Back to Journals » Diabetes, Metabolic Syndrome and Obesity » Volume 13
Glycemic Control, Diabetes Complications and Their Determinants Among Ambulatory Diabetes Mellitus Patients in Southwest Ethiopia: A Prospective Cross-Sectional Study
Authors YimamAhmed M, Hambisa Ejigu S , Zewudie Zeleke A , Yimam Hassen M
Received 17 August 2019
Accepted for publication 26 March 2020
Published 9 April 2020 Volume 2020:13 Pages 1089—1095
DOI https://doi.org/10.2147/DMSO.S227664
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Antonio Brunetti
Mohammed YimamAhmed,1 Solomon Hambisa Ejigu,2 Ameha Zewudie Zeleke,2 Mohammed Yimam Hassen2
1Dubti General Hospital, Dubti, Afar Region, Ethiopia; 2Department of Pharmacy, College of Health Sciences, Mizan-Tepi University, Mizan-Aman, Ethiopia
Correspondence: Mohammed Yimam Hassen Email [email protected]
Background: Over the past two decades, the prevalence of diabetes has increased faster in low- and middle-income countries than in high-income countries. Regardless of the instant growth in the prevalence of diabetes in Ethiopia, up-to-date data regarding glycemic control and related complications of diabetes is inadequate. This study aimed to identify glycemic control and chronic complications and their determinants among ambulatory diabetic patients at Mizan-Tepi University Teaching Hospital (MTUTH).
Methods: We conducted facility-based cross-sectional study from February 25 to March 25, 2019, at Mizan-Tepi University Teaching Hospital. Patients’ demographic data, diabetes complications, and treatments were collected using pretested questionnaire and data abstraction format. Data was entered by using Epidata manager 4.0.2.101, and statistical analysis was done by SPSS version 21. Bivariate logistic regression was done to see the association between independent variables and glycemic control and complication. Multivariable logistic regression analyses using backward selection were done to identify the predictors of poor glycemic control and complication at a P-value of < 0.05.
Results: One hundred ambulatory diabetic patients were included in this study. The mean duration of diabetes and the mean age of the participants were 3.95± 5.85 and 46.66± 15.53 years, respectively. About 71 (71%) of the studied diabetic patients had uncontrolled fasting blood glucose (FBG) level. More than half of the diabetic patients (59%) developed chronic complications of diabetes. Low medication adherence (adjusted odds ratio (AOR)=11.78, 95%CI: 1.09– 17.17) and inappropriate doses in the first, second, and third clinic visits (AOR=7.70, 95%CI: 1.79– 33.01; AOR=8.09, 95%CI: 1.90– 34.33; AOR=4.34, 95%CI: 1.09– 17.17), respectively, were independent predictors of uncontrolled FBG. No variable was found to be an independent predictor of chronic diabetic complication on multivariable logistic regression analyses.
Conclusion: Poor glycemic control and diabetes complications among ambulatory diabetic patients were high. Low medication adherence and inappropriate doses in the first, second, and third clinic visits were independent predictors of poor glycemic control.
