated IUD by eroding through the posterior wall (A) and associated encrustation over its surface (B). |
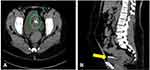
Delivery of both pregnancies occurred vaginally at home without a pre-natal follow-up. The CT scan result showed a T-shaped material penetrating halfway into the posterior bladder wall with no attachment to the uterus (Figure 2A and B). No separate vesical or renal calculi were identified. After consultation with the patient, an open trans-vesical surgical exploration under spinal anesthesia was decided.
The operative findings showed normal appearing bladder mucosa with an encrusted Copper T380A IUD attached to the posterior wall. It was dissected off the surrounding mucosa and successfully extracted together with the stone fragments attached to it (Figure 3). The bladder wall was repaired, and a Foley catheter was left in place. The patient was discharged on the next day without complication, and the catheter was removed on the seventh postoperative day.
 |
Figure 3 Intraoperative pictures showing anteriorly opened bladder wall with the IUD impacted in the posterior wall (A) and the forgotten device extracted in its intact form (B). |
Discussion
Multiple benign and malignant pathologies are known to cause hematuria. A report of gross hematuria should be seen seriously regardless of the number of occurrences, as it might be a sign of malignant pathology. Intravesical foreign bodies are among the least common causes of hematuria encountered by a urologist.2 Many types of vesical foreign bodies are reported in the literature, and a migrated IUD is among the least common ones.1–3
IUD is a well-known and preferred method of contraception in the developing world.11,12 It is easily inserted, has a reversible effect, has a high success rate, and causes few side effects. The common IUD types currently in use are the copper-releasing IUD (TCu-380A) and the Levonorgestrel-releasing IUD (LNG-IUD).1,2 The use of IUD is associated with a 0.2–3.6/1000 overall complication rate.3,13 Uterine wall perforation is the least common and the most feared complication of IUD insertion. It is mostly iatrogenic (primary), occurring at the time of IUD insertion, and the manifestations are immediate with pain and vaginal bleeding. Occasionally, perforation can be spontaneous (secondary) which occurs at a later time, after insertion, likely due to chronic inflammatory process or spontaneous uterine contractions.11,13,15 We believe that our patient had a spontaneous uterine perforation and subsequent intravesical migration as she did not have any immediate complication after the IUD insertion. Spontaneous uterine perforation is very rare, with an incidence of 0.12–0.68/1000 insertions.4,14 There are only few case series and reports in the literature regarding involvement of urinary bladder.1,12–15 Moreover, our encounter of a migrated IUD in a lady with gross hematuria and a suspected bladder tumor is the first of its kind to be reported in Ethiopia.
Many reports indicate that factors like lactational period, congenital uterine abnormality, previous pelvic surgery, postpartum period, and insertion by a non-experienced physician can increase the risk.7,14 Once uterine perforation occurs, the likelihood of IUD migration is high and the subsequent clinical manifestation of women with this complication depends on the organ or cavity involved.8 Accordingly, uterine perforation and IUD migration is classified into complete and partial (Table 1). The most involved sites are the peritoneal cavity, pouch of Douglas, and colon.2,7,12,15,16
 |
Table 1 Types of IUD-Related Uterine Perforations Based on the Extent of Device Migration.16 |
Intravesical IUD migration is a rare complication, and it is reported to commonly occur 2–10 years after device insertion.3,5–8 Our patient was carrying the device for 15 years, and she did not realize its presence despite having two successful pregnancies. Lack of awareness about the device and failure to return to the health center for a follow-up visit are the gaps we identified in our patient. Adequate counseling of women before and after an IUD insertion is recommended to avoid this kind of complication. A migrated IUD into the bladder has no specific symptoms, but rather its symptoms resemble those of UTI, bladder calculus, or a tumor. LUTS are the commonest manifestations, and a recurrent UTI is the usual initial diagnosis.11,13,14 Local mucosal irritation by the copper IUD, proliferation of bacteria, and organization of calculi over the foreign body nidus are responsible for the symptoms.14 Many patients including our case visit multiple physicians looking for a cure without realizing that the primary problem is with the incomplete diagnosis. Our patient reported an intermittent gross hematuria that alerted the urologist to suspect a bladder tumor and order a cystoscopy. A high index of suspicion is needed when urologists evaluate such cases. Women with episodes of recurrent UTI should be worked up for the presence of a persistent risk factor such as a stone or foreign body. A detailed contraceptive history should not be overlooked, as it was the most important diagnostic tip in our patient.1,2,12
