Back to Journals » International Journal of General Medicine » Volume 15
General Medicine Departments of Japanese Universities Contribute to Medical Education in Clinical Settings: A Descriptive Questionnaire Study
Authors Tago M , Shikino K , Hirata R , Watari T , Yamashita S , Tokushima Y, Tokushima M, Aihara H, Katsuki NE, Fujiwara M, Yamashita SI
Received 14 March 2022
Accepted for publication 27 May 2022
Published 23 June 2022 Volume 2022:15 Pages 5785—5793
DOI https://doi.org/10.2147/IJGM.S366411
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Masaki Tago,1 Kiyoshi Shikino,2 Risa Hirata,1 Takashi Watari,3 Shun Yamashita,1 Yoshinori Tokushima,1 Midori Tokushima,1 Hidetoshi Aihara,1 Naoko E Katsuki,1 Motoshi Fujiwara,1 Shu-ichi Yamashita1
1Department of General Medicine, Saga University Hospital, Saga, Japan; 2Department of General Medicine, Chiba University Hospital, Chiba, Japan; 3General Medicine Center, Shimane University Hospital, Shimane, Japan
Correspondence: Masaki Tago, Department of General Medicine, Saga University Hospital, 5-1-1 Nabeshima, Saga, 849-8501, Japan, Email [email protected]
Background: It is unclear how much effort Japanese university general medicine (GM) departments, which teach basic medical skills and have a high affinity for clinical practice, devote to medical education, particularly undergraduate education. This study aimed to clarify the contribution of GM departments of Japanese universities to medical education.
Patients and Methods: This was a questionnaire-based descriptive study of GM departments of Japanese universities. We sent the questionnaire created using Google Forms by email, and the universities responded by Internet. The department chairperson of the universities’ main hospital was responsible for completing the questionnaire. It covered the number of staff, inpatients over the previous 3 years, affiliated hospitals, classroom lectures, and practical training sessions per year for each academic year in medical faculty and students accepted for clinical clerkship. Items also included the effort for clinical training, research, and education and the effort for undergraduate, initial clinical residency, and specialty program training.
Results: In all, 46 of 71 universities responded, and we included 43 in our analysis. The median number of medical staff was 7; the median number of inpatients over the previous 3 years was 76. The median number of classroom lectures of the GM department was 1 for 1st-year, 5 for 3rd-year, 9 for 4th-year, and 0 for 2nd-, 5th-, and 6th-year students. The median total number of accepted students for clinical clerkship was 120. The median educational effort of the GM department was 30. With total educational effort set at 100, the median effort for undergraduate education was 45, for postgraduate residency 30, and for specialty program training 20.
Conclusion: The undergraduate medical education by GM departments of Japanese universities was provided mainly in clinical settings for almost all medical students. A focus on exposing students to GM in early academic years would improve the educational environment.
Keywords: clinical clerkship, general medicine, medical education, specialty program, university
Introduction
Until the 1990s, medical education in Japanese universities was traditionally teacher-centered, and focused on acquiring medical knowledge based on specialized organs.1,2 However, in recent years, there has been a gradual transition to learner-centered education.3,4 In 2001, the Model Core Curriculum for Medical Education was published,5 which clearly outlines the target image of physicians; it has been revised and now constitutes the basis for the medical education curricula at universities. The curriculum covers a wide range of topics regarding symptoms, pathological conditions, and clinical reasoning; it also addresses essential qualities and skills for physicians, such as professionalism, communication skills, quality and safety management of medical care, and self-improvement.5 Furthermore, in their curricula, medical universities are expected to provide extensive clinical clerkship for students toward acquiring clinical competencies that meet global standards.5,6 Clinical clerkship is expected to transition from an observation-based to a participation-based approach in which students participate in clinical care as members of a medical team.2 This transition is occurring as a result of the introduction of standardized achievement tests and legal changes allowing the certification of student doctors.7 The medical education curriculum in Japan consists of liberal arts and basic medicine in the 1st and 2nd years, clinical medicine in the 3rd and 4th years, and a clinical clerkship in the 5th and 6th years of medical school. The curricular structure is designed to overlap each area without a clear division in each year for 6 years of academic training.5
Japanese generalists play various roles in clinical practice; they must possess the skills to work in all settings, including inpatient, outpatient, emergency, intensive, and home care.8,9 Furthermore, contrary to specialists being subdivided by specific organs, they are expected to provide holistic, cross-sectional health care;8,10 they should also adopt roles in preventive medicine and patient education. Such roles are related to the topics listed in the Charter on Medical Professionalism.11,12 To promote the advancement of medicine, professionalism and ongoing education of colleagues and younger physicians are crucial. Therefore, generalists need to provide broad, deep education in various aspects of medicine. Specifically, they should instill in students in their early academic years the motivation to learn basic and clinical medical knowledge and foster the fundamental attitudes and mindsets needed in clinicians.13,14 For students in later academic years, they should teach specific clinical skills and encourage their use in clinical practice.