Keywords: diabetes, glycemic control, complications, Ethiopia
Introduction
Diabetes mellitus (DM) is a group of metabolic disorders characterized by hyperglycemia resulting from absolute insulin deficiency, relative insulin deficiency, and/or peripheral insulin resistance. Untreated and long-term hyperglycemia secondary to DM may irreversibly damage vital organ and results in retinopathy, nephropathy, neuropathy, and failure of other organs like heart and blood vessels.1 The overall global prevalence of DM is 8.8%. This infers that approximately 415 million people are living with diabetes. If this drift continues without any mediation, the number of diabetic patients is estimated to escalate to 642 million by 2040. Estimates by the International Diabetes Federation (IDF) propose about 29.3 million diabetic patients live on the continent of Africa. The projected global expenditure due to diabetes is about 673 billion dollars, of which, nearly 80% was attributed to rich countries while merely 20% was attributed to poor countries.2 DM prevalence has risen faster in low- and middle-income countries than in high income countries over the last 10 years.3 Most of the diabetic patients are unaware that they have the disorder and the rate of undiagnosed DM is relatively high in sub-Saharan countries, so that the patients are high risk of developing chronic diabeticcomplications. In addition to the current challenges of resource limitation, poor countries face a double burden from both communicable and noncommunicable diseases and associated risks.4 Studies reported that >60% of patients with diabetes had poor glycemic control despite strict adherence to clinical practice guidelines.5 Likewise, a study done in primary health clinics of Malaysia shown that hemoglobin A1C (HbA1c) levels was not achieved among diabetic patients. Drug utilization pattern, age, drug adherence, and duration of diabetes were factors that influenced the outcome of glycemic control.6 Moreover, the study conducted at Jimma University Medical Center (JUMC) showed that a substantial number of diabetic patients did not achieve the glycemic target. Antidiabetic treatment, educational status, occupation, and drug adherence of the patients were factors affecting glycemic control.7 Any types of long-term hyperglycemia due to DM may result in permanent organ damage in many parts of the body and it can intensify the premature risk of dying. The potential long-term complication of DM includes renal failure, stroke, heart attack, amputation of lower extremities, loss of vision, and nerve damage.3 These chronic complications are two to fivefold more prevalent among patients with diabetes.8 The study done in Addis Ababa at Minilik II hospital indicated that about 37.5% of diabetic patients had chronic complications. Peripheral neuropathy and retinopathy were the two most commonly diagnosed chronic complications of DM and attributed 35.2% and 31.4% of the cases, respectively.9 The study carried out at JUMC indicated that types of DM, duration of diabetes, age and sex of the patients significantly affects the development of long-term diabetic complications.10 Even though the prevalence of vision-threatening retinopathy is 7%, studies indicated that the prevalence of overall retinopathy is 35%. Diabetic patients with low socioeconomic status, type 1 diabetic patients, and those with longer duration of diabetes were associated with high prevalence of retinopathy. Adult diabetic patients are two to three times more likely to have cardiovascular diseases (CVD) than adults devoid of DM.3 Chronic diabetes complications can be delayed or prevented by controlling blood pressure, blood glucose and blood cholesterol to the normal level or as close as possible to the normal level.2 Studies have showed that poor glycemic control was associated with both micro and macro vascular complications.11 Among sub-Saharan African Countries, Ethiopia is in the top four countries where the prevalence of DM mellitus is relatively high. The rates of attendances and diabetic admissions in major hospitals have increased over the past two decades.12 In Ethiopia, the prevalence of DM has escalated and is becoming the major economic problem in medical admissions and drug expenditure.13 Regardless of the instant growth of the prevalence of DM in Ethiopia, up-to-date data regarding glycemic control and related complications of diabetes is inadequate. Moreover, there is conflicting data with regard to factors affecting glycemic control and no research was done on diabetic complications and its determinants in Southwest Ethiopia. Hence, the aim of this study was to explore the level of glycemic control, chronic complications of diabetes and their determinants in resource constrained setting.
Patients and Methods
Study Setting and Study Design
The study was done in MTUTH in Benchi-Shako Zone, South-west Ethiopia. The hospital has an outpatient service where ambulatory diabetic patients have a regular follow-up every month and sometimes every three months. A facility-based cross-sectional study was conducted prospectively at MTUTH from February 25 to March 25, 2019.
We received ethical clearance from Mizan-Tepi University Ethical review board and letter of permission was received from the chief executive officer of the hospital to access patients’ data. The ethical consideration involved Helsinki declaration statement of ethical principles for medical research involving human subjects. Accordingly, written informed consent was obtained from each study participant prior to data collection and the participants’ right to withdraw at any time of the interview was maintained. Similarly, generated scientific information does not pose any risk to the study participants. Patient charts were also handled properly and data was kept confidential and anonymous.
Patient Population
We undertook our study on 100 diabetic patients. The source populations were all adult diabetic patients who had regular follow-up at MTUTH while the study populations were all adult diabetic patients who attended diabetic clinics during study period and fulfill inclusion criteria. Diabetic patients with age ≥18 years, patients who were on antidiabetic medication and with at least three consecutive blood glucose measurements were included in our study. We excluded patients not willing to give written informed consent, patients who had active psychiatric diseases, and those patients who had incomplete medical records.