The most important clues in the diagnosis of a migrated IUD are failure to visualize the device string at the cervical os and the presence of intrauterine pregnancy. Transvaginal ultrasonography is the best method to localize a suspected migration.10,12–15 An abdominal ultrasonography can also detect a migrated device, but the sensitivity may not be satisfactory. Studies have shown that up to 50% of migrated IUDs can be missed by abdominal ultrasound alone.7,8 A noticeable discrepancy is also reported between the IUD location indicated by ultrasound and subsequent actual location during surgery. In our patient, a normal finding was reported on abdominal ultrasound study; being an operator-dependent technique may have contributed to the low sensitivity. An abdominopelvic radiograph can also be helpful as the device is radiopaque. Cystoscopy is recommended if patient symptoms suggest bladder involvement.3,12,15,16 Our patient’s problem was diagnosed by cystoscopy that was ordered to evaluate a suspected bladder tumor. One of the complications associated with a long-standing migrated IUD is formation of strong local adhesion. In such cases, a contrast-enhanced CT scan is recommended to define the device orientation and possible local attachment.1,16,17
A recommendation from the World Health Organization (WHO) states that migrated IUDs should be removed as soon as they are diagnosed. Neglected cases might end up in severe morbidity and complex lower urinary tract reconstruction procedures.12,17 The management of an intravesical IUD can be variable depending on many factors. Cystoscopy-guided removal is often employed in a complete intravesical migration of IUD.8,11 An encrusted device might require additional fragmentation procedure. Laparoscopic or open surgical removal can also be used in difficult cases.10 At times, IUDs can be impacted in the bladder wall, necessitating an open partial cystectomy.2,5 There are few reports on a modified cystoscopic extraction of embedded IUDs where the bladder mucosa is incised with a J-hook monopolar electrocautery to facilitate removal. However, unless the extraction is performed by experienced hands, the risk of urine leak and uterovesical fistula can be significant.1,3,8,17 In our patient, a trial of cystoscopic removal was unsuccessful due to tight local adhesion, and hence an open trans-vesical removal was performed.
Uterine perforation by IUD should be detected early as failure to do so leads to device migration. Procedures performed by experienced hands are less likely to be complicated with perforation.9,16 Moreover, women should be advised on possible complications and the need for regular follow-up. Had our patient been fully aware of the use and complications of IUD, she would have realized failure of her contraceptive device at the time of her pregnancy. A thorough contraceptive history should not be overlooked in any patient with recurrent UTI and hematuria.12,17
Conclusion
A vesical foreign body can be a cause of gross hematuria and recurrent UTI. A urologist should have a high index of suspicion during evaluation of hematuria in women of reproductive age. Pregnancy after IUD insertion should alert a urologist about a possible uterine perforation and migration. The diagnosis of migrated IUD should be made easily with clinical history, ultrasonography, and pelvic radiography. Early referral to a urologist is also needed if urinary symptoms dominate. Endoscopic, laparoscopic, and open surgical techniques can be used for removal of the migrated IUD. Proper counseling of patients is mandatory before and after IUD insertion so that complications will not be neglected.
Physicians should always rely on clinical history and physical examination as they form the foundation for the clinician’s practice. Unless there is a high index of suspicion, dwelling only on modern investigation modalities such as ultrasonography might be misleading.
Abbreviations
IUD, intrauterine device; CT, computed tomography; UTI, urinary tract infection; LUTS, lower urinary tract symptoms.
Data Sharing Statement
Data sharing is not applicable to this article as no datasets were generated or analyzed during the study.