Generalists’ clinical practice is based on diagnostics;15,16 they are trained in skills related to clinical reasoning, such as medical interviewing, physical examination, selection and interpretation of examination findings, and understanding pathophysiology.8 Thus, undergraduate education by generalists can be expected to improve basic clinical skills.17–19 Residents’ basic clinical competencies improve when they rotate to general medicine departments; generalists should have a broad perspective rather than focusing on a single organ.20 Accordingly, general medicine is highly conducive to a well-rounded medical education. However, the general medicine education offered by Japanese universities has been considered immature, providing medical students little exposure to general medicine and having insufficient related policies.21,22 However, it is unclear how much effort Japanese university general medicine departments (whose personnel have basic medical skills and a high affinity for clinical practice) devote to medical education, particularly undergraduate education. Therefore, this study aimed to clarify the contribution of general medicine departments in Japanese universities to medical education and develop suggestions for future general medicine education at universities.
Materials and Methods
This was a questionnaire-based descriptive study of general medicine departments of the Council of Japanese University Hospitals for General Medicine. The Council’s membership comprises personnel from general medicine departments in university hospitals throughout Japan, and its annual meeting aims to promote communication and information sharing among Japanese university hospitals. Using the council’s mailing list, we sent an email to all 82 Japanese medical universities on June 28, 2021. We created the questionnaire using Google Forms, and each university responded using the Internet. The department chairperson of each university’s main hospital was responsible for completing the questionnaire, which required the department name and chairperson’s position to be stated. We excluded university-affiliated hospitals from this study because their size and role are such that they do not qualify as academic medical centers. In many cases, they serve as places for postgraduate training.
To ascertain the current state of education in the university general medicine departments, five staff members from the general medicine departments of the authors’ three universities developed the questionnaire items through discussions. All five staff members were assistant professors or associate professors and involved in teaching general medicine at their universities. The questionnaire was tested and validated by five physicians and some other doctors in a pilot trial. The questionnaire covered the following: number of staff; number of staff for each position; number of inpatients over the previous 3 years in the general medicine department; number of affiliated hospitals; annual number of classroom lectures and practical training sessions for each academic year in the medical faculty; number of students accepted for clinical clerkship and number of weeks of clerkship; required training period in general medicine department; effort for clinical practice, research, and education (combined score, 100, eg, clinical practice 35, research 35, and education 30); effort for undergraduate studies includes postgraduate residency (1st and 2nd postgraduate years), specialty program training (3rd to 5th postgraduate years), and other (combined score, 100, eg, undergraduate studies 35, postgraduate residency 35, and specialty program training 30). Effort is a subjective scale on which respondents evaluate their impressions of the overall cost and factors related to the time, human, funding, and psychological resources involved in the provision of medical education. Using multiple-choice questions, we asked about the following: presence or absence of a full-time educator (defined as more than 70% of time devoted to education); extracurricular education for students or residents and its frequency (choice of once a year or every 6 months, month, week, or day); and Internet-based extracurricular education for students or residents and its frequency (choice of once a year or every 6 months, month, week, or day).