Data Collection and Outcome of the Study
The main outcomes of our study were glycemic control and chronic diabetes complications. Data abstraction format was used to extract relevant patient data on duration of illness, type of antidiabetic medication, type of diabetes, medication dose, blood glucose measurement, comorbid conditions, and chronic diabetes complications. We used a semi-structured questionnaire to collect patients’ sociodemographic data and medication adherence. Morisky Medication Adherence Scale (MMAS-8) for chronic diseases14 was utilized to collect information regarding patient’s medication adherence. MMAS is and eight-item questionnaire with dichotomous responses (yes/no) for the first seven questions and multiple choice for the last question. A numerical value of 1 was given for yes and 0 for no. If the patient answered never or rarely for the last question it was scored as 0 or 1 and if the patient replied other choices it was scored as 1. Adherence level was measured by taking the summation of the response of eight questions and categorized as high, medium or low, if the total score was 0, 1 to 2 and ≥3 respectively.
Statistical Analysis
Data was entered by using EpiData manager 4.0.2.101 (EpiData Association, Denmark) and statistical analysis was done by SPSS version 21 (IBM Corporation, Armonk, NY, USA). Bivariate logistic regression was done to see the association between independent variables and glycemic control and complications. Variables with P-value ≤0.25 on bivariate logistic regression were entered into multivariate logistic regression. Multivariable logistic regression analyses using backward selection were done to identify predictors of poor glycemic control and complications at P-value of <0.05 significant.
Operational Definitions and Definition of Terms
Comorbidity
The presence of other chronic diseases in addition to diabetic mellitus.
Fasting Blood Glucose
Blood glucose measured from venous blood after at least eight hours of overnight fasting.
Good Glycemic Control
Operationalized as if the patients had 70–130 mg/dL of fasting blood glucose (FBG) upon measurement of three consecutive visits.
Poor Glycemic Control
Operationalized as if the patients had >130 or <70 mg/dL of FBG upon measurement of three consecutive visits.
Results
Characteristics of Participants
Among 105 diabetic patients available during the study period, 100 of them fulfilled the inclusion criteria and were included in the study. The mean age of participants was 46.66±15.35 with range of 11–76 years. Fifty-eight (58%) of them were male. More than half (51%) of the patients had attended secondary school and about one third of them (34%) were government employees (Table 1).
 |
Table 1 Sociodemographic Characteristics of Ambulatory Diabetic Patients at MTUTH, February 25 to March 25, 2019 |
Clinical Characteristics of the Participants
Out of the entire 100 studied diabetic patients, 71 (71%) had poor glycemic control. The mean of FBG measured over three months was 158.75±47.61 mg/dL. The majority, 76 (76%), of the participants were type 2 diabetic patients. The mean duration of diabetes was 3.95±5.85 years. Approximately fewer than half of the patients (46%) were on antidiabetic medications for two to five years. Forty (40%) patients had at least one comorbidity, of which hypertension accounted 82.5% of total comorbidity. A majority, (59%) of the participants had developed chronic complications of diabetes. The most common chronic diabetes complication was peripheral neuropathy and accounted 69.5% of the cases (Table 2).
 |
Table 2 Disease-related Characteristics of Ambulatory Diabetic Patients at MTUTH, February 25 to March 25, 2019 |
Medication-related Factors
Twenty-nine (29%) of the participants were prescribed with insulin while metformin was prescribed for 27% of them. More than third (36%) of diabetic patients were taking the combination of glibenclamide and metformin. Fifty-nine (59%) diabetic patients were on monotherapy. Concerning the antidiabetic medications dose appropriateness in the last three clinic visits, nearly in two-thirds of the patients (63%) it was incorrect. Around half (48%) of the patients had medium level of medication adherence (Table 3).
 |
Table 3 Medication-related Characteristics of Ambulatory Diabetic Patients at MTUTH, February 25 to March 25, 2019 |
Predictors of Poor Glycemic Control
On multivariate logistic regression analysis, low adherence to medication (AOR=11.78, 95%CI: 1.09–17.17), inappropriate doses during the first clinic visit (AOR)=7.70, 95%CI: 1.79–33.01), inappropriate doses during second clinic visit (AOR=8.09, 95%CI: 1.90–34.33) and inappropriate doses during third clinic visits (AOR=4.34, 95%CI: 1.09–17.17) were independent risk factors of poor glycemic control among participants (Table 4).