Consent for Publication
Written and signed informed consent was obtained from the patient for the publication of this case report and accompanying images.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis, and interpretation, or in all these areas; took part in drafting, revising, or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Paré AK, Ouattara A, Yé D., et al. Management of intrauterine device migrated into the bladder: a case report and literature review. Case Rep Urol. 2020;1:31.
2. Akhtar OS, Rasool S, Nazir SS. Migrated intravesical intrauterine contraceptive devices: a case series and a suggested algorithm for management. Cureus. 2021;13(1):29.
3. Waqar M, Moubasher A, Ameen T, Robinson D, Walker NF. Erosion of an intrauterine contraceptive device into the urinary bladder: a case report. Case Rep Women’s Health. 2021;Jan(29):e00274. doi:10.1016/j.crwh.2020.e00274
4. Dimitropoulos K, Skriapas K, Karvounis G, Tzortzis V. Intrauterine device migration to the urinary bladder causing sexual dysfunction: a case report. Hippokratia. 2016;20(1):70.
5. Zhang NN, Zuo N, Sun TS, Yang Q. An effective method combining various endoscopes in the treatment of intravesical migrated intrauterine device. J Minim Invasive Gynecol. 2020;27(3):582. doi:10.1016/j.jmig.2019.07.024
6. Rasekhjahromi A, Chitsazi Z, Khlili A, Babaarabi ZZ. Complications associated with intravesical migration of an intrauterine device. Obstetrics Gynecology Sci. 2020;63(5):675–678. doi:10.5468/ogs.19105
7. De Silva WS, Kodithuwakku KA, Aponsu GU, Rathnayake RM, Rajasegaram E. A large bladder stone caused by the intravesical migration of an intrauterine contraceptive device: a case report. J Med Case Rep. 2017;11(1):1–4. doi:10.1186/s13256-017-1461-6
8. Alabi TO, Keshavamurthy M, Ahmed S, Ojewola RW, Jain M, Tijani KH. Combined laparoscopic and cystoscopic retrieval of forgotten translocated intrauterine contraceptive device. Nigerian J Surgery. 2018;24(1):48–51. doi:10.4103/njs.NJS_18_17
9. Akhtar OS, Rasool S, Nazir SS. Migrated intravesical intrauterine contraceptive devices: a case series and a suggested algorithm for management. Cureus. 2021;13(1):845.
10. Tan JH, Lip HT, Ong WL, Omar S. Intrauterine contraceptive device embedded in bladder wall with calculus formation removed successfully with open surgery. Malaysian family phys. 2019;14(2):29.
11. Qu R, Yang L, Dai Y. Cystoscopy to remove an intrauterine contraceptive device embedded in the urinary bladder wall: a case report and literature review. J Int Med Res. 2021;49(5):3000605211015032. doi:10.1177/03000605211015032
12. Kaplanoğlu M, Bülbül M, Yüce T, Kaplanoğlu D, Aban M. Mislocated extrauterine intrauterine devices: diagnosis and surgical management. J Turkish German Gynecol Assoc. 2015;16(2):91. doi:10.5152/jtgga.2015.15243
13. Makary J, Rathore P. Lost and forgotten: a case of intravesical migration of an intrauterine device. Urol Case Rep. 2021;39:101841. doi:10.1016/j.eucr.2021.101841
14. Shin DG, Kim TN, Lee W. Intrauterine device embedded into the bladder wall with stone formation: laparoscopic removal is a minimally invasive alternative to open surgery. Int Urogynecol J. 2012;23(8):1129–1131. doi:10.1007/s00192-011-1632-8
15. Christodoulides AP, Karaolides T. Intravesical migration of an intrauterine device (IUD)-case report. Urology. 2020;1(139):14–17. doi:10.1016/j.urology.2020.02.009
16. Rowlands S, Oloto E, Horwell DH. Intrauterine devices and risk of uterine perforation: current perspectives. Open Access j Contraception. 2016;7:19. doi:10.2147/OAJC.S85546
17. Basiri A, Shakiba B, Rostaminejad N. Removal of intramural trapped intrauterine device by cystoscopic incision of bladder wall. Int braz j urol. 2019;27(45):408–409. doi:10.1590/s1677-5538.ibju.2018.0056
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.