We expressed continuous variables using medians (interquartile range [IQR]) and categorical variables using real numbers (percentages). Universities that did not provide complete answers to all questions in the questionnaire were excluded from the analysis. IBM SPSS Statistics (version 25.0, IBM, Armonk, New York, USA) was applied for the statistical analyses. We provided the information regarding this study on the first page of the Google Forms. All respondents gave their consent to answer the questionnaire and participate in the study. The Ethics Committee of Saga University Hospital waivered this study because it involved neither human subjects nor personal information, and university names were anonymized in the analysis.
Results
In all, 46 of the 71 universities with general medicine departments responded (response rate, 64.8%). We included 43 universities in our analysis after excluding 3 institutions with missing data (Figure 1). Of the 43 universities, the median number of department staff was 7 (IQR, 4–16); the median number of inpatients over the previous 3 years was 76 (IQR, 0–643); the median number of affiliated hospitals was 3 (IQR, 1–4); and 8 universities (19%) had a full-time educator in the general medicine department (Table 1). The median number of classroom lectures of the university general medicine department was 1 for 1st-year students, 5 for 3rd-year students, and 9 for 4th-year students. In the case of 2nd-, 5th-, and 6th-year students, there were no lectures. The median number of practical training sessions of the university general medicine department was 2 for 4th-year students. No practical sessions were conducted for 1st- to 3rd-year students. The median number of weeks of clinical clerkships was 40; the median number of accepted students was 120; and the median duration of required clinical clerkships by general medicine departments was 2 weeks (Table 2). The median educational effort of the university general medicine department was 30 (IQR, 25–40). With the total educational effort set at 100, the median effort for undergraduate education was valued at 45 (IQR, 30–60); the median effort for postgraduate residency was valued at 30 (IQR, 20–30); and the median effort for specialty program training was valued at 20 (IQR, 10–30). Regardless of the subject, over 90% of respondents stated that extracurricular education was offered less than once a week (Table 3).
 |
Table 1 Background of Japanese University General Medicine Departments |
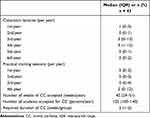 |
Table 2 Educational Activities of University General Medical Departments |
 |
Table 3 Effort and Extracurricular Education of University General Medical Departments |
 |
Figure 1 Data flow. |
Discussion
This study aimed to clarify the contribution of general medicine departments in Japanese universities to medical education and develop suggestions for future general medicine education. The general medical departments responded that they taught almost all medical students using clinical clerkship. General medicine departments at Japanese universities play various roles and are particularly burdened with clinical workloads,23 with only 15% of their working time reportedly devoted to education.24 Nevertheless, the effort dedication to education of the overall workload of general medicine departments was valued at 30%; this finding indicates that the departments made significant contributions to educational activities, including extracurricular education.
As specified in the Model Core Curriculum for Medical Education, bedside training is essential in medical education and general medical education in Japan.25–27 However, over half of general medicine departments in Japanese universities reportedly do not provide inpatient care.28 The median number of inpatients over the previous 3 years in the present study was 76, which suggests that hospital beds in general medicine departments are limited. The quality and quantity of inpatient care education in Japanese medicine have declined, resulting in fewer opportunities for acquiring clinical skills, such as physical examination and clinical reasoning.25 In general medicine in particular, clinical reasoning accounts for the bulk of the skills required.15,16 Thus, inpatient care education is crucial in general medicine departments of universities.