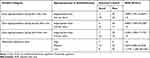 |
Table 4 Predictors of Poor Glycemic Control Among Ambulatory Diabetic Patients at MTUTH, February 25 to March 25, 2019 |
Predictors of Complications
Even if numerous variables were associated with diabetic complications on univariate analysis, no variable was found to be an independent predictor of complications on multivariable analysis (Table 5).
 |
Table 5 Predictors of Complications Among Ambulatory Diabetic Patients at MTUTH, February 25 to March 25, 2019 |
Discussion
This study set out the level of glycemic control and diabetes-related complications. Moreover, we have assessed the factors associated with poor glycemic control and diabetes-related chronic complications. Our study showed that the majority (71%) of patients had poorly controlled DM. The mean FBG was 158.75±47.61 mg/dL. This result is comparable with the study done at Jimma University Teaching Hospital7 where 70.9% of patients had poorly controlled diabetes. Our finding is higher than the Iranian study15 in which 56.3% of diabetic patients had poorly controlled diabetes and the findings of University of Gondar Hospital, Ethiopia16 where 60.5% of patients had poor glycemic control. This difference might be due to variations in the study settings, urbanization, the method of glucose measurement and study populations. For instance, in the Iranian study, all the participants were female diabetic patients.
Conversely, our result is lower than the findings in India11 and Kenya17 in which uncontrolled DM presented in 78.6% and 81.6% of diabetic patients. This discrepancy might be due to inconsistencies in the way of investigating blood glucose levels. HbA1C was used as assessment tool for glycemic control in former studies whereas FBG was used to assess glycemic control in present study.
Low level of medication adherence and inappropriate dose in the first, second, and third clinic visits were independent predictors of poorly controlled DM. This study showed that low level of adherence to the prescribed antidiabetic medications has a deleterious impact on glycemic control. The finding of this study was consistent with findings in research done in Malaysia,6 which indicated that glycemic control was higher among patients who adhered to their antidiabetic medications. This can be elucidated since effectiveness of drug treatment depends principally on the efficacy of the prescribed medication and adherence of the patient to the treatment. In our study, individuals taking inappropriate doses of antidiabetic medications were more likely to have uncontrolled DM compared to their counterparts.
Our study found that 59% of study participants had diabetes-related complications. This finding is considerably higher when compared to those from Minilik II hospital, Ethiopia9 where 37.45% of diabetic patients had one or more chronic complications of diabetes. Moreover, the finding of the present study is higher than that from the University of Gondar Hospital, Ethiopia16 in which chronic diabetes complications were found in 31.33% of diabetic patients. The variation in the sample size and level of care given to diabetes patients might have contributed to this discrepancy. In our set up, patients are often given care by general practitioners and nurses. It is afact that the most beneficial approach in preventing complications of diabetes is optimal treatment of hyperglycemia. Apart from that, the discrepancy might be attributed to the differences in the study settings. Conversely, our finding is comparable with the report in Jimma University Specialized Hospital10 where 52.5% of diabetic patients had one or more chronic complication.
Limitation of the Study
The main limitation of this study was the use of FBG in place of HbA1c to determine the glycemic status. In addition, the cross-sectional nature of the study and the small sample size to oversimplify the findings to the general population.
Conclusions
The prevalence of poor glycemic control and DM complications was noticeably high among diabetes patients. Low medication adherence level and inappropriate doses in the first, second, and third clinic visits were found to be independent predictors of poor glycemic control among diabetic patients. None of the variables were significantly associated with the development of diabetic complications.
Abbreviations
DM, diabetes mellitus; FBG, fasting blood glucose; HbA1C, glycated hemoglobin; IDF, International Diabetes Federation; MMAS, Morisky Medication Adherence Scale; SNNPR, Southern Nations Nationalities and Peoples Region.