Teaching inpatient care provides students with visual, auditory, and tactile experience, and improves their medical interviewing, physical examination, and communication skills.26,27 The median number of full-time physician staff in this study was 7 (IQR, 4–16); thus, lack of human resources may be one reason for the small number of university general medicine departments providing inpatient care. In Japan, some university general medicine departments without hospital beds reportedly practice and teach inpatient care at affiliated hospitals or participating in training programs at other institutions for inpatient care education.29 One model for teaching inpatient care in university general medicine departments lacking hospital beds or with few inpatients is clinical visit teaching. This involves experienced general practitioners visiting training sites to evaluate and teach trainees.30,31 Generalists at universities could contribute to medical education through visit teaching, with students and residents being sent to affiliated community hospitals and providing clinical care at such hospitals. Some Japanese universities send generalists to regional community hospitals for medical education.29 Thus, general medicine departments in universities should provide students and residents with a better educational environment by supporting affiliated hospitals and improving the educational system according to regional circumstances.
The present study shows that general medicine departments in Japanese universities provide inadequate education for younger students—especially in their 1st and 2nd years. The median number of practical training sessions in the 1st–3rd year was 0 sessions/year; the median number of classroom lectures in the 1st–2nd year was similarly 0–1 lectures/year. Accordingly, medical students’ first exposure to general medicine is likely to be in their senior years. This study also found that the clinical effort in university general medicine departments (Table 3), where research and education workloads seem to be relatively high, exceeded 50%. This suggests that general medicine departments have a high affinity with clinical practice. This also indicates that university general medicine departments lack the capacity to sufficiently enough to the medical education of younger medical students with fewer clinical components in their learning. Early clinical exposure is essential in medical education because it motivates students to learn medicine and improves their academic achievements, clinical skills, and communication skills.32 In Europe, general practice and family medicine are a major component of the early clinical exposure of beginning-level undergraduate medical students.33 General medicine in Japan could play a similar role as in European general practice and family medicine by contributing to undergraduate clinical education. Physicians with whom students have contact in their early university years should serve as role models.34 Additionally, exposure to role models is strongly associated with medical students’ career preferences.35 Communication skills and systematic training in symptomatology and diagnostics, which form the foundation of clinical practice, are essential in early education. Community-oriented practice impacts medical students’ career preferences for general medicine and is a suitable topic for early clinical exposure of undergraduate medical students in the earlier academic years.36 Accordingly, general medicine departments, which focus mainly on such clinical skills, should vigorously promote such medical education in the early academic years. In Japan, there is still a shortage of trainees in general medicine;37 thus, greater involvement by generalists in medical education in the early academic years may contribute to more practitioners.
We found that the educational effort for specialty program training was lower than that for pre-graduation and postgraduate residency. The reform of Japan’s medical education system has historically focused on undergraduate and initial postgraduate education, and the government only established the specialty training system with national standards in 2018.38 Therefore, the Japanese perception may still be that specialty training in medical education is not particularly important. Because postgraduate education naturally includes fewer classroom lectures and less extracurricular education, our respondents may not have regarded clinical supervision as education. However, supervisors commonly teach trainees in specialty programs in clinical settings by working alongside them.22 Postgraduate residents and specialty trainees in general medicine could improve their clinical knowledge and skills and motivate their own learning by teaching junior residents and medical students in clinical clerkship. By doing so, they could elevate their status as good leaders.39,40 Working with learners at different levels (such as students, residents, specialty trainees, and specialists) could help those postgraduate residents and specialty trainees enhance their enjoyment of learning and expand their knowledge.41 Recognizing that the clinical setting is the best place for medical education and improving the teaching of specialty trainees in university general medicine departments could help improve the education of residents and medical students working with them. Better undergraduate education would likely lead to more specialty trainees in general medicine, which in turn could eventually aid in the advancement of academic hospitalists with the ability to practice medical education.42,43 Thus, improving undergraduate education in university general medicine departments is crucial to the departments’ development.8
This study has several limitations. It was a questionnaire-based study involving only general medicine departments of Japanese universities, and some universities did not respond. A simplified survey design focused on more explicit goals, as well as incentives to respond, could improve response rates. The questions regarding effort only queried the subjective impressions of the responding departments and may not constitute a well-defined target for evaluation. This was a descriptive study on education in general medicine departments of universities, and the effectiveness and impact of the education provided by those departments were not evaluated. Further research is required to elucidate these aspects.
Conclusion
The undergraduate medical education by general medicine departments of the responding universities was provided mainly in clinical settings for almost all medical students. Teaching of inpatient care could be undertaken by collaborating with affiliated hospitals and dispatching supervisor physicians from the university. General medicine departments could contribute to medical education by focusing on providing clinical exposure to general medicine and community-oriented practice to students in the early academic years, which would motivate students to engage in general medicine and would improve education for specialty trainees.
Abbreviation
IQR, interquartile range.
Ethics Approval and Informed Consent
This study involved neither human subjects nor personal information, and the university names were anonymized for the analysis.
Acknowledgments
We thank Dr. Taro Shimizu, Dokkyo Medical University, Dr. Yosuke Sasaki, Toho University School of Medicine, and Dr. Hiromizu Takahashi, Juntendo University for their support to this work. We thank Edanz for editing a draft of this manuscript.
Author Contributions
All the authors made a significant contribution to the work reported with respect to the conception, study design, execution, acquisition of data, analysis, and interpretation. All authors took part in drafting, revising, or critically reviewing the article, and they gave their final approval of the version submitted for publication. All the authors have agreed on the journal for submission and agree to be accountable for all aspects of the work.
Funding
There is no funding to report.
Disclosure
Masaki Tago is supported by grants from the Japan Society for the Promotion of Science, JSPS KAKENHI Grant Number JP18K17322 and JP21H03166. The sponsor of the study had no role in the preparation of the manuscript. The authors report no other conflicts of interest in this work.
References
1. Saiki T, Imafuku R, Suzuki Y, Ban N. The truth lies somewhere in the middle: swinging between globalization and regionalization of medical education in Japan. Med Teach. 2017;39(10):1016–1022. doi:10.1080/0142159X.2017.1359407
2. Izumi S. 1. Behavioral and social sciences in medical education today. Igaku kyoiku. 2021;52(2):121–127. (in Japanese).
3. Oda Y, Koizumi S. Status of medical education reform at Saga Medical School 5 years after introducing PBL. Kaohsiung J Med Sci. 2008;24(3 Suppl):S46–53. doi:10.1016/S1607-551X(08)70094-9
4. Karimi R. Interface between problem-based learning and a learner-centered paradigm. Adv Med Educ Pract. 2011;2:117–125. doi:10.2147/AMEP.S12794
5. Ministry of Education, Culture, Sports, Science and Technology [homepage on the Internet]. Model core curriculum for medical education in Japan; 2016. Available from: https://www.mext.go.jp/component/a_menu/education/detail/__icsFiles/afieldfile/2018/06/18/1325989_30.pdf.
6. Japan Accreditation Council for Medical Education [homepage on the Internet]. Background of JACME; 2021. Available from: https://www.jacme.or.jp/en/about/index.php. Accessed March 8, 2022.
7. Nakaya H. 3. Medical education in japan and national medical practitioner examination. Igaku kyoiku. 2015;46(1):14–17. (in Japanese).
8. Tago M, Watari T, Shikino K, Sasaki Y, Takahashi H, Shimizu T. A statement on the ten skills characteristic of exemplary Japanese hospitalist practice. J Hosp Gen Med. 2021;3(2):68–70.
9. Yokota Y, Watari T. Various perspectives of “General Medicine” in Japan-Respect for and cooperation with each other as the same “General Medicine Physicians”. J Gen Fam Med. 2021;22(6):314–315. doi:10.1002/jgf2.500
10. Kita K, Shimizu Y, Yamashiro S. Referral and consultation practice between generalists and specialists at a university hospital: a retrospective cross-sectional study. J Japan Prim Care Assoc. 2019;42(2):92–97. (in Japanese). doi:10.14442/generalist.42.92
11. Medical Professionalism Project. Medical professionalism in the new millennium: a physicians’ charter. Lancet. 2002;359(9305):520–522. doi:10.1016/S0140-6736(02)07684-5
12. ABIM Foundation. American Board of Internal Medicine; ACP-ASIM Foundation. American College of Physicians-American Society of Internal Medicine; European Federation of Internal Medicine. Medical professionalism in the new millennium: a physician charter. Ann Intern Med. 2002;136(3):243–246.