Data Sharing Statement
The supporting documents for this study can be available from the corresponding author upon request.
Acknowledgments
We would like to acknowledge the study participants for their consent and patience during data collection.
Author Contributions
All authors contributed to data analysis, drafting and revising the article, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Disclosure
The authors declare that they have no competing interests.
References
1. Association AD. Standards of medical care WT C, editor. Diabetes Care. 2015.
2. Chapter 3 - The global picture. In: Cavan D, da Rocha Fernandes J, Makaroff L, Ogurtsova K, Webber S, editors. IDF Diabetes Atlas .
3. WHO. Global Report on Diabetes. WHO Library Cataloguing-in-Publication Data; 2016.
4. Mbanya JCN, Motala AA, Sobngwi E, Assah FK, Enoru ST. Diabetes in sub-Saharan Africa. Lancet. 2010;375(9733):2254–2266. doi:10.1016/S0140-6736(10)60550-8
5. Del Prato S, Felton AM, Murno N, Nesto R, Zimmet P, Zinman B. Improving glucose management_ ten steps to get more patients with type 2 diabetes to glycaemic goal. Int J Clin Pr. 2005;59(11):1345–1355. doi:10.1111/j.1742-1241.2005.00674.x
6. Su N, Islahudin F, Paraidathathu T, Paraidathathu T. Factors associated with good glycemic control among patients with type 2 diabetes mellitus. J Diabetes Invest. 2014;5(5):563–569. doi:10.1111/jdi.12175
7. Kassahun T, Eshetie T, Gesesew H. Factors associated with glycemic control among adult patients with type 2 diabetes mellitus: a cross - sectional survey in Ethiopia. BMC Res Notes. 2016;1–6. doi:10.1186/s13104-016-1896-7
8. Roman SH, Harris MI. Management of diabetes mellitus from a public health perspective. Endocrinol Metab Clin North Am. 1997;26(3):443–474. doi:10.1016/S0889-8529(05)70260-7
9. Ejigu A. Patterns of chronic complications of diabetic patients in Menelik-II hospital, Ethiopia. Ethiop J Health Dev. 2000;14(1):113–116.
10. Worku D, Hamza L, Woldemichael K. Patterns of diabetic complications at Jimma University specialized Hospital, Southwest Ethiopia. Ethiop J Heal Sci. 2010;20(March).
11. Gopinath B, Sri Sai Prasad M, Jayarama N, Prabhakara K. Study of factors associated with poor glycemic control in type −2 diabetic patients. Glob J Med Public Heal. 2013;2(2):1–5.
12. Abebe N, Kebede T, Addise D. Diabetes in Ethiopia 2000–2016 – prevalence and related acute and chronic complications; a systematic review. Afr J Diabetes Med. 2017;25(2):7–12.
13. Feleke Y, Enquselassie F. Cost of hospitalization of diabetic patients admitted at Tikur Anbessa Specialized Hospital, Addis Ababa, Ethiopia. Ethiop Med J. 2007;45(3):275–282.
14. Morisky DE, Green LW, Levine DM. Concurrent and predictive validity of a self-reported measure of medication adherence. Med Care. 1986;24:67–74. doi:10.1097/00005650-198601000-00007
15. Ghazanfari Z, Niknami S, Ghofranipour F, Larijani B, Agha-alinejad H. Determinants of glycemic control in female diabetic patients: a study from Iran. Lipids Health Dis. 2010;9(1):83. doi:10.1186/1476-511X-9-83
16. Fasil A, Biadgo B, Abebe M. Glycemic control and diabetes complications among diabetes mellitus patients attending at University of Gondar hospital, Northwest Ethiopia. Diabetes, Metab Syndr Obes Targets Ther. 2019;12:75–83. doi:10.2147/DMSO.S185614
17. Nduati NJ, Simon K, Eva N, Lawrence M. Factors Associated with glycemic control among type 2 diabetes patients attending Mathari National Teaching Hospital, Nairobi Kenya. J Endocrinol Diabetes. 2016;3(6):1–11. doi:10.15226/2374-6890/3/6/00162
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