13. Verma M. Early clinical exposure: new paradigm in medical and dental education. Contemp Clin Dent. 2016;7(3):287–288. doi:10.4103/0976-237X.188536
14. Dornan T, Littlewood S, Margolis SA, Scherpbier A, Spencer J, Ypinazar V. How can experience in clinical and community settings contribute to early medical education? A BEME systematic review. Med Teach. 2006;28(1):3–18. doi:10.1080/01421590500410971
15. Yazdani S, Hosseinzadeh M, Hosseini F. Models of clinical reasoning with a focus on general practice: a critical review. J Adv Med Educ Prof. 2017;5(4):177–184.
16. Stolper E, Van Royen P, Jack E, Uleman J, Olde Rikkert M. Embracing complexity with systems thinking in general practitioners’ clinical reasoning helps handling uncertainty. J Eval Clin Pract. 2021;27(5):1175–1181. doi:10.1111/jep.13549
17. Kendrick T, Freeling P. A communication skills course for preclinical students: evaluation of general practice based teaching using group methods. Med Educ. 1993;27(3):211–217. doi:10.1111/j.1365-2923.1993.tb00259.x
18. Parle JV, Greenfield SM, Skelton J, Lester H, Hobbs FDR. Acquisition of basic clinical skills in the general practice setting. Med Educ. 1997;31:99–104. doi:10.1111/j.1365-2923.1997.tb02466.x
19. Janjigian MP, Charap M, Kalet A. Development of a hospitalist-led-and-directed physical examination curriculum. J Hosp Med. 2012;7(8):640–643. doi:10.1002/jhm.1954
20. Nishizaki Y, Shimizu T, Shinozaki T, et al. Impact of general medicine rotation training on the in-training examination scores of 11, 244 Japanese resident physicians: a Nationwide multi-center cross-sectional study. BMC Med Educ. 2020;20(1):426. doi:10.1186/s12909-020-02334-8
21. Nishikawa K, Ohta R, Sano C. The perception of rural medical students regarding the future of general medicine: a thematic Analysis. Healthcare. 2021;9(10):1256. doi:10.3390/healthcare9101256
22. Heist BS, Matsubara Torok H, Michael Elnicki D. Working to change systems: repatriated U.S. Trained Japanese physicians and the reform of generalist fields in Japan. Teach Learn Med. 2019;31(4):412–423. doi:10.1080/10401334.2019.1574580
23. Miyagami T, Yamada T, Kanzawa Y, et al. Large-scale observational study on the current status and challenges of general medicine in Japan: job description and required skills. Int J Gen Med. 2022;15:975–984. doi:10.2147/IJGM.S336828
24. Ministry of Health, Labour and Welfare [homepage on the Internet]. The 9th Study Group on Work Style Reform for Medical Doctors. Reference material #3, page 17; September 30, 2020. Available from: https://www.mhlw.go.jp/content/10800000/000677264.pdf. (in Japanese).
25. Peters M, Ten Cate O. Bedside teaching in medical education: a literature review. Perspect Med Educ. 2014;3(2):76–88. doi:10.1007/s40037-013-0083-y
26. Ahmed Mel-B K. What is happening to bedside clinical teaching? Med Educ. 2002;36(12):1185–1188. doi:10.1046/j.1365-2923.2002.01372.x
27. Crumlish CM, Yialamas MA, McMahon GT. Quantification of bedside teaching by an academic hospitalist group. J Hosp Med. 2009;4(5):304–307. doi:10.1002/jhm.540
28. Takeoka H, Horibata K, Masui S, Ajisaka K, Nabeshima S. Trends in departments of general medicine in university hospitals in Japan searched from websites. Med bull Fukuoka Univ. 2017;44(2):81–86.
29. Yokoya S. University-community collaboration with education as the key and contribution to community-based integrated care systems. J Health Care Soc. 2019;29(1):71–84. (in Japanese). doi:10.4091/iken.29-071
30. Fielding A, Mundy BE, Tapley A, et al. Study protocol: content and perceived educational utility of different modalities of clinical teaching visit (CTV) workplace-based assessments within Australian general practice vocational training: a cross-sectional study. BMJ Open. 2021;11(4):e045643. doi:10.1136/bmjopen-2020-045643
31. Remote Vocational Training Scheme LTD [homepage on the Internet]. Guide to conducting clinical teaching visits; 2018. Available from: https://rvts.org.au/downloads/Guide%20to%20Conducting%20Clinical%20Teaching%20Visits%202018.pdf.
32. Tayade MC, Latti RG. Effectiveness of early clinical exposure in medical education: settings and scientific theories - Review. J Educ Health Promot. 2021;10:117. doi:10.4103/jehp.jehp_988_20
33. Başak O, Yaphe J, Spiegel W, Wilm S, Carelli F, Metsemakers JF. Early clinical exposure in medical curricula across Europe: an overview. Eur J Gen Pract. 2009;15(1):4–10. doi:10.1080/13814780902745930
34. Haffling AC, Håkansson A, Hagander B. Early patient contact in primary care: a new challenge. Med Educ. 2001;35(9):901–908. doi:10.1046/j.1365-2923.2001.01001.x
35. Wright S, Wong A, Newill C. The impact of role models on medical students. J Gen Intern Med. 1997;12(1):53–56. doi:10.1007/s11606-006-0007-1
36. Ie K, Murata A, Tahara M, et al. What determines medical students’ career preference for general practice residency training?: a multicenter survey in Japan. Asia Pac Fam Med. 2018;17:1–6. doi:10.1186/s12930-018-0039-9
37. Ministry of Health, Labour and Welfare [homepage on the Internet]. The 1st meeting of the Medical Ethics Council, the Medical Doctors Association, the Division of Specialist Training for Medical Doctors. Reference material #1, page 8; September 17, 2021. Available from: https://www.mhlw.go.jp/content/10803000/000833608.pdf. (in Japanese).
38. Japanese Medical Specialty Board [homepage on the Internet]. Message from the Board Chairperson; June, 2021. Available from: https://jbgm.org/menu/%e7%b7%8f%e5%90%88%e8%a8%ba%e7%99%82%e5%b0%82%e9%96%80%e5%8c%bb%e6%a4%9c%e8%a8%8e%e5%a7%94%e5%93%a1%e4%bc%9a/#con1. (in Japanese). Accessed May 4, 2022.
39. Hill AG, Yu TC, Barrow M, Hattie J. A systematic review of resident-as-teacher programmes. Med Educ. 2009;43(12):1129–1140. doi:10.1111/j.1365-2923.2009.03523.x
40. Morrison EH, Hollingshead J, Hubbell FA, Hitchcock MA, Rucker L, Prislin MD. Reach out and teach someone: generalist residents’ needs for teaching skills development. Fam Med. 2002;34(6):445–450.
41. Thomson JS, Anderson K, Haesler E, Barnard A, Glasgow N. The learner’s perspective in GP teaching practices with multi-level learners: a qualitative study. BMC Med Educ. 2014;14:55. doi:10.1186/1472-6920-14-55
42. Nicholson S, Hastings AM, McKinley RK. Influences on students’ career decisions concerning general practice: a focus group study. Br J Gen Pract. 2016;66(651):e768–e775. doi:10.3399/bjgp16X687049
43. Alberti H, Randles HL, Harding A, McKinley RK. Exposure of undergraduates to authentic GP teaching and subsequent entry to GP training: a quantitative study of UK medical schools. Br J Gen Pract. 2017;67(657):e248–e252. doi:10.3399/bjgp17X689881
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
